Abstract
Purpose
To demonstrate the reality of a transverse plane pattern independent of the scoliotic curve location and to show the importance of the transverse plane pattern in the assessment of the progression risk in a population of mild scoliosis.
Methods
Spines of 111 patients with adolescent idiopathic mild scoliosis were reconstructed using biplanar stereoradiography. The apical axial rotation, the intervertebral axial rotation at junctions and the torsion index were computed. Mean values of each parameter were compared between thoracic, thoracolumbar and lumbar curves. Then a cluster analysis was performed using these parameters on 78 patients with effective outcomes at skeletal maturity. The effective outcomes and the results reached with the statistical analysis were compared and analyzed (ROC and logistic regression).
Results
No statistical difference was observed when considering each parameter between the different types of curves. Two clusters independent of the curve type were identified. The mean values of transverse plane parameters were significantly higher in Cluster 1 than in Cluster 2. 91 % of patients classified in Cluster 1 had progressive curve and 73 % of patients classified in Cluster 2 remained stable at skeletal maturity. All parameters were good predictors but the best was the torsion index.
Conclusions
This study demonstrated that a transverse plane pattern combining apical axial rotation, the intervertebral axial rotation at junctions and the torsion index is independent of the scoliotic curve location and significant in the determination of the progression risk of mild scoliosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The challenge in the management of mild scoliosis is to evaluate the progression risk. The Cobb angle is still the major parameter of severity, combined with the clinical aspects of skeletal and sexual maturation, that allow a prognosis [1, 2]. Identification of different scoliotic curve shape patterns could be a step for a better understanding of pathomechanisms, genesis and evolution of adolescent idiopathic scoliosis (AIS).
AIS described as a 3D deformity of the spine and transverse plane analysis are two concepts initiated by Perdriolle [3]. The Perdiolle’s “torsiometer” is still the most accurate method of measurement of axial vertebral rotation on 2D A-P radiographs [4]. Then, MRI and CT have improved accuracy of vertebral rotations measurements but their clinical relevance is limited by the supine position of the patient and radiation exposition for CT [5]. In the past decade, the development of stereoradiography and semi-automated 3D reconstructions of the spine, has provided measurements of transverse plane parameters in standing position which have generated novel 3D classifications of AIS [4, 6–8]. However, these novel classifications have not yet modified the management of patient with mild AIS.
Transverse plane parameters like axial vertebral rotation, intervertebral rotations at upper and lower junctions [3], and torsion index [9] are associated with the description of severe AIS. The hypothesis developed in our institution is that a scoliotic 3D pattern, independent of the location of the curve, based on the combination of these parameters, could be a sign of high risk of progression. The determination of such 3D pattern at an early stage of development of AIS could improve the management of mild scoliosis.
The aim of this study is, first, to demonstrate the reality of a transverse plane pattern independent of the scoliotic curve location, and second, to show the importance of the transverse plane pattern in the assessment of the progression risk in a population of mild scoliosis.
Methods
Patients
Spines of 111 patients with adolescent idiopathic scoliosis were reconstructed using the EOS System (EOS-Imaging).
EOS* (EOS-Imaging) is a low-dose imaging system providing simultaneous AP and lateral views in a stand-up position [10–12]. Semiautomatic 3D reconstruction, using SterEOS software [12, 13] (EOS-Imaging), is based on identifiable anatomic points. It provides a 3D image of the spine deformity giving measurements of vertebral and intervertebral axial rotations in a stand-up position. The spine 3D geometry is limited between T1 and S1 since cervical spine is not routinely captured. Validation of the accuracy and reproducibility of the 3D reconstruction method has been reported in previous studies [13–15] particularly the reliability of 3D reconstruction of the spine of mild scoliotic patients [16]: the 95 % prediction limits for the intra- and inter-observer errors in measurement were computed. 95 % prediction limits indicate the difference between two successive replicate measurements that would exceed approximately 5 % of the time due to an error of measurement. Inter-observer 95 % prediction for Cobb angle was 2.8° and 2° for IAR and AVR. Intra-observer 95 % predication for Cobb angle was 2°, 1.8° for AVR and 0.8° for IAR.
Only patients with mild scoliosis were selected. There were 78 girls and 33 boys. The mean age at the radiological examination was 11 (range 8–14). Ninety-one were classified Risser 0 or 1 at the radiological examination, 7 were Risser 2, 8 were Risser 3, and 5 were Risser 4. Inclusion criteria were a Cobb angle larger than 4° and lower than 25° by automatic measurement. The mean Cobb angle was 14 (5) degrees.
There were 57 thoracic (Apex between T1 and T11), 25 thoracolumbar (Apex between T12 and L1), and 29 lumbar (Apex between L2 and L5) curves.
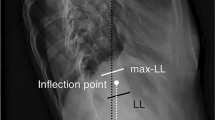
3D shape parameters were automatically calculated using SterEOS software [12, 13] (EOS-Imaging). Four 3D parameters were defined (Fig. 1):
Illustration of the four transverse plane parameters. The axial apical vertebral rotation (AVR) corresponds to the rotation of the axial apical vertebra in the reference coordinate system (EOS system). The intervertebral axial rotations correspond to the angle of axial rotation between the end vertebrae of the curve and the adjacent vertebrae at lower and upper junctions. The torsion index is the mean of the two sums of intervertebral axial rotations from lower junction to the apex, then from the apex to the upper junction
-
1.
Apical axial rotation (AVR).
-
2.
Intervertebral axial rotation at the upper neutral zone (upper IAR) as described by Perdriolle et al. [3].
-
3.
Intervertebral axial rotation at the lower neutral zone (lower IAR) as described by Perdriolle et al. [3].
-
4.
Torsion index: this index, proposed by Steib et al. [9], indicates to what extent vertebrae are continuously rotated with regard to the other from lower neutral vertebra to the apex, and then from the apex to the upper neutral vertebra. The torsion index is the mean of the two sums of intervertebral axial rotations from lower junction to the apex, and then from the apex to the upper junction.
Statistical analysis
The statistical analysis was performed in the SPSS version 12.0,1 for Windows (SPSS inc., Chicago, IL, USA) and a Cluster analysis was performed in Weka version 3.6.2 (Hamilton, NZ) using the K-means Cluster analysis routine [17].
A statistical analysis was performed on the entire population. Mean values of the Cobb angle and each transverse plane parameter were compared using a non-parametric test for k independent samples (Kruskal–Wallis; α = 0.05) thoracic, thoracolumbar and lumbar curves.
Then a k-means Cluster analysis was performed. Only patients with documentation of progression or stability of the curve at skeletal maturity were involved in the Cluster analysis. Seventy-eight out of 111 patients were followed clinically and radiographically until skeletal maturity to document the progression of the scoliosis. There were 56 girls and 22 boys. The mean Cobb angle was 14 (5) degrees. There were 40 thoracic (Apex between T1 and T11), 18 thoracolumbar (Apex between T12 and L1), and 20 lumbar (Apex between L2 and L5) curves.
k-means is a unsupervised learning algorithms that solve clustering problem [17]. The procedure follows a simple way to classify n observations into k Clusters, fixed a priori, in which each observation belongs to the Cluster with the nearest mean. In this work, parameters used in the Cluster analysis were: the AVR, the upper IAR, the lower IAR and the torsion index. The number of Clusters (k) fixed a priori was two.
Then we searched for statistically significant differences between groups. Mean values of each transverse plane parameter were compared using a non-parametric test for two independent samples (Mann–Whitney; α = 0.05).
Follow-up
Seventy-eight out of 111 patients were followed clinically and radiographically until skeletal maturity to document the progression of the scoliosis. The mean follow-up time was 5 years (range 2–8). For each of these patients, the effective outcome of the scoliosis, stable or progression was compared to the group initially assigned to the patient. The inter- and intra-observer reproducibility measurement (95 % precision) of Cobb angle with the EOS system is 2° for mild scoliosis [16]. Therefore, the criterion for progression was an increase in the curve of 5° or more that was confirmed radiographically on two consecutive occasions or the initiation of brace treatment. Subsequently, a ROC analysis and an ascendant step-by-step method of logistic regression analysis (Wald; α = 0.05) including the Cobb angle and all the transverse plane parameters were performed to assess the relative strength of each factor in determining progression potential.
Results
Kruskal–Wallis test
Regarding the entire population, no statistical difference (p ≫ 0.05) was observed between the mean value of the Cobb angle, the upper and lower intervertebral axial rotation and the apical vertebral axial rotation when comparing thoracic with lumbar and thoracolumbar. A significant difference was observed for the torsion index (p = 0.04) between thoracic and lumbar curves. The difference was not significant for this parameter between thoracic and thoracolumbar curves and between lumbar and thoracolumbar curves.
Cluster analysis
The automatic Cluster analysis based on the above-mentioned parameters identified groupings within the entire dataset when it searched for two groups after three iterations. Thirty-three patients (42 %) were classified in a first Cluster and 45 patients (58 %) were classified in second Cluster.
Each of the two groups included thoracic, thoracolumbar and lumbar curves. Seventeen thoracic, 10 thoracolumbar and 6 lumbar curves were assigned to Cluster 1, while 23 thoracic, 8 thoracolumbar and 14 lumbar curves were assigned to Cluster 2.
The mean Cobb angle was 16° (4°) for Cluster 1 and 13° (5°) for Cluster 2 (p = 0.001).
The Mann–Whitney test applied for each parameter between the two groups revealed no statistically significant difference (U = 702; p = 0.68) for the location of the apical vertebra (i.e. type of curve). However, it revealed a significant difference for the other parameters: the torsion index (U = 105; p ≪ 0.001), the upper IAR (U = 302; p ≪ 0.001), the lower IAR (U = 409; p = 0.001), the AVR (U = 129; p ≪ 0.001) and the Cobb angle (U = 454; p = 0.004).
The mean values of each parameter within the two groups are recorded in Fig. 2. The mean value of torsion index was 4° higher in Cluster 1 [7° (2°)] than in Cluster 2 [3° (1°)]. The mean value of upper IAR was 3° higher in Cluster 1 [−4° (2°)] than in Cluster 2 [−1° (3°)] and the mean value of lower IAR was 2° higher in Cluster 1 [3° (3°)] than in Cluster 2 [1° (2°)]. Finally, the value of AVR in Cluster 1 [9° (3°)] was 5° higher than in Cluster 2 [4° (2°)].
Correlation between clustering and progression
Thirty patients out of 33 (91 %) classified in Cluster 1 had a progressive curve or required brace treatment during follow-up. Thirty-three patients out of 45 (73 %) classified in Cluster 2 remained stable at skeletal maturity. In Cluster 1, the mean progression of Cobb angle was 14° (range 1°–37°), 17° (range 8°–37°) for the lumbar curves, 14° (range 2°–30°) for the thoracic and 12° (range 1°–23°) for the thoracolumbar curves. In the Cluster 2, the mean progression of Cobb angle was 6° (range 0°–29°), 5° (range 0°–20°) for the lumbar curves, 6° (range 1°–29°) for the thoracic and 5° (range 0°–17°) for the thoracolumbar curves.
The ROC analysis for each parameter is depicted in Fig. 3. The area under the curve (AUC) gives a measure of the quality of the parameter. The AUC was 0.85 for the torsion index with a 95 % confidence interval of [0.77–0.94], 0.81 [0.72–0.91] for AVR and upper IAR, 0.77 [0.67–0.88] for the lower IAR and 0.74 [0.63–0.85] for the Cobb angle. For each parameter, threshold values have been searched for optimized sensibility and specificity. For the torsion index, a threshold of 3.7 gives a sensibility of 81 % and a specificity of 81 %. For the lower IAR, a threshold of 2.2° gives a sensibility of 70 % and a specificity of 78 %. For the upper IAR, a threshold of −6° gives a sensibility of 90 % and a specificity of 95 %. For the AVR, a threshold of 5.8° gives a sensibility of 70 % and a specificity of 70 %.
In the logistic regression analysis, all transverse plane parameters improved the model but the ascendant step-by-step procedure stopped before including the Cobb angle. Odds ratios were, respectively, 1.43 (p = 0.05) for the torsion index, 1.39 (p = 0.006) for the AVR, 1.35 (p = 0.04) for the lower IAR and 0.7 (p = 0.03) for the upper IAR. The correlation coefficients computed between all parameters were low, meaning that each parameter was associated individually to progression of the curve.
Discussion
The aim of this study was, first, to demonstrate the reality of a transverse plane pattern independent of the scoliotic curve location, and second, to show the importance of the transverse plane pattern in the assessment of the progression risk in a population of mild scoliosis.
The standard statistical analysis among the entire population of 111 patients with mild scoliosis showed only a slight significant difference of the torsion index between thoracic and lumbar curves (p = 0.04). But no statistical difference was observed between the other transverse plane parameters and Cobb angle when comparing thoracic, thoracolumbar or lumbar curves two by two. The difference of the torsion index between thoracic and lumbar curves could be either explained by the higher, but not significant, Cobb angle in the thoracic sample or an effective higher structural torsion index in thoracic curves. Thoracic curves are indeed known to be more at risk of progression than other curves [18]. However, the Cluster analysis based upon transverse parameters did not discriminate the curve location. The number of thoracic, thoracolumbar and lumbar curves was indeed equivalent in both Clusters and the mean apex location was not significantly different between the two Clusters. There is in fact no evidence in the literature of a different origin of the vertebral deformity considering the location. The growth disturbance of some vertebrae which leads to the global scoliotic deformity is in our opinion similar within the entire spine. The current study demonstrates, that a transverse plane pattern, resulting in the combination of the AVR, lower and upper IAR and torsion index, is independent of the curve location.
The Cluster analysis identified two subgroups of 33 and 45 patients, among a population of 78 with mild scoliosis (range of Cobb angle 4°–25°). The statistical analysis showed that the magnitude of the values the transverse plane parameters and Cobb angle in the Cluster 1 was significantly higher than in Cluster 2. The relationship between AVR and Cobb angle in severe scoliosis has been previously documented [7, 19]. The transverse plane parameters are not strictly independent of the Cobb angle. Thus, the significant difference between the transverse plane values in the two Clusters may be partially explained by the higher significant Cobb angle in Cluster 1 [16° (4°)] than in Cluster 2 [13° (5°)]. However, the values of transverse parameters of patients with similar Cobb angle pertaining to the different Clusters were in many cases discordant. An example, with two patients with a Cobb angle of 10° and similar apical vertebra is depicted in Figs. 4 and 5. Despite the small Cobb angle, the magnitude of the transverse plane parameters is significantly higher for the patient assigned to Cluster 1 than for the patient assigned to Cluster 2. These findings support that the transverse plane parameters seem to play an independent role, besides the Cobb angle, in the characterisation of the severity of mild scoliotic curves.
Upper and anteroposterior views of 3D reconstructions of the spine of two patients with the same Cobb angle (10°) and same type of curve [same apex (L1)] picked in each Cluster. Note the difference in the magnitude of torsion index and apical axial rotation of patient on the left (respectively 1° and 2°) and the patient on the right (respectively 5° and 8°)
Transverse parameters values corresponding to the two curves showed in Fig. 4
The final outcome at skeletal maturity showed a 91 % correlation between Cluster 1 and progression of the curve and 73 % of correspondence between Cluster 2 and stable curves. In addition, transverse plane parameters values were higher in the cluster 1 that in the cluster 2. The effective progression analysis seems to corroborate the importance of the transverse plane parameters and the Cobb angle in the curve progression risk. Moreover, the ROC and the logistic regression analysis showed that all transverse plane parameters individually were good predictors of progression. The best predictor was the torsion index followed by AVR and IAR. In contrast, the Cobb angle was automatically excluded of the step-by-step logistic regression analysis and the AUC of the Cobb angle was worse than all transverse plane parameters. If a higher torsion index is indeed a significant structural characteristic of thoracic curves and the best predictor of progression, this result could explain why thoracic curves are classically more at risk of progression than the other curves. Interestingly, the Cobb angle is not as good as the transverse plane parameters in the assessment of the progression risk of mild scoliosis. These results emphasize the interest of the transverse plane parameters individually and the interest grouping all the parameters values under the concept of a transverse plane pattern, associated to the Cobb angle, to improve the prediction of scoliosis progression.
Conclusion
This study demonstrated the reality of a transverse plane pattern, resulting in the combination of the AVR, lower and upper IAR and the torsion index, independent of the scoliotic curve location. It also stressed the importance of the transverse plane pattern in the determination of the progression risk of mild scoliosis. With the constant expansion of 3D imaging technologies of the spine in a standing position, the transverse plane pattern could be soon routinely added to the Cobb angle and skeletal and sexual maturity indices to improve the prediction of scoliotic curve progression.
References
Duval-Beaupere G (1996) Threshold values for supine and standing Cobb angles and rib hump measurements: prognostic factors for scoliosis. Eur Spine J 5:79–84
Duval-Beaupere G, Lamireau T (1985) Scoliosis at less than 30 degrees. Properties of the evolutivity (risk of progression). Spine (Phila Pa 1976) 10:421–424
Perdriolle R, Vidal J (1981) A study of scoliotic curve. The importance of extension and vertebral rotation (author’s transl). Rev Chir Orthop Reparatrice Appar Mot 67:25–34
Vrtovec T, Pernus F, Likar B (2009) A review of methods for quantitative evaluation of axial vertebral rotation. Eur Spine J 18:1079–1090
Vrtovec T, Pernus F, Likar B (2010) Determination of axial vertebral rotation in MR images: comparison of four manual and a computerized method. Eur Spine J 19:774–781
Stokes IA, Sangole AP, Aubin CE (2009) Classification of scoliosis deformity three-dimensional spinal shape by cluster analysis. Spine (Phila Pa 1976) 34:584–590
Sangole AP, Aubin CE, Labelle H, Stokes IA, Lenke LG, Jackson R, Newton P (2009) Three-dimensional classification of thoracic scoliotic curves. Spine (Phila Pa 1976) 34:91–99
Duong L, Cheriet F, Labelle H (2006) Three-dimensional classification of spinal deformities using fuzzy clustering. Spine (Phila Pa 1976) 31:923–930
Steib JP, Dumas R, Mitton D, Skalli W (2004) Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine (Phila Pa 1976) 29:193–199
Kalifa G, Charpak Y, Maccia C, Fery-Lemonnier E, Bloch J, Boussard JM, Attal M, Dubousset J, Adamsbaum C (1998) Evaluation of a new low-dose digital x-ray device: first dosimetric and clinical results in children. Pediatr Radiol 28:557–561
Dubousset J, Charpak G, Dorion I, Skalli W, Lavaste F, Deguise J, Kalifa G, Ferey S (2005) A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med 189:287–297; discussion 297–300
Dubousset J, Charpak G, Skalli W, Kalifa G, Lazennec JY (2007) EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose. Rev Chir Orthop Reparatrice Appar Mot 93:141–143
Humbert L, De Guise JA, Aubert B, Godbout B, Skalli W (2009) 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys 31:681–687
Humbert L, Carlioz H, Baudoin A, Skalli W, Mitton D (2008) 3D Evaluation of the acetabular coverage assessed by biplanar X-rays or single anteroposterior X-ray compared with CT-scan. Comput Methods Biomech Biomed Eng 11:257–262
Pomero V, Mitton D, Laporte S, de Guise JA, Skalli W (2004) Fast accurate stereoradiographic 3D-reconstruction of the spine using a combined geometric and statistic model. Clin Biomech (Bristol, Avon) 19:240–247
Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W (2007) Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine (Phila Pa 1976) 32:568–573
MacQueen J (1967) Some methods for classification and analysis of multivariate observations. In: Proceedings of 5th Berkeley Symposium on Mathematical Statistics and Probability, vol 1, pp 281–297
Peterson LE, Nachemson AL (1995) Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity. Logistic regression analysis based on data from The Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am 77:823–827
Duong L, Mac-Thiong JM, Cheriet F, Labelle H (2009) Three-dimensional subclassification of Lenke type 1 scoliotic curves. J Spinal Disord Tech 22:135–143
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Courvoisier, A., Drevelle, X., Dubousset, J. et al. Transverse plane 3D analysis of mild scoliosis. Eur Spine J 22, 2427–2432 (2013). https://doi.org/10.1007/s00586-013-2862-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2862-x