Abstract
Purpose
The impact of percutaneous internal fixation as a supplement to percutaneous kyphoplasty (PKP) for the management of thoracolumbar burst fractures in elderly patients is unclear. We conducted a clinical controlled trial to investigate the effect and outcomes of this technique in such patients.
Methods
Forty-three patients over 65 years old with thoracolumbar burst fractures without nerve injuries were enrolled. They were randomly assigned to treatment with simple PKP (control group, n = 22) or percutaneous short-segment pedicle screw internal fixation with PKP (treatment group, n = 21). The patients were followed for at least 2 years postoperatively and were assessed with regard to clinical and radiological outcomes. Clinical outcomes were evaluated mainly with use of visual analog scale (VAS) for pain and the Oswestry Disability Index (ODI) questionnaire. Radiological outcomes were assessed mainly on the basis of Cobb kyphosis angle and loss of kyphosis correction.
Results
There were no significant differences between the two groups with regard to preoperative indices. The treatment group had better VAS scores and greater postoperative improvement on the ODI compared with the control group (P < 0.05). Postoperative kyphosis angle correction in the treatment group was superior to that in the control group, and loss of correction postoperatively was significantly less (P < 0.05). In the control group, two patients suffered refractures of the injured vertebra postoperatively and one had a fracture in the adjacent vertebra. No postoperative complications needing management were noted in either group.
Conclusions
Compared with simple PKP, percutaneous internal fixation with PKP is a valuable surgical option for the treatment of selected elderly patients with thoracolumbar burst fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Percutaneous kyphoplasty (PKP) is safe and effective in the management of thoracolumbar compression fractures in elderly patients. However, when PKP is used to treat thoracolumbar burst fractures, there are some defects such as bone cement leakage, or unsatisfactory reduction of fractures [1, 2]. Especially, postoperative complications like the adjacent vertebra fractures or the injured vertebra refractures may often occur, which always lead to severe pain and dysfunction [3, 4]. Pedicle screw internal fixation alone can achieve satisfactory reduction but may increase the trauma, and screw loosening often occurs due to senile osteoporosis; there is also a higher incidence of late kyphosis deformity [5–7].
Because some researchers have used short-segment pedicle screw internal fixation combined with percutaneous vertebroplasty (PVP) or PKP to treat thoracolumbar burst fractures in young adults [8–10], we wondered if PKP could be used after percutaneous internal fixation to treat thoracolumbar burst fractures in elderly patients. We conducted a prospective randomized controlled trial comparing simple PKP (control group) with percutaneous short-segment pedicle screw fixation with PKP (treatment group). Our hypothesis was that the efficacy of percutaneous internal fixation with PKP is superior to that of simple PKP in the management of thoracolumbar burst fractures in selected elderly patients.
Materials and methods
This prospective randomized controlled study was approved by the institutional review board and the ethics committee of our medical college. The included cases were elderly patients with a single-level thoracolumbar burst fracture (T11–L2) who were diagnosed and treated in our hospital’s spinal surgery unit between January 2007 and December 2008.
The inclusion criteria were: more than 65 years old, no or mild organic disease, clear history of trauma (e.g. fall, road traffic accident), imaging (radiography, computed tomography and/or magnetic resonance imaging) performed within 3 days after the injury showing a single-level vertebral burst fracture (involving the posterior wall of a vertebra), fragment of fractured lamina encroaching into vertebral canal by less than one-quarter of the canal’s transverse diameter, no nerve damage, decompression surgery not required, the fracture type belonged to type A3 according to AO classification. Exclusion criteria were: patient could not tolerate surgery, pathologic fracture, fracture associated with ankylosing spondylitis, and multiple osteoporotic fractures, fracture associated with disc damage.
Fifty-two consecutive patients met the criteria for inclusion. Four patients refused to undergo surgical treatment and five were lost to follow-up. Thus, forty-three patients were enrolled in the study, comprising 21 males and 22 females with an average age of 72.5 years. The cause of the injury was the ground falls in 19 patients, a bicycle or motorcycle accident in 12, a pedestrian–motor vehicle accident in 9, a fall from a height in 2 and a crush injury in 1. The level of injury was T11 in 4 patients, T12 in 11, L1 in 20 and L2 in 8. The load sharing scores of the patients were 2–7 according to McCormack’s method. All patients had no nerve damage when they were admitted to the hospital.
Informed written consent was obtained from each patient and his or her family, and the patients were then randomized on the basis of a computer-generated random-allocation sequence. 22 patients were randomized to treatment with simple PKP (PKP group, controls) and 21 were assigned to treatment with percutaneous short-segment pedicle screw internal fixation with PKP (PIF–PKP group, treatment). The baseline characteristics of the patients are displayed in Table 1. The treatment and control groups were similar with respect to most demographic variables (P > 0.05).
All enrolled patients of two groups were managed with posterior spinal operation by the same doctor at an average of 3.8 days (range 2–7 days) after the initial trauma. Patients in the PKP group were given general or local anesthesia and placed in the prone position so the spine was in hyperextension state. The range of reduction of the fracture site was felt under the proper pressure of the doctor’s palm. After disinfection and placement of sterile drapes, a skin incision of about 3 mm was made unilaterally in the pedicle of the injured vertebra. Under fluoroscopy using a C-arm X-ray machine, the injured vertebral segment was confirmed and a needle puncture channel was created. Percutaneous puncture balloon kyphoplasty (Shandong Guanlong Company of China) was then performed, and polymethylmethacrylate (PMMA) bone cement (Tianjin Synthetic Materials Company of China) was prepared and pushed into the injured vertebral body under low pressure while in its dough state.
Patients in the PIF–PKP group were placed in the prone position under general anesthesia with endotracheal intubation. Using a specialized metal frame, the projected positions of the pedicle of the injured vertebra and the adjacent upper/lower segments were marked on the body surface preoperatively. After disinfection and placement of sterile drapes, four skin incisions of about 1.5 cm were made at the surface markers (Fig. 1). Four pedicle screws were then implanted percutaneously under C-arm X-ray machine monitoring, pre-bent longitudinal connecting rods were then inserted into the U-shaped slots of the screws under the paraspinal muscles. The distraction reposition of the fractured vertebra was performed along the longitudinal direction of the connecting rods using a distraction and compression tool which is matched with percutaneous transpedicular systems, and the screws were tightened after a satisfactory vertebra reduction. Subsequently, PKP was performed. Avoiding the longitudinal connecting rods, a trocar of 5 mm diameter was inserted into the injured vertebral body in the side of the pedicle with the larger E-angle, which enabled puncture close to the vertebral midline (Fig. 1). Bone cement was pushed into the fractured vertebra after the balloon expansion. The minimally invasive internal fixation stabilization system was supplied by Zhejiang Kehui Company of China; the PKP system and bone cement were the same as that of the PKP group.
Postoperative management was the same in both groups. The use of a brace was not required and all patients were encouraged to stand and walk when they could tolerate the pain and when their general condition and neurologic status permitted.
Clinical data including operative time, blood loss, volume of bone cement injected, leakage of bone cement, time from surgery to ambulation and length of hospital stay were recorded for each group. Any perioperative medical or surgical complications that might need specific intervention or treatment were noted.
All patients were evaluated at 1, 3 and 6 months after surgery and semi-annually thereafter. Functional outcomes were assessed by two independent observers using a visual analog scale (VAS) for pain and the Oswestry Disability Index (ODI) questionnaire. All radiographs and CT scans were evaluated. The local kyphosis angle (Cobb angle, formed by the inferior end plate of the intact vertebra cephalad to the fracture and the superior end plate of the intact vertebra caudad to the fracture) was measured on lateral plain radiographs of the standing position using the Cobb method, to determine loss or persistence of kyphosis correction [11]. CT-scan is used to evaluate bone cement leakage, internal fixation loosening, and vertebral refracture. Any refracture of the injured vertebra, adjacent vertebral fracture or loosening of the internal fixation was recorded.
Statistical analysis
We used SPSS statistical software (version 15.0; SPSS, Inc., USA) for all analyses of continuous variables, which were recorded as the mean and standard deviation. The two groups were compared using the paired t test or Wilcoxon rank-sum test, with the level of significance set at P < 0.05. For sex and vertebral fracture type, we used the Chi-square test with an R × C table.
Results
There were no differences between the two groups with regard to time from surgery to walking and duration of hospitalization (P > 0.05). Amount of bone cement injected of PIF–PKP group was more than that of PKP group (P < 0.05), but these amounts could be accepted by all elderly patients. Operative time and perioperative blood loss differed significantly between the two groups (P < 0.05), but both parameters were within the range of the operative tolerance of elderly patients. Bone cement leakage was observed during the procedure in 14 cases—10 in the PKP group and 4 in the PIF–PKP group—but all leaks were from the side of the vertebra, with no leakage into the spinal canal and no need for specific treatment (Table 2).
No nerve damage occurred in either group postoperatively and no major complications or wound infections were noted perioperatively. One patient in the PKP group suffered an acute exacerbation of chronic bronchitis postoperatively, but improved and was discharged after antibiotic therapy.
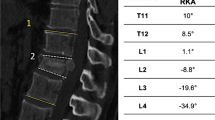
There was no difference between the two groups with regard to preoperative Cobb angle (P > 0.05). However, the PIF–PKP group had better clinical outcomes than the PKP group in terms of both postoperative Cobb angle of kyphosis correction and the persistence of the corrected angle (P < 0.05). Typical patient images were displayed in Figs. 2, 3. Statistical results are shown in Fig. 4.
Preoperative magnetic resonance image and postoperative radiograph of typical cases treated with simple percutaneous kyphoplasty (PKP). a1 Case 1, female, 66 years, T12 burst fracture, fall from a height, b1 at postoperative 1 week, c1 at postoperative 35 months, a2 Case 2, female, 65 years, T12 burst fracture, traffic accident injury, b2 at postoperative 1 week, c2 at postoperative 28 months
Preoperative magnetic resonance image and postoperative CT image of typical cases treated with percutaneous internal fixation with PKP. a3 Case 3, female, 68 years, T12 burst fracture, motor-bicycle accident, b3 at postoperative 1 week, c3 at postoperative 31 months, a4 Case 4, female, 70 years, L2 burst fracture, fall from a height, b4 at postoperative 1 week, c4 at postoperative 25 months
There was no difference between the two groups with regard to preoperative VAS score for low back pain (P > 0.05), but postoperatively and at each follow-up assessment their VAS scores differed significantly (P < 0.05). The two groups’ ODI results in pre-injury were no difference (P > 0.05), but the two groups’ ODI results at postoperatively were significant different (P < 0.05). Postoperative pain (VAS) and functional (ODI) results are shown in Figs. 5, 6.
During the follow-up period, two patients in the PKP group suffered refractures in the injured vertebra (X-ray images prompted that the injured vertebra occurred a compression change again, and the patients felt significantly lower back pain) and one patient had a fracture in the adjacent vertebra; no further fractures occurred in the PIF–PKP group. There were no instances of hardware failure such as implant dislodgment or screw loosening, bending or breakage in the PIF–PKP group, and no patient required a revision procedure or surgery to remove their internal fixation device.
Discussion
The present randomized controlled trial with over 2 years’ follow-up found that, for the treatment of thoracolumbar burst fracture in elderly patients, percutaneous internal fixation with PKP had significant advantages over simple PKP in terms of postoperative lumbar back pain relief and rapid recovery of motor function. The procedure involved two minimally invasive techniques, an operative time of about 1.5 h, blood loss within 100 ml and no increase in postoperative complications. This clinical trial demonstrates that percutaneous internal fixation combined with PKP is effective and safe for the treatment of the elderly patients.
Percutaneous kyphoplasty is one of the currently used methods for the surgical treatment of elderly patients with thoracolumbar burst fractures in spite of the cement leakage and other disputes [12–14]. It theoretically corrects kyphotic deformities, but in practice corrects kyphosis by postural reduction [15, 16] and does not provide a strong correctional force during the procedure. Therefore, patients treated with PKP might be prone to residual kyphosis after surgery. The lack of kyphosis correction may lead to the spinal load force line moving forward and may result in the stress concentration in the anterior column of the fractured vertebra or the adjacent vertebral body. This is the main reason for postoperative lumbar back pain in elderly patients treated for thoracolumbar fractures and is an important cause of refracture of the injured vertebra or adjacent vertebral fracture [17]. However, percutaneous internal fixation combined with PKP can not only effectively correct the kyphotic deformity by way of internal fixation reduction, but also instantly strengthens the anterior and middle spinal columns by the solidification of bone cement in the vertebral body. This excellent reduction and strong support aids rapid postoperative rehabilitation in elderly patients, as has been confirmed by biomechanical studies [18, 19].
Bone cement leakage is a common complication of PKP in elderly patients. Bone cement that permeates into the spinal canal can easily injure the spinal cord, and such damage is more prone to aggravated in thoracolumbar burst fractures involving posterior vertebral wall rupture. In the present study, fractured vertebra exhibited an “eggshell” like change after reduction by the internal fixation device, which created a negative pressure space in the vertebral body. Under these conditions, injection of thicker, more dough-like bone cement became possible and leakage was significantly reduced. Therefore, in surgery of percutaneous internal fixation with PKP, the entire process of fractured vertebral strengthening became more safe and effective.
Vertebral pedicle screws implanted into the spine of elderly patients with thoracolumbar fractures are prone to loosening, which is a relatively common complication. In the present study, however, during the follow-up period of over 2 years, none of the patients in the treatment group exhibited loosening or shifting of their internal fixation device, which differs from previous reports [5–7]. The main reason for this difference may be that the anterior and middle spinal columns of our patients were immediately strengthened by the use of bone cement early after the reduction by internal fixation. Another reason may be related to bone density, because the degree of osteoporosis in our patients was not severe. If, over a longer period of follow-up, loosening of internal fixation occurs, the internal fixators should be removed. Meanwhile, we think that an elderly patient with very severe osteoporosis may need long segmental fixation, or the screw fixation augmented with PMMA to avoid internal fixators loosening.
Percutaneous internal fixation with PKP was initially applied in young and middle-aged patients with thoracolumbar burst fractures [8–10]. However, we believe that it is especially suitable for many elderly patients. Because the procedure is minimally invasive and promotes a rapid return to the activities of daily living, it may avoid the many complications suffered by elderly patients who remain in bed for a long period of time. However, percutaneous internal fixation with PKP is not always suitable for all elderly thoracolumbar burst fracture patients. Elderly patients who might need this procedure should undergo a detailed preoperative assessment to clarify their tolerance for surgery, to ensure operative safety.
Conclusions
Compared with simple PKP, percutaneous short-segment pedicle screw internal fixation with PKP is more suitable for the treatment of elderly patients with thoracolumbar burst fractures. The advantages include greater strength of the fractured vertebral body, effective maintenance of kyphosis angle correction, rapid relief of lumbar back pain and promotion of early rehabilitation and ambulation. We recommend percutaneous internal fixation with PKP for the treatment of thoracolumbar burst fractures in selected elderly patients.
References
Baumann C, Fuchs H, Kiwit J et al (2007) Complications in percutaneous vertebroplasty associated with puncture or cement leakage. Cardiovasc Intervent Radiol 30(2):161–168
Patel AA, Vaccaro AR, Martyak GG et al (2007) Neurologic deficit following percutaneous vertebral stabilization. Spine 32(16):1728–1734
Rho YJ, Choe WJ, Chun YI (2012) Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J 21(5):905–911
Lin WC, Lee YC, Lee CH et al (2008) Refractures in cemented vertebrae after percutaneous vertebroplasty: a retrospective analysis. Eur Spine J 17(4):592–599
Knop C, Fabian HF, Bastian L et al (2001) Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine 26(1):88–99
Sudo H, Ito M, Abumi K et al (2010) One-stage posterior instrumentation surgery for the treatment of osteoporotic vertebral collapse with neurological deficits. Eur Spine J 19(6):907–915
Ito M, Harada A, Nakano T et al (2010) Retrospective multicenter study of surgical treatments for osteoporotic vertebral fractures. J Orthop Sci 15(3):289–293
Marco RA, Meyer BC, Kushwaha VP (2010) Thoracolumbar burst fractures treated with posterior decompression and pedicle screw instrumentation supplemented with balloon-assisted vertebroplasty and calcium phosphate reconstruction. J Bone Joint Surg Am 92(Supplement 1 Part 1): 67–76
Fuentes S, Blondel B, Metellus P et al (2010) Percutaneous kyphoplasty and pedicle screw fixation for the management of thoraco-lumbar burst fractures. Eur Spine J 19(8):1281–1287
Bironneau A, Bouquet C, Millet-Barbe B et al (2011) Percutaneous internal fixation combined with kyphoplasty for neurologically intact thoracolumbar fractures: a prospective cohort study of 24 patients with one year of follow-up. Orthop Traumatol Surg Res 97(4):389–395
He D, Wu L, Chi Y, Zhong S (2011) Facet joint plus interspinous process graft fusion to prevent postoperative late correction loss in thoracolumbar fractures with disc damage: finite element analysis and small clinical trials. Clin Biomech 26(3):229–237
Carbognin G, Sandri A, Girardi V et al (2009) Treatment of type-A3 amyelic thoracolumbar fractures (burst fractures) with kyphoplasty: initial experience. Radio Med 114(1):133–140
Hartmann F, Gercek E, Leiner L, Rommens PM (2012) Kyphoplasty as an alternative treatment of traumatic thoracolumbar burst fractures magerl type A3. Injury 43(4):409–415
Gan M, Yang H, Zhou F et al (2010) Kyphoplasty for the treatment of painful osteoporotic thoracolumbar burst fractures. Orthopedics 33(2):88–92
Chin DK, Kim YS, Cho YE, Shin JJ (2006) Efficacy of postural reduction osteoporotic vertebral compression fractures followed by percutaneous vertebroplasty. Neurosurgery 58(4):695–700
Shin JJ, Chin DK, Yoon YS (2009) Percutaneous vertebroplasty for the treatment of osteoporotic burst fractures. Acta Neurochir 151(2):141–148
Gaitanis IN, Carandang G, Phillips FM et al (2005) Restoring geometric and loading alignment of the thoracic spine with a vertebral compression fracture: effects of balloon (bone tamp) inflation and spinal extension. Spine J 5(1):45–54
Mermelstein LE, McLain RF, Yerby SA (1998) Reinforcement of thoracolumbar burst fractures with calcium phosphate cement: a biomechanical study. Spine 23(6):664–670
Zhang L, Yang G, Wu L, Yu B (2010) The biomechanical effects of osteoporosis vertebral augmentation with cancellous bone granules or bone cement on treated and adjacent non-treated vertebral bodies: a finite element evaluation. Clin Biomech 25(2):166–172
Acknowledgments
This project is supported by the National Natural Science Foundation of China (30970702, 81271663), Zhejiang Science and Technology program foundation of China (2011C33026), and Zhejiang Wenzhou Medical College Scientific Development Foundation of China (QTJ06012).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
He, D., Wu, L., Sheng, X. et al. Internal fixation with percutaneous kyphoplasty compared with simple percutaneous kyphoplasty for thoracolumbar burst fractures in elderly patients: a prospective randomized controlled trial. Eur Spine J 22, 2256–2263 (2013). https://doi.org/10.1007/s00586-013-2972-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2972-5