Abstract
Instrumentation and fusion to the sacrum/pelvis has been a mainstay in the surgical treatment of scoliosis in Duchenne muscular dystrophy (DMD) and is recommended to correct pelvic obliquity. The caudal extent of instrumentation and fusion in the surgical treatment of scoliosis in DMD has remained a matter of considerable debate, and there have been few studies on the use of segmental pedicle screw instrumentation for this pathology. From 2004 to 2007, a total of 28 patients with DMD underwent segmental pedicle screw instrumentation and fusion only to L5. Assessment was performed clinically and with radiologic measurements. All patients had a curve with the apex at L2 or higher preoperatively. Preoperative coronal curve averaged 74°, with a postoperative mean of 14°, and 17° at the last follow-up. The pelvic obliquity improved from 17° preoperatively to 6° postoperatively, and 6° at the last follow-up. Good sagittal plane alignment was recreated after surgery and maintained long term. In 23 patients with a preoperative L5 tilt of less than 15°, the pelvic obliquity was effectively corrected to less than 10° and maintained by adequately addressing spinal deformity, while five patients with a preoperative L5 tilt of more than 15° had a postoperative pelvic obliquity of more than 15°. Segmental pedicle screw instrumentation and fusion to L5 was effective and safe in patients with DMD scoliosis with a minimal L5 tilt (<15°) and a curve with the apex at L2 or higher, both initially and long term, obviating the need for fixation to the sacrum/pelvis. Segmental pedicle screw instrumentation and fusion to L5 was safe and effective in patients with DMD scoliosis with stable L5/S1 articulation as evidenced by a minimal L5 tilt of less than 15°, even though pelvic obliquity was significant. There was no major complication. With rigid segmental pedicle screw instrumentation, the caudal extent of fusion in the treatment of DMD scoliosis should be determined by the degree of L5 tilt. This method in appropriate patients can be a viable alternative to instrumentation and fusion to the sacrum/pelvis in the surgical treatment of DMD scoliosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Duchenne muscular dystrophy (DMD) is the most common and severe form of muscular dystrophy and is a flaccid neuromuscular disorder in which gradual deterioration is the hallmark [7, 11, 19, 22, 27, 29, 33]. Spinal deformity such as scoliosis is almost universal in patients with DMD [7, 11, 19, 22, 27].
Non-operated scoliotic curves in patients with DMD progress relentlessly to levels as great as 80° or more [31, 33]. Natural history studies on neuromuscular scoliosis demonstrated an almost invariable progression [2, 18, 31, 33]. The progression of untreated spinal deformity in this population causes increasing pain [14, 35], difficulties in sitting [2, 9, 22, 27], decreased pulmonary function [4, 27] and an increase in mortality [28]. Surgical management is the most reliable treatment for this deformity. Posterior spinal fusion in patients with DMD has been accepted as an optimal procedure to stabilize the spine and maintain an upright and comfortable sitting balance [5, 9, 13].
Major changes affected scoliosis surgery: earlier spinal stabilization and improvement in implants and instrumentation technique. However, most reports on scoliosis surgery in patients with DMD have dealt with spinal instrumentation using hooks, wires and hybrid constructs with lumbar pedicle screws [4, 12, 17, 22, 23, 30], yet it is difficult to provide strong and stable fixation with hook and wire anchors in patients with DMD [23, 38].
The development of the intrailiac post by Allen and Ferguson [1] has provided a reliable means to achieve pelvic fixation and address pelvic obliquity. Several studies have reported that instrumentation and fusion to the sacrum/pelvis should be reserved for patients with large coronal curves (>40°) and severe pelvic obliquity (>10°) [27, 35, 37]. However, the indications for extending the instrumentation and fusion to the pelvis/sacrum have remained controversial [23, 30]. Furthermore, pelvic or sacral fixation has several disadvantages [25, 27].
The purpose of this study was to determine the efficacy and safety of stopping segmental pedicle screw instrumentation constructs at L5 in the treatment of scoliosis in DMD.
Patients and methods
Patients
From December 2004 to October 2007, a total of 28 consecutive patients with DMD underwent posterior spinal fusion and segmental pedicle screw instrumentation for scoliosis at our institute. All patients were non-ambulatory. All the operations were performed by the same surgeon (M.T.).
Surgical techniques
The primary aim of the surgery was to obtain a solid fusion, level pelvis, and a balanced spine in the coronal and sagittal planes in these patients. The incision was midline and extended over. The posterior elements of the spine were exposed from the upper thoracic spine to the sacrum by stripping the muscles subperiosteally. The spinous process, the lamina, and the base of the transverse process of the vertebrae were stripped of periosteum. After removal of all soft tissue, local autograft bone was obtained from the spinous process, laminae, and transverse process of all the vertebrae, which did not support instrumentation, as a bone graft source. All articular facets were removed carefully. Spinal cord function was monitored throughout the procedure. Autotransfusion via preoperative storage and intraoperative collection was used. Correction of the curves was maintained by segmental pedicle screw and rod instrumentation. Instrumentation was Expedium instrumentation with a 5.5 mm titanium rod (Expedium, DePuy-Acromed, Raynham, MA, USA). Pedicle screws with a diameter of 5 mm were used in the thoracic and lumbar spine. Cross-links were employed as needed. The pelvis was not included in the instrumentation. All curves were instrumented and fused from T3 or T4 to L5 regardless of the severity of spinal deformity and pelvic obliquity. For the segmental pedicle screw instrumentation, every level was instrumented on at least one side. No image-guided spinal navigation system was employed. Screws were placed with free-hand technique. Fluoroscopy was employed to confirm acceptable screw position. The segmental pedicle screw correction was performed with rod insertion, rod rotation, translation of the rod, appropriate distraction and compression to level the proximal and distal end vertebra. Extensive posterior elements decortication for local bone graft was performed using a motorized gouge. The local bone graft was packed onto the prepared surfaces and placed carefully in each facet. The wound was sutured in three layers with two drainage tubes.
Radiographic assessment
Preoperative and postoperative radiographic evaluation included sitting posterior–anterior (PA) and lateral radiographs and best-effort spine side-bending radiographs. The sitting PA radiograph and side-bending films were examined and Cobb angles of the curve were needed to determine flexibility and correction. Sitting PA and lateral radiographs were taken the day before surgery, in a week after surgery and thereafter at a 3-month interval after surgery. On the coronal plane, the Cobb angles of the curves were measured. Lumbar 5 (L5) tilt (the angle between a line across the top of L5 and the intercristal line) and spinal pelvic obliquity (SPO) (the angle between the perpendicular of the spine line from T1 to S1 and a line across the top of the pelvis) were measured (Fig. 1). There have been some definitions of pelvic obliquity. It is important to identify a method to measure pelvic obliquity. SPO is the most commonly used method to calculate pelvic obliquity, while the line from T1 to S1 is not necessarily the same as the line that represents the obliquity of the trunk and the chest cage. However, several studies have concluded that obliquity measured by SPO is the most reliable and the standard method by which pelvic obliquity can be defined [15, 23]. Therefore, the current authors used SPO to measure the pelvic obliquity in this study. On the sagittal plane, thoracic kyphosis between T3 and T12, and lumbar lordosis between L1 and L5 were measured. Fusion was defined as: first, stable coronal and sagittal alignment over the follow-up period; second, no clinical complaints; third, no evidence of nonunion radiographically; and fourth, stable instrumentation. All four criteria must be present for the definition of fusion.
The technique of determining the L5 tilt and spinal pelvic obliquity (SPO). L5 tilt (the angle between a line across the top of L5 and the intercristal line) and spinal pelvic obliquity (the angle between the perpendicular of the spine line from T1 to S1 and a line across the top of the pelvis) were measured
Results
Twenty-eight patients who were followed up for a minimum of 2 years were enrolled into this study. No patients were lost to follow-up. Demographic details and surgical parameters for the study group patients are demonstrated in Table 1. Radiographic measurements in the coronal and sagittal plane alignment are demonstrated in Table 2. Changes in the pelvic obliquity and L5 tilt are demonstrated in Fig. 2. The mean age at surgery was 13 years and 6 months (range: 11 years 8 months–14 years 10 months). All scoliosis curves were single curves (23 right thoracolumbar, three left thoracolumbar and two right thoracic curves). The mean operating time was 282 min (range: 232–308 min). The mean intraoperative blood loss was 950 ml (range: 660–1,260 ml). The mean total blood loss was 2,150 ml (range: 1,250–2,880 ml). The mean follow-up period was 40 months (range: 24–57 months).
Changes in pelvic obliquity (a) and L5 (b). Twenty-one of 25 patients had pelvic obliquity of less than 10° postoperatively. All these patients had L5 tilt of more than 15° preoperatively. Four patients had pelvic obliquity of more than 10° postoperatively and all these patients had L5 tilt of more than 15° preoperatively
During hospitalization, most patients reported back pain in the region of surgery. At 3 months after surgery, no patients reported back pain and clinical complaints in the region of surgery. On the coronal plane, the mean preoperative coronal curve measured 74° (range: 51–88°). The mean preoperative coronal curve on best-effort spine side-bending radiograph was 16° (range: 10–27°) and the preoperative flexibility of the curve averaged 78%. The mean immediate postoperative coronal curve measured 14° (range: 8–25°) (81% correction). At the last follow-up, the mean curve measured 17° (range: 9–27°) and we noticed less than 3° in the loss of correction in all patients at the last follow-up. On the sagittal plane, the mean preoperative sagittal thoracic curve (T3–T12) measured 10° (range: −8° to 23°). The mean immediate postoperative sagittal thoracic curve measured 20° (range: 12–28°). At the last follow-up, this curve measured 21° (range: 13–28°). The mean preoperative sagittal lumbar curve (L1–L5) measured 15° (range: −18° to 58°), including many kyphotic patients and the mean immediate postoperative curve measured 34° (range: 8–45°). This curve measured 35° (range: 7–44°) at the last follow-up. Therefore, no significant loss of correction in the coronal and sagittal plane was noted between postoperative time and the last follow-up. The L5 tilt improved from a preoperative mean of 9° (range: 5–20°) to a postoperative mean of 3° (range: 0–18°) and 3° (range: 0–20°) at the last follow-up. The pelvic obliquity improved from a preoperative mean of 17° (range: 10–38°) to a postoperative mean of 6° (range: 2–22°) and 6° (range: 2–25°) at the last follow-up. We noticed no significant loss of correction of pelvic obliquity and L5 tilt.
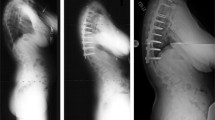
Of the 28 patients, 23 had an SPO of less than 10° postoperatively. A good pelvic balance was achieved and maintained despite the fusion only to L5 in these patients. These 23 patients had a preoperative L5 tilt of less than 15° and the SPO was effectively corrected to less than 10° and maintained by adequately addressing spinal deformity (Table 2, Fig. 2). Figure 3 shows a radiographic example. Of the 28 patients, five had an SPO of more than 15° postoperatively. In these five patients, scoliotic curvature was well corrected and maintained but a residual SPO of more than 15° was observed (Table 2, Fig. 2). These five patients had an L5 tilt of more than 15° preoperatively. Figure 4 shows a radiographic example.
A 13-year 2-month-old boy (patient 6). a and b Preoperative sitting anteroposterior radiograph shows significant thoracolumbar curve of 72° and SPO of 25°. L5 tilt is 12°. Sagittal thoracic kyphosis is 10° and lumbar lordosis is 8°. c and d Postoperative sitting views show significant correction of scoliosis of 9° and SPO of 5°. L5 tilt is 5°. Good reconstruction of thoracic kyphosis and lumbar lordosis is achieved postoperatively
A 13-year 4-month-old boy (patient 2). a and b Preoperative sitting anteroposterior radiograph shows significant thoracolumbar curve of 95° and SPO of 38°. L5 tilt is 20°. Sagittal thoracic kyphosis is 8° and lumbar lordosis is only 0°. c and d Postoperative sitting views show significant correction of scoliosis, yet show an appreciable residual SPO of 22°. L5 tilt is 17°. Sagittal plane alignment is well created
The mean number of levels fused was 14.5 (range: 14–15). In the 28 patients, a total of 616 screws was placed safely with no reoperations for screw malposition. The mean number of screws per patient was 22. Clinically, there were no neurologic deficits or radicular symptoms.
There were five postoperative complications. All complications were paralytic ileus, occurring in five patients, which resolved with observation without oral intake in at least 48 h. There were no neurologic complications, instrumentation failure, pull out of fixation or infections. There were no reoperations for any reason, nor any second hospitalizations related to scoliosis surgery.
Discussion
Spinal deformity is almost universal and progressive in patients with DMD [7, 11, 19, 29, 33]. The posterior spinal fusion for neuromuscular scoliosis has been highly effective in stabilizing the spine and maintaining an upright and comfortable sitting balance [5, 9, 13].
The most recent instrumentation innovation for the treatment of scoliosis is the pedicle screw. To our knowledge, this study is the only reported series of consecutive cases of scoliosis in DMD treated with segmental pedicle screw instrumentation and fusion to L5. Excellent minimum 2-year results are shown in this study, with no reoperations for nonunion, infection or instrumentation failure. Radiographically, the coronal curves were flexible (78% compensation on preoperative best-effort spine side-bending radiographs) preoperatively and there was 81% coronal curve correction and normalization of sagittal plane postoperatively. Loss of correction was minimal at the last follow-up. Good pelvic balance was achieved and maintained in all but five patients.
In the surgical treatment of spinal deformity in DMD, strong anchors are needed because of increased loss of muscular stability in neuromuscular disorders that causes asymmetrical muscle balance leading to progression of spinal deformity [8, 38] and because of osteopenia in this population [6, 24, 38]. In addition, it is difficult to provide strong and stable fixation with hook or wire anchors [38]. Pedicle screws offer a better vertebral grip with three-column purchase and a longer moment arm due to the anatomic location of the pedicle screw as compared to other forms of spinal bone–implant interfaces such as hook placement on the laminar or sublaminar wires. The screws are immediately stable in all directions after insertion. The superior biomechanical advantages of pedicle screws over other forms of spinal bone–implant interfaces allow the correction technique to generate powerful corrective forces in all planes. Segmental pedicle screw instrumentation has been reported to offer a significant coronal curve correction and maintenance of correction in patients with adolescent idiopathic scoliosis [20, 36]. In addition, significant correction and maintenance of correction in sagittal plane alignment has been reported with the use of segmental pedicle screw instrumentation as compared to those with other forms of instrumentation in patients with adolescent idiopathic scoliosis [20, 36]. Although pedicle screws have been thought to carry a higher complication risk (particularly, potential for neurologic complications), many studies have reported no increased neurologic risk with pedicle screw fixation and confirmed that pedicle screw placement in the thoracic and lumbar spine can be performed with both accuracy and safety [20, 36, 38].
Most studies on scoliosis surgery in patients with DMD have dealt with spinal instrumentation using hooks, wires or hybrid constructs with pedicle screws in the lumbar spine. Sussman [37] reported 25 patients with neuromuscular scoliosis who were treated with Luque rod instrumentation and fusion to L5, with a 48% postoperative correction and 35% correction at the last follow-up. The preoperative curve size in that study was 67°. Whitacker et al. [38] reported 23 patients with neuromuscular scoliosis, who were treated with hybrid constructs using pedicle screws ending in the distal lumbar spine. The preoperative curve size in that study was 71°, with a 64% initial correction and 55% correction at the last follow-up. McCall and Hayes [23] reported 75% initial correction of scoliotic curvature and 69% correction at the last follow-up using the U-rod and fusion to L5. The curve size was 65°. They reported 76% initial correction of pelvic obliquity and 68% final correction. They also reported 80% initial correction of scoliotic curvature and 70% correction at the last follow-up using the unit rod and fusion to the pelvis. The curve size was 70°. They reported 80% initial correction of pelvic obliquity and 75% correction at the last follow-up. Our results compared favorably with those published data. There are few studies on the use of pedicle-screws-alone fixation for scoliosis in DMD. Hahn et al. [16] reported excellent results for the coronal deformity with 77% correction, both initially and long-term, using pedicle-screw-alone fixation to the pelvis (not segmental pedicle screw instrumentation). The mean preoperative curve size in that study was 44°. They reported 78% initial correction of pelvic obliquity and 80% correction at the last follow-up. Modi et al. [26] found that in patients with neuromuscular scoliosis, acceptable amounts of curve correction (a mean of 61% initial correction and 58% correction at the last follow-up) can be achieved and maintained with posterior-only pedicle screw instrumentation to the pelvis without anterior release procedure. The mean preoperative curve size in that study was 79°. They reported 45% initial correction of pelvic obliquity and 47% correction at the last follow-up. We have challenged the long-term belief that fusion to the pelvis can be avoided even in non-ambulatory patients with DMD. In the current study, the scoliotic curvature improved 80% from a preoperative mean of 73° to an immediate postoperative mean of 14° and a mean of 17° at the last follow-up. The pelvic obliquity improved 65% from a preoperative mean of 17° to a postoperative mean of 6°, and 6° at the last follow-up. However, four patients had pelvic obliquity of more than 15°, postoperatively.
Pelvic obliquity associated with scoliosis in DMD continues to pose one of the most challenging instrumentation problems there is [3, 10, 27]. Instrumentation and fusion to the sacrum/pelvis has been a mainstay in the treatment of spinal deformity in DMD since the development of intrailiac post and recommended to prevent and/or correct pelvic obliquity [1, 9]. However, controversy remains concerning the necessity of extending the implant constructs and fusion to the sacrum/pelvis [23, 30, 38]. In addition, pelvic fixation has certain disadvantages, including increased blood loss, longer operative time and technical difficulty [5, 10, 25, 36]. In addition, the sacrum and the pelvis in patients with DMD are often small and osteoporotic [4, 16].
With severe scoliotic curve and higher pelvic obliquity, suprapelvic fusion has shown higher loss of long-term correction, especially, of pelvic obliquity. However, there is growing evidence that adequate correction can be obtained and maintained by fusion to the distal lumbar spine or even short segment anterior instrumentation [12, 26, 38].
The L5/S1 articulation is normally a very stable joint secondary to traction exerted by the iliolumbar ligament and stability imparted by the disc complex (annulus fibrosis and anterior longitudinal ligament) [21, 34]. Therefore, with stable L5/S1 articulation, pedicle screw fixation into L5 should allow correction of pelvic obliquity [23]. Pelvic obliquity is due to the suprapelvic effects of scoliosis [38]. Therefore, addressing the spinal deformity must effectively correct pelvic obliquity. Frischut et al. [10] found pelvic obliquity was effectively corrected by correcting the spinal deformity. Wild et al. [39] noted a spontaneous correction of pelvic obliquity after the spinal deformity was adequately addressed. Thus, we have challenged the long-term belief that instrumentation and fusion to the sacrum/pelvis can be avoided even in non-ambulatory DMD patients. In all our patients, there was a significant improvement in the Cobb angle. Of the 28 patients, 23 had pelvic obliquity of less than 10° postoperatively and a good pelvic balance was achieved and maintained in these patients. However, five patients had pelvic obliquity of 15° postoperatively. These five patients had preoperative Cobb angles of 86°, 95°, 86°, 86° and 88°, respectively, and an SPO of 36°, 38°, 33°, 36° and 30°, respectively; in addition, they had a preoperative L5 tilt of 18°, 20°, 17°, 17° and 16°, respectively. They should have had fusion to the sacrum/pelvis.
The basis of successful treatment with instrumentation and fusion only to L5 appears to be a stable L5/S1 articulation. Some authors have noted that an L5 tilt of more than 15° represented an unstable L5/S1 joint complex caused by attenuation of the iliolumbar ligaments or the disc complex, or both, and consequently, would not support L5-based constructs [21, 34]. McCall and Hayes [23] documented that possible contraindications to instrumentation (using the U-rod) and fusion only to L5 included indication of L5/S1 instability as evidenced by an excessive L5 tilt of more than 15° and a lumbar curve with the apex at L3 or lower as a result of the inability to achieve an adequate number of distal fixation points. In the current study, all the patients had a curve with the apex at L2 or higher. Of the 28 patients, 23 with a preoperative L5 tilt of less than 15° had a postoperative pelvic obliquity of 10°, even if they had high pelvic obliquity preoperatively. However, five patients with pelvic obliquity of more than 15° postoperatively had an L5 tilt of 15° preoperatively.
Thus, with rigid segmental pedicle screw instrumentation and fusion only to L5, the pelvic obliquity, even if it was high, was effectively corrected and maintained within 10° by adequately addressing spinal deformity in patients with stable L5/S1 articulation as evidenced by a preoperative L5 tilt of less than 15°. Instrumentation and fusion to the sacrum/pelvis should be reserved for the patients with unstable L5/S1 articulation as evidenced by an excessive L5 tilt of more than 15° preoperatively.
The sagittal plane alignment was well recreated in our series. Correction of thoracic hypokyphosis was found, with a preoperative mean of 10° to a postoperative mean of 20°. With a postoperative mean of 35°, an excellent reconstruction of lumbar lordosis was achieved in all our patients. The change in the sagittal plane alignment reflected the intention to re-create a good sagittal profile. Adequate lumbar lordosis is important for good and balanced sitting in patients with DMD in whom flexion contractures of the hips and knees are often present.
There was no significant loss of correction or progression of scoliosis at the last follow-up. Some authors described a loss of correction with the Luque or hook instrumentation [8, 32], which was not the case when the U-rod, the unit rod or pedicle-screw-alone fixation systems were used according to other studies [3, 4, 23]. We suggest a diligent procedure during the exposure of the spinal posterior element to enhance an excellent arthrodesis. The lack of loss of correction in our series is felt to be due to the diligent procedure, which exposes a large surface area of contact within facets possibly permitting early facet arthrodesis. This is coupled with the use of anchors at every level providing true segmental fixation.
Instrumentation and fusion to L5 has been reported to decrease operating time and complexity, decrease blood and avoid injury to the sacrum/pelvis. In our series, this procedure could be accomplished with less exposure and less complexity, translating into decreased blood loss and decreased operating time. In our series of patients treated with fusion to L5, the L5/S1 articulation is preserved. The advantage of the mobile L5/S1 disc space includes absorption of much of the angular and rotational movement of the trunk during wheelchair activities. The presence of mobility at L5/S1 may assist in sitting and transfer activities. However, longer-term follow-up should be performed to determine whether segmental pedicle screw instrumentation and fusion only to L5 is adequate to maintain spinal alignment and pelvic balance and prevent junctional problems at the L5/S1 motion segment.
In our series of segmental pedicle screw instrumentation, every level was instrumented on at least one side and several vertebrae received two pedicle screws. Controversy may arise concerning the necessity of placing two pedicle screws at every level, especially for mild or moderate curves. Also, this method increases operating time and blood loss and represents a significant cost. It is important to provide strong and stable fixation in the lumbar spine. Strong anchors in the lumbar spine are needed. We believe pedicle screws should be placed bilaterally at every level in the lumbar spine to give a solid foundation, on which the rest of the spine may be held upright, well balanced, and without rotation, thus this helps to correct and maintain pelvic obliquity. However, we also think screw placement at every two or three levels in the thoracic spine may be sufficient in this patient population.
Conclusions
Segmental pedicle screw instrumentation and fusion to L5 was safe and effective in patients with DMD scoliosis with stable L5/S1 articulation as evidenced by a minimal L5 tilt of less than 15°, even though pelvic obliquity was relatively large. This method in appropriate patients can be a viable alternative to instrumentation and fusion to the sacrum/pelvis in the surgical treatment of DMD scoliosis.
Study limitations
Although the minimum 2-year results are encouraging, and there has been no significant deterioration in curve magnitude, pelvic obliquity or development of lumbosacral junctional instability and pain, it remains to be elucidated whether segmental pedicle screw instrumentation and fusion to L5 is adequate to maintain spinal and pelvic alignment and sitting balance and prevent junctional problems at the L5/S1 motion segment with a longer-term follow-up. Furthermore, the number of the patients, who had a preoperative L5 tilt of more than 15° and a postoperative pelvic obliquity of more than 10°, was too small. Therefore, it may be impossible to draw significant conclusions from the measurement of the L5 tilt in a small group of only five patients. However, this study shows the introduction of segmental pedicle screw instrumentation and fusion to increase the potential amount of curve correction and correction of pelvic obliquity in patients with DMD scoliosis.
References
Allen B Jr, Ferguson R (1982) The Galveston technique for L rod instrumentation of the scoliotic spine. Spine 10:276–284
Askin GN, Hallettv R, Hare N, Webb JK (1997) The outcome of scoliosis surgery in the severely handicapped child: an objective and subjective assessment. Spine 22:44–50
Basobas L, Mardjerko S, Hammerberg K, Lubicky J (2003) Selective anterior fusion and instrumentation for the treatment of neuromuscular scoliosis. Spine 28:S245–S248
Bell DF, Moseley CF, Koreska J (1989) Unit rod segmental spinal instrumentation in the management of patients with progressive neuromuscular spinal deformity. Spine 14:1301–1307
Benson ER, Thomson JD, Smith BG, Banta JV (1998) Results and morbidity in a consecutive series of patients undergoing spinal fusion for neuromuscular scoliosis. Spine 23:2308–2317
Bentley G, Haddad F, Bull TM, Seingry D (2001) The treatment of scoliosis in muscular dystrophy using modified Luque and Harrington-Luque instrumentation. J Bone Joint Surg Br 83:22–28
Bridwell KH, Baldus C, Iffrig TM, Lenke LG, Blanke K (1999) Process measures and patient/parent evaluation of surgical management of spinal deformities in patients with progressive flaccid neuromuscular scoliosis (Duchenne’s muscular dystrophy and spinal muscular atrophy). Spine 24:1300–1309
Daher Y, Lonstein J, Winter R, Bradford D (1985) Spinal surgery in spinal muscular atrophy. J Pediatr Orthop 5:391–395
Dias RC, Miller F, Dabney K, Lipton G, Thomas TT (1996) Surgical correction of spinal deformity using a unit rod in children with cerebral palsy. J Pediatr Orthop 16:734–740
Frischut B, Krismer M, Stoeckl B (2000) Pelvic tilt in neuromuscular disorders. J Paediatr Orthop B 9:221–228
Furumasu J, Swank SM, Brown JC, Gilgoff I, Warath SL, Zeller JL (1989) Functional activities in spinal muscular atrophy patients after spine fusion. Spine 14:771–775
Gaine WJ, Lim J, Stephenson W, Galasko CBS (2004) Progression of scoliosis after spinal fusion in Duchenne muscular dystrophy. J Bone Joint Surg Br 86:550–555
Galasko CBS, Delany C, Morris P (1992) Spinal stabilisation in Duchenne muscular dystrophy. J Bone Joint Surg Br 74:210–220
Granata C, Merlini L, Cervellati S (1996) Long term results of spine surgery in Duchenne muscular dystrophy. Neuromuscul Disord 6:61–68
Gupta MC, Wijesekera S, Sossan A, Martin L, Vogel LC, Boakes JL, Lerman JA, McDonald CM, Betz RR (2007) Reliability of radiographic parameters in neuromuscular scoliosis. Spine 32:691–695
Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K (2008) Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Euro Spine J 17:255–261
Heller KD, Wirtz DC, Siebert CH, Forst R (2001) Spinal stabilization in Duchenne muscular dystrophy: principles of treatment and record of 31 operative treated cases. J Pediatr Orthop B 10:18–24
Hsu JD (1983) The natural history of spinal curve progression in the nonambulatory Duchenne muscular dystrophy patient. Spine 8:771–775
Kennedy JD, Staples AJ, Brook PD, Parsons DW, Sutherland AD, Martin AJ (1995) Effect of spinal surgery on lung function in Duchenne muscular dystrophy. Thorax 50:1173–1178
Lowenstein JE, Hiroko Matsumoto, Vitale MG, Weidenbaum M, Gomez JA, Lee FY, Hyman JE, Roye DP (2007) Coronal and sagittal plane correction in adolescent idiopathic scoliosis—a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 32:448–452
Luk KD, Ho HC, Leong JC (1986) Iliolumbar ligament. J Bone Joint Surg Br 68:197–200
Marsh A, Edge G, Lehovsky J (2003) Spinal fusion in patients with Duchenne muscular dystrophy and a low forced vital capacity. Euro Spine J 12:507–512
McCall RE, Hayes B (2005) Long-term outcome in neuromuscular scoliuosis fused only to lumbar 5. Spine 30:2056–2060
McCord DH, Cunningham BW, Shono Y (1992) Biomechanical analysis of lumbosacral fixation. Spine 17:S235–S243
Miladi LT, Ghanem TB, Draui MM, Zeller RD, Dubousset JF (1997) Iliosacral screw fixation for pelvic obliquity in neuromuscular scoliosis. Spine 22:1722–1729
Modi HN, Suh SW, Song HR, Fernandez HM, Yang JH (2008) Treatment of neuromuscular scoliosis with posterior-only pedicle screw fixation. J Orthop Surg 3:23
Mubarak SJ, Morin WD, Leach J (1993) Spinal fusion in Duchenne muscular dystrophy and fusion to the sacro-pelvis? J Paediatr Orthop 13:752–760
Pehrsson K, Larsson S, Oden A (1992) Long term follow-up of patients untreated scoliosis. A study of mortality, causes of death, and symptoms. Spine 17:1091–1096
Rawlins BA, Winter RB, Lonstein JF, Denis F, Kubic PT, Wheeler WB, Ozolins AL (1996) Reconstructive spinal surgery in pediatric patients with major loss in vital capacity. J Pediatr Orthop 16:284–292
Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK (2002) Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine 27:2072–2079
Shapiro F, Specht L (1993) The diagnosis and orthopaedic treatment of inherited muscular diseases of childhood. J Bone Joint Surg Am 75:439–454
Sink EL, Newton PO, Mubarak SJ, Wenger DR (2003) Maintenance of sagittal plane alignment after surgical correction of spinal deformity in patients with cerebral palsy. Spine 28:1396–1403
Smith A, Koreska J, Mosley CF (1989) Progression of scoliosis in Duchenne muscular dystrophy. J Bone Joint Surg Am 71:1066–1074
Smucker JD, Miler F (2001) Crankshaft effect after fusion of and Unit Rod instrumentation in children with cerebral palsy. J Pediatr Orthop 21:108–112
Sticker U, Moser H, Aebi M (1996) Predominantly posterior instrumentation and fusion in neuromuscular and neurogenic scoliosis in children and adolescents. Euro Spine J 5:101–106
Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB (1995) Segmental pedicle screw fixation in the treatment of adolescent idiopathic scoliosis. Spine 20:1399–1405
Sussman MD (1984) Advantage of early spinal stabilization and fusion in patients with Duchenne muscular dystrophy. J Paediatr Orthop 4:532–538
Whitacker C, Burton D, Asher M (2000) Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with pedicle screw anchorage. Spine 25:2312–2318
Wild A, Haak A, Kumar M (2001) Is sacral instrumentation mandatory neuromuscular thoracolumbar scoliosis due to myelomeningocele? Spine 26:E325–E329
Acknowledgments
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript. Informed consent was obtained from the all patients before entering the study. Institutional review board approval of Kitasato University was obtained for this study.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takaso, M., Nakazawa, T., Imura, T. et al. Can the caudal extent of fusion in the surgical treatment of scoliosis in Duchenne muscular dystrophy be stopped at lumbar 5?. Eur Spine J 19, 787–796 (2010). https://doi.org/10.1007/s00586-010-1347-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-010-1347-4