Abstract
Purpose
To compare the 9-year outcome in patients with chronic low back pain treated by instrumented lumbar fusion versus cognitive intervention and exercises.
Methods
The main outcome measure was the Oswestry Disability Index (ODI). Secondary outcome measures included pain, fear-avoidance beliefs, trunk muscle strength, medication, and return to work.
Results
One-third of the patients randomized to cognitive intervention and exercises had crossed over and been operated and one-third of the patients allocated to lumbar fusion had been re-operated. The intention-to-treat analysis detected no differences between the two groups. The mean adjusted treatment effect for ODI was 1.9 (95 % CI −7.8 to 11.6). Analysed according to the treatment received, more operated patients used pain medication and were out of work.
Conclusions
The outcome at 9 years was not different between instrumented lumbar fusion and cognitive intervention and exercises.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The use of surgery for treatment of non-specific low back pain has increased considerably over the past two decades [1]. Four randomized trials have compared instrumented lumbar fusion with conservative treatment [2–5]. Fritzell et al. [2] reported that patients randomized to lumbar fusion had improved back-specific disability at 2-year follow-up compared to patients who received unstructured community care. No difference has been reported in the trials comparing lumbar fusion and cognitive behavioural intervention after 1- or 4-year follow-up [3–6]. In a recent cohort study of workers operated with lumbar fusion, it was reported that the re-operation rate was 25 %, opioid use 76 %, and return to work only 26 % [7]. Similar results were described by Brox et al. [6] in a 4-year follow-up study.
The main objective of the present study was to compare primary and secondary outcome measures in patients randomized to lumbar fusion or cognitive intervention and exercises 9 years following treatment. The evaluation had a specific focus on the number of patients who changed treatment group (crossover), had re-operations, returned to work, and used pain medication.
Methods
Study design
The present study is a 9-year follow-up of two randomized controlled trials conducted to compare instrumented lumbar fusion and cognitive intervention and exercises for chronic low back pain (CLBP) [3, 5]. The two studies were merged before the 4-year follow-up [6].
Patients
During the period 1997–2000, patients with CLBP were recruited from the department of orthopaedic surgery, neurosurgery, and physical medicine and rehabilitation from all regions of Norway. Clinicians at the referral hospitals performed a brief examination of patients with respect to inclusion and exclusion criteria and informed eligible patients about the trial. All patients underwent plain radiography; in addition, most of the patients had computer tomography (CT) or magnetic resonance (MRI) at inclusion. A research physiotherapist coordinated the study and verified eligibility.
The criteria for inclusion at baseline were patients aged 25–60 years, with reported low back pain for at least 1 year, a score of 30 out of 100 points on the Oswestry Disability Index (ODI) [8], and degenerative changes at the L4–L5 and/or L5–S1 on plain radiographs. One of the merged studies excluded patients with previous disc surgery [3], while the other did not [5]. The criteria for exclusion included widespread myofascial pain, spinal stenosis with reduced walking distance and neurologic signs, disc herniation or lateral recess stenosis with clinical signs of radiculopathy, inflammatory disease, previous spinal fracture, the pelvic girdle syndrome, generalized degenerative changes on plain radiograph examination, serious somatic or psychiatric disease that excluded either one or both treatment alternatives, registered medical abuse, or reluctance to accept one or both of the treatment regimens of the study. All eligible patients were given oral and written information about the study and the two interventions.
Patients were re-contacted by mail and invited to participate in the long-term follow-up study. The Ethics Committee for Medical Research in health region I of Norway approved the study.
Outcome measures
The primary outcome measure was the Norwegian version of the original ODI (version 1.0) to evaluate condition-specific disability and pain [8, 9]. This score has ten questions about pain and disability and ranges from 0 % (no pain and disability) to 100 % (worst possible pain and disability). Measurement error in a single patient is 12 % [10–13].
Secondary outcome measures included back and leg pain [2], global back disability question for the assessment of patients’ overall rating [10], fear-avoidance beliefs for physical activity (FABQ-PA), [14], life satisfaction [15], fingertip–floor distance [16], isokinetic trunk muscle strength [17], complications, crossover and re-operation, use of pain medication and work status. Return to work included full-time and part-time work.
The following additional questions were included at the 9-year follow-up: Are your back problems better after compared to before the treatment? It had two response alternatives: yes/no; How satisfied are you with the treatment for your back problem? It had five response alternatives: very satisfied, satisfied, neither satisfied nor dissatisfied, dissatisfied, and very dissatisfied; and questions about treatment taken after the last follow-up. Additional surgery was verified from medical records. An experienced physiotherapist, who had conducted the tests both at baseline and at 1-year follow-up, supervised the tests of isokinetic trunk muscle strength [17, 18].
At long-term follow-up, the patients were examined by a specialist in physical medicine and rehabilitation (AF) and a physiotherapist (IH). None of them were engaged in the treatment of patients.
Randomization
The randomization procedure has been described previously [3, 5, 6]. Treatments were started within 3 months after randomization.
Treatments
Lumbar fusion consisted of posterolateral autologous bone transplantation and transpedicular screw fixation of the L4–L5 and/or L5–S1 segments. Physiotherapists at the respective departments provided advice about recommended daily activities during the first 3 months after surgery. The surgeons conducted follow-up consultations with each patient at 3 and 6 months and prescribed physiotherapy, including exercises. Information about content and compliance of postoperative physiotherapy in the lumbar fusion group after discharge from hospital are based on a standardized question answered by the patients at the 1-year follow-up. After discharge from the hospital or the patient’s hotel, the lumbar fusion group had a median number of 32 physiotherapy sessions during the first year.
The cognitive intervention and exercises programme has been previously described [3, 5]. It included 1 week at the outpatient clinic, 2 weeks at home, followed by 2 weeks at the outpatient clinic. The programme was conducted by physiotherapists and a specialist in physical medicine and rehabilitation. Patients were divided into treatment groups consisting of four to seven patients. Three daily workouts were performed: aerobics or outdoors activities, water gymnastics, and individual or group exercises. The intensity of the physical activities was gradually increased during the last 2 weeks. The average duration of the rehabilitation programme was 25 h per week. Patients were challenged in their thoughts about, and participation in, physical activities previously labelled as not recommended including jumping, lifting, and ball games. The essential message in the cognitive intervention was that the patients could not do any harm to their back by participating in daily activities (i.e. vacuum cleaning, ironing, gardening, etc.). Endurance and coordination exercises were recommended, not necessarily with the goal of increasing aerobic capacity and trunk muscle strength, but to allow the patients to gain confidence towards engaging in ordinary activities of daily life. Individual goals for the rehabilitation process were established based on the patients’ answers to a comprehensive questionnaire (thoughts and feelings) and their test results (physical function and behaviour). After the programme was fulfilled, the cognitive intervention and exercise group had a median of zero physiotherapy sessions during the first year.
Statistical analysis
Estimation of sample size has been reported previously [3, 5]. Results were analysed both with an intention-to-treat- and with an as-treated approach. Linear regression (ANCOVA) with adjustments for gender, age, fusion, previous discectomy, and baseline scores was used to detect treatment effects between interventions at 9 years. Mean adjusted differences between groups (95 % CI) in those who attended the long-term follow-up are reported. A mixed between-within subjects analysis of variance (SPANOVA) was conducted to compare the time course for primary and secondary outcome measures in both treatment groups. Scores for ODI and back pain were assessed across four time periods: at baseline, and 1-, 4-, and 9-year follow-up. Ordered variables were analysed with a Mann–Whitney U test. Categorical variables (patients’ overall rating, work, and medication) were dichotomized and χ2 tests were conducted to compare differences between the two groups. Logistic regression, with adjustments for age, gender, lumbar fusion, previous discectomy, and baseline scores, was used to calculate OR (95 % CI). Analyses were carried out with the use of SPSS software, version 18.0.
Results
Patients
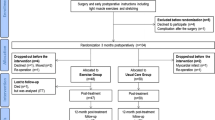
The recruitment and follow-up of study participants are shown in Fig. 1. Of 124 patients included at baseline, 99 (80 %) attended the long-term follow-up: 55 randomized to lumbar fusion and 44 to cognitive intervention and exercises. In the surgical group, 90 % had undergone surgery at 9 years, and the corresponding number for the cognitive intervention and exercise group was 31 %.
Return to work and health-care utilization
Nineteen (35 %) of the patients randomized to lumbar fusion were working full- or part time at long-term follow-up, compared to 16 (36 %) in the cognitive intervention and exercises group (p = 0.85). Thirty-five (64 %) patients in the lumbar fusion group were out of work compared to 26 (59 %) in the cognitive intervention and exercise group (p = 0.53). Nineteen (35 %) patients randomized to lumbar fusion reported that they had visited a physician and 14 (25 %) had received physiotherapy the year before the 9-year follow-up. In the cognitive intervention and exercise group, 19 (43 %) reported visits to a physician and 13 (30 %) had received physiotherapy.
Dropout rate, crossover, complications, and re-operations
Patients who did not attend the 9-year follow-up were not different from dropouts at baseline or the latest follow-up before 9 years (Tables 1, 2). Three patients randomized to fusion crossed over and had cognitive intervention and exercises after 1-year follow-up. At the 4-year follow-up, 60/66 patients had undergone surgery and 15/60 had undergone re-surgery. Between 4 and 9 years, the implant was removed in four patients in the surgical group, resulting in re-operation in 19/60 patients.
Three of the 58 patients randomized to cognitive intervention and exercises did not have the allocated treatment. At the 4-year follow-up, 14/58 patients had undergone surgery and 4 patients had re-surgery. Four patients were operated between 4 and 9 years: two for spinal stenosis; one had disc prosthesis for recurrent pain; one patient, who did not have the allocated intervention, had instruments removed. A total of 18/58 patients had operation (Fig. 1). The reasons for re-operations were removal of instrumentation because of persistent pain. There were no infections.
Main treatment effects
The adjusted treatment effect for ODI between fusion and cognitive intervention and exercises was 1.9 (−7.8 to 11.6) (Table 3). Figure 2 shows the ODI score from baseline to long-term follow-up. There was no significant interaction between intervention and time. There was a substantial main effect for time, Wilks λ = 0.50, F (3.93) = 31.2; p < 0.001, partial η2 = 0.50, with both groups showing a reduction in ODI score from baseline to long-term follow-up. There was a reduction in ODI score within both groups from 4- to 9-year follow-up (p < 0.05). The main effect comparing the two treatments from 4- to 9-year follow-up was not significant.
Secondary outcome
Secondary outcomes were not significantly different between lumbar fusion and cognitive intervention and exercises at 9-year follow-up (Table 3).
Both groups reported significantly (p < 0.01) less back and leg pain, less fear-avoidance beliefs, less emotional distress, and improved general function score at 9 years compared to baseline. No differences between the two groups were found for overall rating and satisfaction with treatment results.
Sensitivity analyses
Sixty-three of the patients attending the 9-year follow-up had been operated and 36 were not operated. More operated patients (68 vs. 42 %) were out of work at the 9-year follow-up compared to those who had cognitive intervention and exercises and were not operated (adjusted OR 3.0; 95 % CI 1.3–7.4, p = 0.013). Pain medication was taken daily or weekly by 44 % treated by lumbar fusion versus 17 % of the patients in the cognitive intervention and exercise group (adjusted OR 4.0; 95 % CI 1.5–11.0; p = 0.005).
More operated patients reported that their back problems were better compared to pre-treatment (adjusted OR 2.8; CI 1.2–6.5, p = 0.02) (Table 4).
Seventeen percent were dissatisfied after surgery compared with 3 % in the cognitive intervention and exercise group (p = 0.03).
Discussion
There were no differences in primary or secondary outcomes at the 9-year follow-up between patients randomized to lumbar fusion or cognitive intervention and exercises. The long-term results are largely consistent with previously reported results at 1- and 4-year follow-up [3, 5, 6].
A difference in return to work in favour of the cognitive intervention and exercises was found in the as-treated analysis. This is in agreement with the results from Nguyen et al. [7], who in a large cohort study showed that patients on worker’s compensation, who had undergone lumbar fusion, had significantly higher permanent disability rates compared to non-operated controls randomly selected from the same database. Return to work (RTW) is an important outcome when treating CLBP patients, because RTW is an objective personal health outcome. Multiple studies have shown that being out of work is associated with poor health [7]. There may be different explanations for the higher disability rate in the operated patients, but our interpretation is that disability pension may be easier to achieve when operated, because the claim adjuster may consider lumbar fusion to represent the end stage of treatment. We can, however, not conclude that fusion is inferior to cognitive intervention and exercises for return to work, because results in the intention-to-treat analyses were not significant.
The as-treated analysis in the present study showed that patients operated with lumbar fusion have an increased and higher use of pain medication (opioids) compared to patients who were not operated. These findings are in accordance with previous published studies [7, 19]. One possible explanation for this increased use of medication may be that patients have persistent, disabling low back pain for years in spite of the surgery [19]. The operated patients may experience more pain because of the surgical procedures through disruption of anatomy and biomechanics, leading to flat-back syndrome or adjacent level degeneration, kyphosis, or scoliosis [20], or they may have been habituated to addictive medication. No difference between groups was found in the intention-to-treat analysis, which makes a conclusion about the cause for the observed medication consumption in the operated patients difficult.
There are limitations to the present study. One-third of the patients allocated to the cognitive intervention and exercise group crossed over and were operated after the 1-year follow-up.
The high number of crossover patients and the patients who did not attend long-term follow-up make a firm scientific conclusion about results at 9 years difficult, but on comparing the last observed data of those who did not attend the 9-year follow-up with those who attended we found only minor differences between the randomized groups suggesting that analyses at 9 years were not biased.
The study has been criticised for lack of power to detect important clinical differences [21, 22]. Nevertheless, the study had enough power to detect significant differences for secondary outcomes at the 1- and 4-year follow-up [3, 5, 6]. The observed difference for the primary outcome is much smaller than the study was designed to detect, although the upper 95 % confidence level is about the size of minimal clinically important difference (MCID).
The main strength of the present study is that this is the first long-term follow-up of a randomized trial to compare lumbar fusion and non-operative treatment in non-specific or degenerative CLBP. The primary and secondary outcomes of the present study are validated and the follow-up rate is relatively high for long-term follow-up, with 80 % attendance.
In conclusion, patients randomized to lumbar fusion did not report better long-term outcome compared to cognitive intervention and exercises. Both randomized groups reported less pain and better function at 9 years compared to baseline (and 1-year follow-up), but more operated patients used pain medication and were out of work. However, more patients operated reported that they were better than before surgery.
References
Cowan JA Jr, Dimick JB, Wainess R et al (2006) Changes in the utilization of spinal fusion in the United States. Neurosurgery 59:15–20
Fritzell P, Hagg O, Wessberg P et al (2001) 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine 26:2521–2532
Brox JI, Sorensen R, Friis A et al (2003) Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine 28:1913–1921
Fairbank J, Frost H, Wilson-MacDonald J et al (2005) Randomised controlled trial to compare surgical stabilisation of the lumbar spine with an intensive rehabilitation programme for patients with chronic low back pain: the MRC Spine Stabilisation Trial. BMJ 330:1233–1239
Brox JI, Reikeras O, Nygaard O et al (2006) Lumbar instrumented fusion compared with cognitive intervention and exercises in patients with chronic back pain after previous surgery for disc herniation: a prospective randomized controlled study. Pain 122:145–155
Brox JI, Nygaard OP, Holm I et al (2010) Four-year follow-up of surgical versus non-surgical therapy for chronic low back pain. Ann Rheum Dis 69:1643–1648
Nguyen TH, Randolph DC, Talmage J et al (2011) Long-term outcomes of lumbar fusion among workers’ compensation subjects: a historical cohort study. Spine 36:320–331
Fairbank JC, Couper J, Davies JB et al (1980) The Oswestry Low Back Pain Disability Questionnaire. Physiotherapy 66:271–273
Grotle M, Brox JI, Vollestad NK (2003) Cross-cultural adaptation of the Norwegian versions of the Roland–Morris Disability Questionnaire and the Oswestry Disability Index. J Rehabil Med 35:241–247
Holm I, Friis A, Storheim K et al (2003) Measuring self-reported functional status and pain in patients with chronic low back pain by postal questionnaires: a reliability study. Spine 28:828–833
Hagg O, Fritzell P, Romberg K et al (2001) The General Function Score: a useful tool for measurement of physical disability. Validity and reliability. Eur Spine J 10:203–210
Grotle M, Vollestad NK, Veierod MB et al (2004) Fear-avoidance beliefs and distress in relation to disability in acute and chronic low back pain. Pain 112:343–352
Grotle M, Brox JI, Vollestad NK (2004) Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine 29:E492–E501
Waddell G, Newton M, Henderson I et al (1993) A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 52:157–168
Andrews FM, Robinson JP, Shaver PR et al. (1991) Measures of subjective well-being. Measures of personality and social psychological attitudes. Academic Press, San Diego
Hyytiainen K, Salminen JJ, Suvitie T et al (1991) Reproducibility of nine tests to measure spinal mobility and trunk muscle strength. Scand J Rehabil Med 23:3–10
Keller A, Hellesnes J, Brox JI (2001) Reliability of the isokinetic trunk extensor test, Biering–Sorensen test, and Astrand bicycle test: assessment of intraclass correlation coefficient and critical difference in patients with chronic low back pain and healthy individuals. Spine 26:771–777
Karatas GK, Gogus F, Meray J (2002) Reliability of isokinetic trunk muscle strength measurement. Am J Phys Med Rehabil 81:79–85
Crisostomo RA, Schmidt JE, Hooten WM et al (2008) Withdrawal of analgesic medication for chronic low-back pain patients: improvement in outcomes of multidisciplinary rehabilitation regardless of surgical history. Am J Phys Med Rehabil 87:527–536
Diwan AD, Parvartaneni H, Cammisa F (2003) Failed degenerative lumbar spine surgery. Orthop Clin North Am 34:309–324
Hagg O, Fritzell P (2003) Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine 28:1913–1921
Brox JI, Sorensen R, Friis A et al (2004) Re: Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine 29:1160–1161
Acknowledgments
The long-term follow-up study was funded by the Research Council of Norway.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Froholdt, A., Reikeraas, O., Holm, I. et al. No difference in 9-year outcome in CLBP patients randomized to lumbar fusion versus cognitive intervention and exercises. Eur Spine J 21, 2531–2538 (2012). https://doi.org/10.1007/s00586-012-2382-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2382-0