Abstract
Introduction
Magnetic resonance images (MRI) fluid sign and intravertebral vacuum phenomenon of the plain radiograph are considered as the characteristic radiological findings for vertebral osteonecrosis after spinal fractures. We aim to study the association between the radiological and histopathologic findings of vertebral osteonecrosis through the use of an open retrieval of specimens.
Materials and methods
Twenty consecutive patients (54–84 years, mean 73 years) of unstable vertebral compression fractures treated with anterior corpectomy and fusion were included. All the images and pathologies were correlated, especially the histopathologic changes to the fluid sign and vacuum phenomenon.
Results
MRI fluid signs and the histopathologic findings of vertebral osteonecrosis were significantly correlated and both were noted in the first 5 months after injury. The power of the fluid sign in diagnosing vertebral osteonecrosis was better than that of the intravertebral vacuum phenomenon (diagnostic odds ratio 65 vs. 2, sensitivity 86 vs. 50 %, specificity 100 vs. 67 %).
Conclusion
MRI fluid sign is more predictable to diagnose vertebral osteonecrosis in operative case, especially within the initial 5 months after injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major public health concern worldwide and a major cause of spinal fracture in the elderly. The prevalence of vertebral fractures has been reported to range between 15 and 35 % among postmenopausal Caucasian and Asian women [1–3]. Most patients with such injuries might sustain a low-energy injury due to poor bone quality. The majority of these fractures heals uneventfully with conservative treatment with a mild backache as a residual. However, some of these patients continue to experience pain or neurological deficits: some of them may have developed delayed posttraumatic osteonecrosis [4–6]. The understanding of the natural history of vertebral fracture remains challenging because the healing potential is influenced by a variety of biochemical, biomechanical, cellular, and pathological mechanisms [7].
In the middle of the last century, many thought that the eponymous designation of “Kummell’s disease” referred to post-traumatic vertebral fractures which were initially asymptomatic, but then progressed [8, 9]. More recently, Kummell’s disease has been felt to represent the vertebral body collapse after a minor trauma seemingly because of osteonecrosis (ON) [4, 6]. This definition most likely arises from the work of Schmorl and Junghanns on the basis of histopathologic analysis at autopsy of patients with posttraumatic vertebral collapse, suggested that Kummell’s disease is caused by ischemia [10].
However, the diagnostic criteria for establishing Kummell’s disease (or posttraumatic vertebral ON) are still unclear and a subject of debate. With the advent of radiograph technology, the researches of modern imaging have offered a great contribution to the clinical diagnosis, decision of treatment and prognosis of spinal disorders [11–13]. In the literatures, posttraumatic vertebral ON was diagnosed based on the radiological findings of a fluid sign or intravertebral vacuum phenomenon [14–17]. Nevertheless, the correlation between the radiological and histopathologic findings has seldom been reported, especially by means of an open retrieval of specimens.
The purpose of this study was to investigate the relationship among the radiological findings, fluid signs and vacuum phenomena, and the histopathology and specimens retrieved from operation on fractures of vertebral bodies.
Materials and methods
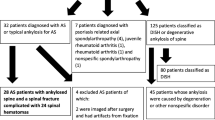
We performed a retrospective review of patients of unstable vertebral compression fractures treated with anterior corpectomy and fusion at our institution between November 2004 and March 2008. Twenty consecutive patients, 17 women and 3 men, with a mean age of 73 years (range 54–84 years), were included in this study (Table 1). All patients had sustained low-energy injuries, including injury following a slip, standing, and bending. They all had an unhealed vertebral compression fracture with collapse, failed conservative treatment, and a compromised spinal canal. Eight patients were suffered with a neurological deficit. On the American Spinal Injury Association (ASIA) impairment scale, five patients were classified as “D”, two patients were “C” and one was “B”. Most patients had comorbidities of aging such as cardiovascular diseases, degenerative joint disorders, etc. Those with malignancy, metabolic disease, inflammatory disease, chronic steroid administration, previous spinal surgery, radiation therapy, alcoholism or infection were excluded from the study.
Radiological evaluation
All patients underwent imaging with magnetic resonance images (MRI) and plain radiographs preoperatively, including conventional anteroposterior, lateral, lateral flexion, and extension stress radiography (cross-table lateral supine stress radiograph to increase the discovery of intravertebral vacuum phenomenon [18]) preoperatively. The MRI protocol included sagittal and axial T1-weighted fast spin-echo images, axial T2-weighted fast spin-echo images, and sagittal short inversion time inversion-recovery (STIR) images with 4-mm section thickness. The vertebral compression fractures might contain an accumulation of intravertebral fluid described as a well-circumscribed area of low signal intensity on T1-weighted MRI and high signal intensity on T2-weighted images (isointense to cerebrospinal fluid), which belongs to the fluid sign [14, 16]. The vacuum phenomenon is a collection of gas which creates a linear or semi-lunar radiolucent shadow on the radiograph [15, 17]. Two experienced orthopaedic surgeons evaluated the images in a blinded fashion with respect to the histology results independently. A senior musculoskeletal radiologist had been consulted if disagreements existed regarding the image findings. All disagreements were resolved by consensus.
Surgical procedure
All patients underwent open anterior spinal surgery with anterior corpectomy to decompress the retropulsed bone fragments to relieve the pressure on the spinal cord or dural sac. Then, we performed vertebral body replacement with an expandable cage or strut bone graft, and fixed with rod and pedicle screw instrumentation [19]. During the operation, the specimens from corpectomy, containing the area of interest which was determined by both the preoperative images and intraoperative findings, were prepared with a bone chisel. We retrieved the specimens whose location, usually a cavity with or without fluid, is correlated with the radiological lesion to study the histopathologic changes. For all cases, the technique of taking specimens was standard [20].
Histology
The suspicious specimens retrieved from corpectomy were used for the histopathologic study in all 20 patients. All surgical samples were immediately fixed in 4–6 % buffered formaldehyde and gently decalcified in 0.1 M EDTA. The paraffin-embedded specimens were cut 3 μm in slices and mounted on glass slides for hematoxylin and eosin staining. A histomorphological analysis was performed using light microscope allowing the evaluation of bone necrosis and regeneration. Two senior pathologists reviewed the histologies with no knowledge of the image findings independently. All disagreements were resolved by consensus.
Statistical analysis
The level of fracture sites, duration of symptoms, MRI findings, plain X-ray findings, and histopathological characteristics were recorded by cases for further studies (Table 1). Back pain intensity was recorded using the visual analog scale (VAS) score (10-point scale). All the images and pathologies were correlated, especially the histopathologic changes to the fluid sign and vacuum phenomenon. Sensitivity, specificity, positive and negative predictive values, positive and negative likelihood ratios, and diagnostic odds ratio with 95 % confidence intervals were calculated by the statistic software Meta-DiSc (developed by Ramón y Cajal Hospital, Madrid, Spain) [21].
Results
The mean interval from injury to image and operation was 6.5 months (range 1–22 months). The levels of fractures in these 20 patients were located from T8 to L3. Most of the fractures (18/20) led to more than 50 % anterior vertebral body height loss. The average local kyphotic angle was 17.2° ± 10.9° (8.5°–42.3°). The average VAS score for back pain was 8.3 ± 1.5 (range 6–10). In analyzing the MRI findings, the fluid sign could be recognized in 12 patients (Fig. 1). Intravertebral vacuums were identified in the preoperative plain radiograph in 9 patients (Fig. 2). Four patients did not have the fluid sign neither the intravertebral vacuums, while all of four images were obtained more than 12 months after injury.
Specimens of the vertebral bodies were retrieved from all 20 patients. The histological analysis revealed that 14 patients had dispersed small necrotic bone fragments, with empty lacuna within the trabecular network, surrounded with a fibrous stroma that was consistent with the phenomenon of ON. Normal bone marrow with hematopoietic cells and fat cells was replaced by reactive fibrosis (Fig. 3). Among the 14 patients, 86 % (12/14) had fluid signs identified in the MRI and 50 % (7/14) had intravertebral vacuums in the plain x-ray. For the six cases without the findings of ON, no fluid sign but two intravertebral vacuums were noted. Regarding the date of ON onset, all specimens retrieved within the initial 5 months after fracture had ON. In all cases in which pathologies were obtained more than 5 months after fracture there was no ON. Interestingly, all MRI fluid signs were also identified in the first 5 months after injury.
If viewing from the MR findings, all of the 12 patients with a fluid sign in the MRI had vertebral ON. The sensitivity and specificity of the fluid sign in diagnosing ON were 86 and 100 %; the positive and negative predictive values were 100 and 75 %, and the positive and negative likelihood ratios were 11.7 and 0.18. The diagnostic odds ratio was 65 and the diagnostic accuracy was 90 % (Table 2).
If viewing from the X-ray findings, the sensitivity and specificity of the vacuum phenomenon in diagnosing ON were 50 and 67 %; the positive and negative predictive values were 78 and 36 %, and the positive and negative likelihood ratios were 1.5 and 0.75. The diagnostic odds ratio was two and the diagnostic accuracy was 55 %. The diagnosing power of the fluid sign in MRI was better than the intravertebral vacuum phenomenon in plain radiography in all parameters (Table 2).
Bone regeneration, including mesenchymal cell proliferation, neovascularization, dead bone resorption by osteoclasts, or new woven bone formation by osteoblasts, could be identified in 16 patients between 1 and 18 months after initial trauma (Fig. 4). The findings of bone regeneration were found to have occurred in 86 % (12/14) of ON cases. Patients with a fluid sign seemed to be more prone to having bone regeneration (10/12) than those without a fluid sign (6/8). Patients with an intravertebral vacuum phenomenon also seemed to have a greater chance of having bone regeneration (8/9) than those without such a phenomenon (8/11). However, neither association reached statistical significance.
Histological sections of block specimens retrieved from operation (hematoxylin and eosin, ×10 (a) and ×40 (b). a Regenerative area with granulation tissue (double asterisk) and new bone formation (asterisk). b Osteoblast rimming the new bone (black arrow) and neovasculization in the granulation tissue (white arrow)
Discussion
In summary, the present study suggested that the MRI fluid sign is powerful in correlating with the histopathologic signs of vertebral ON, as defined by the presence of dispersed small necrotic bone fragments surrounded with fibrous stroma. The diagnostic odds ratio was up to 65. The sensitivity and specificity were 86 and 100 %, respectively.
The diagnosis of vertebral ON carries historical baggage with regard to conceptualization of the image, pathology, the prognosis, and treatment implications. Recollapse of the treated vertebrae and PMMA cement dislodgment after percutaneous vertebroplasty were reported as early complications with the predisposing factor of pre-operative ON [22–24]. Thus, it is important to obtain the diagnosis of vertebral ON prior to making a decision on treatment, since it should be taken into consideration. Currently, vertebral ON remains a radiographic diagnosis, but most studies correlated the histopathology and image finding from percutaneous needle biopsy [4, 25, 26]. To the best of our knowledge, only Baur et al. [27] reported the histological comparison of fluid sign in four osteoporotic and one metastatic fracture by open retrieval of specimen from surgery. In the present study, we took the specimen during operation which was obtained from the intravertebral cavity and its neighboring tissue. It will be more reliable for analysis and evidence.
The Kummell’s disease represents posttraumatic avascular necrosis of the vertebral body that is thought to be the consequence of vascular insult at the anterior segment of the vertebral body. The possible pathogenesis is disruption of the blood supply related to fracture and inadequate revascularization of bone marrow [4, 28]. Besides, increased marrow pressure caused by intramedullary hemorrhage leads to increased adipocyte size with a proportionate decrease in intraosseous blood flow, also predisposing patients to ischemic necrosis of the vertebral body [29]. Additional risk factors for Kummell’s disease include age-related osteoporosis and steroid usage [6]. The histologic hallmarks include the presence of marrow fat necrosis and empty osteocyte lacunae. The reparative process usually begins thereafter, replacing necrotic bone marrow with scar-like fibrous tissue [30]. Our study also found that vertebral ON could be recognized only in the initial 5 months while regeneration continued until 18 months after osteoporotic fracture.
Controversies exist regarding the pathomechanism of the fluid sign and intravertebral vacuum cleft in the osteoporotic spinal fracture. Some authors have proposed that osteoporotic fracture leads to interruption of the blood supply to the vertebral body and fluid accumulation in the ON space [14, 27]. If nonunion occurred and resulted in excessive motion, the central portion of the callus might undergo cystic degeneration. A synovial-lined membrane secreting synovial fluid might later envelope this degeneration cavity [30]. Regarding the intravertebral vacuum phenomenon, some authors think it is the result of vertebral ON [15, 16, 31], whereas some believe that it signifies nonunion and pseudoarthrosis [32, 33]. Lafforgue et al. [34] argued that the intravertebral vacuum phenomenon could simply be a result of the migration of an intradiscal gaseous collection through a fractured endplate of an osteoporotic collapse. However, the causes of both the fluid sign and intravertebral vacuum phenomenon are still uncertain and need further investigation.
The early stages of vertebral ON are thought to be characterized by fluid and inflammatory exudate components [35]. In the latter stages, air might accumulate in the void formed by the sclerotic bone. In a retrospective MRI study, Yu et al. [25] reported a sequential change from intravertebral fluid to gas in some of their patients who had a follow-up MRI. Our results revealed that the MRI fluid sign was identified from 1 to 5 months, while intravertebral vacuum phenomenon was noted from 2 to 10 months after fracture of the vertebrae. The equating of the fluid sign to vertebral ON might be explained by the early avascular and inflammatory stage. Further studies are required to clarify the sequential pathological changes after vertebral osteoporotic fracture.
The exact date of ON onset is usually unknown, though it should be considered as when patients are exposed to the risk factors, such as trauma or glucocorticoid use. Prospective MRI studies of patients with femoral neck fractures showed evidence of femoral head avascular necrosis in some cases after operation, all of which were diagnosed 1–6 months after the fracture [35, 36]. Kawasaki et al. [36] suggested that the interval providing the greatest sensitivity, specificity, and accuracy of the diagnosis of ON of the femoral head by MRI was 6 months after surgery. With good correlation in MRI fluid signs and the histopathologic findings of vertebral osteonecrosis, our series had similar findings, in that all vertebral ON occurred and all MRI fluid signs were identified in the initial 5 months after fracture.
While regeneration occurred in most (80 %) cases, we found that patients with a fluid sign or intravertebral vacuum phenomenon were both prone to bone regeneration, such as dead bone resorption, new bone formation, and primary mesenchymal cell proliferation after vertebral osteoporotic fracture. In spite of the regeneration process, these patients were still liable to have unstable collapsed vertebra, canal compromise, neurologic deficits, and clinical symptoms; so ultimately, they underwent anterior corpectomy, anterior spinal fusion, and instrumentation in this series. There were four patients (20 %) without histological characteristics of regeneration. The reason remains unclear but might be attributed to bias in retrospective analysis.
There are limitations of this study including limited case number and lack of longitudinal data. However, we can still have a more clear profile of the correlation between the images and histopathologies with time sequence through this study, although future researches are required to clarify the detailed sequential pathological changes. Besides, all the samples were vertebral fractures with surgical indications. These fractures tended to be more unstable, and possibly non-united with a greater degree of fracture severity. Thus, the results are obtained from selected cases and might not be applicable to all fractures of the vertebrae. Another limitation is the retrospective design of our study. A prospective study is still needed to further clarify the correlation between the radiological and histological findings of vertebral ON.
Conclusion
In conclusion, there was significant correlation of the histopathologic signs of ON and MRI fluid sign in our study population of 20 operative cases. MRI fluid sign seemed to be reliable for predicting ON in vertebral fracture caused by minor trauma (sensitivity 86 %, specificity 100 %, diagnostic odds ratio 65). Therefore, patients, who sustained vertebral fractures caused by low-energy trauma and presented with surgical indications and MRI fluid signs, should be highly suspected to have vertebral ON, especially within the initial 5 months after injury.
References
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European vertebral osteoporosis study. J Bone Miner Res 11:1010–1018
Lau EM, Chan HH, Woo J, Lin F, Black D, Nevitt M, Leung PC (1996) Normal ranges for vertebral height ratios and prevalence of vertebral fracture in Hong Kong Chinese: a comparison with American Caucasians. J Bone Miner Res 11:1364–1368
Ho-Pham LT, Nguyen ND, Vu BQ, Pham HN, Nguyen TV (2009) Prevalence and risk factors of radiographic vertebral fracture in postmenopausal Vietnamese women. Bone 45:213–217. doi:10.1016/j.bone.2009.04.199
Swartz K, Fee D (2008) Kummell’s disease: a case report and literature review. Spine (Phila Pa 1976) 33:E152–155. doi:10.1097/BRS.0b013e3181657f31
Ma R, Chow R, Shen FH (2010) Kummell’s disease: delayed post-traumatic osteonecrosis of the vertebral body. Eur Spine J 19:1065–1070. doi:10.1007/s00586-009-1205-4
Young WF, Brown D, Kendler A, Clements D (2002) Delayed post-traumatic osteonecrosis of a vertebral body (Kummell’s disease). Acta Orthop Belg 68:13–19
Kalfas IH (2001) Principles of bone healing. Neurosurg Focus 10:E1
Steel HH (1951) Kummell’s disease. Am J Surg 81:161–167
Kummell H (1895) Die raretizierende Ostitis der Wirbelkörper. Deutselse Med 21:180–181
Schmorl H, Junghanns G (1971) The huınan spine in health and disease. 2nd edn. Grune & Stratton, New York, pp 154–156
Arlet V, Orndorff DG, Jagannathan J, Dumont A (2009) Reverse and pseudoreverse cortical sign in thoracolumbar burst fracture: radiologic description and distinction–a propos of three cases. Eur Spine J 18:282–287. doi:10.1007/s00586-008-0848-x
Lin WC, Lu CH, Chen HL, Wang HC, Yu CY, Wu RW, Cheng YF, Lui CC (2010) The impact of preoperative magnetic resonance images on outcome of cemented vertebrae. Eur Spine J 19:1899–1906. doi:10.1007/s00586-010-1434-6
Brown DB, Glaiberman CB, Gilula LA, Shimony JS (2005) Correlation between preprocedural MRI findings and clinical outcomes in the treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. AJR Am J Roentgenol 184:1951–1955
Dupuy DE, Palmer WE, Rosenthal DI (1996) Vertebral fluid collection associated with vertebral collapse. AJR Am J Roentgenol 167:1535–1538
Maldague BE, Noel HM, Malghem JJ (1978) The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 129:23–29
Naul LG, Peet GJ, Maupin WB (1989) Avascular necrosis of the vertebral body: MR imaging. Radiology 172:219–222
Theodorou DJ (2001) The intravertebral vacuum cleft sign. Radiology 221:787–788
Kim DY, Lee SH, Jang JS, Chung SK, Lee HY (2004) Intravertebral vacuum phenomenon in osteoporotic compression fracture: report of 67 cases with quantitative evaluation of intravertebral instability. J Neurosurg 100:24–31
Lin RM, Huang KY, Lai KA (2008) Mini-open anterior spine surgery for anterior lumbar diseases. Eur Spine J 17:691–697. doi:10.1007/s00586-008-0644-7
Huang KY, Yan JJ, Lin RM (2005) Histopathologic findings of retrieved specimens of vertebroplasty with polymethylmethacrylate cement: case control study. Spine (Phila Pa 1976) 30:E585–588
Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A (2006) Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Methodol 6:31. doi:10.1186/1471-2288-6-31
Heo DH, Chin DK, Yoon YS, Kuh SU (2009) Recollapse of previous vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int 20:473–480. doi:10.1007/s00198-008-0682-3
Leslie-Mazwi T, Deen HG (2006) Repeated fracture of a vertebral body after treatment with balloon kyphoplasty: case illustration. J Neurosurg Spine 4:270. doi:10.3171/spi.2006.4.3.270
Tsai TT, Chen WJ, Lai PL, Chen LH, Niu CC, Fu TS, Wong CB (1976) Polymethylmethacrylate cement dislodgment following percutaneous vertebroplasty: a case report. Spine (Phila Pa 1976) 28:E457–460. doi:10.1097/01.BRS.0000096668.54378.25
Yu CW, Hsu CY, Shih TT, Chen BB, Fu CJ (2007) Vertebral osteonecrosis: MR imaging findings and related changes on adjacent levels. AJNR Am J Neuroradiol 28:42–47
Libicher M, Appelt A, Berger I, Baier M, Meeder PJ, Grafe I, Dafonseca K, Noldge G, Kasperk C (2007) The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol 17:2248–2252. doi:10.1007/s00330-007-0684-0
Baur A, Stabler A, Arbogast S, Duerr HR, Bartl R, Reiser M (2002) Acute osteoporotic and neoplastic vertebral compression fractures: fluid sign at MR imaging. Radiology 225:730–735
Lafforgue P (2006) Pathophysiology and natural history of avascular necrosis of bone. Joint Bone Spine 73:500–507. doi:10.1016/j.jbspin.2006.01.025
Saito S, Inoue A, Ono K (1987) Intramedullary haemorrhage as a possible cause of avascular necrosis of the femoral head. The histology of 16 femoral heads at the silent stage. J Bone Joint Surg Br 69:346–351
Kilpatrick SE RJ (2004) Diagnostic musculoskeletal surgical pathology. 1st edn. Saunders, Philadelphia, pp 362–364
Ma R, Chow R, Shen FH (2010) Kummell’s disease: delayed post-traumatic osteonecrosis of the vertebral body. Eur Spine J 19:1065–1070. doi:10.1007/s00586-009-1205-4
Hasegawa K, Homma T, Uchiyama S, Takahashi H (1998) Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976) 23:2201–2206
Hasegawa K, Homma T, Uchiyama S, Takahashi HE (1997) Osteosynthesis without instrumentation for vertebral pseudarthrosis in the osteoporotic spine. J Bone Joint Surg Br 79:452–456
Lafforgue P, Chagnaud C, Daumen-Legre V, Daver L, Kasbarian M, Acquaviva PC (1997) The intravertebral vacuum phenomenon (“vertebral osteonecrosis”). Migration of intradiscal gas in a fractured vertebral body? Spine 22:1885–1891
Sugano N, Masuhara K, Nakamura N, Ochi T, Hirooka A, Hayami Y (1996) MRI of early osteonecrosis of the femoral head after transcervical fracture. J Bone Joint Surg Br 78:253–257
Kawasaki M, Hasegawa Y, Sakano S, Sugiyama H, Tajima T, Iwasada S, Iwata H (2001) Prediction of osteonecrosis by magnetic resonance imaging after femoral neck fractures. Clin Orthop Relat Res: 157–164
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, CL., Lin, RM., Huang, KY. et al. MRI fluid sign is reliable in correlation with osteonecrosis after vertebral fractures: a histopathologic study. Eur Spine J 22, 1617–1623 (2013). https://doi.org/10.1007/s00586-012-2618-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2618-z