Abstract
Introduction
Pedicle screw instrumentation in AIS has advantages of rigid fixation, improved deformity correction and a shorter fusion, but needs an exacting technique.
Materials and methods
The author has been using the K-wire method with intraoperative single PA and lateral radiographs, because it is safe, accurate and fast. Pedicle screws are inserted in every segment on the correction side (thoracic concave) and every 2–3 on the supportive side (thoracic convex). After an over-bent rod is inserted on the corrective side, the rod is rotated 90° counterclockwise. This maneuver corrects the coronal and sagittal curves. Then the vertebra is derotated by direct vertebral rotation (DVR) correcting the rotational deformity. The direction of DVR should be opposite to that of the vertebral rotation. A rigid rod has to be used to prevent the rod from straightening out during the rod derotation and DVR. The ideal classification of AIS should address all curve patterns, predicts accurate fusion extent and have good inter/intraobserver reliability. The Suk classification matches the ideal classification is simple and memorable, and has only four structural curve patterns; single thoracic, double thoracic, double major and thoracolumbar/lumbar. Each curve has two types, A and B. When using pedicle screws in thoracic AIS, curves are usually fused from upper neutral to lower neutral vertebra. Identification of the end vertebra and the neutral vertebra is important in deciding the fusion levels and the direction of DVR. In lumbar AIS, fusion is performed from upper neutral vertebra to L3 or L4 depending on its curve types.
Conclusions
Rod derotation and DVR using pedicle screw instrumentation give true three dimensional deformity correction in the treatment of AIS. Suk classification with these methods predicts exact fusion extent and is easy to understand and remember.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pedicle screw instrumentation in AIS offers an enhanced three-dimensional deformity correction and preserves of motion segments by reducing the number of levels fused [1–5]. Pedicle screw fixation of the spine was first described by Boucher [6] and popularized by Roy-Camille et al. [7].
The author has been using pedicle screws for the management of thoracic AIS since 1988. The advantages are excellent deformity correction and maintenance with rigid fixation, shorter fusion and less operation time [8–10] (Table 1). In the beginning, pedicle screws in thoracic AIS were not widely used because of the fear of causing neurological injuries, despite the superb biomechanical advantages of pedicle screws over other forms of spinal instrumentation [11–13]. As more experience was gained thoracic pedicle screw instrumentation in the correction and fixation AIS became accepted as a reliable method with a high degree of safety. Many techniques of pedicle screw insertion were reported [14]. The most important step in the prevention of complications is accurate pedicle screw insertion, but an accurate pedicle screw insertion is not easy and sometimes dangerous. Complications of thoracic pedicle screw insertion in spine deformity are reported [5, 15–17] (Table 2). Pedicle screw insertion needs an exacting technique, especially in thoracic and small or deformed pedicles. A safe and accurate pedicle screw insertion is imperative and many methods are reported. Fluoroscopic or portable radiograph using in every screw insertion have high radiation and time consuming. Screw insertion without radiographic control is difficult and inaccurate to determine the pedicle entry point. Image guided surgery system still need experienced hand in the final screw insertion. The K-wire method needs only two radiographs of PA and lateral views after all K-wires are inserted at every level of the presumed screw entry points, and then all screws were inserted under the guidance of K-wires. The author has been using the K-wire method which is the most safe, accurate and rapid.
Pedicle screw insertion technique using K-wires [4, 5, 14, 18]
Incision, exposure and facetectomy
A standard posterior midline incision is made and exposed to the tip of the transverse processes bilaterally, staying strictly subperiosteal to reduce bleeding. The facets included in the fusion are destroyed by inferior facetectomy and removal of the articular cartilage.
K-wire insertion and radiographs
Presumed pedicle entry points are decorticated with a rongeur or burr to facilitate the insertion of the guide pins. In the upper thoracic spine, the presumed pedicle entry point is located at the junction of lateral margin of facet joint and the upper one-third of transverse process. The entry point is at the superior margin of transverse process in the middle thoracic spine and the middle of the transverse process in the lower thoracic spine. Then guide pins are inserted 1 cm deep through the exposed cancellous bone at the presumed pedicle entry point. Different sizes of K-wire are used on both sides. To facilitate radiograph interpretation, the guide pins are directed along the axis of the pedicle in the frontal and sagittal planes. After the guide pins are in place at the planned pedicle screw sites, intraoperative PA and lateral roentgenograms are taken to determine the association between the presumed entry point and the ideal entry point identifiable on the radiograph. Taking the transverse angle of the pedicles into consideration, the ideal pedicle entry point (IPEP) in a neutrally rotated vertebra is at the junction of a line parallel to the vertebral end plates bisecting the pedicle and the lateral margin of the pedicle ring shadow on a PA X-ray. In the rotated vertebra, the IPEP of the pedicles on the side of the rotation (convex side of scoliosis) moves more medially, whereas the IPEP on the opposite side (concave side) moves more laterally with increasing vertebral rotation (Fig. 1).
Screw hole preparation [19]
After determining the position of the IPEP and the direction of the ideal pedicle paths relative to the guide pin, the pedicle is entered through the starting point with an awl and then a small drill (60% of the outer pedicle diameter) or a small curette. It is important to keep in mind the normal transverse angle of the pedicles for the particular level to prevent inadvertent pedicle perforation. Then the hole is checked with a blunt-ended probe. A safe entry into the pedicle is confirmed when the probe meets bony resistance in all directions and cancellous bone at the tip, meaning that the hole is surrounded by bone.
Screw insertion
The screw has to be turned with gentle force so that the screw follows the predrilled path. The ideal screw diameter is about 80% of the pedicle diameter. However, in pediatric patients oversized screws up to 115% of the inside pedicle diameter may be inserted without causing a significant decrease in the screw holding power because of plasticity of the pedicular cortex. The ideal screw length is about 70% penetration of the vertebral body on a lateral radiograph to avoid complications of screw overpenetration. Screws are inserted in every segment on the correction side (thoracic concave and lumbar convex) and every second or third on the support side (thoracic convex and lumbar concave). When the deformity is flexible and not severe, screws are inserted at every other segment and used translation method in reduction. In severe rigid scoliosis, bilateral segmental insertion at each pedicular level can be applied to increase the rigidity of the fixation, especially in lumbar levels.
Deformity correction
Rod derotation [20–23]
After the insertion of the screws on both the concave and the convex sides is complete, a rod contoured to have a slight exaggeration (about one-third) of the normal sagittal contour of the instrumented segment is inserted into the correction (concave) side. Insertion of the rod may be difficult when there is a large discrepancy between the contour of the vertebral column and the rod. This may be facilitated by using rod introducers or sequentially closing the screw caps while rotating the rod to fit the contour of the vertebral column. Long arm reduction screws can be used effectively. For long curves that span both the thoracic and the lumbar region, either a long rod spanning the entire correction side or shorter rods spanning each of the curves may be used. For a double thoracic curve, separate correction of each curve is carried out with short rods on the respective concave sides. When the plan is to perform separate correction of individual structural curves, remove a pedicle screw at the junction of the rods to make room for rod connectors. Following the rod insertion, the eye bolts are inserted loosely over the screws.
Using clamps or rod holders, the correction rod is rotated 90° to transform the scoliosis into a kyphosis at thoracic spine and a lordosis at lumbar spine, restoring the sagittal profile in the corrected position. Correction of the deformity is performed solely by derotation without any additional compression or distraction. As considerable straightening of the contoured rod occurs during the process of derotation, it is advantageous to use large-bore stiff rods with exaggeration of the normal sagittal profile. When a rod straightens-out, remove it, rebend to an over bent shape and reinsert it. Do this until the desired sagittal curve is obtained.
As the rod is just supportive at the convex side in the thoracic and the concave side in the lumbar, the rod is bent conforming to the shape of the corrected curve and placed in situ without forceful manipulation. In double thoracic curves using a four-rod correction technique, support rods are connected to the correction rods by means of connectors.
Direct vertebral rotation (DVR) [24–26]
After the rod derotation correcting the coronal and the sagittal curves, then the DVR is performed to correct the rotational deformity. There are two forces induced by rod derotation. First, the vector of “rod derotation” is directed posteriorly and medially. This force corrects both the coronal and sagittal plane deformities, but not that in the transverse plane. Second, the rod is also rotated about 90° on its own axis during rod derotation. This may affect the vertebral rotation in scoliosis. In the cases with severe or rigid scoliosis, for example, there is friction between the rod and the pedicle screws during rod derotation. This rotational force tends to increase the rotational deformity. If there is no friction between the rod and the screws, then the screws will glide on the rod. In this situation, the rotational deformity may be corrected depending on the angle between the pedicle screws and the vector of rod derotation. This might be similar to rod derotation in flexible mild curves. Derotation in flexible curves is promoted by the posterior force vector by the rod moving posterior during derotation, which thus pulls the concave side posterior while the opposite side moves to a lesser distance. The effect of rod derotation on the rotational correction is negligible because there always exists some amount of friction between the screws and the rod during rod derotation. Clinically, the rotational correction obtained by rod derotation is probably from the translation of the vertebra.
The concept of the DVR is simple. That is to say that it is correction of the vertebral rotation by application of a force directed posteriorly in the direction opposite to that of the deformity. The pedicle screw enters the pedicle posteriorly and penetrates to the anterior vertebral body. This makes it possible to transmit the rotational force to the entire vertebral body and thus to correct the rotational deformity. Other posterior instrumentations such as hooks or wire systems cannot deliver a sufficient torque to enable vertebral rotation because the axis of fixation is posterior to that of vertebral rotation. The torque is applied to the pedicle screw using long screw derotators on both concave and convex sides of the curve. The DVR corrects the intervertebral rotation, which means it enables a three-dimensional correction in scoliosis surgery. The DVR was performed a segmental rotation using 2–3 anchors at the same time to avoid screw pull-out and for more effective derotation and DVR. The direction of the DVR is important and should be opposite to that of the vertebral rotation. In the right thoracic curve, the apical and juxta-apical vertebrae are rotated clockwise in the transverse plane as seen from a caudal position. The uppermost one or two vertebra have to be derotated opposite the direction of the thoracic DVR. On the lowermost one or two screws, however, the direction of DVR depends on the rotation of vertebra in the compensatory lumbar curve.
Suk classification, fusion levels and DVR in AIS [5, 27–29]
The fusion level is very important and an inappropriate fusion level may result in under or overcorrection of the major and compensatory curves, and result in failure to stabilize the index curve, increase of the unfused curve, trunk imbalance and/or decompensation. Pedicle screw fixation effectively shortens the distal fusion level by improved three-dimensional deformity correction with rod derotation and DVR. In AIS, identification of curve patterns and determination of fusion levels are most important factors for deformity correction, trunk balance and saving motion segments. There are many classifications of AIS (Table 3). The King-Moe classification applies for the thoracic curve and the Lenke classification is complicated. The ideal classification of AIS should address all patterns, predict accurate limits of the deformity and fusion levels be reproducible and have good inter/intraobserver reliability. The Suk classification that matches the ideal classification is simple and memorable and applies to pedicle screw instrumentation. The Suk classification defines four structural curves; single thoracic, double thoracic, double major and thoracolumbar/lumbar. For the distal fusion levels, there are two types, A and B, for the thoracic curves and another for the TL/L curve (Table 4).
Single thoracic curve [30, 31]
Single thoracic curve is defined as a thoracic more than 40°, that is larger than the lumbar curve. If the lumbar curve is more than 40°, the thoracic curve must be more than 5° larger than the lumbar curve and the apical vertebra rotation of the lumbar spine should be less than Nash-Moe grade II. A selective thoracic fusion is appropriate in the single thoracic curve. After a selective thoracic fusion, the results, regardless of the rotational status of the lumbar curve, were satisfactory, with straightening of the lumbar curves and good balance. A selective thoracic fusion is a fusion to the proximal neutral vertebra (NV) and to the distal NV. It is important to determine the exact distal fusion level. The NV is an important factor for the determination of the fusion level. There are two types, A and B, depending on relation between the end vertebra (EV) and the NV. When the preoperative EV and the NV show no more than one-level gap difference or are the same (type A), the curve could be fused down to the NV. When the NV is same as the EV, fusion can be stopped at the EV. If the NV is located 2–3 levels more distally than the EV (type B), fusion must go down one more level distally than type A or NV-1. In this way, one or two motion segments can be saved, compared to fusion extending to the stable vertebra.
The direction of DVR on the vertebra on each side of the apex vertebra is opposite to the rotation of the vertebrae. During or after the rod is derotated 90° counterclockwise, the DVR on the juxta-apical screws should be rotated clockwise. The direction of the DVR of the proximal 1 or 2 vertebras have to be opposite to the direction of the thoracic DVR to preserve shoulder balance. For the lowermost 1 or 2 screws in the distal curve, there are two options depending on the lowermost uninstrumented lumbar curve. These screws have an important role in regulating the compensatory lumbar curve. In type A, the two lowermost screws should be rotated opposite (OD) to the direction of the thoracic DVR, that is, the direction of lessening lumbar rotation. One reason for this is that the remaining thoracic rotational deformity inhibits the ultimate rotational correction in the lumbar curve, even though a significant amount of lumbar rotation is spontaneously corrected. In this situation, the lumbar rotation is improved by DVR of the lowermost screws in the opposite direction (OD) of the thoracic DVR. On the other hand, when the distal vertebra is rotated in the same direction as the thoracic rotation (type B), the DVR has to be the same direction (SD) as the thoracic DVR. When the lumbar rotation is more severe, more forceful DVR must be employed (Figs. 2, 3).
a A 15-year-old girl with a single thoracic AIS, type A, in which the NV is the same as the EV. The distal fusion level is T12 (NV) and the direction of the DVR of the distal NV is the opposite direction compared with the thoracic DVR. b The patient is treated with the rod derotation and DVR, and the postoperative radiographs show a well balanced spine
a A 14-year-old girl with a single thoracic AIS, type B, in which the NV is located at the EV + 3. The distal fusion level is the NV-1 (L2) and the direction of the DVR of the two lowest instrumented vertebrae is the same direction compared with the thoracic DVR. b The patient is treated with the rod derotation and the DVR method
Double thoracic curve [32–35]
It is important to determine the indication for fusing the proximal thoracic curve when correcting double thoracic scoliosis with segmental instrumentation. Failure to recognize a significant proximal thoracic curve often results in postoperative shoulder asymmetry due to relative overcorrection of the lower thoracic curve. With segmental instrumentation that enhances the correction of the instrumented curve, the double thoracic curve pattern that needs fusion of both the proximal and the distal thoracic curves is redefined as follows [34]: idiopathic thoracic scoliosis with a distal thoracic curve of more than 40°, and a proximal thoracic curve of more than 30°, level or elevated left shoulder and T1 tilted should be considered a double thoracic curve pattern and should be treated by fusing both the proximal and the distal curves. The distal fusion levels are same as in the single thoracic curve, depend on whether type A or B.
The DVR direction of both the proximal and the distal thoracic curves are opposite to the rotation of the vertebra in the transverse plane, the same as in the single thoracic curve. The DVR direction of the distal vertebra is different and depends on type A or B, like in the single thoracic curve (Fig. 4).
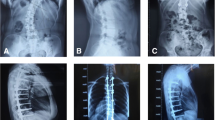
a A 13-year-old girl with a double thoracic AIS. The distal fusion level is the NV, which is L1, and the direction of the DVR is the opposite direction compared to the thoracic DVR. b Both thoracic curves are fused with four rods, rod derotation and DVR. c The preoperative unequal shoulder height is well corrected postoperatively
Double major curve [5, 18]
The double major curve is defined as follows: the lumbar curve is larger than the thoracic curve, and the lumbar curve is more than 40° and the thoracic curve is more than 30°; and the thoracic curve is less than 5° larger than the lumbar curve and the apical vertebra rotation of the lumbar is more than grade II. In these cases, both the thoracic and the lumbar curves have to be fused. It is important to save the distal fusion level. There are two types A and B, depending on the lumbar bending radiographs. The type A curve is when L3 crosses the central sacral vertical line (CSVL) in right bending and L3 rotation is less than grade II in left bending, and has to be fused to the EV which is L3. When L3 does not cross the CSVL in right bending and L3 rotation is more than grade II in left bending (Type B), fuse to the EV + 1 which is L4.
The DVR direction of the thoracic curve should be rotated clockwise, the same as in the single thoracic curve and the lumbar curve is rotated toward the opposite direction of the thoracic DVR (Figs. 5, 6).
a A 13-year-old girl with a double major curve of AIS. The DVR direction of the lumbar curve is the opposite to the direction of the thoracic DVR. b Bending radiographs show that L3 is cross mid-sacral line and L3 rotation is less than grade 2 (type A). This is fused to the NV-1 (L3). c Both thoracic and lumbar curves are treated with two rods, the translation and DVR
a A 17-year-old girl with a double major curve, type B. The DVR direction of the lumbar curve is the opposite to the direction of the thoracic DVR. b Bending radiographs show that L3 not cross mid sacral line and L3 rotation is more than grade II (type B), which is fused to the NV (L4). c The patient is treated with two rods, rod derotation and DVR
Thoracolumbar and lumbar (TL and L) curve [5, 18]
The TL and L curve is a curve that is more than 40° and the thoracic curve is less than 30°. In this case, the TL and L curve only needs to be fused. There are types A and B for the distal fusion levels depending on the lumbar bending films, the same as in the double major curve. The DVR direction of TL and L curves is opposite to their vertebral rotation toward improving rotational deformity, same as in the lumbar curve of the double major curve. With this principle, the TL and L curve can be fused short, similar to anterior instrumentation [36] (Figs. 7, 8).
a A 12-year-old girl with a thoracolumbar curve with fusion of the TL curve only. The direction of DVR is the same in both the thoracic and the lumbar curve. b Bending radiographs show L3 cross the mid-sacral line and L3 rotation is less than grade II (type A) on bending film. c The patient is fused to the NV-1 (L3) with rod derotation (S bended rod) and DVR
In summary for the distal fusion level in AIS, there are two groups, type A and B, one in the thoracic curve and another in the lumbar curve (Fig. 9). Type A and B in the thoracic curve is decided with the location of the neutral vertebra (NV), whether the NV is located at 1 or 3 levels distal of the end vertebra (EV). Type A and B in the lumbar curve is decided with both lumbar bending (right and left) radiographs, whether the L3 cross or not cross over the central sacral line, and whether the L3 rotation is more or less than Nash-Moe grade II.
Type A & B for the distal fusion levels. Thoracic curve type A; the neutral vertebra (NV) is located 1 level distal from the end vertebra (EV), fuse to the NV. Thoracic curve type B; the NV is located 3 levels distal from the EV, fuse to the NV-1. Lumbar curve type A; L3 cross the central sacral line and rotation is less than G2, fuse to the L3. Lumbar curve type B; L3 not cross central sacral line and rotation is more than G2, fuse to the L4
Direction of DVR
Single thoracic curve The direction of DVR on the juxta-apical vertebrae is opposite to the rotation of the vertebrae in the transverse plane. During or after the rod is derotated 90° counterclockwise, the DVR on the juxta-apical screws should be rotated clockwise. The direction of the DVR of the proximal 1 or 2 vertebras has to be opposite to the direction of the thoracic DVR for obtaining correct shoulder balance. For the lowermost one or two screws, there are two options depending on the distal uninstrumented lumbar curve. These screws have an important role in regulating the compensatory lumbar curve. In a thoracic concave, whether single or double curve, when the preoperative compensatory lumbar curve crosses the center sacral vertical line with a rotation (Type A), the two lowermost screws should be rotated opposite (OD) to the direction of the thoracic DVR, that is, in the direction of lessening the lumbar rotation. One reason for this is that the remnant thoracic rotational deformity inhibits the ultimate rotational correction in the lumbar curve, even though a significant amount of lumbar rotation is spontaneously corrected. In this situation, the lumbar rotation is improved by rotating the lowermost screws to the opposite direction (OD) of the thoracic DVR. On the other hand, when the distal vertebra are rotated in the same direction as that of the thoracic rotation, like in a type B thoracic curve, the DVR has to be rotated the same direction (SD) of the thoracic DVR, and with more forceful DVR when the lumbar rotation is more severe.
Double thoracic curve The DVR direction of both the proximal and the distal thoracic curves in the double thoracic curves are same as that in a single thoracic curve. The distal fusion levels are also the same as that in the single thoracic curve, type A and B.
Double major curve The DVR direction of the thoracic curve is same as that in a single thoracic curve and the lumbar curve is rotated toward the opposite direction of the thoracic DVR. The distal fusion levels are at L3 in type A and L4 in type B.
Thoracolumbar/lumbar curve The DVR direction of the TL/L curve is toward the opposite direction of the thoracic DVR, the same as that in the double major curve. With this principle, the TL/L curve can be fused short, like in the anterior instrumentation.
Procedures of pedicle screw instrumentation for AIS: Pedicle screw insertion, rod derotation and DVR
-
1.
Insert the pedicle screws at each segment on the correction sides (thoracic concave) and every second or third segment on the support side (thoracic convex) of the curves.
-
2.
Rotate the precontoured rod on the correction side (counter-clockwise) without any compression or distraction.
-
3.
Insert the screw derotators (2–3 derotators) onto the pedicle screws of the juxta-apical vertebrae on the concave side, or both the concave and the convex sides.
-
4.
After the rod derotation and maintaining the rod derotation, rotate the screw derotators to the opposite direction (clockwise) of the rod derotation.
-
5.
Rotate the uppermost pedicle screws to the opposite direction of the thoracic DVR.
-
6.
Rotate the lowermost pedicle screws depending on the unfused lumbar curve.
-
7.
After locking the concave rod in the corrected position, a rod contoured to the corrected curve is placed on the convex side and it is locked in situ.
The transverse rotation can be easily corrected using long lever-arm screw derotators, 2–3 screws at the same time. This will distribute the rotational torque among several pedicles to help prevent pedicle breakage. There is little chance of canal intrusion due to pedicle breakage during the DVR when the screws are inserted correctly because the medial wall of the pedicle is three times stronger than the lateral wall.
The Suk classification, fusion levels and DVR directions for AIS is summarized (Table 5).
Conclusion
Thoracic pedicle screw instrumentation is a safe and reliable method of treating AIS with rigid fixation, shorter fusion levels and excellent three dimensional deformity correction. Rod derotation corrects the coronal and sagittal curves and DVR corrects the rotational deformity. It is imperative to understand each of curve patterns of AIS as defined in the Suk classification, with four structural curves each with A and B types that, address all curve patterns, predicts exact fusion extent and is easy to understand and remember.
References
Harrington PR (1962) Treatment of scoliosis. J Bone Joint Surg Am 44:591–610
Goldstein LA (1969) Treatment of idiopathic scoliosis by Harrington instrumentation and fusion with fresh autogenous iliac bone grafts. J Bone Joint Surg Am 51:209–222
King H, Moe JH, Bradford DS et al (1983) The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am 65:1302–1313
Suk SI, Lee CK, Kim WJ et al (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 20:1399–1405
Suk SI, Kim WJ, Lee SM et al (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine 26:2049–2057
Boucher HH (1959) A method of spinal fusion. J Bone Joint Surg Br 41:248–259
Roy-Camille R, Saillant G, Mazel C (1986) Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop 203:7–17
Cotrel Y, Dubousset J, Guillaumat M (1988) New universal instrumentation in spinal surgery. Clin Orthop 227:10–23
Suk SI, Lee CK, Min HJ et al (1994) Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop 18:341–346
Liljenqvist UR, Halm HF, Link TM (1997) Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine 22:2239–2245
Esses SI, Sachs BL, Dreyzin V (1993) Complications associated with the technique of pedicle screw fixation: a selected survey of ABS members. Spine 18:2231–2239
Brown CA, Lenke LG, Bridwell KH et al (1998) Complications of pedicle thoracolumbar and lumbar pedicle screws. Spine 23:1566–1571
Lonstein JE, Denis F, Perra JH et al (1999) Complications associated with pedicle screws. J Bone Joint Surg Am 81:1519–1528
Lenke LG, Edwards CC II, Bridwell KH (2003) The Lenke classification adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine 28:S199–S207
Kim YJ, Lenke LG, Bridwell KH et al (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29:333–342
Wong CC, Ting F, Wong B et al (2005) Accuracy of the funnel technique of thoracic pedicle in scoliosis surgery––an evaluation by CT-scans. Med J Malaysia 60S:35–40
Di Silvestre M, Parisini P, Lolli F et al (2007) Complications of thoracic pedicle screws in scoliosis treatment. Spine 32:1655–1661
Suk SI, Kim WJ (1998) Pedicle screw fixation for thoracic scoliosis. In: Brown CW (ed) Spinal instrumentation techniques. Scoliosis Research Society, Rosemont
Suk SI, Cha SI, Lee CK et al (1995) A study on the pullout strength of pedicle screws in relation to the size of the drill holes and inserted screws. Presented at the 30th annual meeting of the scoliosis research society, Asheville, NC
Zindrick MR, Wiltse LL, Doomik A et al (1987) Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine 12:160–166
Misenhimer GR, Peek RD, Wiltse LL et al (1989) Anatomic analysis of pedicle cortical and cancellous diameter as related to screw size. Spine 14:367
Suk SI, Lee JH (1994) A study of the diameter and change of the vertebral pedicle after screw insertion. Presented at third intermeeting SIROT, Boston, Massachusetts
Bridwell KH, McAllister JW, Betz RR et al (1991) Coronal decompensation produced by Cotrel–Dubousset “derotation” maneuver for idiopathic right thoracic scoliosis. Spine 16:769–777
Labelle H, Dansereau J, Bellefleur C et al (1995) Preoperative three-dimensional correction of idiopathic scoliosis with the Cotrel-Dubousset procedure. Spine 20:1406–1409
Suk SI, Kim WJ, Kim JH et al (1999) Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord 12:489–495
Lee SM, Suk SI, Chung ER (2004) Direct vertebral rotation: A new technique of three-dimensionaldeformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine 29:343–349
Lenke LG, Betz RR, Bridwell KH et al (1999) Spontaneous lumbar curve coronal correction after selective anterior or posterior thoracic fusion in adolescent idiopathic scoliosis. Spine 24:1663–1671
Shufflebarger HL, Clark CE (1990) Fusion levels and hook patterns in thoracic scoliosis with Cotrel–Dubousset instrumentation. Spine 15:916–920
Marguilis JY, Floman Y, Robin GC et al (1998) An algorithm for selection of instrumentation levels in scoliosis. Eur Spine J 7:88–94
Suk SI, Lee SM, Chung ER et al (2003) Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine 28:484–491
Arlet V, Marchesi D, Papin P et al (2000) Decompensation following scoliosis surgery: treatment by decreasing the correction of the main thoracic curve or “letting the spine go”. Eur Spine J 9:156–160
Lee CK, Denis F, Winter RB et al (1993) Analysis of upper thoracic curve in surgically treated idiopathic scoliosis: a new concept of double thoracic curve pattern. Spine 18:1599–1608
Lenke LG, Bridwell KH, O’Brien MF et al (1994) Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel–Dubousset instrumentation. Spine 19:1589–1597
Winter RB, Denis F (1994) The King type V curve pattern. Its analysis and surgical treatment. Orthop Clin North Am 25:353–362
Suk SI, Kim WJ, Lee CS et al (2000) Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis. Spine 25:2342–2349
Suk SI, Lee CK, Chung SS (1994) Comparison of Zielke ventral derotation system and Cotrel-Dubousset instrumentation in the treatment of idiopathic lumbar and thoracolumbar scoliosis. Spine 19:419–429
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suk, SI., Kim, JH., Kim, SS. et al. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J 21, 13–22 (2012). https://doi.org/10.1007/s00586-011-1986-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1986-0