Abstract
Introduction
Restitution of sagittal balance is important after lumbar fusion, because it improves fusion rate and may reduce the rate of adjacent segment disease. The purpose of the present study was to describe the impact of transforaminal lumbar interbody fusion (TLIF) procedures on pelvic and spinal parameters and sagittal balance.
Materials and methods
Forty-five patients who had single-level TLIF were included in this study. Pelvic and spinal radiological parameters of sagittal balance were measured preoperatively, postoperatively and at latest follow-up.
Results
Age at surgery averaged 58.4 (±9.6) years. Mean follow-up was 35.1 months (±4.1). Twenty-nine percent of the patients exhibited anterior imbalance preoperatively, with high pelvic tilt (17.6° ± 7.9°). Of the 32 (71%) patients well balanced before the procedure, 22 (70%) had a large pelvic tilt (>20°), due to retroversion of the pelvis as an adaptive response to the loss of lordosis. Three dural tears (7%) were reported intraoperatively. Interbody cages were more posterior than intended in 27% of the cases. Disc height and lumbar lordosis at fusion level significantly increased postoperatively (p < 0.05 and p < 0.001). Pelvic tilt was significantly reduced (p < 0.01) postoperatively, whereas the global sagittal balance was not significantly modified (p = 0.07).
Conclusion
Single-level circumferential fusion helps patients reducing their pelvic compensation, but the amount of correction does not allow for complete correction of sagittal imbalance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In lumbar degenerative disease, loss of lordosis typically develops, with a reversed ratio of extensors/flexors muscle power compared with normal controls [1, 2]. It is important to analyze parameters of sagittal balance before lumbosacral surgical treatment, especially if fusion is considered. Biomechanical studies have shown that procedures improving disc height and lumbar lordosis increase tension in the anterior longitudinal ligament mediating better control of forces affecting the fused levels [3–5].
For each type of spinal fusion procedure, various corresponding advantages and drawbacks have been reported. Anterior lumbar interbody fusion (ALIF) gives better access to the disc space than posterior approaches, permitting more thorough discectomy and larger bone grafts [6, 7]. However, ALIF is associated with urological and vascular complications [8]. Posterior procedures include posterior lumbar interbody fusion (PLIF) as well as transforaminal lumbar interbody fusion (TLIF). With TLIF, because the preparation of the disc space and placement of the interbody cage is transforaminal, traction on the nerve root and the dura is minimized. Consequently, while clinical outcomes and fusion rates of TLIF and PLIF are comparable [9], TLIF is associated with a lower risk of postoperative radiculitis [10, 11].
To date, few studies have evaluated the radiological outcomes after TLIF procedures, and the global postoperative sagittal balance of the spine and the pelvis has never been reported to the best of our knowledge. The purpose of the present study was to evaluate the modifications of pelvic and spinal sagittal parameters after TLIF procedures for degenerative spinal disorders.
Materials and Methods
All patients who underwent a single-level TLIF procedure between June 2006 and June 2008 at our institution were included in this retrospective study. A minimum 2-year follow-up was required. The exclusion criteria were multilevel TLIF, previous spine surgery, degenerative scoliosis or preoperative frontal imbalance.
Data reported included demographic information, operative time, complications, as well as pre- and postoperative clinical records and radiographs.
Surgical procedure
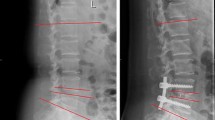
All patients were operated in knee–chest position, through a posterior approach. They underwent single-level posterolateral instrumented arthrodesis using monoaxial pedicle screws (Easyspine, LDR Medical, Troyes, France or CD Horizon Legacy, Medtronic Sofamor Danek, Memphis, USA), combined with a TLIF procedure using an interbody cage (ROI-T, LDR Medical, Troyes, France). A laminoarthrectomy was performed on one side to allow cage introduction. The interbody cage was placed as anteriorly as possible, under fluoroscopic control, and the highest implant was chosen to obtain a lordosing effect. In addition, in situ contouring was used on the rods to restore segmental lordosis (Fig. 1). Bone obtained from laminectomy was morselized and applied as graft material. No iliac crest was harvested.
Radiographic analysis
Standing anteroposterior and lateral radiographs were obtained preoperatively, postoperatively, and at latest follow-up. Measurements were made on 36 in. long-cassette radiographs, with the patient standing, knees fully extended and arms folded at 45° to avoid superposition with the spine. Patients were asked to hold their breath during the acquisition. All images included both the external auditory ducts and the superior third of the femurs. All lateral films were digitalized using a VIDAR VXR8 scanner and analyzed by the same investigator using a validated software (Optispine, Optimage, Lyon, France) [12].
The parameters measured were, as described by Mac-Thiong et al. [13]:
-
Pelvic incidence (PI) defined as the angle between a line joining the center of the upper endplate of S1 to the bicoxo-femoral axis and a line perpendicular to the upper endplate of S1.
-
Pelvic tilt (PT), angle between a vertical line and the line joining the middle of the sacral plate and the bicoxo-femoral axis.
-
Sacral slope (SS), angle between the endplate of S1 and a horizontal line.
-
Lumbar lordosis (LL), angle between the upper endplate of L1 and S1.
-
Segmental lordosis (Lseg) measured between the upper endplate of the vertebra above the instrumented disc and the lower endplate of the vertebra below the instrumented disc.
-
Sagittal vertical axis (SVA), measured as the offset between the C7 plumbline and the posterior superior corner of the sacrum. A sagittal forward imbalance was defined by a SVA >25 mm [14].
-
T9 sagittal offset (T9SO), angle between the vertical plumbline and the line joining the center of the vertebral body of T9 and the center of the bicoxo-femoral axis [15].
-
Disc height (DH), according to the method reported by Drain et al. [4] (Fig. 2).
The anteroposterior position of the cage, according to the intervertebral space, was also reported (anterior, middle or posterior third).
Statistical analysis
All statistical analyses were conducted using SPSS version 12.0 (SPSS Inc, Chicago, IL, USA). Paired-samples t tests were used to compare the preoperative and postoperative radiological parameters. All statistical tests were two-tailed, and a p value < 0.05 was considered to be significant.
Results
Patient data
Forty-five patients met the inclusion criteria (26 women and 19 men). Mean age was 58.4 (±9.6) years, mean body mass index was 27 (±3.6), and the American Society of Anesthesiologists (ASA) score averaged 1.8 (±0.4). Thirty patients (67%) were operated for degenerative spondylolisthesis, three (7%) for spondylolisthesis by isthmic lysis, six (13%) for painful disc degeneration, and six (13%) for disc herniation. Mean follow-up was 35.1 (±4.1) months.
Surgical procedure
Fusion level was L4–L5 in 28 patients (62%), L5–S1 in 9 (20%) and L3–L4 in 8 (18%). The anteroposterior height of the interbody cage was 8 mm in 22 cases (48%), 10 mm in 19 (43%) or 12 mm in 4 (9%). Forty-two cages (93%) had a lordosis angle of 9° and two cages (7%) had a lordosis of 5°. In all cases, the cage was introduced on the side of the preoperative radiculitis. The mean operative time was 124 (±37) minutes, and the intraoperative blood loss averaged 570 (±360) mL. No transfusion was necessary. There were three cases (7%) of intraoperative dural tear, and 1 deep infection (2%) occured postoperatively. Mean hospital stay was 10.6 (±2.8) days. Two patients required revision surgery during follow-up for persistent radiculitis.
Preoperative radiological measures
Twenty-nine percent of the patients exhibited anterior imbalance, with an average SVA of 52 mm (±17 mm).
In comparison to previous series reported [13, 16, 17], patients had a comparable mean pelvic incidence but a higher pelvic tilt (Table 1). Of the 32 (71%) patients well balanced in terms of SVA, 22 (70%) had a large pelvic tilt (>20°), due to retroversion of the pelvis as an adaptive response to the loss of lordosis. No patient presented a posterior imbalance preoperatively.
Postoperative radiological measures
Postoperative measurements of the parameters are reported in Table 1. Disc height (p < 0.05), lumbar lordosis at fusion level (p < 0.001) and maximum lumbar lordosis (p < 0.01) significantly increased postoperatively. These results were confirmed at latest follow-up, without significant loss of correction. On lateral radiographs, 12 (27%) interbody cages were more posterior than intended, in the middle third of the vertebral body instead of in the anterior third (Fig. 3). None was in the posterior part of the interbody space. However, the postoperative change in maximum lordosis remained significant regardless of the anteroposterior cage position, suggesting that placing the cage in the middle third of the interbody space might be sufficient to improve segmental lordosis (p < 0.02). At latest follow-up, pelvic tilt was significantly reduced (p < 0.01) and the global sagittal balance tended to improve, even though this trend failed to reach significance (p = 0.07).
Discussion
The purpose of this study was to describe the modifications of pelvic and spinal parameters of sagittal balance after a TLIF procedure. Disc height, lordosis at fusion level and maximum lordosis were statistically improved after surgery, whereas the global sagittal balance was not significantly modified.
Preoperative analysis
The preoperative analysis of spinal and pelvic sagittal balance is essential, because it helps in determining how much correction is needed, and then in choosing the type of procedure required to reach this goal [18, 19]. In addition, restoring spinal sagittal balance has been reported to improve fusion rates and reduce the rate of adjacent segment disease [20–22].
Thirteen patients (30%) had an anterior translation of the SVA, illustrating the natural kyphosing course of the degenerative lumbar spine [16, 23] (Fig. 3). The high rate of anteriorly imbalanced patients might be explained by the mean age of our population, which was higher than the one reported in most of the previous reports about TLIF, and by the fact that many patients were operated for spinal stenosis, responsible for functional (rather than structural) imbalance [24–28]. Mean pelvic tilt was large in our study group (17.6° ± 7.9°). The high pelvic tilt systematically present in patients with anterior translation of the SVA indicated that the pelvis was already in the position of maximum adaptation, but insufficiently to achieve sagittal spinal balance. Twenty-seven patients (60%) who had a normally positioned SVA had pelvic retroversion. These elements might reflect the adaptive position of the spine and pelvis adopted by the patients creating a situation of compensated sagittal balance (Fig. 4). Several studies have evaluated correlations between pelvic parameters and clinical outcomes. Schwab et al. [29] reported a correlation between pain (analogic pain scale) and loss of lordosis in a series of 95 patients. In a series of 298 patients, Glassman et al. [30] observed that anterior translation of the spine was associated with poorer clinical outcome scores measured by SF-12, SRS-23 and Oswestry disability index.
Lateral standing radiograph of a 72 year-old patient, sagittally balanced (SVA = 18 mm), but with increased pelvic tilt (PT = 30°), traducing a compensating pelvic retroversion. Parameters were measured with Optispine (Optimage, Lyon, France) [12]
TLIF procedure
TLIF procedures have been widely used since their first description in 1998 [31]. They have showed to improve disc space height and initial stability of the construct in comparison to posterolateral fusion [9]. In addition, the procedure is effective in improving sagittal spinal alignment, in combination with posterior instrumentation, if the appropriate surgical technique is implemented [24]. Recent studies reported that the TLIF technique had comparable results to other interbody fusions, such as PLIF or ALIF techniques, in terms of fusion or functional outcomes [27, 32]. However, the potential advantages of TLIF include avoidance of the anterior approach and reduction of the approach related posterior trauma to the spinal canal. This was confirmed by Faundez et al. [27], who found that TLIF procedures were associated with less intraoperative complications, but with more early postoperative revision surgery (hematoma, graft extrusion). In the present study, 3 dural tears (7%) occurred, a rate in accordance with previous studies [25, 26]. Aoki et al. [33] described 3 cases of migration of TLIF cages, but only one patient required revision surgery because of radicular pain. The cage was removed without any complication and replaced by a larger one. In our series, no case of cage migration was observed, although 12 cages (27%) were considered to have an overly posterior placement.
Segmental and local sagittal balance
In the current series, the TLIF procedure improved disc height (p < 0.05), lordosis at the level fused (p < 0.001), and maximum lumbar lordosis (p < 0.01). This was consistent with an earlier report [24]. However, the change in pelvic parameters had never been analyzed before. Physiological values of segmental lumbar lordosis have previously been reported by Guigui et al. [34]. The postoperative measures obtained in the current series are lower (−17.2° ± 7.4°), but the mean age of the group studied by Guigui et al. was younger (34 years), and their subjects did not suffer from degenerative lumbar disorders.
One of our goals was to place the cage in the anterior portion of the interbody space to improve lordosis (Fig. 1). However, the fact that this goal was not reached in 12 cases (27%) (Fig. 5) had no impact on the lordotic effect of the cage (p < 0.02). The same finding was previously reported in an in vitro biomechanical study [27], which showed that the position of the cage had no influence on the postoperative segmental lordosis or spinal mobility.
Global sagittal balance
Results of the present study show that a single-level circumferential fusion, combining posterolateral arthrodesis and TLIF, does not effectively correct severe anterior imbalance. Thus, there is long-term risk of accelerated degeneration at mobile segments above and below the fused spinal segment known as adjacent segment disease [15]. Retrolisthesis is the most common type of adjacent segment change, and Kumar et al. [35] showed that normal C7 plumb line and normal sacral inclination after lumbar fusions were important parameters for minimizing the incidence of adjacent level degeneration [35]. However, radiographically apparent adjacent segment disease is common but does not correlate with functional outcomes [36].
Complete correction of sagittal imbalances requires more invasive surgical procedures, such as multi-level fusion or osteotomies [4]. According to Rose et al. [37], pelvic incidence (PI) and thoracic kyphosis (TK) can predict with high sensitivity the lumbar lordosis (LL) necessary to correct sagittal imbalance in patients undergoing pedicle subtraction osteotomy. The formula PI + LL + TK < 45° shows 91% sensitivity for predicting ideal sagittal equilibrium at 24 months (p < 0.001). The reduction of the pelvic tilt (and increase of the sacral slope) observed at last follow-up in our series confirms that it is an adaptive parameter [17]. Theoretically, pelvic tilt reduction should increase the adaptive capacities of patients with lumbar degenerative pathologies. Moreover, its reduction is associated with less postoperative pain [22, 38].
Limitations
The main limitations of this study are the absence of a control group, the small number of patients, and the lack of functional outcome measurements. The effect of pain relief on the modification of sagittal parameters was not evaluated. The correlation between pain intensity and radiological measurements needs to be further studied, as it may provide information regarding the functional part of the spinal imbalance. The fusion status was not investigated in this series, but no loss of correction was observed at latest follow-up. In addition, the follow-up was short and further studies remain necessary to assess the long-term risk of adjacent segment disease.
Conclusion
TLIF procedures significantly improve lumbar lordosis and result in little morbidity. Single-level circumferential fusion helps patients reducing their pelvic compensation, but the amount of correction does not allow for complete correction of sagittal imbalance. Further studies are still needed to analyse functional outcomes of this procedure.
References
Jang JS, Lee SH, Min JH, Han KM (2007) Lumbar degenerative kyphosis : radiographic analysis and classifications. Spine (Phila Pa 1976) 32(24):2694–2699
Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y (1988) Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976) 13(11):1317–1326
Cloward RB (1953) The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 10(2):154–168
Drain O, Lenoir T, Dauzac C, Rillardon L, Guigui P (2008) Influence de la hauteur discale sur le devenir d’une arthrodèse postérolatérale. Rev Chir Orthop Reparatrice Appar Mot 94(5):472–480
Evans JH (1985) Biomechanics of lumbar fusion. Clin Orthop Relat Res (193):38–46
Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, Liu JC (2007) Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7(4):379–386
Hee HT, Castro FP Jr, Majd ME, Holt RT, Myers L (2001) Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord 14(6):533–540
Garg J, Woo K, Hirsch J, Bruffey JD, Dilley RB (2010) Vascular complications of exposure for anterior lumbar interbody fusion. J Vasc Surg 51(4):946–950 (discussion 950)
Humphreys SC, Hodges SD, Patwardhan AG, Eck JC, Murphy RB, Covington LA (2001) Comparison of posterior and transforaminal approaches to lumbar interbody fusion. Spine (Phila Pa 1976) 26(5):567–571
Cole CD, McCall TD, Schmidt MH, Dailey AT (2009) Comparison of low back fusion techniques: transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med 2(2):118–126
Grob D (2009) Surgery for degenerative lumbar disease: transforaminal lumbar interbody fusion. Eur Spine J 18(12):1991–1992
Berthonnaud E, Dimnet J, Roussouly P, Labelle H (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18(1):40–47
Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P (2010) Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine caucasian asymptomatic adults. Spine (Phila Pa 1976) 35(22):1193–1198
Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, Farcy JP (2008) Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 33(14):1572–1578
Morel E, Ilharreborde B, Lenoir T, Hoffmann E, Vialle R, Rillardon L, Guigui P (2005) Analyse de l’équilibre sagittal du rachis dans les spondylolisthésis dégénératifs. Rev Chir Orthop Reparatrice Appar Mot 91(7):615–626
Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11(1):80–87
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 30(3):346–353
Pellet N, Aunoble S, Meyrat R, Rigal J, Le Huec JC (2011) Sagittal balance parameters influence indications for lumbar disc arthroplasty or ALIF. Eur Spine J 20(Suppl 5):647–662
Obeid I, Hauger O, Aunoble S, Bourghli A, Pellet N, Vital JM (2011) Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J 20(Suppl 5):681–685
Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30(18):2024–2029
Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T, O’Brien M (2008) Spino-pelvic alignment after surgical correction for developmental spondylolisthesis. Eur Spine J 17(9):1170–1176
Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9(1):47–55
Videman T, Battie MC, Ripatti S, Gill K, Manninen H, Kaprio J (2006) Determinants of the progression in lumbar degeneration: a 5-year follow-up study of adult male monozygotic twins. Spine (Phila Pa 1976) 31(6):671–678
Jagannathan J, Sansur CA, Oskouian RJ, Jr, Fu KM, Shaffrey CI (2009) Radiographic restoration of lumbar alignment after transforaminal lumbar interbody fusion. Neurosurgery 64(5):955–963 (discussion 963–954)
Potter BK, Freedman BA, Verwiebe EG, Hall JM, Polly DW Jr, Kuklo TR (2005) Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech 18(4):337–346
Rihn JA, Patel R, Makda J, Hong J, Anderson DG, Vaccaro AR, Hilibrand AS, Albert TJ (2009) Complications associated with single-level transforaminal lumbar interbody fusion. Spine J 9(8):623–629
Faundez AA, Mehbod AA, Wu C, Wu W, Ploumis A, Transfeldt EE (2008) Position of interbody spacer in transforaminal lumbar interbody fusion : effect on 3-dimensional stability and sagittal lumbar contour. Eur Spine J 21(3):175–180
Yan DL, Pei FX, Li J, Soo CL (2008) Comparative study of PLIF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J 17(10):1311–1316
Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M (2002) Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976) 27(4):387–392
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30(6):682–688
Harms JG, Jeszenszky D (1998) The unilateral, transforaminal approaches to lumbar interbody fusion. Oper Orthop Traumatol 10(2):90–102
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U (2005) Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 14(6):551–558
Aoki Y, Yamagata M, Nakajima F, Ikeda Y, Takahashi K (2009) Posterior migration of fusion cages in degenerative lumbar disease treated with transforaminal lumbar interbody fusion: a report of three patients. Spine (Phila Pa 1976) 34(1):54–58
Guigui P, Levassor N, Rillardon L, Wodecki P, Cardinne L (2003) Valeur physiologique des paramètres pelviens et rachidiens de l’équilibre sagittal du rachis : analyse d’une série de 250 volontaires sains. Rev Chir Orthop Reparatrice Appar Mot 89(6):496–506
Kumar MN, Baklanov A, Chopin D (2001) Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 10(4):314–319
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29(17):1938–1944
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976) 34(8):785–791
Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP (2009) Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976) 34(17):599–606
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ould-Slimane, M., Lenoir, T., Dauzac, C. et al. Influence of transforaminal lumbar interbody fusion procedures on spinal and pelvic parameters of sagittal balance. Eur Spine J 21, 1200–1206 (2012). https://doi.org/10.1007/s00586-011-2124-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-2124-8