Abstract
Purpose
The purpose is to study rates, trends, geographic variations and outcome of lumbar spine surgery in the Belgian population during the last decade.
Methods
This is a retrospective cohort study using administrative data of the largest Belgian sickness fund from January 1, 2000 through December 31, 2009. Cases included lumbar laminectomy, combined discectomy and fusion, posterior interarticular fusion, anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF) and standard discectomy. The main outcome measures were age- and sex-adjusted rates of lumbar spine surgery, 1-year mortality, 1-year iterative surgery, no return to work (RTW) rate 1 year after surgery and length of hospital stay. Multivariate logistic regression analysis was used to determine the association between age, sex, geographic region, type of surgery, year of intervention and duration of pre-operative sick leave on outcome.
Results
Spine surgery rates rose 44 % from 2001 through 2009 and data for 2009 showed twofold variations in spine surgery rates among 10 Belgian provinces. Reported 1-year mortality varied from 0.6 to 2.5 % among surgical procedures performed in 2008. The overall 5-year reoperation rate was 12 %. RTW rates 1 year after standard discectomy, ALIF, PLIF and combined discectomy and fusion for the follow-up sample of 2008 were 14.4, 22.7, 26.1 and 30.6 %, respectively. The median length of hospital stay significantly decreased throughout the decade. Type of surgery and geographic region were significantly related to patient outcomes.
Conclusions
Regional variations highlight professional uncertainty and controversy. The study results point to the need for peer comparisons and surgeon feedback.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 85–90 % of all individuals suffering from low back pain (LBP) no precise structure or systemic disease, infection, injury or trauma could be identified causing the pain. Standard treatment for this so-called nonspecific lower-back pain when lasting between 0 and 12 weeks is essentially conservative and includes self-care with over-the-counter medication and maintaining activity as tolerated in the acute phase and a graded activity program and cognitive-behavioral treatment during the sub-acute phase. In cases of chronic nonspecific lower-back pain due to degenerative disc disease based on provocative discography there is moderate evidence that surgery is as effective as intensive rehabilitation with a cognitive-behavioral emphasis [1, 2].
In the few patients suffering from specific lower-back pain due to disc prolapse or spinal stenosis, nerve root pain usually represents about 5 % of the pain [3]. Several randomized trials have compared surgery with conservative treatment [1, 4]. For radiculopathy with herniated lumbar disc, there is inconsistent evidence that open discectomy and microdiscectomy are superior to non-surgical therapy for long-term improvement in pain and function [4]. A randomized controlled trial demonstrated that 1-year outcomes for patients assigned to early surgery and those assigned to conservative treatment were similar except for pain relief and perceived recovery, which were faster following surgery [5]. For spinal stenosis with or without degenerative spondylolisthesis, there is good evidence that decompressive laminectomy is moderately superior to non-surgical therapy for improvement in pain and function through 1 to 2 years [4].
As a general rule, standard treatment for low back pain is essentially conservative in the absence of red flags [6, 7]. When medical management fails, spinal surgery is often performed despite its non-proven superiority [1, 7]. United States Medicare claims analysis has shown that lumbar spine surgery rates rose during the 1980s and between 1990 and 2003, which revealed tripling spinal fusion rates. Population-based research had clearly demonstrated variations in proportion of spinal surgery across regions and subsequent geographic variations in outcome [8–10]. Regional variability is a hallmark of scientific uncertainty about the likely outcomes of spinal surgery. The internationally rising trend in spinal surgery despite constant LBP diagnosis rate and the wide US geographic variation in spinal surgery at least suggests that patients are not receiving appropriate care based on conventional wisdom. If that trend in more expensive clinical management of low back pain patients translates in devastating outcomes is not clear.
The objectives of the present study were both to examine recent trends of spinal surgery in Belgium and how it aligns with current international practice and to compare low back pain surgery in different geographic areas of the kingdom. An additional purpose was to determine the outcome of spinal surgery through a decade’s experience.
Patients and methods
Setting
Belgium has a compulsory health insurance system with universal coverage organized through private non-profit sickness funds. The law requires inhabitants to join a sickness fund using a free choice enrolment model. Approximately, 42 % of the entire Belgian population is legally insured through the Alliance of Christian Sickness Funds.
Data sources
All inpatient and disability claim files came from the administrative database of the Alliance of Christian Sickness Funds for all beneficiaries who underwent spinal surgery from January 1, 2001 through December 31, 2009. This database covers discharges from all hospitals where enrollees have been treated. The inpatient files contain beneficiary demographic data, dates of death, intervention procedure, admission date, discharge data and enrollment information. Patient demographic characteristics included age, sex and state of residence. The disability claim files contain all sick leave periods for 100 % of Christian Sickness Fund beneficiaries who were employed prior to spine surgery. The reimbursement database from the Alliance of Christian Sickness Funds is perceived to be reliable and accurate since it is subjected to audit by two independent supervisory agents.
Case selection
We studied lumbar spinal surgery. Data were retrieved using the Belgian nomenclature. This is a numerically encoded official fee schedule encompassing different medical acts and their accompanying reimbursement rate. Preliminary analysis of the Alliance of Christian Sickness Fund claims database showed that the top six most common procedures were lumbar laminectomy (nomenclature code 232805), combined discectomy and fusion (nomenclature code 281805), posterior interarticular fusion (nomenclature code 281643), anterior lumbar interbody fusion (ALIF) (nomenclature code 281665), posterior lumbar interbody fusion (PLIF) (nomenclature code 281680) and standard discectomy (nomenclature code 281783). We used the six nomenclature codes (232805, 281865, 281643, 281665, 281680, 281783) to identify cases from the medical bill payments database. The Belgian nomenclature is essentially procedure based and does not encompass International Classification of Disease (ICD-9) codes. Appropriate diagnoses were not available unless they were included in the description of a specific surgical procedure. The available codes do not indicate more detail about these procedures such as numbers of levels operated on and use of microsurgical techniques. We assigned each beneficiary to one of nine provinces according to zip code of residence, regardless of where they were hospitalized.
Analysis
The methodology and presentation were inspired by Patel et al. [11] who investigated the geographic variation in carotid revascularization. Surgery rates were analyzed using procedure counts as the numerator and the total number of beneficiaries as the denominator. Rates for 2001–2009 were standardized age- and sex-adjusted to the 2000 Christian Sickness Fund enrollees who cover 42 % of the compulsory insured population in Belgium. Return to work (RTW) was defined as resumption of full time activity within 1 year after surgery. We identified mortality as any death occurring within 1 year after surgery. A reoperation was counted if a second back operation was performed on the same individual during 1 year after initial surgical intervention.
Of the cases identified, no were excluded or had missing data. Aside from age, data were not normally distributed. Logistic regression makes no assumption about the distribution of independent variables and was therefore chosen to predict predefined discrete outcomes. A simultaneous entry logistic regression was performed to determine the magnitude of association of the independent variables with 1-year mortality, 1-year iterative surgery and 1 year return to work. Multivariate logistic regression was used to compare selected outcomes after adjusting for the following potential confounding factors: age, gender, year when surgery was performed, type of surgery and provincial region. One-year return to work was also adjusted for length of sick leave before surgery. The adjusted odds ratios (ORs) and 95 % confidence intervals for the significant predictors were reported from the multivariate models adjusting for all the above-mentioned covariates. When considering geographic variation cases were attributed to the province of residence at the time of operation. All analyses were performed using SPSS software version 17.0. P < 0.05 is considered to be statistically significant.
Results
A total of 73,393 beneficiaries underwent lumbar spinal surgery from 2001 through 2009. The study subjects had a mean age of 52.7 years and 49.8 % were women. Mean age was the highest among beneficiaries who underwent decompressive laminectomy (63 years) and the lowest in claimants who had ALIF (45 years). Table 1 shows the lumbar spinal surgery rates in this patient sample. The most common surgical intervention was standard discectomy followed by lumbar laminectomy. The overall rate of spinal surgery in Belgium increased from 16.2 in 2000 to 23.3 in 2009. During the 10-year study interval, standard discectomy rate increased minimally, from 9.6 to 10.6 per 10,000 enrollees. The rate of PLIF rose slightly during this period from 1.4 to 2.0 per 10,000 beneficiaries. We also found a 50 % increase in combined discectomy and fusion, and a nearly doubling of the rates of ALIF and lumbar laminectomy. This made ALIF and lumbar laminectomy one of the most rapidly increasing forms of spinal surgery in Belgium. The proportion of patients having spine fusion changed little from 20 % in 2000 to 22 % in 2009.
Low back surgery rates among residents in the ten provinces of Belgium are presented in Fig. 1. Substantial geographic variation was seen in the age-adjusted rates of spinal surgery in the 2009 period, with a nearly twofold difference between the highest ratio of provincial rate of lumbar spine surgery to the Alliance of Christian Sickness Fund population average (1.41 in West Flanders) and the lowest rate (0.69 in Liege). Apart from Luxembourg, rates in the predominantly French-speaking southern region of Belgium were below the Dutch-speaking region of Flanders in the north.
Variations in the use of posterior interarticular fusion, ALIF, PLIF and combined discectomy and fusion were significantly more pronounced than for standard discectomy and lumbar laminectomy over the studied period. Rates of ALIF and PLIF varied approximately twofold among geographic areas whereas rates of posterior interarticular fusion and combined discectomy and fusion varied threefold. The coefficient of variation in surgery rates was similar when comparing total hip arthroplasty (21.3) with standard discectomy (25.6) and laminectomy (26.2) and below the magnitude of variability in rates of fusion (at least 55.1) in accordance with the results of Weinstein et al. [12].
Table 2 shows the factors associated with the use of types of spinal surgery. Lumbar laminectomy was performed more often in older patients. More female underwent ALIF, PLIF and combined discectomy and fusion. Posterior interarticular fusion is less likely to be used in Antwerp whereas ALIF was more likely to occur in East Flanders. Standard discectomy was more likely to be used in Liege at the expense of PLIF. Combined discectomy and fusion and decompressive laminectomy is likely to be more popular in Antwerp. Lumbar laminectomy, posterior interarticular fusion and ALIF were statistically significantly gaining interest in the course of the last decade in disfavor of standard discectomy.
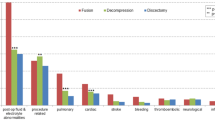
One-year postoperative mortality for patients who underwent spinal surgery in 2008 was almost twice as high among patients undergoing fusions as in patients undergoing standard discectomy (Table 3). There were no statistically significant differences in mortality over the studied decade.
After 5 years of follow-up 12 % of patients with a surgery in 2000 had a second back operation. Standard discectomy showed the highest iterative surgery rate. The hospital length of stay significantly decreased over the studied decade. The median hospital length of stay for patients undergoing lumbar laminectomy was almost 50 % shorter over the studied decade.
In 2008, 20.5 % of the patients were unable to resume work 1 year after surgery. In comparing surgical interventions we found spinal fusion leading to substantially lower rates of return to work in contrast to standard discectomy. Over a decade unadjusted outcomes with regard to return to work showed only improvement for ALIF and PLIF.
Tables 4, 5 and 6 depict the results of a multiple logistic regression analysis of the presurgical variables on mortality, RTW and reiterative surgery. Mortality within 1 year after surgery was more likely in case of older age at the time of surgery, male gender, posterior interarticular fusion, combined discectomy and fusion and for patients who resided in Liege or Hainaut. Younger age, male gender and posterior articular fusion were statistically significant factors associated with iterative surgery. Reoperation was more likely for patients domiciled in Antwerp and East Flanders. Length of sick leave before surgery was the most important factor that correlated with poor work resumption. Older age, female gender, posterior interarticular fusion and combined discectomy and fusion were other significant factors associated with no return to work 1 year after surgery. Return to work was more likely after ALIF and standard discectomy. The significantly poorest RTW rates were observed in descending order in Hainaut (69.3 %), Liege (73.3 %) and West Flanders (78.9 %). East Flanders (83.0 %) and Antwerp (82.7 %) enjoyed the best RTW rates. RTW rates were significantly higher in the second half of the observed decade.
Discussion
Overall, spinal surgery rates in Belgium have continued to rise gradually from 2001 through 2010. There was a sharp increase in laminectomy, combined discectomy and fusion, posterior interarticular fusion, ALIF and PLIF despite lacking evidence of an increasing prevalence of spinal disease in the global population. Conversely, the proportion of standard discectomy remained fairly stable. These findings corroborate with the United States trends [8, 13, 14]. Previous research suggests that these changes were related, at least in part to the technologic innovation and marketing. The Swedish Spine Register demonstrates the increasing trend in spinal stenosis surgery over the last 10 years, which is in line with the rise in decompressive laminectomy in Belgium [15]. Both demand factors including an ageing population structure and supply factors including the density of spine surgeons provide explanations for the rise in spinal surgery procedures in Belgium. Since 2000, the number of neurosurgeons per capita has substantially increased rising by nearly 51 % (from 10.8 per 1,000.000 population in 2000 to 16.3 in 2010) [16]. Orthopedist density grew at a rate of 18 % over a decade, rising from 778 physicians per 1,000.000 population to 917. Health care systems like Belgium based on a fee-for-service payment model rather than on capitation or managed care may allow healthcare professionals to maximize healthcare claims and may further add to the rise in surgery rates.
This analysis documents important trends and provincial variations in the management of low back disorders in Belgium. Fusion rates are more variable than overall rates of spine surgery and crude spine surgery rates are the highest in the northern part of Belgium. Because all rates were standardized to the 2000 Sickness fund population, variations cannot be attributed to differences in age distributions or changes in population size. In comparison with orthopedic procedures, back surgery especially spinal fusion surgery varies substantially among geographic areas. It has been suggested that overall spine surgeon density, individual surgeons’ backgrounds like age and spine surgery training or experience and patient factors including age, lifestyle, patient expectations, insurance status and overall health status contribute to this variation [8–10, 14, 17]. These findings suggest a poor consensus on the appropriate indications for spinal surgery and that surgery may be over- or underused in some areas. Additional reasons that explain regional variations in the number of spine surgery procedures are differences in coding and reporting. The influx of patients from abroad to some neighboring Belgian provinces further contribute to the intra and inter-country variations in spine surgery rates [18]. Variations by a factor of two or more across geographic areas are of clinical concern. It is hypothesized that differences in clinical philosophy between the northern and southern part of Belgium largely account for the variation in rates. Interpretation differences of available literature and inadequate dissemination of scientific information may further affect surgical approach. This opens perspectives for third party payers. Sickness funds may assist in clinician education in close cooperation with local opinion leaders by providing a performance feedback to increase compliance with beneficial low back pain therapies as outlined in the available guidelines.
Mortality rates were higher for fusion than for standard discectomy and increased steadily with older age. These findings are generally consistent with a review by Deyo et al. [8]. Our overall mortality rates are comparable to those found by Street et al. [19] and in agreement with a systematic review of the literature reporting mortality rates for cervical spine and lumbar spine surgery <1 %. In disagreement with Malter et al. [20] we demonstrated that fusion especially PLIF was associated with lower rates of iterative surgery than decompression alone. Reoperation rates after decompressive surgical procedures are reported to range from 6 to 23 % and are well above our findings which corroborate fairly well with the range of repeat surgery after lumbar decompression for herniated disc (4.3 to 10.5 %) reported by Martin et al. [21, 22]. Median hospital length of stay for lumbar fusion in 2000 was higher than reported data from the US [10, 23]. However there was a significant declining trend in hospital stay for all surgical procedures.
Our analysis revealed a significant variation in RTW rate among patients who had decompression surgery, lumbar spinal fusion and standard discectomy. Claimants who underwent a less invasive procedure with a shorter recovery period such as standard discectomy were more likely to return to work than patients undergoing fusions. Spinal fusion is a more complicated procedure because it involves bone grafting with or without internal fixation devices resulting in a larger dissection and a longer operating time [20, 24, 25]. Return to work status after standard discectomy was in line with the Spine Patient Outcomes Research Trial (SPORT) and substantially above the 64 % return to work found by Veresciagina et al. [26, 27]. Multivariate analysis indicated that geographic region was an important factor associated with RTW following spine surgery. These results corroborate with the previously reported geographic region variations in outcome for lumbar spine surgeries [10]. Our data showed an interregional variety in spine surgery and return to work rates between the Dutch-speaking northern part of Belgium (Flanders) and the French-speaking southern part (Wallonia). These results are in line with a population-based survey on Belgian adults that clearly demonstrated that low back pain frequency, health beliefs, and socio-cultural factors influence health care behaviors and utilization in a society with equal access to high-quality medical care and under universal insurance coverage [28]. Our results further suggest that higher rates of surgery are not necessarily worse and that the lowest surgical rates may be associated with worse average outcomes. Prior European research based on Spine Tango, the international spine registry of Eurospine, the Spine Society of Europe reported 1 year good or excellent global outcome after surgery between 62 % (patient-rated) and 80 % (surgeon-rated) [29–31]. Outcome was measured by the Core Outcome Measures Index (COMI) questionnaire consisting of validated questions covering the domains of pain, function, symptom-specific well-being, general quality of life, and social and work disability. Detailed information on work disability was not available. The Spine Tango shows an overall functional improvement of about 60 % in all follow-ups equally distributed between Benelux, Scandinavia and German speaking groups [32].
It is worth noting that sick leave before surgery proved to be a stronger variable associated with low RTW rates than the type of spine surgery performed did. Den Boer et al. [33] found duration of sick leave a consistent predictor in a systematic review of bio-psychosocial risk factors for an unfavorable outcome after lumbar disc surgery. Long-term disabled claimants should be educated about their poor chances to resume work and be guided not to opt for surgery if professional reintegration is set as primary objective. In any way they need to be closely probed into the origins of the prior long-term disability before pursuing surgery [17]. Of particular note is the role of sickness funds in the secondary prevention of long-term work absence due to low back pain after the onset of symptoms. A randomized controlled trial showed that LBP patients who were provided information and advice by the medical advisers of the Alliance of Christian Sickness Fund experienced a significantly higher return to work rate due to a low relapse rate [34]. A practical screening tool to identify patients at risk of long-term sick leave may further enhance cost-effectiveness [35]. In case of severe relapsing low back pain despite conservative treatment and when surgery is perceived as an invaluable option, intervention needs to be performed without undue delay [36–38].
Our investigation has important strengths and weaknesses. The Belgian social security system offers a unique opportunity to conduct population-based outcome analyses. Equal access to high-quality medical care and freedom of choice by both patients and providers are the basic principles of the Belgian compulsory health insurance. Approximately 42 % of the entire Belgian population is legally insured through the Alliance of Christian Sickness Funds by free choice enrolment. Christian sickness fund coverage includes all provincial regions with a higher penetration rate in the northern part of Belgium (Flanders).The administrative claims data source is as such not subjected to participation or geographic bias. Mandatory sickness fund enrollment does not restrict freedom of choice of provider. Since all physicians are paid on a fee-for-service basis and, the data set completely captures their activities and is consequently also representative for Belgian health care providers. Sickness fund claims provide data for all beneficiaries undergoing surgery and represent the types of care that the majority of low back pain patients in Belgium likely receive and not just for selected patients or elite surgeons. However, the present retrospective study with administrative data did not allow us to identify the primary diagnoses so that patients with serious comorbid conditions that could result in misleading rates or mortality were also included. For the same reason, we could not demonstrate the well-known deleterious effects of litigation and psychosocial factors on surgical outcome.
In sum, our univariate and multivariate analyses highlight the potential over- or underutilization of low back treatments in some provinces of Belgium. A more consistent approach to clinical care is called for by educating spine surgeons more uniformly. To date, information regarding variations in practice is not widespread in Belgium. As important stakeholder in health care, sickness funds have the legal and moral duty to present the results of large database analyses to health care providers. Administrative database feedback may provide impetus to peer-review current practice against evidence- and consensus-based clinical guidelines. We strongly believe that physician knowledge of local practice patterns and peer comparisons are imperative in reducing geographic variations and bridging local quality gaps while covered by a nationwide social security system.
References
Nordin M, Balagué F, Cedraschi C (2006) Nonspecific lower-back pain: surgical versus nonsurgical treatment. Clin Orthop Relat Res 443:156–167. doi:10.1097/01.blo.0000198721.75976.d9
Vanwye WR (2010) Nonspecific low back pain: evaluation and treatment tips. J Fam Pract 59(8):445–448
Balagué F, Borenstein DG (1998) How to recognize and treat specific low back pain? Baillieres Clin Rheumatol 12(1):37–73
Chou R, Baisden J, Carragee EJ, Resnick DK, Shaffer WO, Loeser JD (2009) Surgery for low back pain: a review of the evidence for an American Pain Society Clinical Practice Guideline. Spine (Phila Pa 1976) 34(10):1094–1109. doi:10.1097/BRS.0b013e3181a105fc
Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, Thomeer RT, Koes BW (2007) Surgery versus prolonged conservative treatment for sciatica. N Engl J 356(22):2245–2256. doi:10.1056/NEJMoa064039
Duffy RL (2010) Low back pain: an approach to diagnosis and management. Prim Care 37(4):729–741. doi:10.1016/j.pop.2010.07.003
Bach SM, Holten KB (2009) Guideline update: what’s the best approach to acute low back pain? J Fam Pract 58(12):E1
Deyo RA, Mirza SK (2006) Trends and variations in the use of spine surgery. Clin Orthop Relat Res 443:139–146. doi:10.1097/01.blo.0000198726.62514.75
Irwin ZN, Hilibrand A, Gustavel M, McLain R, Shaffer W, Myers M, Glaser J, Hart RA (2005) Variation in surgical decision making for degenerative spinal disorders. Part I: lumbar spine. Spine (Phila Pa 1976) 30(19):2208–2213
Cook C, Santos GC, Lima R, Pietrobon R, Jacobs DO, Richardson W (2007) Geographic variation in lumbar fusion for degenerative disorders: 1990 to 2000. Spine J 7(5):552–557. doi:10.1016/j.spinee.2006.09.010
Patel MR, Greiner MA, DiMartino LD, Schulman KA, Duncan PW, Matchar DB, Curtis LH (2010) Geographic variation in carotid revascularization among Medicare beneficiaries, 2003–2006. Arch Intern Med 170(14):1218–1225. doi:10.1001/archinternmed.2010.194
Weinstein JN, Lurie JD, Olson PR, Bronner KK, Fisher ES (2006) United States’ trends and regional variations in lumbar spine surgery: 1992–2003. Spine (Phila Pa 1976) 31(23):2707–2714. doi:10.1097/01.brs.0000248132.15231.fe2
Maghout Juratli S, Franklin GM, Mirza SK, Wickizer TM, Fulton-Kehoe D (2006) Lumbar fusion outcomes in Washington State workers’ compensation. Spine (Phila Pa 1976) 31:2715–2723. doi:10.1097/01.brs.0000244589.13674.11
Taylor VM, Deyo RA, Cherkin DC, Kreuter W (1994) Low back pain hospitalization. Recent United States trends and regional variations. Spine (Phila Pa 1976) 19(11):1207–1212
Strömqvist B, Fritzell P, Hägg O, Jönsson B, Swedish Society of Spinal Surgeons (2009) The Swedish Spine Register: development, design and utility. Eur Spine J. 18:294–304. doi:10.1007/s00586-009-1043-4
Belgian National Institute for Health and Disability Insurance (2009). http://www.riziv.be/information/nl/statistics/health/2009/pdf/statisticshealth2009all.pdf. Accessed 27 July 2011
DeBerard, Masters KS, Colledge AL, Schleusener RL, Schlegel JD (2001) Outcomes of posterolateral lumbar fusion in Utah patients receiving workers’ compensation: a retrospective cohort study. Spine (Phila Pa 1976) 26(7):738–746. doi:10.1097/BRS.0b013e318226abf7
Arts MP, Peul WC, Koes BW, Thomeer RT, Leiden-The Hague Spine Intervention Prognostic Study (SIPS) Group (2008) Management of sciatica due to lumbar disc herniation in The Netherlands: a survey among spine surgeons. J Neurosurg Spin 9:32–39. doi:10.3171/SPI/2008/9/7/032
Street JT, Lenehan BJ, DiPaola CP, Boyd MD, Kwon BK, Paquette SJ, Dvorak MF, Rampersaud YR, Fisher CG (2012) Morbidity and mortality of major adult spinal surgery. A prospective cohort analysis of 942 consecutive patients. Spine J 12:22–34. doi:10.1016/j.spinee.2011.12.003
Malter AD, McNeney B, Loeser JD, Deyo RA (1998) 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 23(7):814–820
Sur YJ, Kong CG, Park JB (2011) Survivorship analysis of 150 consecutive patients with DIAM™ implantation for surgery of lumbar spinal stenosis and disc herniation. Eur Spine J 20:280–288. doi:10.1007/s00586-010-1599-z
Martin BI, Mirza SK, Flum DR, Wickizer TM, Heagerty PJ, Lenkoski AF, Deyo RA (2012) Repeat surgery after lumbar decompression for herniated disc: the quality implications of hospital and surgeon variation. Spine J 12:89–97. doi:10.1016/j.spinee.2011.11.010
Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ (1993) Lumbar spinal fusion. A cohort study of complications, reoperations, and resource use in the Medicare population. Spine (Phila Pa 1976) 18(11):1463–1470
Nguyen TH, Randolph DC, Talmage J, Succop P, Travis R (2011) Long-term outcomes of lumbar fusion among workers’ compensation subjects: a historical cohort study. Spine (Phila Pa 1976) 36(4):320–331. doi:10.1097/BRS.0b013e3181ccc220
Hodges SD, Humphreys SC, Eck JC, Covington LA, Harrom H (2001) Predicting factors of successful recovery from lumbar spine surgery among workers’ compensation patients. J Am Osteopath Assoc 101(2):78–83
Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, Herkowitz H, Fischgrund J, Cammisa FP, Albert T, Deyo RA (2006) Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA 296:2451–2459. doi:10.1001/jama.296.20.2451
Veresciagina K, Spakauskas B, Ambrozaitis KV (2010) Clinical outcomes of patients with lumbar disc herniation, selected for one-level open-discectomy and microdiscectomy. Eur Spine J 19:1450–1458. doi:10.1007/s00586-010-1431-9
Szpalski M, Nordin M, Skovron ML, Melot C, Cukier D (1995) Health care utilization for low back pain in Belgium. Influence of sociocultural factors and health beliefs. Spine (Phila Pa 1976) 20:431–442
Sobottke R, Aghayev E, Röder C, Eysel P, Delank SK, Zweig T (2012) Predictors of surgical, general and follow-up complications in lumbar spinal stenosis relative to patient age as emerged from the Spine Tango Registry. Eur Spine J 21:411–417. doi:10.1007/s00586-011-2016-y
Kleinstück FS, Grob D, Lattig F, Bartanusz V, Porchet F, Jeszenszky D, O’Riordan D, Mannion AF (2009) The influence of preoperative back pain on the outcome of lumbar decompression surgery. Spine (Phila Pa 1976) 34:1198–1203. doi:10.1097/BRS.0b013e31819fcf35
Kleinstueck FS, Fekete T, Jeszenszky D, Mannion AF, Grob D, Lattig F, Mutter U, Porchet F (2011) The outcome of decompression surgery for lumbar herniated disc is influenced by the level of concomitant preoperative low back pain. Eur Spine J 20(7):1166–1173. doi:10.1007/s00586-010-1670-9
EuroSpine, the spine society of Europe (2010). http://www.eurospine.org/cm_data/SSE_2010_Final_09.08.2011.pdf. Accessed 31 March 2012
den Boer JJ, Oostendorp RA, Beems T, Munneke M, Oerlemans M, Evers AW (2006) A systematic review of bio-psychosocial risk factors for an unfavourable outcome after lumbar disc surgery. Eur Spine J 15:527–536. doi:10.1007/s00586-005-0910-x
Du Bois MG, Donceel P (2012) Guiding low back claimants to work a randomized controlled trial. Spine (Phila Pa 1976) [Epub ahead of print] doi:10.1097/BRS.0b013e31824e4ada
Du Bois M, Donceel P (2008) A screening questionnaire to predict no return to work within 3 months for low back pain claimants. Eur Spine J 17:380–385. doi:10.1007/s00586-007-0567-8
Hägg O, Fritzell P, Ekselius L, Nordwall A, Swedish Lumbar Spine Study (2003) Predictors of outcome in fusion surgery for chronic low back pain. A report from the Swedish Lumbar Spine Study. Eur Spine J 12:22–33. doi:10.1007/s00586-002-0465-z
Herno A, Airaksinen O, Saari T, Svomalainen O (1996) Pre- and postoperative factors associated with return to work following surgery for lumbar spinal stenosis. Am J Ind Med 30:473–478. doi:10.1002/(SICI)1097-0274(199610)30:4<473:AID-AJIM13>3.0.CO;2-1
Rothoerl RD, Woertgen C, Brawanski A (2002) When should conservative treatment for lumbar disc herniation be ceased and surgery considered? Neurosurg Rev 25:162–165
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Du Bois, M., Szpalski, M. & Donceel, P. A decade’s experience in lumbar spine surgery in Belgium: sickness fund beneficiaries, 2000–2009. Eur Spine J 21, 2693–2703 (2012). https://doi.org/10.1007/s00586-012-2381-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2381-1