Abstract
Purpose
There exist not much data regarding the surgical treatment of pure congenital kyphosis (CK) in the literature. The purpose of this study was to evaluate the results of closing wedge osteotomy with posterior instrumented fusion in patients with congenital kyphotic deformity.
Methods
We retrospectively evaluated the radiographical results of 10 patients who were subject to closing wedge vertebral osteotomy and posterior instrumented fusion due to CK. The mean age of the patients at surgery was 12.6 ± 3.72 years (range 8–18 years). Radiographical measurements including local kyphosis, correction loss, global kyphosis and sagittal balance values were noted for the preoperative, postoperative and final follow up periods, respectively. The data obtained from those periods underwent statistical analysis.
Results
Average follow-up period was 51.8 ± 29.32 months (range 26–96 months). The mean local kyphosis angle was 67.7° ± 15.64° (range 42°–88°) prior to the surgery, 31.5° ± 17.12 (range 14°–73°) following the surgery and 31.9° ± 15.98° (range 14°–71°) during the follow up-period, respectively (p < 0.05). A correction rate of 53.5 % was reported at the final follow up. Average sagittal balance was measured as 33.1 ± 24.48 mm (range 2–77 mm) prior to the surgery, 20.8 ± 15.46 mm (range 5–46 mm) following the surgery (p < 0.05) and 14.1 ± 9.2 mm (range 0–30 mm) during follow-up period (p > 0.05). Complications consisted of a rod fracture due to pseudoarthrosis, an implant failure with loosening of screws and a proximal junctional kyphosis. No neurological deficit or deep infection were encountered in any of the patients in the study group.
Conclusion
Closing wedge osteotomy with posterior instrumented fusion is an efficient method of surgical treatment in terms of sagittal balance restoration and deformity correction in patients with congenital kyphosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital kyphosis (CK) is caused by a mismatch during the final stages of ossification and cartilage formation in embryological development [1]. Ongoing growth in the posterior elements of the spine when there is a formation and/or segmentation failure in anterior structures of the spinal column may cause progressive segmental kyphosis resulting in sagittal imbalance [1]. Although the exact mechanism of these deformities is not well understood, studies on animals suggest that the defect is mainly related to a vascularization disorder [2]. Neural arch anomalies are not part of this deformity pattern since the anomalies in the central zone occur during the final stages of cartilage formation [3]. Additionally, one should not underestimate the renal and cardiac anomalies that may accompany with the aforementioned deformity since the renal and cardiac formations occur at this stage as well.
Congenital kyphosis is classified by McMaster and Singh as: a defect of formation in the anterior spinal column (type 1), segmentation failure (type II) and combined formation with segmentation failure (type III) [1, 4]. Type I, with a kyphotic deformity localized in thoracic or thoracolumbar region is the most common type, which has a rapid progression and high risk of spinal cord compression resulting in paraplegia if not treated. Cardiopulmonary dysfunction may also develop in case of progressive deformity [4]. Type II has a low risk of neurological deterioration. It is usually progressive but, without causing extreme deformities. Cranial lumbar region or thoracolumbar junction area are frequently involved. The size of the deformity and the number of segments involved in type II does not correlate with each other all the time [1]. Type III deformities are usually seen at T10–L-1 segments and may progress faster than type II deformities irrespective of the localization on the spinal column [1, 5].
Bracing is not effective as treatment in CK [4, 6, 7]. Surgery is usually required for the treatment of deformities [4, 8–10]. Factors such as age, type, size of deformity and existence of neurological deficit due to spinal cord compression play an important role in the management of CK [11]. There is little evidence in the literature regarding the surgical treatment of CK to avoid deformity progression and the relevance of this for the sagittal balance of the spine. The purpose of this retrospective study was to evaluate the radiographical results of closing wedge osteotomy followed by posterior instrumented fusion at the apex of the deformity in congenital kyphosis.
Materials and methods
Ten consecutive patients with isolated CK treated by closing wedge vertebral osteotomy followed by posterior instrumented fusion in two different clinics from 2004 to 2009 were included in the study. Five of the patients were male. Seven patients had type I, one type II and two had type III deformity. Vertebral levels involved are listed in Table 1. The average age of the patients at the index operation was 12.6 ± 3.72 years (range 8–18 years). Five patients were skeletally immature according to the definition of skeletal maturation as closure of acetabular cartilage complex and complete ossification or fusion of pelvic apophysis on radiograms (Table 1). Preoperative radiological assessment of the patients was performed using anteroposterior and lateral standing digital full-spine X-rays, computerized tomography (CT) and magnetic resonance imaging (MRI). Echocardiography and abdominal ultrasonography were performed in all patients. Neurological examination of all patients prior to surgery was within normal limits. No intraspinal pathologies including spinal cord edema in MRI was encountered in any of the patients. Only one patient was operated on due to a cardiac pathology.
Surgical decision making was based on the factors consisting of age, type of the kyphotic deformity, local kyphosis angle and the sagittal imbalance of the spine.
All patients were examined and followed in the two involved clinics. Fusion mass, implant failure and correction loss of the patients were assessed by both clinics in collaboration with each other. Radiographical measurements and complications were recorded prior to operation, following the operation and during the follow-up period in a standard fashion.
Radiographic measurements were performed twice by two different specialists using the same reference points on the radiographical images. Local kyphosis, global kyphosis and lumbar lordosis angles were measured using digital lateral standing X-rays via Cobb method prior to operation, following the operation and at the end of follow up. Sagittal balance on digital lateral standing X-rays was measured by drawing a straight line from the center of C7 to the posterosuperior corner of the S1 vertebra body (Table 2).
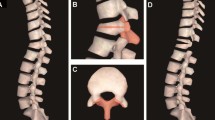
General anesthesia in prone position on a radiolucent modular operating table in the operating rooms was used for all patients. Double-sided polyaxial screws were inserted via free-hand technique in the pedicles between the levels that were planned to be fused. The osteotomy side was secured via a temporary rod, which was introduced into the screws on one side (Fig. 1). Wedge-shaped vertebral osteotomy was performed by resecting both facet joints, pedicles, laminae and transverse process together with posterior part of the vertebral body in the apical region of kyphotic deformity (Fig. 2). Segmental nerve roots were explored and protected in the osteotomy region. Costotransversectomy was applied to both sides during thoracic region osteotomies. Access to vertebra was gained through both pedicle locations after removal of posterior elements. Posterior and lateral walls of the vertebra were weakened using angled curette after removal of posterior longitudinal ligament and a wedge-shaped cavity was created using osteotomes. Attempts were made to preserve anterior longitudinal ligament. Two previously bended titanium rods were fixed to the screws afterward and osteotomy line was gently closed through an extension maneuver via application of sequential compression on both rods with an in situ bending force and the screws were locked after correction. The lower and upper part of the adjacent cephalad and caudad laminae were resected to avoid cord impingement during correction. Fusion through short segment instrumentation was performed in five patients and long segment instrumentation was performed in remaining five patients. Pedicles and laminae of all patients in instrumentation level were decorticated using osteotomes. Autografts derived from posterior elements, costa and vertebral body together with allografts were used for arthrodesis. At the time interval which the current study was conducted, we were unable to use spinal cord monitoring due to financial issues. So, we were able to evaluate the motor functions of the patients only after the wound closure and transferring the patient in the supine position while still intubated, which may be defined as a post operative wake up test. No braces were used in any patients after the operations. Patients were initially engaged in a supervised rehabilitation program in the departments.
For statistical analysis of the radiographic measurements, we used SPSS 11.5 (Lead Technologies, Inc., Chicago, IL, USA). Wilcoxon-signed ranks test was used for the comparison of thoracic kyphosis, sagittal balance, lumbar lordosis and deformity correction. p values <0.05 were accepted as significant.
Results
Average follow up was 51.8 ± 29.32 months (range 26–96 months). The mean operation time was 240 ± 48.07 min (range 180–320 min). Average blood loss was 1,070 ± 427 ml (range 600–1,800 ml) (Table 1).
The mean global kyphosis angle was measured as 69.8° ± 10.46° (range 56°–85°) prior to the surgery, 47.1° ± 10.84° (range 33°–70°) following the surgery (p < 0.05) and 57.1° ± 18.84° (range 38°–88°) during the final follow up (p > 0.05) (Table 2).
The mean lordosis was measured as −71.9° ± 9.9° (range −90°–56°) prior to the surgery, −61.2° ± 8.87° (range −72°–42°) following the surgery (p < 0.05) and −59.5° ± 7.77° (range −77°–51°) during the final follow up (p > 0.05) (Table 2). Average local kyphosis angle was 67.7° ± 15.64° (range 42°–88°) prior to the surgery, 31.5° ± 17.12° (range 14°–73°) following the surgery (p < 0.05) and 31.9° ± 15.98° (range 14°–71°) during the final follow up (p > 0.05) (Table 2). The deformity correction rate was 53.5 % (35.8°) in terms of local kyphosis angle after surgery and 0.6 % (≅1°) correction loss was observed at the final follow up.
The mean sagittal balance value was measured as 33.1 ± 24.48 mm (range 2–77 mm) prior to the surgery, 20.8 ± 15.46 mm (range 5–46 mm) following the surgery (p < 0.05) and 14.1 ± 9.2 mm (range 0–30 mm) during the follow-up period (p > 0.05) (Table 2).
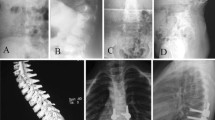
Three patients (30 %) had major complications (Table 3). The first patient with pseudoarthrosis had a bilateral rod fracture 2 years after the surgery. Rods were replaced and they were supported with two additional rods laterally. The pseudoarthrosis region was debrided and decorticated. It was grafted with cancellous allograft chips and demineralized bone matrix resulting in pain-free solid fusion after 6 months (Figs. 3, 4, 5). The second patient had an implant failure due to loosening of screw/rod connection 3 months after the initial procedure. The instrumentation level of the patient was between T4 and L2. The fusion was extended to L4 distally and cap screws were replaced. The last patient had junctional kyphosis without clinical complaints so no intervention took place. There was no neurological deficit or deep infection in any of the patients. No patients were lost to follow up.
Discussion
There is not much data regarding the surgical treatment of isolated congenital kyphosis via closing wedge osteotomy in the literature. We evaluated the radiographical results of 10 patients with CK treated by a closing wedge osteotomy with instrumented posterior fusion in this retrospective study.
The main objective when planning a surgical intervention for a spinal deformity is to provide a better sagittal balance without causing neurological deficit. Method of surgery depends on the factors such as age of the patient, size of the deformity and existence of a spinal cord compression [1]. Neurological deficit related to anterior cord compression may develop due to the progression of deformity in CK. Early interference with the deformity may result in extensive corrections [11].
Use of braces for the treatment of patients suffering progressive CK seems not to be effective [12]. Mayfield et al. [12] argued that the use of braces neither prevented the progression of deformity nor was successful in the final treatment of CK. They also added that the extreme back pain due to hyperlordosis and the cosmetic deformity were other problems encountered in CK [12].
In CK, there exists a deformity in sagittal plane due to abnormal posterior angulation of the vertebral segment. Immediate operation is required for patients with type 1 deformity since the progression of the disease will not only result in sagittal imbalance, but also may cause neurological deterioration. Spontaneous spastic paraparesia was seen in 10 % in the series of McMaster and Singh [1] and 7 of the 11 patients were type 1 cases. It was indicated that anomaly was localized in central or distal thoracic region in nine patients. Average kyphosis of those patients was measured as 111° [1]. In the study of Winter et al. [4], paraparesia was seen in 12 % of the patients and it was reported that all of those patients suffered type 1 CK. The anomaly in majority of those patients was located in the proximal thoracic region [4]. According to Kim et al. [13], paralysis was seen in 2 (over 100°) of 14 patients who were operated for kypotic deformity. They concluded that patients younger than age of 3 did not have any kind of neurological deficit. They suggested that patients with CK should be operated at early stages when their deformity was <60°. They listed risk factors such as late correction, combined anterior and posterior antrodesis, extreme deformities and previous cord compressions as reasons for neurological deterioration [13]. Operation during early stages would have been of use to avoid complications due to surgery [5]. In the current report, no neurological impairment was seen in any of our patients and local kyphosis angles of all our patients were <90°.
Unsegmented bar is located symmetrically or in anterolaterally in type 2 CK. Although symmetric bar results in pure kyphosis, this may progress slowly. Kyphoscoliosis develops in the cases with anterolateral bar and this is associated with poor prognosis. Probability of a neurological complication is not high. These patients may be operated if advanced deformity is evident. If deformity is not severe the patients may be observed and followed up conservatively [1]. Mayfield et al. [12] determined progression of 5° per year during the spine growth period in their study including 27 patients. It was also indicated that type 3 CK with unsegmented anterolateral bar including posterolateral wedge on the opposite side was the most progressive spinal deformity and the rarest combination so far. They suggested that these patients should be operated immediately [12].
McMaster and Singh [1] stated that CK was a rapid progressing disease during adolescent growth spurt. They concluded that posterolateral deformity progressed 2.5° annually before the age of 10 and it progressed 5° per year after the age of 10. They also mentioned that progression in posterior hemivertebra was likely to be better than the previous case. They observed that butterfly and wedge vertebral deformities were less aggressive when compared to the other two deformities [1]. Another important finding in their study was that the formation defect in two adjacent vertebrae progressed much faster than the defect in a single one [1]. Anomaly in two adjacent vertebrae was observed in seven patients in our study. Six of these patients were classified as type 1 and one patient as type 3.
Spinal osteotomies are useful for the surgical management of the deformities that are too rigid to be corrected either with instrumentation alone or with the addition of simple posterior soft tissue releases [14]. There are different types of osteotomies including Smith-Peterson osteotomy (SPO), pedicle subtraction osteotomy (PSO), bone-disk-bone osteotomy (BDBO) and vertebral column resection (VCR) for deformity correction and maintenance of sagittal and coronal balance [14] In the current report, all of the patients were older than 8 years and local kyphosis angles were significant (>60°), thus, we decided to perform closing wedge osteotomy followed by posterior instrumented fusion for the management of kyphotic deformity.
Vertebral wedge osteotomy was first described by Scudese and Calabro [15] in a young woman with lumbar kyphotic deformity due to advanced Romatoid Spondylitis via resection of a portion of the posterior elements, lumbar disk and vertebral body with subsequent manipulation of the spine into extension. Then numerous studies on the management of adult sagittal imbalance came up with different osteotomy options and posterior only approaches became more popular in recent years [14]. Closing wedge osteotomy, hinging on the intact anterior cortex has the advantage of achieving correction through all three columns. An average of 30°–40° correction can be achieved at one level via closing wedge osteotomy [14]. Although it is a technically demanding procedure with potential complications good to excellent clinical and radiological outcomes with the technique have been reported in the literature (Table 4). This technique aims to correct the deformity by single surgery from posterior to the apex of kyphosis in order to reduce morbidity of combined approaches. Shimode et al. [16] mentioned that they accomplished 52.9 % correction in kyphosis with sufficient sagittal balance correction via posterior wedge osteotomy on seven patients with kyphosis due to rigid kyphoscoliosis. They concluded that although this technique was not a simple one, it was safe and effective. Monitoring of the spinal cord function during surgery has also provided additional safety in carrying out an osteotomy [16], but pseudoarthrosis in the postoperative period and neurological complications still appear to be major risk factors of the procedure. In the current study, we did not have the chance to use a neuromonitoring system but a supine wake up test was used and we achieved 53.5 % correction in local kyphosis angle and sagittal balance was restored. Although complications were observed in three patients, none of the patients suffered neurological deficit.
The retrospective nature of the study, the lack of adequate clinical data and the limited number of patients involved may be defined as the weaknesses of the current study.
In conclusion, our results consisting of a mean follow-up period of 4 years suggest that closing wedge osteotomy with posterior instrumented fusion performed in the early stages of the deformity is an efficient method of surgical treatment in terms of sagittal balance restoration and deformity correction in patients with congenital kyphosis. Although we did not use spinal cord monitoring at the time, we recommend its use for extra safety.
References
McMaster MJ, Singh H (1999) Natural history of congenital kyphosis and kyphoscoliosis. A study of one hundred and twelve patients. J Bone Joint Surg Am 81:1367–1383
Tsou PM (1977) Embryology of congenital kyphosis. Clin Orthop 128:18–25
Morin B, Poitras B, Duhaime M et al (1985) Congenital kyphosis by segmentation defect: etiologic and pathologic studies. J Ped Orthop 5:309–314
Winter RB, Moe JH, Wang JF (1973) Congenital kyphosis. Its natural history and treatment as observed in a study of one hundred and thirty patients. J Bone Joint Surg Am 55:223–256
Marks DS, Qaimkhani SA (2009) The Natural history of congenital scoliosis and kyphosis. Spine 34(17):1751–1755 (Review)
James JI (1955) Kyphoscoliosis. J Bone Joint Surg Br 37:414–426
Lubicky JP (1997) Congenital scoliosis. In: Weinstein SL (ed) The textbook of spinal surgery, 2nd edn. Lippincott Williams and Wilkins, Philadelphia
Montgomery SP, Hall JE (1982) Congenital kyphosis. Spine 4:360–364
Winter RB, Moe JH (1982) The results of spinal arthrodesis of congenital spinal deformities in patients younger than five years old. J Bone Joint Surg 64-A:419–432
Winter RB, Moe JH, Lonstein JE (1985) The surgical treatment of congenital kyphosis: a review of 94 patients age 5 years or older with 2 years or more follow-up in 77 patients. Spine 10:224–231
McMaster MJ, Singh H (2001) The surgical management of congenital kyphosis and kyphoscoliosis. Spine 26(19):2146–2154 (discussion 2155)
Mayfield JK, Winter RB, Bradford DS, Moe JH (1980) Congenital kyphosis due to defects of anterior segmentation. J Bone Joint Surg Am 62(8):1291–1301
Kim YJ, Otsuka NY, Flynn JM, Hall JE, Emans JB, Hresko MT (2001) Surgical treatment of congenital kyphosis. Spine 26(20):2251–2257
Enercan M, Ozturk C, Kahraman S, Sarier M, Hamzaoglu A, Alanay A (2012) Osteotomies/spinal column resections in adult deformity Eur Spine J (Epub ahead of print. doi:10.1007/s00586-012-2313-0)
Scudese VA, Calabro JJ (1963) Vertebral wedge osteotomy. JAMA 186(7):627–631
Shimode M, Kojima T, Sowa K (2002) Spinal wedge osteotomy by a single posterior approach for correction of severe and rigid kyphosis or kyphoscoliosis. Spine 27(20):2260–2267
Zeng Y, Chen Z, Qi Q, Guo Z, Li W, Sun C, Liu N (2012) The posterior surgical correction of congenital kyphosis and kyphoscoliosis: 23 cases with minimum 2 years follow-up. Eur Spine J (Epub ahead of print. doi:10.1007/s00586-012-2463-0)
Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine 37(19):1667–1675
Zeng Y, Chen Z, Guo Z, Qi Q, Li W, Sun C (2012) Complications of correction for focal kyphosis after posterior osteotomy and the corresponding management. J Spinal Disord Tech (Epub ahead of print)
Bakaloudis G, Lolli F, Silvestre DM, Greggi T, Astolfi S, Martikos K, Vommaro F, Barbanti-Brodano G, Cioni A, Giacomini S (2011) Thoracic pedicle subtraction osteotomy in the treatment of severe pediatric deformities. Eur Spine J 20(Suppl 1):S95–S104. doi:10.1007/s00586-011-1749-y
Li XF, Liu ZD, Hu GY, Chen B, Zhong GB, Zang WP, Wang HT (2011) Posterior unilateral pedicle subtraction osteotomy of hemivertebra for correction of the adolescent congenital spinal deformity. Spine J 11(2):111–118
Hyun SJ, Rim SC (2010) Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc 47:95–101
Mummaneni PV, Dhall SS, Ondra SL, Mummaneni VP, Berven S (2008) Pedicle subtraction osteotomy. Neurosurgery 63(3 Suppl):171–176
Kim YJ, Bridwell KH, Lenke LG, Cheh G, Baldus C (2007) Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine 32(20):2189–2197
Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, Baldus C, Blanke K (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine 28(18):2093–2101
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Atici, Y., Sökücü, S., Üzümcügil, O. et al. The results of closing wedge osteotomy with posterior instrumented fusion for the surgical treatment of congenital kyphosis. Eur Spine J 22, 1368–1374 (2013). https://doi.org/10.1007/s00586-013-2755-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2755-z