Abstract
Purpose
To identify potential prognostic factors predicting functional outcome and survival after surgery followed by radiotherapy for metastatic spinal cord compression due to solid tumors.
Methods
531 consecutive patients with metastatic epidural spinal cord compression (MESCC) were treated at our institution. Surgery followed by radiation therapy was performed in 151 patients (30%) with various histological diagnoses. Three different surgical procedures were performed: minimal resection with or without instrumented fixation, curettage, and total tumorectomy. Within 1 month after surgery, RT was performed, delivering a total dose of 30–36 Gy (3 Gy per fraction). Ten potential prognostic factors were investigated for relationship with functional outcome and survival.
Results
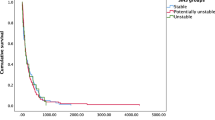
Clinical remission of pain was obtained in 91% of patients and 94 (62.5%) had recovery of neurological deficit. Recurrence in the same site of treatment occurred in nine (6%) patients. Median survival was 14 months (range 0–52 months); OS at 1, 2, and 3 years was 43.6, 37, and 21.5%, respectively. Survival was significantly associated with the histology of primary tumor (P < 0.001) and visceral metastases (P < 0.001) in the whole group; for histology, the prognostic factors statistically significant were other bone metastases in breast cancer, control of primary tumor, and the absence of visceral metastases in NSCLC and kind of surgery in the other.
Conclusions
The key element for successful treatment of MESCC is multidisciplinary care of the patient, which includes all of those prognostic factors that have been, until now, analyzed and compared. In our set of patients treated for vertebral metastases, PS, time to development of symptoms, and the presence of visceral metastases affected functional outcome and survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metastatic epidural spinal cord compression (MESCC) represents a major clinical problem adversely affects patient’s quality of life and outcome [1]. As many as 40% of cancer patients are diagnosed with spinal metastases. Although surgery combined with radiation therapy (RT) is more effective than radiation alone, surgical approach should be reserved for selected cases [2]. Many factors should be considered in the treatment of spinal metastatic lesions: patient’s general condition (age, comorbidity), status of disease (histological type of primary tumors, other metastatic sites), clinical status (back pain, neurological deficit, and stability of the spine), and life expectancy. An individual therapy should be chosen to provide the maximum palliative effect (reduction of pain, restoration of stability and function) with a minimum of operative morbidity and mortality [3]. Predicting survival is the key factor in selecting the proper treatment modality [4, 5]. Until now, current indications for surgery were the presence of progressive neurologic deficit not longer than 24 h, bone fragment in the spinal canal, instability of the spine due to pathological fracture, and life expectancy of at least 3 months, especially in cases of chemo- and radio-resistant tumors. In relation to the estimate of life expectancy to the types of vertebral lesions and to the objectives to be achieved, different surgical approaches are used: en bloc resection, corpectomy with reconstruction, debulking and stabilization, laminectomy for decompression, and percutaneous augmentation procedures [3, 6]. However, many patients with symptomatic spinal cord compression because of poor performance status and/or comorbidity are at high risk for surgical morbidity. Various assessment systems, above all surgical score, have been designed to predict survival time and to select the better treatment approaches [5–7]. We have retrospectively reviewed a set of our patients treated with surgery and radiotherapy for vertebral metastatic spinal compressive disease at our institution; the aim of this study was to identify potential prognostic factors predicting functional outcome and survival. Nine prognostic factors were investigated: sex, age, performance status (PS), according to ECOG Scale, time to development of symptoms from diagnosis, histotype of primary tumor, other sites of metastases, control of primary tumor, timing to tumor progression, previous therapy, and kind of surgery.
Materials and methods
From January 2004 to December 2007, 531 consecutive patients with MESCC were treated at our institution. Surgery followed by radiation therapy was performed in 151 patients (30%). Of these patients, 74 (49.0%) were women and 77 (51%) were men, with a median age of 62 years (range 22–76 years). The primary cancers were lung in 46 (30.5%), breast in 41 (27.1%), urologic in 29 (19.2%), gastrointestinal in 20 (13.3%), and other histology in 15 (9.9%). Three different surgical procedures were performed: minimal resection with or without instrumented fixation (palliative surgery) in 38 patients (38%), curettage (subtotal tumorectomy) in 91 (60.2%), and total tumorectomy (spondylectomy and vertebrectomy) in 22 (14.5%). The treated levels were cervical in 19 (12.5%), thoracic in 85 (56.0%), and lumbar in 35 (35%); in 12 (8.0%) surgery included the thoracolumbar junction. Radiotherapy was performed after surgery within the first month postoperatively (range 14–28 days) delivering a total dose of 30–36 Gy/10–12 fractions.
Results
Clinical remission of pain was obtained in 137 patients (91%) and recovery of neurological deficit in 94 (62.5%). Recurrence in the same site of treatment was observed in nine patients (6%), in eight of whom associated with distant tumor progression. The median survival time was 14 months (range 0–52 months), with a 1-year survival rate of 43.6%, 2-year survival rate of 37%, and 3-year survival rate of 21.5%. We conducted multivariate analysis on the data considered at the beginning to assess the significant correlation between our results. Upon multivariate analysis, the effect of combined treatment, surgery and radiotherapy, on functional outcome was significantly associated with performance status (PS) (P < 0.001) and time to development of symptoms from diagnosis (P < 0.002). Survival was significantly associated with the histology of primary tumor (P < 0.001) and the presence of visceral metastases (P < 0.001). In particular, in patients with breast cancer (41 patients), the median overall survival was 36 months (range 3–60 months). With a median observation time of 26 months (range 3–60 months), 18 patients (43.4%) are alive and 23 (56.6%) died. The 1-year survival rate was 70%, 2 years 60%, 3 years 42%, 4 and 5 years 34%. Survival was not related to age, time of evidence of metastases at diagnosis of primary tumor or subsequently. The only statistically significant factor affecting survival was the evidence of other bone (vertebral or other site) metastases. In this group of patients, the 1-, 2- and 3-year survival was 53.3% (vs. 100%) 46.7% (vs. 100%) and 19.4% (vs. 85.7%), respectively. According to the surgery type, all patients (8/8) treated with minimal resection died within a median time of 5 months; of 28 cases undergoing curettage, 12 (44.4%) are still alive at the last follow-up and 16 (55.6%) are dead. Among patients treated with total tumorectomy, 3/5 (66.7%) are alive at the last follow-up. This data suggest that in good performance patients, an aggressive treatment should be considered to afford a life expectancy prolongation, even if a statistical significance lacks. In patients with NSCLC (46 patients), median time of local progression was 8.5 months (range 3–23 months) and the median overall survival was 9 months (range 3–40 months). The 1-year survival rate was 16%, 2-year survival was 8%, and 3-year survival was 6%. At the last follow-up, 11 patients (24%) were alive and 35 dead (76%). At univariate analysis, we found that the following as positive predictive factors: primary tumor controlled, spinal metastases developed 1 year after the diagnosis of lung cancer (range 25–62 months), no visceral metastases, single spinal metastases, and few bone metastases (2–3 sites). These data were associated with a median survival >12 months (range 13–23 months). On the other hand, negative prognostic factors were observed as follows: persistence of primary tumor (unresectable), spinal lesions at diagnosis, and visceral metastases. In this subgroup of patients, median survival was 3–5 months. In patients with urologic cancer (29 patients) and GI (20 patients), the median overall survival was 22 months (range 2–45) and 16 months (range 3–28 months), respectively; 1, 2 and 3 years OS was 35, 30, and 25% in urologic patients and 40, 30, and 20% in patients with the GI tumor. In this set of patients, survival was not related to age, time of evidence of metastases at diagnosis of primary tumor or subsequently. The statistically significant factors affecting survival were the evidence of visceral metastases and the kind of surgery; all patients with single vertebral metastases who had undergone total tumorectomy are alive without recurrence of disease at the last follow-up (28 months GI cancer, 45 months urologic cancer).
Conclusions
Well-designed collaborative trials, including stratification of patients by histology, are necessary to draw final conclusion in this field. We believe that multidisciplinary approach and strict collaboration between the various figures involved in cancer care are the keys to tailor a therapeutic path on every patient.
References
Chi JH, Gokaslan Z, McCormick P, Tibbs PA, Kryscio RJ, Patchell RA (2009) Selecting treatment for patients with malignant epidural spinal cord compression-does age matter? Results from a randomized clinical trial. Spine 34(5):431–435
Gokaslan ZL (1996) Spine surgery for cancer. Curr Opin Oncol 8(3):178–181 (review)
Hunter RE, Wigfield CC (2008) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomized trial. Br J Neurosurg 22(5):713–714
Meyer SA, Singh H, Jenkins AL (2010) Surgical treatment of metastatic spinal tumors. Mt Sinai J Med 77(1):124–129 (review)
Rades D, Abrahm JL (2010) The role of radiotherapy for metastatic epidural spinal cord compression. Nat Rev Clin Oncol 7(10):590–598 (review)
Tancioni F, Navarria P, Lorenzetti MA, Pedrazzoli P, Masci G, Mancosu P, Alloisio M, Morenghi E, Santoro A, Rodriguez Y Baena R, Scorsetti M (2010) Multimodal approach to the management of metastatic epidural spinal cord compression (MESCC) due to solid tumor. Int J Radiat Oncol Biol Phys 78(5):1467–1473
Witham TF, Khavkin YA, Gallia GL, Wolinsky JP, Gokaslan ZL (2006) Surgery insight: current management of epidural spinal cord compression from metastatic spine disease. Nat Clin Pract Neurol 2(2):87–94
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tancioni, F., Navarria, P., Pessina, F. et al. Assessment of prognostic factors in patients with metastatic epidural spinal cord compression (MESCC) from solid tumor after surgery plus radiotherapy: a single institution experience. Eur Spine J 21 (Suppl 1), 146–148 (2012). https://doi.org/10.1007/s00586-012-2232-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2232-0