Abstract
Purpose
The combined recordings of epidural-(D wave) and muscle motor evoked potentials (m-MEPs) have been proposed in many studies in intramedullary spinal cord tumour (IMSCT) surgery, although not all agree. Furthermore, the usefulness of the intraoperative monitoring of motor systems using these methods in other types of spine surgery has not yet been clearly confirmed. The aim of this study is to test the impact of intraoperative D wave on the monitorability and motor outcome in spine surgery.
Methods
Intraoperative recording of posterior tibial nerve somatosensory potentials, lower limb m-MEPs (LLm-MEPs) and epidurally recorded D wave caudally to the surgical level was attempted in a total of 103 spine and spinal cord surgeries (23 IMSCT, 55 extramedullary spinal cord tumours and 25 myelopathies).
Results
There was a 97.1 %, overall monitorability where at least 1 of the 3 modalities was applicable in 100 surgical procedures. Baseline LLm-MEPs were recorded bilaterally in 85 cases and unilaterally in 11. A caudal D wave was recorded in 97 cases. Transient, or persistent intraoperative modifications occurred in 14/23 IMSCT, 5/55 extramedullary spinal cord tumours and in 2/25 myelopathies. The presence of a persistent stable caudal D wave was predictive of a good motor outcome even when the LL-MEPs were absent and/or when lost during surgery.
Conclusions
Not only is intraoperative D wave recording to be considered mandatory in IMSCT surgery but it should also be attempted in other types of spine/spinal cord surgeries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Persistent neurologic sequelae may be the devastating consequences of spine and spinal cord surgery. The aim of neurophysiologic intraoperative monitoring (IOM) is to identify a spinal cord injury at a reversible stage or, in the case of neurologic damage, its documentation, as well as to provide information as to motor outcome.
An ideal technique tailored to this aim should have a solid neurophysiologic basis, be system-specific, provide a (quasi) real-time assessment, be applicable even in compromised patients and it should be safe.
The introduction of transcranially motor evoked potentials (MEPs) represented a significant step forward for intraoperative assessment of motor pathway function in spine surgery [1–7]. Two methodologies have been developed to elicit MEPs by transcranial electrical stimulation [7]:
-
1.
Recording the D wave directly from the epidural space (e-MEPs; in this study e-MEPs and D wave are used as synonyms) evoked by a single electrical shock (single pulse technique) [1, 2];
-
2.
Recording of MEPs in limb muscles (m-MEPs) elicited by a short train of electrical stimuli (multipulse technique) [4, 5].
The information provided by these two techniques is complementary, as the D wave is generated by the direct activation of the axons of fast-conducting fibres of the cortico-spinal tract [8]. Whilst m-MEPs depend also by the excitability of facilitatory cortical motor neurons, beyond the spinal cord conductivity and the excitability of lower motoneurons [7, 9].
Numerous studies have proposed the combined use of D wave recordings and m-MEPs in intramedullary spinal cord surgery [6, 10–13], however, not all literature is in agreement [14–16].
Furthermore, the usefulness of the IOM of motor systems using both methods in other types of spine surgery has still not been fully clarified. This is particularly true in compromised patients where the multipulse technique may fail to evoke m-MEPs in one, or more target muscles [3, 16]. Indeed, epidurally recorded D wave is mainly generated by the sub-anodal hemisphere, but a contribution from the controlateral cortical spinal tract is highly probable, particularly with the stimulation intensities used in spine surgery [17, 18].
The aims of this study were:
-
1.
To investigate the registrability of the D wave caudal to the surgical site in comparison with neurologic status, posterior tibial nerve somatosensory evoked potentials (ptn-SEPs) and lower limbs muscle MEPs (LLm-MEPs)
-
2.
To study the impact of intraoperative D wave recording on motor outcome in a series of spine and spinal cord surgical procedures.
Materials and methods
An attempt was made to carry out LLm-MEP, e-MEPs and SEPs monitoring in a total of 103 surgical procedures for 101 patients (61 females, 40 males, average age 56.3 ± 19.2 years, range 3–85). Surgery was planned for intramedullary spinal cord tumour (IMSCT) resection in 23 procedures, for extramedullary spinal cord tumours (EMSCT) in 55 and 25 for myelopathies. Three surgical procedures involved the occipito-cervical region, 36 the cervical cord, 9 the cervico-dorsal level and 55 the dorsal level.
The clinical data are summarized in Table 1.
Any patients with lesions located below D10, or who had documented desynchronized D waves during previous surgical procedures were excluded. Preoperative neurological status was scored by the McCormick scale [19] as, although this scale has been proposed for IMSCT, it can also be used for scoring neurologic status in other spinal cord pathologies (Table 2).
There was a McCormick grade of I in 30 procedures (29.13 %), II in 48 (46.6 %), III in 17 (26.5 %) and IV in 8 (7.77 %).
All patients gave an informed consent after having been informed that potential risks included: seizures, skin burns from stimulating electrodes, tongue/lip bites, cardiac arrhythmias, inadvertent injury caused by TES-induced patient movement, epidural bleeding and/or infections.
The anaesthetic protocol used during surgery included a combination of the two drugs, remifentanil and propofol, with total intravenous anaesthesia (TIVA). Induction was obtained with a continuous infusion of Remifentanil at 0.10–0.20 mg/kg/min and maintained with 0.25–0.40 mg/kg/min. Target-controlled infusion was used for Propofol with a plasma concentration for induction of 3–4 mg/ml and maintenance with 4–5 mg/ml. No muscle relaxants were used after induction and intubation.
Ptn-SEPs were elicited by a 100–300 μs square-wave electrical pulses presented sequentially to the posterior tibial nerve at the ankle (rate 4.1–7.1/s, stimulus intensity adjusted individually from 15 to 40 mA). In order to optimize the montage, monopolar needle electrodes were placed at Cz′, C3′, C4′ and Fz (international 10-20 EEG system) and the best traces among Cz′-Fz, C3′-Fz, C4′-Fz, C3′-C4, C4′-C3 were used for monitoring. Filtering was typically 30–1,000 Hz, with a 100 ms analysis time; averaging was stopped manually at such times as potentials were clearly reproducible.
The m-MEPs were elicited with a brief duration of transcranially applied electrical pulse anodal electrical stimulus train (N = 3–7, ISI 2–4 ms), delivered by two corkscrew-type electrodes inserted over the motor cortex regions, at C1, C2, C3 and C4 (international 10-20 EEG system). A C1–C2, or C3–C4 dipole was used to elicit right m-MEPs and vice versa. Stimuli were delivered through a commercially available constant-voltage electrical stimulator (D185; Digitimer, Welwyn Garden City, United Kingdom) (pulse width = 50 μs, voltage 200–700 V) or a constant-voltage stimulator (CRO STIM 2, Inomed, Tenningen, Germany; pulse width = 500 μs, current 80–200 mA). Responses were recorded on commercially available neurophysiology instrumentation (Nicolet Endeavor; Nicolet Biomedical, Madison, WI, USA). Right extremity MEPs were monitored after left-cranium anodal stimulation and vice versa.
The m-MEPs were recorded by a needle electrode placed in the muscle with a belly-tendon montage from the abductor pollicis brevis in the upper extremities and both the tibialis anterior and the abductor hallucis muscles in the lower extremities. The time base was 100–200 ms and the filter bandpass 30–3,000 Hz, occasionally a restricted bandpass was used to reduce artefacts. A rolled piece of gauze was used as a bite block after induction, to avoid lip and/or tongue bites.
Two flexible three-contact platinum epidural electrodes (CEDL-3PIDINX, Ad-Tech Medical instruments corporation, Racine, WI, USA) were inserted by the surgeon above and below the site of surgery, to record e-MEPs.
The D waves were elicited by a single anodal stimulus, delivered with the same electrodes and stimulators as that used for the m-MEPs, with a constantly lower stimulus intensity; filters were typically 200/500–3,000 Hz. The time base was 10–50 ms and, in some cases, an average of 4–10 responses was necessary to improve noise to signal ratio.
The recording montage was electrode 1 to 2 (active to reference) and/or 2 to 3 for the rostral electrode and 2 to 1 and/or 3 to 2 for the caudal electrode, so as to obtain the same polarity response from both electrodes.
A persistent unilateral, or bilateral amplitude loss of at least 50 % of cortical SEPs was used as warning criteria and the surgical team was informed to be on the alert for an amplitude of D wave decrease between 30 and 50 % of baseline values. Any decrement of D waves over and above that of 50 % of baseline value was considered significant. Because there is a large trial-to-trial variability of the normal background for m-MEPs, the warning criteria were set as the disappearing of responses. However, the surgeon was warned if there were persistent amplitude decrements of more than 60 % of baseline values, even if they were not associated to a reduction of complexity.
Results
With the exception of one minor tongue bite, due to the bite block slipping out of place during surgery, none of aforementioned IOM complications were reported in our patients. There was an overall monitorability of 97.1 %, where at least 1 of the 3 modalities was applicable in 100 surgical procedures. Indeed, in three markedly compromised subjects (McKormick grade IV), baseline ptn-SEPs, LLm-MEPs and D wave from the lower epidural electrode were absent.
Therefore, the data herein reported refer to 100 surgical procedures, carried out in 98 subjects where it was possible to apply at least 1 intraoperative neurophysiologic technique.
Baseline ptn-SEPs were recordable for a total of 79 procedures, 74 bilaterally and 5 unilaterally. Baseline LLm-MEPs were recorded bilaterally in 85 surgical procedures and unilaterally in 11. However, whilst a clear caudal D wave was recorded in 97 subjects, it was absent in 3 who were affected by IMSCT and poorly compromised (McKormicK grade I in two, II in 1). Table 3 summarizes the data.
As shown in Table 3, there was a good correlation between neurological status and monitorability of both ptn-SEPs and LLm-MEPs. Baseline bilateral ptn-SEPs were present bilaterally in 85.9 % of grades I–II and in 31.8 % of grades III–IV, unilaterally in 2.6 of grades I–II and 13.6 of grades III–IV, bilaterally absent in 11.5 of grades I–II and 54.6 of grades III–IV. Baseline bilateral LL m-MEPs were recordable bilaterally in 97.4 % of grades I–II and in 40.9 % of grades III–IV, unilaterally in 2.6 of grades I–II and 40.9 of grades III–IV, bilaterally absent in 18.2 of grades III–IV.
The caudal D wave was recordable in 96.2 % of grades I–II and in 100 % of grades III–IV.
The most frequent IOM setting was represented by a caudal D wave associated with both bilateral lower limb LLm-MEPs and ptn-SEPs (68 procedures), followed by caudal D wave and bilateral (12 procedures), or unilateral (6) LLm-MEPs. The D wave was the only recordable neurophysiologic parameter in three surgical procedures. Other combinations are reported in Table 4.
No monitoring changes were observed in 79/100 of the procedures and none of these subjects had postoperative deficits. Therefore, the number of procedures with transient, or persistent modifications was 21, 19 of which were persistent and 2 transitory (Table 5).
In two cases (all of them affected by IMSCT) the modifications were persistent loss of SEPs after myelotomy, with stable MEPs (both D wave and m-MEPs).
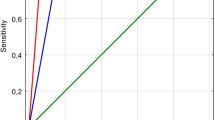
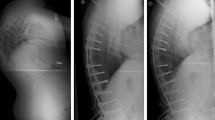
In 16 surgical procedures, a transitory (2 cases), or a persistent loss, or a marked amplitude reduction of lower limb m-MEPs was observed (14 cases), either isolated or in association with a modification of ptn-SEPs (Figs. 1, 2).
IOM of patient #4, affected by cervico-dorsal IMSCT. Despite intraoperative loss/deterioration of LLm-MEPs, associated with D wave (asterisk) amplitude reduction of 40 %, the patient awoke with a mild paraparesis and recovered within 48 h. RTA right tibialis anterior, RAH right abductor hallucis, LTA left tibialis anterior, LAH left abductor hallucis
Intraoperative loss of right LLm-MEPs in a compromised patient (#15, Table 5), affected by EMSCT, with baseline absent left LLm-MEPs and ptn-SEPs. The caudal D wave (*) was recordable and remained stable during the surgical manoeuvres. The patient awoke with a worsening of pre-existing paraparesis and quickly improved. RAH right abductor hallucis, LAH left abductor hallucis
In three cases (affected by IMSCT), baseline D wave was absent and LLm-MEPs disappeared during surgery. Postoperatively, one patient showed transient paraparesis and 2/3 had persistent major motor deficits. In the remaining 13 procedures, a transient, or persistent deterioration of LL m-MEPs with stable caudal D wave, was observed. No postoperative motor deficit was observed in five cases, whilst eight patients presented transient postoperative motor signs. In three cases an intraoperative improvement of MEPs was observed: in 2/3, m-MEPs reappeared, or improved (Fig. 3) and in one case the D wave amplitude increased (baseline ptn-SEPs and LL m-MEPs were absent—Fig. 4).
Intraoperative reappearance of LLm MEPs, in a severely compromised patient affected by a dorsal meningioma (#18). Baseline ptn-SEPs were absent. The patient improved quickly in the postoperative period. RTA right tibialis anterior, RAH right abductor hallucis, LTA left tibialis anterior, LAH left abductor hallucis
Therefore, in five cases, the D wave did not provide relevant data as to motor outcome:
-
In two cases because of the persistent stability of LL m-MEPs;
-
In three cases because of the caudal D wave was absent
In 16 cases, the impact of the intraoperative D wave was significant:
-
In 13 cases a stable caudal D wave predicted no new deficit, or transient postoperative motor deficits in case of loss/deterioration of LL m-MEPs
-
In three compromised patients the caudal D wave predicted the intraoperative reappearance of LL-mMEPs and/or a postoperative improvement.
Briefly, a stable caudal D wave correctly predicted the motor outcome in all cases, even when baseline LL-mMEPs were or in the presence of intraoperative loss/deterioration. When considering the aetiologies, the D wave adds a relevant prognostic value in 9/14 intraoperative modification in IMSCT, as in the remaining cases the modifications were limited to ptn-SEPs, or the D wave was either absent, or chronodispersed. In the remaining diagnostic categories, the impact of D wave was relevant, both in EMSCT (5/55) and myelopathies (2/25), although intraoperative modifications were less frequent than in IMSCT.
Discussion
Transcranial MEPs significantly improved the intraoperative testing of spinal cord function. Nowadays, the combined recording of SEPs and MEPs has become a well-established method for intraoperative testing of spinal cord function in complex spine and/or spinal cord surgery (see ref. [7] for a comprehensive review). Although there is general agreement as to the methodology to elicit both e-MEPs and m-MEPs, controversies do persist as to the indications for IOM with both e-MEPs and m-MEPs [6, 10–16].
Numerous studies have proposed that a combined recording of epidural and muscle MEPs be carried out during IMSCT surgery [6, 10–13] to predict motor outcome in the presence of deterioration/disappearance of LLm-MEPs, however, not all agree [14–16].
Indeed, muscle MEPs may be completely lost during surgery for intramedullary spinal cord tumours but, if the D wave amplitude is either stable, or decreased by less than 50 %, then although the patient will present additional transient motor deficit postoperatively, motor strength will be recovered in terms of post-surgery hours or days [17].
This phenomenon has been defined as “surgically induced transient paraplegia” [17] and is most likely attributable to the reversible inactivation of noncorticospinal descending tracts and the propriospinal system, whilst fast-conducting corticospinal fibres are mostly preserved [17].
If the intraoperative assessment of motor pathways is limited to the m-MEPs, an intraoperative disappearance/deterioration of m-MEPs can be followed by persistent, or transient motor deficit [14–16]. This fact has led to the using of the term false positive, which may be confusing as this refers to m-MEPs that should be considered as only a part, though relevant, of the intraoperative assessment of motor function.
Indeed, the D wave amplitude is a direct measure of the number of functioning fast-conducting fibres in the corticospinal tracts [8]. Since no synapses are involved between the stimulating and the recording site (the proximal axon of the cortical motoneuron is stimulated and the recording site is located below the lesional site, but above the synapses at the alpha-motoneuron), the D wave has been considered the gold-standard in the assessment of the integrity of the cortico-spinal tract [17].
As m-MEP generation depends on the excitability of facilitatory cortical motor neurons, beyond the spinal cord conductivity and the excitability of lower motoneurons, they represent the correlate of not only the cortico-spinal but also of the non-corticospinal tract motor pathways.
In our series, the caudal D wave was the most recordable intraoperative neurophysiologic parameter, particularly in compromised patients, even in cases where baseline LLm-MEPs were unilaterally, or bilaterally absent. Furthermore, the impact of the intraoperative recording of the D wave is relevant in a large percentage of surgical procedures. Indeed, a persistent stability of the caudal D wave is predictive of a good motor outcome, even when the LLm-MEPs are intraoperatively abolished, or diminished. This is particularly true for IMSCT, and also in the other categories studied.
If in our study the intraoperative assessment of motor tracts was limited to m-MEPs, all patients with transient postoperative motor deficit were considered as “false” positive. Conversely, the combined recording of D waves and LLm-MEPs reduces the number of false positives to zero.
Interestingly, in our series, all the three IMSCT patients without a clear caudal D wave intraoperatively lost m-MEPs and two of them presented persistent neurological deficits at follow-up. As there is evidence that SEPs and muscle MEPs are more sensitive to intraoperative spinal cord ischaemia than is the D wave [20], the IOM protocol does not generally include e-MEPs when the risk of spinal cord damage is thought to be ischaemic. However, in the presence of LL m-MEP deterioration, the caudal D wave provides the opportunity to check the cortico-spinal tract function, while countermeasures are taken to avoid persistent spinal cord damage.
The lateralizing value of the D wave is generally considered poor because of the midline recording and the difficulty to restrict the stimulation to a single hemisphere [18]. However, in compromised patients where the multipulse technique may fail to evoke unilateral, or bilateral LLm-MEPs, the caudal D wave may represent the correlate of still functioning fibres of both cortico-spinal tracts. Therefore, it is reasonable that monitoring the D wave may contribute to reducing further damage in an already compromised patient.
As aforementioned, in two cases, the recordability of the caudal D wave was associated to an intraoperative reappearance of LLm-MEPs and, in a third case, an increase in amplitude and latency shortening of the caudal D wave was observed. These intraoperative data were associated to a postoperative improvement of motor status. Although the primary scope of IOM is to prevent any iatrogenic injury, an intraoperative improvement is of primary relevance, not only from a prognostic point of view but also for a correct planning of rehabilitation strategy.
Finally, although this study has demonstrated that MEPs were percentually more recordable than are SEPs for our series, SEPs do retain a great value in assessing dorsal column function, such as proprioception, which is of paramount importance even for locomotion. Moreover, although there is still some concern about D wave recording as it is invasive, intraoperative techniques, in particular transcranial electrical stimulation and spinal epidural recording electrodes are generally considered safe when in the hands of a skilled IOM team [18]. None of our patients reported any of the iatrogenic complications that have been described in literature [18] i.e. injury, infection due to electrode placement, spinal epidural haematomas following insertion of epidural electrodes, neurological complications associated with transcranial motor cortex stimulation and seizures.
In conclusion, our study provides further evidence as to the relevance, impact and safety of epidural motor evoked potentials in spine and spinal cord surgery.
On the basis of our results and personal experience, we are of the opinion that not only should intraoperative D wave recording be considered mandatory in IMSCT surgery but that it should also be attempted in other types of spine and spinal cord surgical procedures, particularly for compromised patients with absent, or poorly defined LL m-MEPs.
References
Boyd SG, Rothwell JC, Cowan JM, Webb PJ, Morley T, Asselman P, Marsden CD (1986) A method of monitoring function in corticospinal pathways during scoliosis surgery with a note on motor conduction velocities. J Neurol Neurosurg Psychiatry 49:251–257
Hicks RG, Burke DJ, Stephen JP (1991) Monitoring spinal cord function during scoliosis surgery with Cotrel-Dubousset instrumentation. Med J Aust 154:82–86
Burke D, Hicks R, Stephen J, Woodforth I, Crawford M (1992) Assessment of corticospinal and somatosensory conduction simultaneously during scoliosis surgery. Electroencephalogr Clin Neurophysiol 85:388–396
Pechstein U, Cedzich C, Nadstawek J, Schramm J (1996) Transcranial high-frequency repetitive electrical stimulation of recording myogenic motor evoked potential with the patient under general anesthesia. Neurosurgery 1996(39):335–344
Jones SJ, Harrison R, Koh KF, Mendoza N, Crockard HA (1996) Motor evoked potential monitoring during spinal surgery: responses of distal limb muscles to transcranial cortical stimulation with pulse trains. Electroencephalogr Clin Neurophysiol 100:375–383
Kothbauer KF, Deletis V, Epstein FJ (1998) Motor-evoked potential monitoring for intramedullary spinal cord tumor surgery: correlation of clinical and neurophysiological data in a series of 100 consecutive procedures. Neurosurg Focus 4:1–9
Deletis V, Sala F (2008) Intraoperative neurophysiological monitoring of the spinal cord during spinal cord and spine surgery: a review focus on the corticospinal tracts. Clin Neurophysiol 119:248–264
Patton HD (1954) Amassian VE Single and multiple unit analisys of cortical stage of pyramidal tract activation. J Neurophysiol 17:345–363
Deletis V, Sala F. Corticospinal tract monitoring with D- and I-waves from the spinal cord and muscle MEPs from limb muscles. In: Daube JR, Mauguiére F (eds) Handbook of clinical neurophysiology. Volume 8. Intraoperative Monitoring of Neural Function [Volume Editor Nuwer MR].Elsevier, 2008, pp.235-251
Kothbauer K, Deletis V, Epstein FJ (1997) Intraoperative spinal cord monitoring for intramedullary surgery: an essential adjunct. Pediatr Neurosurg 26:247–254
Cioni B, Meglio M, Rossi GF (1999) Intraoperative motor evoked potentials monitoring in spinal neurosurgery. Arch Ital Biol 137:115–126
Deletis V (1999) Intraoperative neurophysiological monitoring. In: MacLeone D (ed) Pediatric neurosurgery: surgery of the developing nervous system. 3rd edn. W.B. Saunders, Philadelphia, pp 1204–1213
Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F et al (2006) Intraoperative motor evoked potential monitoring improves outcome after surgery of intramedullary spinal cord tumor: a historical control study in 50 patients. Neurosurgery 58:1129–1143
Quiñones-Hinojosa A, Lyon R, Zada G, Lamborn KR, Gupta N, Parsa AT, McDermott MW, Weinstein PR (2005) Changes in transcranial motor evoked potentials during intramedullary spinal cord tumor resection correlate with postoperative motor function. Neurosurgery 56:982–993
Hyun SJ, Rhim SC (2009) Combined motor and somatosensory evoked potential monitoring for intramedullary spinal cord tumor surgery: correlation of clinical and neurophysiological data in 17 consecutive procedures. Br J Neurosurg 23:393–400
Calancie B, Molano MR (2008) Alarm criteria for motor-evoked potentials: what’s wrong with the “presence-or-absence” approach? Spine (Phila Pa 1976) 33:406–414
Deletis V (2002) Intraoperative neurophysiology and methodologies used to monitor the functional integrity of the motor system. In: Deletis V, Shils JL (eds) Neurophysiology in neurosurgery. Academic Press, New York, pp 25–51
MacDonald DB (2006) Intraoperative motor evoked potentials monitoring: overview and update. J Clin Monit Comput 20:347–377
McCormick PC, Torres R, Post KD, Stein BM (1990) Intramedullary ependymoma of the spinal cord. J Neurosurg 72:525–532
MacDonald DB, Janusz M (2002) An approach to intraoperative neurophysiological monitoring of thoracoabdominal aneurysm surgery. J Clin Neurophysiol 2002(19):43–54
Acknowledgments
This study would not have been possible without the expert technical assistance of Alessandro Borio, Marta Giacobbi, Sonia Marmolino, Maurizio Mogno, Domenico Serpella, Angela Palmitessa and Daniela Milani. The authors thank Mrs. Barbara Wade for her helpful suggestions during the English editing of the manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Costa, P., Peretta, P. & Faccani, G. Relevance of intraoperative D wave in spine and spinal cord surgeries. Eur Spine J 22, 840–848 (2013). https://doi.org/10.1007/s00586-012-2576-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2576-5