Abstract
Purpose
The pathomechanism of cervical myelopathy due to cervical ossification of posterior longitudinal ligament (C-OPLL) remains unclear. No previous literature has quantified the influence of dynamic factors on cervical myelopathy due to C-OPLL. The purpose was to investigate the influence of dynamic factors on the spinal column in the patients with C-OPLL using CT scan after myelography (MCT).
Methods
The study included 41 patients with cervical myelopathy due to C-OPLL. An MCT was done during neck flexion and extension, and spinal cord cross-sectional areas (SCCSA) were measured at each disc level between C2/3 and C7/T1. Ossification morphology at each segment was divided into three groups, connection department, coating part, and non-connection department of OPLL group. Dynamic changes of SCCSA in each group of ossification morphology were calculated. The relationship between clinical results and SCCSA at the narrowest level was investigated.
Results
MCT showed SCCSA changes during neck extension; 7.4 ± 5.1 mm2 in the connection department, 5.8 ± 6.0 mm2 in the coating part, and 6.7 ± 6.4 mm2 in the non-connection department of OPLL group. There difference was not statistically significant. There was a weak correlation between the JOA score and SCCSA at the narrowest level (R = 0.49). There was no significant correlation between the recovery rate of JOA score and SCCSA at the narrowest level (R = 0.37).
Conclusion
Dynamic factors are seen both in cervical myelopathy patients with the continuous type of OPLL and others. Deterioration of myelopathy could be induced by motion effects even in the connection department of OPLL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent years, cervical spondylotic myelopathy (CSM) and compressive myelopathy caused by cervical ossification of posterior longitudinal ligament (C-OPLL) are increasing with the aging population. Dynamic factors are one of the causes of CSM [12]. However, the pathomechanism of cervical myelopathy caused by C-OPLL remains unknown. Despite spinal stenosis (6 mm < space available for the spinal cord <14 mm), myelopathy may not develop in patients with the severe limitation of range of cervical spine [5]. This indicates that not only static factors but also dynamic factors, such as listhesis or hypermobility at the discontinuity of the ossified lesion, play important roles in the development of myelopathy, especially in mixed and segmental OPLL. It is thought that spinal cord cross-sectional areas (SCCSA) in patients with C-OPLL slowly become narrower, and the influence of dynamic factors is not as important as in the patients with C-OPLL. However, this concept does not always apply to patients with C-OPLL. The purpose of this study was to measure SCCSA during flexion and extension in patients with C-OPLL, and to elucidate the influence of dynamic factors on the spinal cord in those patients.
Materials and methods
Forty-one patients (Male 32; Female 9) were enrolled in this study. Their average age was 63 years (44–81 years). All these patients had undergone surgical treatment for cervical myelopathy due to C-OPLL. The surgical methods of all cases were double-door laminoplasty. Informed consent was obtained from all patients before enrollment. Patients with spinal cord injury without radiological evidence of trauma were excluded from this study.
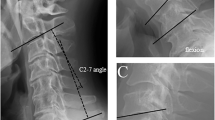
Preoperative CT scans after myelography (MCT) were taken in all subjects in maximum neck flexion and extension (Fig. 1). SCCSA at each disc level between C2/3 and C7/T1 in axial view were measured using imaging (NIH image) software (Fig. 2). The images were perpendicularly as much as possible. Ossification morphology at each disc segment was divided into three groups: connection department, coating part, and non-connection department of OPLL. The connection department of OPLL group included continuous type and localized type of OPLL. The coating part of OPLL group included tip of continuous type and segmental type of OPLL (Fig. 3). The relationship between dynamic changes of SCCSA and the type of ossification morphology was also investigated.
A functional scale based on the Japanese Orthopedic Association (JOA) score was used for the assessment of patient disability resulting from cervical myelopathy. The JOA score quantifies neurologic impairment by evaluating upper extremity function (4 points), lower extremity function (4 points), sensations (6 points), and urinary bladder function (3 points), amounting up to a full score of 17 points. The recovery rate after surgery was evaluated with the formula suggested by Hirabayashi et al. [2].
SCCSA during neck flexion and extension were measured twice [1], and these data never varied more than 5 % in the statistical analysis. Data analysis was performed with Stat View 5.0 software (ABACUS, Berkeley, CA). All the values are expressed as mean ± standard deviation. Correlation between the JOA score and SCCSA at the narrowest level and also correlation between recovery rate of the JOA score and SCCSA at the narrowest level were examined. Comparisons between the groups were performed using analysis of variance with a post hoc test (Kruskal–Wallis test). A P value < 0.05 was considered significant. Spearman rank correlation coefficient was used to determine correlations.
Results
The results of all SCCSA were summarized in Table 1.
There were 18 disc levels of the connection department, 21 disc levels of the coating part, and 207 disc levels of the non-connection department of OPLL group. The average SCCSA changes during flexion and extension were 7.4 ± 5.1 mm2 in the connection department, 5.8 ± 6.0 mm2 in the coating part, and 6.7 ± 6.4 mm2 in the non-connection department of OPLL group. There was no statistically significant difference (Fig. 4).
Spinal cord cross-sectional area according to ossification morphology at flexion and extension, and amount of change. The average SCCSA changes during flexion and extension were 7.4 ± 5.1 mm2 in the connection department of OPLL group, 5.8 ± 6.0 mm2 in the coating part of OPLL group, and 6.7 ± 6.4 mm2 in the non-connection department of OPLL group
The JOA score was 9.6 ± 3.0 points preoperatively, and 12.7 ± 2.5 points at the final follow-up. There was a weak correlation between the preoperative JOA score and SCCSA at the maximally stenotic level (R = 0.49, Fig. 5). The recovery rate of the JOA score was 42 ± 29 %. There was no significant correlation between the recovery rate of the JOA score and SCCSA at the narrowest level (R = 0.37, Fig. 6).
Discussion
The influence of dynamic factors on the cervical spine has been reported using flexion–extension MRI [4]. Dynamic factors are proposed to be involved in the pathogenesis of CSM. However, the pathomechanism of myelopathy in C-OPLL remains unknown. In addition, no previous literature has quantified the level of dynamic factor involvement in C-OPLL. Therefore, SCCSA using MCT were measured to elucidate the influence of dynamic factors. There was no significant difference in the dynamic changes of SCCSA between the connection department, coating part, and non-connection department of OPLL.
It is thought that SCCSA in patients with C-OPLL gradually become narrower [7]. It has been suggested that the influence of dynamic factors is less in patients with matured continuous OPLL. However, this concept does not always apply to all patients with continuous OPLL. Matsunaga et al. [8, 9] showed that in patients with C-OPLL, involvement of not only chronic pathologic compressive factors caused by OPLL but also of circulatory and dynamic factors were thought to be important in development and aggravation of myelopathy. Morio et al. [11] suggested that important factors in the onset or aggravation of myelopathy are related to pathological compression by OPLL, cervical soft disc herniation, a developmentally narrow spinal canal, and a local or non-proportional hypermobility.
Matsunaga et al. [6] also reported that during the natural course of OPLL in the cervical spine, 37 (22 %) of 167 patients developed or suffered from aggravated spinal symptoms. All patients with less than 6 mm space available for the spinal cord (SAC) suffered from myelopathy, whereas patients with 14 mm or greater did not. No correlation was found between the presence and absence of myelopathy in patients whose SAC diameter ranged from 6 to 14 mm. However, in this study, there was a weak correlation between the preoperative JOA score and SCCSA at the narrowest level. There is a possibility that myelopathy is aggravated by dynamic factors, even in the connection department of OPLL.
Uchida et al. [14] reported a significant correlation between the proportion of apoptotic oligodendrocytes in the compressed area of the spinal cord and the magnitude of cord compression in the spinal hyperostotic mouse (twy/twy). Sun et al. [13] suggested that regardless of hyperintensity on T2-weighted imaging or hypointensity on T1-weighted imaging on magnetic resonance imaging (MRI) in patients with OPLL, severe damage to the spinal cord is indicated. They recommended that surgical treatment should be provided before the advent of intramedullary spinal cord changes in signal intensity on MRI. Liu et al. [5] also suggested that preoperative assessment of cervical curvature, MRIT2 signal, and occupying ratio can be used to guide clinical surgical approach selection to potentially produce better long-term outcomes in patients with OPLL.
Turel et al. [10] reported that oblique cervical corpectomy for CSM preserves segmental and the whole spine ROM. The whole spine and segmental ROM decreased by 11.2° and 10.9°, respectively. The reduction in this ROM is probably related to degenerative ossification of spinal ligaments. Inoue et al. [3] reported a case with multiple-level cervical ossification of the ligamentum flavum (OLF) combined with calcification of the posterior atlanto-axial membrane and ligamentum flavum (CLF). Simultaneous development of cervical OLF and CLF in this case seems unlikely to have occurred coincidentally and suggests that the pathogenesis of OLF and CLF may share a common initiation factor.
Limitations of the study are examination about the ROM, the spinal cord changes in signal intensity on MRI, and existence of CLF. Examination will be necessary about the differences between the ROM based on MCT and based on X-ray. Examination is necessary about these relations and should assume it a help of the surgical method choice.
We should observe closely the natural course of patients with C-OPLL from dynamic factors even in patients with mature C-OPLL, and it will be necessary to think about treatment with dynamic factors.
Conclusions
This study was performed to measure SCCSA during neck flexion and extension in patients with C-OPLL, and to investigate the influence of dynamic factors on the spinal cord. The average SCCSA changes during flexion and extension were 7.4 ± 5.1 mm2 in the connection department of OPLL group, 5.8 ± 6.0 mm2 in the coating part of OPLL group, and 6.7 ± 6.4 mm2 in the non-connection department of OPLL group. There was no statistically significant difference. This study demonstrates that there is an influence of dynamic factors on spinal cord compression even in the connection department of OPLL.
References
Chen CJ, Hsu HL, Niu CC, Chen TY, Chen MC, Tseng YC, Wong YC, Wang LJ (2003) Cervical degenerative disease at flexion–extension MR imaging: prediction criteria. Radiology 227:136–142
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K (1981) Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 6:354–364
Inoue H, Seichi A, Kimura A, Endo T, Hoshino Y (2013) Multiple-level ossification of the ligamentum flavum in the cervical spine combined with calcification of the cervical ligamentum flavum and posterior atlanto-axial membrane. Eur Spine J 22(Suppl 3):416–420
Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K (2002) Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: more than 10 years follow up. J Neurosurg 96(2 Suppl):180–189
Liu H, Li Y, Chen Y, Wu W, Zou D (2013) Cervical curvature, spinal cord MRIT2 signal, and occupying ratio impact surgical approach selection in patients with ossification of the posterior longitudinal ligament. Eur Spine J 22(7):1480–1488
Matsunaga S, Kukita M, Hayashi K et al (2002) Pathogenesis of myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg 96:168–172
Matsunaga S, Sakou T, Taketomi E et al (1994) The natural course of myelopathy caused by ossification of the posterior longitudinal ligament in cervical spine. Clin Orthop Relat Res 305:168–177
Matsunaga S, Nakamura K, Seichi A et al (2008) Radiographic predictors for the development of myelopathy in patients with ossification of the posterior longitudinal ligament: a multicenter cohort study. Spine 33(24):2648–2650
Matsunaga S, Komiya S, Toyama Y (2013) Risk factors for development of myelopathy in patients with cervical spondylotic cord compression. Eur Spine J. [Epub ahead of print]
Turel MK, Sarkar S, Prabhu K, Daniel RT, Jacob KS, Chacko AG (2013) Reduction in range of cervical motion on serial long-term follow-up in patients undergoing oblique corpectomy for cervical spondylotic myelopathy. Eur Spine J 22(7):1509–1516
Morio Y, Nagashima H, Teshima R et al (1999) Radiological pathogenesis of cervical myelopathy in 60 consecutive patients with cervical ossification of the posterior longitudinal ligament. Spinal Cord 37(12):853–857
Sumi M, Osamu K, Satoru S et al (1998) Radiological analysis of cervical spondylotic myelopathy. Rinsho seikei geka 33(11):1277–1286 (in Japanese)
Sun Q, Hu H, Zhang Y, Li Y, Chen L, Chen H, Yuan W (2011) Do intramedullary spinal cord changes in signal intensity on MRI affect surgical opportunity and approach for cervical myelopathy due to ossification of the posterior longitudinal ligament? Eur Spine J 20(9):1466–1473
Uchida K, Nakajima H, Watanabe S, Yayama T, Guerrero AR, Inukai T, Hirai T, Sugita D, Johnson WE, Baba H (2012) Apoptosis of neurons and oligodendrocytes in the spinal cord of spinal hyperostotic mouse (twy/twy): possible pathomechanism of human cervical compressive myelopathy. Eur Spine J 21(3):490–497
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ito, K., Yukawa, Y., Machino, M. et al. Spinal cord cross-sectional area during flexion and extension in the patients with cervical ossification of posterior longitudinal ligament. Eur Spine J 22, 2564–2568 (2013). https://doi.org/10.1007/s00586-013-2982-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2982-3