Abstract
Cervical pedicle screw fixation is an effective procedure for stabilising an unstable motion segment; however, it has generally been considered too risky due to the potential for injury to neurovascular structures, such as the spinal cord, nerve roots or vertebral arteries. Since 1995, we have treated 144 unstable cervical injury patients with pedicle screws using a fluoroscopy-assisted pedicle axis view technique. The purpose of this study was to investigate the efficacy of this technique in accurately placing pedicle screws to treat unstable cervical injuries, and the ensuing clinical outcomes and complications. The accuracy of pedicle screw placement was postoperatively examined by axial computed tomography scans and oblique radiographs. Solid posterior bony fusion without secondary dislodgement was accomplished in 96% of all cases. Of the 620 cervical pedicle screws inserted, 57 (9.2%) demonstrated screw exposure (<50% of the screw outside the pedicle) and 24 (3.9%) demonstrated pedicle perforation (>50% of the screw outside the pedicle). There was one case in which a probe penetrated a vertebral artery without further complication and one case with transient radiculopathy. Pre- and postoperative tracheotomy was required in 20 (13.9%) of the 144 patients. However, the tracheotomies were easily performed, because those patients underwent posterior surgery alone without postoperative external fixation. The placement of cervical pedicle screws using a fluoroscopy-assisted pedicle axis view technique provided good clinical results and a few complications for unstable cervical injuries, but a careful surgical procedure was needed to safely insert the screws and more improvement in imaging and navigation system is expected.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The concept of pedicle screw fixation for mid- and lower cervical spine reconstruction was introduced by Abumi et al. [1], who along with others have reported good clinical results and relatively low rates of complications from this procedure [1–3, 20, 22]. However, because it has the potential to seriously injure the spinal cord, nerve roots or vertebral arteries, pedicle screw fixation has generally been considered a risky surgery [18]. For cases in which posterior wiring or lateral mass plating cannot be applied, transpedicular fixation may provide optimal stabilisation for an unstable motion segment [6, 19, 21]. Therefore, when the safety of the procedure is ensured, cervical pedicle screw fixation could become an effective procedure for reconstructing the cervical spine.
Previous anatomical studies have demonstrated that the small diameter of mid-cervical pedicles, large obliquity of the cervical pedicle axis and individual variations in cervical pedicle size limit the application of pedicle screws for cervical spine stabilisation [10, 15, 17, 20]. Nevertheless, broad guidelines have been developed to successfully locate the entry point for cervical pedicles on the lateral mass [1, 2, 8, 11], and the rate of successful screw placement may be as high as 87.5% [16]. Because of the lack of landmarks and an accurate entrance to the cervical pedicles, direct exposure of the pedicle cavity [1], foramino-laminotomies [7, 15] and the use of expensive stereotactic image-guided systems or computed tomography (CT) [13] have been suggested as the ways to improve the accuracy of screw placement.
There are only a few reports that have described methods for the accurate insertion of pedicle screws and clinical complications that may arise following the procedure. Locating an accurate entry point for screws as well as determining the correct screw trajectory angle in the horizontal plane is crucial factors for the safe insertion of the screws within the pedicle cortex.
The purpose of this study was to investigate the efficacy of a fluoroscopy-assisted imaging technique (pedicle axis view) in accurately placing pedicle screws to treat unstable cervical injuries, and the ensuing clinical outcomes and complications.
Materials and methods
Patients
From 1995 to 2006, 144 consecutive patients (125 males and 19 females; mean age 44.1 years, range 14–90 years) with unstable cervical spine injuries underwent posterior spine arthrodesis and placement of pedicle screw instrumentation. The types of fractures and dislocations were categorised according to the mechanistic classification of Allen et al. [4]. Of the 144 cases, 81 were distractive flexion (DF) injuries, 25 were compressive flexion (CF), 27 were compressive extension (CE), 7 were vertical compression (VC) and 4 were distractive extension (DE). The patients’ neurological status was graded according to the ASIA classification system. There were 57 cases of ASIA A, 8 of ASIA B, 23 of ASIA C, 36 of ASIA D and 20 of ASIA E.
We performed preoperative radiography (AP, lateral and oblique views), CT and magnetic resonance imaging (MRI). Pedicle morphology and the medial inclination of the pedicle axis were fully evaluated on examination. MR angiography and/or CT angiography were recently obtained in most of the cases to observe patency of vertebral artery.
The surgeries were performed by one of the three attending spine surgeons, who were well experienced with the thoracolumbar pedicle screw fixation. Four different instrumentation systems were used: axis screw fixation (99 cases), Olerud cervical system (3), Vertex system (1) and OASYS system (42).
The patients began postoperative rehabilitation within a few days of removal of the postoperative drain. A Philadelphia collar was worn for approximately 1 month, but no external fixation was applied to the patients with ASIA A or B neurological deficit.
Neurological complications were assessed by reviewing preoperative, immediate postoperative and follow-up neurological examinations. Postoperative infection and vascular complications were evaluated by reviewing operative reports, patients’ medical records and clinical notes. Instrumentation failure was reviewed using postoperative radiographs and CT scans. Bony union was investigated with flexion–extension radiographs at the final follow-up. The sagittal alignment of the cervical vertebrae around the injured segment was measured on pre- and postoperative lateral radiographs.
Surgical procedure
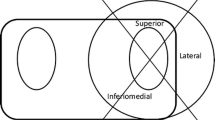
All patients were placed on a Relton–Hall frame with their skull fixed in a Mayfield 3-point fixator and the cervical spine was positioned parallel to the floor. Shoulder girdles were pulled caudally and fixed by taping. A multiplanar fluoroscope was rotated so that an approximate circular portion of the pedicle cortex wall could be visualised in the transverse plane of the vertebral body, and the axis of rotation was set to the cervical longitudinal axis (Fig. 1). The screw insertion point was located at the centre of the circle on the cervical lateral mass (Fig. 2). The inclined axis of the fluoroscope showed that the pedicle axis matched with the insertion point. Usually, the axis inclines from 30° to 55° from the mid-sagittal plane (C2–7) [10, 15, 17, 20] (Fig. 3). Due to a larger inclination of the screw trajectory would require further surgical exposure, we employed a trajectory angle of 30°–35° from the sagittal plane. An entry hole was created with an awl, and a fine pedicle probe with a blunt tip was inserted through the entry hole into the pedicle cavity. Kirschner wires were inserted into the pedicle holes, and the accuracy of the trajectory angle was confirmed on lateral and pedicle axis views using a fluoroscope. If they did not provide the correct pathway, probing was reattempted. Subsequently Kirschner wires were reinserted into the pedicles and the accuracy of the trajectory angle was confirmed again. Tapping was performed before inserting the pedicle screws. For the mid- and lower cervical spine, we used 3.5-mm (diameter) × 20–22 mm (length) screws. Anatomical lordosis was created by bending the plates (axis) or rods (Olerud, Vertex or Oasys). Decortication of the facets and lateral masses were performed with a burr, and chips of local bone from spinous processes were grafted into the facets and onto the lateral masses. In this study, all procedures were performed manually so that the surgeon could acquire tactile feedback. No power drilling was used to avoid injury to the neurovascular structures.
Postoperative assessment of screw placement
The accuracy of the placement of the pedicle screws into the medial/lateral pedicle walls was evaluated on axial CT scans (2-mm slices), whereas superior/inferior pedicle wall screw location was examined on oblique radiographs. The position of the cervical pedicle screws was assessed by an independent radiologist. Incorrect screw placement was classified as either screw exposure or pedicle perforation. A screw was exposed if it broke the pedicle wall, but more than 50% of the screw diameter remained within the pedicle. A pedicle perforation occurred if a screw breached the pedicle wall and more than 50% of the screw diameter was outside the pedicle. The latter indicated a potential risk for neurovascular injury (Fig. 4).
Results
The mean operative time was 101 min (range 52–228 min) and the mean blood loss was 190 ml (range 10–2,100 ml). Four anterior reconstructive surgeries with iliac bone grafts and 11 posterior decompressive surgeries were performed simultaneously. Local sagittal alignment of the vertebrae around the injured lesion measured 6.8° of kyphosis preoperatively and 6.0° of lordosis at the last follow-up. Six hundred twenty pedicle screws were used in total; 57 (9.2%) demonstrated screw exposure and 24 (3.9%) exhibited pedicle perforation. Of these 81 screws, 24 (30%) breached the medial pedicle wall, 56 (69%) the lateral wall, and 1 (1%) the infralateral wall (Table 1). The screw malposition was most seen at C5 level (28/153 screws) and 26 of those 28 screws aimed lateral.
Four patients died of renal failure (n = 1), pneumonia (n = 2), or pulmonary embolism (n = 1) within 2 months of surgery. All of these patients suffered from ASIA A neurological injury above C5 level. The remaining 140 patients were followed up for more than 6 months after surgery.
There were two cases with intraoperative complications: one case with a penetration of the pedicle probe into the vertebral artery and one with transient radiculopathy. The bleeding from the vertebral artery was easily stopped with bone wax and there were no further complications. Because this patient had pedicle and articular process fractures caused by the presenting trauma, it was difficult to control the trajectory of the probe into the pedicle during surgery; however, radicular pain was gradually relieved with time. Nine postoperative complications occurred: two cases associated with the loss of correction due to instrumentation failure (screw breakage and dislodgement), three cases with loss of correction (more than 10°) and four deep wound infections. These five cases with instrumentation failure or correction loss were treated with screw–plate system (non-constrained fixation). The postoperative deep infection was successfully managed by surgical debridement, continuous irrigation and intravenous administration of antibiotics without the need to remove the hardware. Good cervical vertebrae alignment was maintained at final follow-up in 135 of the 140 patients (96%).
Finally, the bony fusion was obtained in all cases. Pre- and postoperative tracheotomy was required in 20 (13.9%) of the 144 patients. Because the patients underwent posterior surgery alone without postoperative external fixation, the tracheotomies were easily performed.
Illustrative case
A 38-year-old man incurred a C5–7 fracture and dislocation (CE stage 5, Allen classification [4]) and an ASIA A neurological deficit. Sagittal and axial CT images showed C5–7 lamina fracture, left C5 and right C6 pedicle fracture, and C7 vertebral body fracture (Fig. 5a, b). Posterior open reduction, Halo vest fixation and tracheotomy due to respiratory failure were conducted in the regional hospital near the trauma site. After arriving at our hospital, a CT scan demonstrated good alignment and a tracheal tube anterior to the cervical spine. We performed C5–7 pedicle screw fixation (Fig. 5d). The patient started his rehabilitation a day following the surgery without external fixation. A postoperative CT scan showed good placement of the pedicle screws within the pedicle cortex (Fig. 5e).
Imaging studies of an illustrative case. Preoperative sagittal and axial image of CT shows C6/7 fracture—dislocation, C5–7 lamina—vertebral body separation and left C5 and right C6 pedicle fracture without displacement (a, b). Good alignment after open reduction and a tracheal tube anterior to the cervical spine are seen on another sagittal image (c). Postoperative AP and lateral radiograph show good alignment and C5–7 pedicle screw fixation (d). Postoperative CT scans show good placement of pedicle screws at C5, C6, C7 levels (e)
Discussion
Cervical pedicle screw fixation has been shown to be the most stable form of cervical instrumentation [9, 12, 14]. However, due to the close proximity of the spinal cord, nerve roots and vertebral arteries, this type of surgery is generally considered too risky. Only a few reports have discussed the clinical application of placing cervical pedicle screws in the C3–6 region. The purpose of the present study was to investigate the accuracy of screw placement using a fluoroscopy-assisted pedicle axis view technique and evaluate the clinical outcomes and complications of the procedure for treating unstable cervical injuries.
In this study, cervical pedicle screw fixation provided good correction of sagittal alignment, a high-fusion rate and only a few surgical complications. However, we have experienced two cases of instrumentation failure and three cases of large correction loss using screw–plate system. We found that it was much easier to perform a tracheotomy in patients treated with posterior cervical pedicle screw fixation than in those treated with anterior cervical surgery or Halo vest fixation.
Anatomically, the cervical pedicle diameter is smaller than the thoracolumbar pedicle, and the pedicle axis is largely inclined in the transverse plane [10, 15, 17, 20]. Successful placement of pedicle screws requires an accurate identification of the pedicle axis. If an accurate entry point that coincided with the correct trajectory angle is determined during surgery, it would vastly improve the accuracy of screw placement. In the conventional technique, the screw entry point was determined through a small hole, which was made with a high-speed burr, to locate the inner wall of the pedicle [1]; however, a larger hole was sometimes necessary to accomplish this task, but a larger hole could create a cortical defect in the lateral mass and result in decreased screw stability within the pedicle.
Fluoroscopic lateral imaging was recommended in a study describing the conventional technique [1], but this method only provides information regarding the vertical plane and not the horizontal plane. Sometimes in lateral images, the pedicles in the lower cervical spine are difficult to visualise due to the overlying shoulders, but we had no such problem in locating the correct entry points using the pedicle axis view technique. Although cadaver studies have described detailed surface landmarks for a posterior cervical pedicle entrance [11, 15], the cervical lateral masses have small bony undulations that differ from the thoracic or lumbar spine. In fact, during surgery, there are fewer morphometric landmarks than in cadaver demonstrations [15]. Furthermore, the location of the pedicle entrance is unique to each level of the cervical vertebra and large variations are found amongst individuals even at the same vertebral level [11, 15].
The fluoroscopy-assisted pedicle axis view technique helped to determine the appropriate entry point that coincided with the correct trajectory angle for each cervical vertebra in both sagittal and transverse planes. The strength of this technique is indicating both inserting point and trajectory angle of screws at the same time. If each of them is not correct, pedicle perforation are likely to occur. Using this technique, our rate of pedicle perforation was lower than that reported for the conventional technique (3.9 vs. 6.7%) [2]. Screw malposition was seen most at C5 level. Screw malposition is likely seen in lateral side at C5 level and medial side in C2. It is necessary to keep the anatomical difference at each level [10, 17].
Pedicle screw fixation in the cervical spine has been considered a serious risk to the surrounding structures. Roy-Camille stated that the placement of transpedicular screws into the C3–6 pedicles would be an unacceptable risk for injury to the vertebral artery, spinal cord and nerve roots [18]. However, in this study, there were no spinal cord injuries, one transient root injury and one vertebral artery penetration. Despite the several clinically silent pedicle perforations, performing the procedure manually caused only a few neurovascular complications and one case of nerve root injury that demonstrated gradual recovery over time. Vertebral artery bleeding was stopped by bone wax, and fortunately set up no postoperative symptoms. Injury to bilateral vertebral arteries might cause serious problems such as cerebral infarction or death. When the occlusion of unilateral vertebral artery is seen preoperatively, the insertion of pedicle screws in the remaining side should be avoided. In such case, pedicle screw fixation in the occluded side and lateral mass screw fixation in the remaining side are recommended. Pedicle screw fixation is strong and useful procedure, but should be avoided in the risky cases with pedicle fracture or angioplany of vertebral artery.
Because CT scanning produced a metal artefact around the screws and periodically produced an exaggerated screw outline, it was somewhat problematic to correctly identify a location for proper screw placement, but using axial CT scanning with 2-mm slices improved our accuracy.
A computer-guided surgical navigation system has been reported to improve the accuracy of screw placement [5, 13, 16] but these systems are cumbersome and time-consuming and some, based on the preoperative CT imaging, have no utility following the reduction of a fracture and/or a dislocation. Furthermore, owing to their high cost and user unfriendliness, these systems are not installed in most hospitals. It is hoped that in the near future, a more accurate, user-friendly and real-time navigation system will be developed for clinical practice.
We believe, as do surgeons with extensive clinical experience, that the best tool for providing safe and accurate pedicle screw placement is the spinal surgeons’ intimate knowledge of cervical anatomy [2, 15]. Owing to the possibilities of serious risks, this procedure should not be performed easily. Surgeons must select better procedure for each patient with cervical trauma, evaluating risks and benefits of each procedure.
Conclusions
In the present study, pedicle screw fixation provided good reduction, a high-fusion rate and relatively few complications. Of the 620 cervical pedicle screws, 57 (9.2%) demonstrated screw exposure and 24 (3.9%) pedicle perforation. Hence, using the fluoroscopy-assisted pedicle axis view technique for determining the appropriate pedicle screw entry point that coincides with the correct trajectory angle should improve the accuracy and safety in cervical pedicle screw placement.
References
Abumi K, Itoh H, Taneichi H, Kaneda K (1994) Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord 7(1):19–28. doi:10.1097/00002517-199407010-00003
Abumi K, Kaneda K (1997) Pedicle screw fixation for nontraumatic lesions of the cervical spine. Spine 22(16):1853–1863. doi:10.1097/00007632-199708150-00010
Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K (2000) Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine 25(8):962–969. doi:10.1097/00007632-200004150-00011
Allen BL Jr, Ferguson RL, Lehmann TR, O’Brien RP (1982) A mechanistic classification of closed, indirect fractures and dislocations of the lower cervical spine. Spine 7(1):1–27. doi:10.1097/00007632-198200710-00001
Assaker R, Reyns N, Vinchon M, Demondion X, Louis E (2001) Transpedicular screw placement: image-guided versus lateral-view fluoroscopy: in vitro simulation. Spine 26(19):2160–2164. doi:10.1097/00007632-200110010-00024
Benzel EC, Kesterson L (1989) Posterior cervical interspinous compression wiring and fusion for mid to low cervical spinal injuries. J Neurosurg 70(6):893–899
Ebraheim NA, Xu R, Knight T, Yeasting RA (1997) Morphometric evaluation of lower cervical pedicle and its projection. Spine 22(1):1–6. doi:10.1097/00007632-199701010-00001
Jeanneret B, Gebhard JS, Magerl F (1994) Transpedicular screw fixation of articular mass fracture-separation: results of an anatomical study and operative technique. J Spinal Disord 7(3):222–229. doi:10.1097/00002517-199407030-00004
Jones EL, Heller JG, Silcox DH, Hutton WC (1997) Cervical pedicle screws versus lateral mass screws: anatomic feasibility and biomechanical comparison. Spine 22(9):977–982. doi:10.1097/00007632-199705010-00009
Karaikovic EE, Daubs MD, Madsen RW, Gaines RW Jr (1997) Morphologic characteristics of human cervical pedicles. Spine 22(5):493–500. doi:10.1097/00007632-199703010-00005
Karaikovic EE, Kunakornsawat S, Daubs MD, Madsen TW, Gaines RW Jr (2000) Surgical anatomy of the cervical pedicles: landmarks for posterior cervical pedicle entrance localization. J Spinal Disord 13(1):63–72. doi:10.1097/00002517-200002000-00013
Kotani Y, Cunningham BW, Abumi K, McAfee PC (1994) Biomechanical analysis of cervical stabilization systems: an assessment of transpedicular screw fixation in the cervical spine. Spine 19(22):2529–2539
Kotani Y, Abumi K, Ito M, Minami A (2003) Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg Spine 99(3 Suppl):257–263
Kothe R, Ruther W, Schneider E, Linke B (2004) Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine 29(17):1869–1875. doi:10.1097/01.brs.0000137287.67388.0b
Ludwig SC, Kramer DL, Vaccaro AR, Albert TJ (1999) Transpedicle screw fixation of the cervical spine. Clin Orthop Relat Res 359:77–88. doi:10.1097/00003086-199902000-00009 (Review)
Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ (2000) Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine 25(13):1655–1667. doi:10.1097/00007632-200007010-00009
Panjabi MM, Shin EK, Chen NC, Wang JL (2000) Internal morphology of human cervical pedicles. Spine 25(10):1197–1205. doi:10.1097/00007632-200005150-00002
Roy-Camille R (1991) Rationale and techniques of internal fixation in trauma of the cervical spine. In: Errico T, Bauer RD, Waugh T (eds) Spinal trauma. JB Lippincott, Philadelphia, pp 163–191
Roy-Camille R, Saillant G, Laville C, Benazet JP (1992) Treatment of lower cervical spinal injuries—C3 to C7. Spine 17(10 Suppl):S442–S446. doi:10.1097/00007632-199210001-00017
Sakamoto T, Neo M, Nakamura T (2004) Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine 29(22):2510–2514. doi:10.1097/01.brs.0000144404.68486.85 discussion 2515
Swank ML, Sutterlin CE 3rd, Bossons CR, Dials BE (1997) Rigid internal fixation with lateral mass plates in multilevel anterior and posterior reconstruction of the cervical spine. Spine 22(3):274–282. doi:10.1097/00007632-199702010-00009
Yukawa Y, Kato F, Yoshihara H, Yanase M, Ito K (2006) Cervical pedicle screw fixation for 100 cases of unstable cervical injuries using pedicle axis views by fluoroscopy. J Neurosurg Spine 5(6):488–493. doi:10.3171/spi.2006.5.6.488
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yukawa, Y., Kato, F., Ito, K. et al. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J 18, 1293–1299 (2009). https://doi.org/10.1007/s00586-009-1032-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1032-7