Abstract

A 27-year-old woman presented with bilateral weakness of her all extremities for 5 years. She had a spastic gait and was unable to ambulate without assistance. Neurologic examination revealed increased deep tendon reflexes and positive pathologic reflexes. Radiographs showed occipitalization of the atlas, C2–C3 congenital fusion and fixed atlantoaxial dislocation with an atlanto-dental interval of 10 mm. MRI demonstrated cervicomedullary junction (CMJ) compression from the odontoid, a Chiari type I malformation, and syringomyelia extending from the foramen magnum to C5. The patient underwent transoral atlantoaxial release followed by posterior internal fixation from the occiput to the axis, which resulted in a significant improvement in motor function in all extremities. Post-operative images showed anatomical reduction of the atlantoaxial joint. However, an MRI performed 8 days following surgery showed a new retro-odontoid pannus had developed that was compressing the spinal cord at CMJ. A follow-up CT scan performed at 6 months post-operatively demonstrated a solid bony fusion between the occiput and C2, while an MRI at that time showed complete resolution of the retro-odontoid soft tissue mass with correction of the Chiari I malformation, and resolution of the syringomyelia. Final follow-up at 2-years revealed an excellent clinical outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Case presentation
A 27-year-old woman presented with a 5-year history of progressive weakness and numbness that began in her right extremities. Her symptoms progressed rapidly for the first year and eventually her entire right side became involved. When admitted, she complained of an unsteady gait requiring an assistive device to ambulate, and lacked coordination in her hands (impossible to button up her shirt). Neurologic examination of the lower extremities revealed normal sensation to light touch, pain and temperature, while sensory dysfunction of the upper limbs was present. Symmetrical hyperreflexia, as well as positive Hoffman’s and Babinski signs were present bilaterally. Weakness was present on both sides, with the right side being more severe. Her gait was wide-based, spastic, and unsteady. She also had limited range of motion on cervical in both flexion and extension. No other significant medical history was present.
Diagnostic imaging section
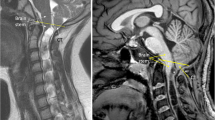
Plain and dynamic flexion extension radiographs demonstrated occipitalization of the atlas, C2–C3 congenital fusion and fixed atlantoaxial dislocation with an atlanto-dental interval of 10 mm (Fig. 1a, b). Complete reduction of the atlantoaxial joint was not achieved with neck extension (Fig. 1a). MRI showed that the cervicomedullary junction was being compressed by the odontoid, as well as evidence of a type I Chiari malformation, and a syringomyelia extending from the foramen magnum to C5 (Fig. 1c, d). CT scan showed migration of the odontoid process above the foramen magnum (Fig. 1e).
History, diagnostic, differential diagnosis, epidemiology
Syringomyelia occurs in conjunction with Chiari I malformation (CMI) in 50–76% of patients [1]. The presence of concomitant bone abnormalities is rarely reported, but its incidence is often underestimated and importance overlooked. Patients with these bone abnormalities have a high failure rate after simple decompression without fusion [5]. It is important that these underlying pathologies are carefully understood before treatment. Menezes stated that in craniocervical anomaly (like atlas assimilation) cases, further developmental and acquired phenomenon may supervene, producing basilar invagination.
Osseous anomalies of the craniovertebral junction (CVJ) are believed to arise during weeks 4 and 12 of gestation, during which the occipital bone and vertebrae originate from sclerotomes in the mesoderm and differentiation ensues [2].
In Menezes’ study of 2,200 child cases [5], primary BI formed a very large group consisting of atlas assimilation in 75%, the Klippel–Feil syndrome in 72%, hindbrain herniation in 50%, and hydromyelia in 18%. In Goel’s series of 163 syringomyelia cases, 133 had BI and 4 had atlantoaxial dislocation (AAD). In his another study, 46% (88/190) of basilar invagination (BI) cases had AAD. In a series of 364 patients with symptomatic CMI, Milhorat et al. [7] reported (BI) in 12%, atlas assimilation in 5.2%, and the Klippel–Feil anomaly in 4.9%. Such disparity has probably several reasons, such as different including criteria, surgeon’s clinical experience and the use of more accurate preoperative examinations (CT and MRI).
Conditions such as trauma, congenital anomalies, and inflammatory arthritis can lead to instability. Without early intervention, instability at this segment may progress to dislocation. Dislocations that can be reduced by using skull traction are referred to as reducible atlantoaxial dislocations, while those dislocations that are unable to be reduced with skeletal traction, even with the assistance of general anesthesia and complete muscle relaxation, are referred to as fixed or irreducible atlantoaxial dislocation (IAAD) [9].
The underlying cause of syringomyelia is an alteration in physiologic cerebrospinal fluid (CSF) flow dynamics. The principle etiology of CMI is an overcrowding of the hindbrain in an underdeveloped posterior cranial fossa. In contrast, different pathology exists in syringomyelia associated with AAD. Goel and Menezes have stated that some of BI cases are associated with a reducible subtype of atlantoaxial dislocation (AAD). Menezes [2] stated that when associated with AAD cases, concomitant hindbrain herniation may be a secondary etiology. In his opinion, atlas assimilation is a predisposing factor to AAI. In AAI and IAAD cases, the odontoid shifts posteriorly and rostrally, which compresses the CMJ. This can lead to posterior fossa overcrowding and interruption of the CSF circulation, which can then induce syringomyelia as a tertiary etiology.
Comprehensive preoperative evaluation is critical for making an accurate diagnosis and making an appropriate treatment. Flexion/extension plain radiographs are necessary to assess CMJ stability. Menezes [5] also suggested that dynamic cervical lateral radiography, CT reconstructions and dynamic MRI be obtained. CT reconstructions help clearly define the osseous anomalies, while dynamic MRI evaluates the extent of ventral and dorsal cervicomedullary compression.
Rationale for treatment and evidence based literature
Treatment of syringomyelia with IAAD and/or BI is still controversial. Several treatment options have been reported described below.
Conservative treatment
Resolution of syrinx had been reported by traction for syringomyelia with BI. But the fusion is still needed to maintain the result.
Decompression
Posterior fossa decompression (PFD) with/without fusion
Isolated PFD can effectively treat many cases of BI and syringomyelia; however, iatrogenic AAI after repeated PFD has been reported [4]. An adverse outcome can occur in approximately 35–40% of patients treated with a dorsal decompression with a fixed AAD at CVJ [5]. Several authors [2, 4] added fusion to maintain regional stability. PFD has recently been replaced by anterior decompression for the ventral compression.
Anterior decompression by odontoidectomy (via transoral or lateral approach)
Menezes has the largest series study of transoral odontoidectomy for the treatment of IAAD. Recently posterolateral approach [8] and endoscopic approach [10] (transnasal transclival or standard anterior cervical approach) have also been reported, but literature on these techniques is limited to several case reports making them difficult to evaluate. Promising results have been reported for transoral decompression, but there are several inherent disadvantages in case of syringomyelia with AAD. (1) In AAD, especially IAAD, the odontoid is shifted posteriorly and rostrally inhiniting clear visualization. Even more extensive exposure, such as soft and/or hard palate splitting or extended maxillotomy, might be needed to achieve the direct vision of the odontoid. With limited exposure in this deep operative field, complete odontoid resection can be challenging for surgeons. Several reports have documented residual posterior odontoid cortex following these procedures. (2) The medulla is more vulnerable when removing the posterior cortex, since there is little space between the odontoid and the medulla in this dislocated position. (3) Transoral decompression itself may also worsen atlantoaxial stability, leading to increases in translation and range of motion (ROM) in all movements except axial rotation. Worsening of BI as a result of transoral odontoidectomy has also been reported. Goel [4] had reported ten cases required reoperation for recurrent brainstem compression and three cases with progressive BI following transoral odontoidectomy which improved with distraction and fixation. (4) Removal of the lower clivus and/or superior C2 vertebral body may be required to achieve optimal decompression in severe BI cases. However, excessive removal of the C2 vertebral body may preclude the use of short segmental fixation due to insufficient bony purchase.
Reduction
AAD/AAI appears the primary etiology. The treatment strategy in AAD cases with syringomyelia should emphasize reduction of the dislocation and stabilization of the atlantoaxial joint. Although, IAAD is referred to as irreducible, reduction can be obtained in most cases [9]. Based on his experience with 5300 cases, Menezes [6] provided a decision tree for treatment with reducibility as the goal. This tree seems need revision since most IAAD could be changed into reducible.
Posterior reduction
Goel [3] described the use of atlantoaxial joint distraction to reduce BI in IAAD with/without syringomyelia. He used cranial traction to reduce the dislocation and atlantoaxial lateral mass fixation with bilateral spacer placed between atlantoaxial lateral joint to maintain realignment. It is unclear whether the syrinx resolved because postoperative MRIs were not obtained. This technique has several inadequacies. In the presence of kyphosis, it is the anterior contraction of the muscles, ligaments and capsules of lateral mass joint that prevent reduction, which can not be easily released from a posterior approach. In Goel’s procedure, it is mandatory to resect the C2 nerve ganglion and the venous plexus at this level. This is technical demanding and results in permanent numbness along the distribution of the greater occipital nerve [3, 4].
Anterior reduction
Anterior reduction has been reported by two independent authors. Anterior reduction by anterior soft tissue release is quite similar to the transoral odontoidectomy, but less aggressive.
Under general anesthesia and continuous skull traction, exposure is performed with the transoral approach. The bilateral musculatures and anterior longitudinal ligament are transected. The capsule of the atlantoaxial lateral mass joint and the articular adhesions are resected. At this point, the majority of reduction can be obtained. When necessary, improved reduction can be achieved with resection of the anterior arch of C1 and soft tissue release between the odontoid and C1 (transverse ligament and granulation tissue). The reduction can be maintained and further achieved by posterior fixation. In Wang’s series of 33 IAAD cases [9], 26 (79%) obtained complete anatomical reduction. Some authors reported similar result but with anterior release and anterior fixation.
Fixation and fusion techniques
Menezes et al. [2] have demonstrated the necessity of fusion in cases of syringomyelia with hindbrain herniation.
External fixation
Halo-vest immobilization was the traditional treatment, but it provided limited control of atlantoaxial stability, and more rigid fixation methods were introduced.
Semi-rigid fixations
Gallie and Brooks techniques, as well as combinations of these, have been used for atlantoaxial fixation. Menezes et al. [2] also described occipitocervical fusion with titanium loop and cable instrumentation following posterior fossa decompression.
Rigid fixations (posterior and anterior)
Magerl’s transatlantoaxial screw, C1 lateral mass screw and C2 pedicle screw construct, occipitocervical screw fixation have all been shown to provide better immediate postoperative stability. These techniques provide short segment fixation and reserve more cervical mobility, but they are also technical demanding and expensive.
In conclusion, the pathological mechanism of syringomyelia with IAAD and BI is still not clearly demonstrated. Bony abnormalities should not be overlooked. The BI could be subdivided into two groups: a congenital group which requires bony decompression and an AAD group which requires reduction. The syrinx cavity can often be relieved without direct decompression in AAD subtype cases. Some IAAD could be reduced with anterior transoral soft tissue release. The surgical choice should be individualized and based on comprehensive preoperative imaging and surgeon experience.
Surgical procedure
Following induction of general anesthesia, the patient was placed in Trendelenburg position, with the head in hyperextension using skeletal traction (8 kg, less than one-seventh body weight). Atlantoaxial reduction remained unsuccessful after 10 min, and the atlantoaxial dislocation was classified as IAAD. A tracheostomy was then performed. We inserted a transoral retractor, and a rubber catheter was placed through the nostril and sutured to the uvula. Traction on the catheter allowed us to move the uvula and soft palate out of the operative field (Fig. 2a). Dissection of bilateral longus coli and longus capitis muscles, and the anterior longitudinal ligament was performed, followed by partial resection of the C1 anterior arch. Soft tissue releases were performed between the odontoid and C1, removing the apical and alar ligaments with a curette. The curette was placed at the posterior-superior border of the odontoid and pulled anteriorly and inferiorly to obtain an anatomic reduction (Fig. 2b). To maintain this reduction, a posterior occipitocervical fixation (C0–C2) was added (Fig. 2c).
Outcome
The patient experienced significant improvement in motor function of all extremities immediately following the operation. Post-operative radiographs showed anatomic reduction of the atlantoaxial joint (Fig. 3a, d); however, an MRI obtained 8 days following the operation showed that a new retro-odontoid soft tissue mass (arrow) appeared resulting in mild compression of the spinal cord (Fig. 3b, c).
Six months following the surgery, MRI showed continued reduction of the Chiari I malformation and near complete reduction of the syringomyelia. The retro-odontoid soft tissue mass disappeared with no spinal cord compression evident (Fig. 4b, c). X-ray and CT confirmed a solid fusion extending from the occiput to C2 (Fig. 4a, d). Two-year follow-up revealed a successful clinical outcome as she was able to return to her previous work as a farmer.
References
Ergün R, Akdemir G, Gezici AR, Tezel K, Beskonakli E, Ergüngör F, Taskin Y (2000) Surgical management of syringomyelia–Chiari complex. European Spine J 9:553–557
Fenoy AJ, Menezes AH, Fenoy KA (2008) Craniocervical junction fusions in patients with hindbrain herniation and syringohydromyelia. J Neurosurg Spine 9:1–9
Goel A (2004) Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine 1:281–286
Goel A (2005) Progressive basilar invagination after transoral odontoidectomy treatment by atlantoaxial facet distraction and craniovertebral realignment. Spine 30:E551–E555
Menezes AH (2008) Craniovertebral junction database analysis: incidence, classification, presentation, and treatment algorithms. Childs Nerv Syst 24:1101–1108
Menezes AH (2008) Craniocervical developmental anatomy and its implications. Childs Nerv Syst 24:1109–1122
Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, Speer MC (1999) Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery 44:1005–1017
Oya S, Tsutsumi K, Shigeno T, Takahashi H (2004) Posterolateral odontoidectomy for irreducible atlantoaxial dislocation: a technical case report. Spine J 4:591–594
Wang C, Yan M, Zhou HT, Wang SL, Dang GT (2006) Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine 31:E306–E313
Wu JC, Huang WC, Cheng H (2008) Endoscopic transnasal transclival odontoidectomy: a new approach to decompression: technical case report. Neurosurgery S1:92–94
Acknowledgment
The authors thank Dr. Kirkham B. Wood for the help in manuscript editing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, S., Wang, C., Yan, M. et al. Syringomyelia with irreducible atlantoaxial dislocation, basilar invagination and Chiari I malformation. Eur Spine J 19, 361–366 (2010). https://doi.org/10.1007/s00586-009-1208-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1208-1