Abstract
Multilevel cervical spine procedures can challenge the stability of current anterior cervical screw-and-plate systems, particularly in cases of severe three-column subaxial cervical spine injuries and multilevel plated reconstructions in osteoporotic bone. Supplemental posterior instrumentation is therefore recommended to increase primary construct rigidity and diminish early failure rates. The increasing number of successfully performed posterior cervical pedicle screw fixations have enabled more stable fixations, however most cervical pathologies are located anteriorly and preferably addressed by an anterior approach. To combine the advantages of the anterior approach with the superior biomechanical characteristics of cervical pedicle screw fixation, the authors developed a new concept of a cervical anterior transpedicular screw-and-plate system. An in vivo anatomical study was performed to explore the feasibility of anterior transpedicular screw fixation (ATPS) in the cervical spine. The morphological study was conducted based on 29 cervical spine CT scans from healthy patients and measurements were performed on the pedicle sizes, angulations, vertebral body depth, height and width at C2 to T1. Significant morphologic parameters for the new technique are discussed. These parameters include the sagittal and transverse intersection points of the pedicle axis with the anterior vertebral body wall, as well as the distances between sagittal intersection points from C2 to T1. On the basis of these results, standard spine models were reconstructed and used for the conceptual development of a preclinical release prototype of an anterior transpedicular screw-and-plate system. The morphological feasibility of the new technique is demonstrated, and its indications, biomechanical considerations, as well as surgical prerequisites are thoroughly discussed. In the future, the technique of cervical anterior transpedicular screw fixation might diminish the number of failures in the reconstruction of multilevel and three-column cervical spine instabilities, and avoid the need for supplemental posterior instrumentation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In cervical traumatic, degenerative, and pathologic disorders, the problem frequently lies anteriorly and the anterior approach is commonly preferred to address these disorders with the use of anterior cervical interbody grafts/cages combined with plates [8, 31].
The anterior is more atraumatic than the posterior approach and complications are rare [15, 38]. There is no damage to the paravertebral muscles, and it allows for anterior instrumentation as far as T1 [34]. However, in anterior cervical spine surgery following one-level three-column injuries [16, 38, 103] or multilevel discectomies/corpectomies [7, 18, 22, 37, 39, 63, 82, 92, 93, 101] the biomechanical stability of current anterior cervical spine screw-and-plate systems is limited. Salvage operations as well as some primary intended plated reconstructions need supplemental posterior stabilization, hence a second surgical approach with its potential risks of increased morbidity and complications [5, 12, 27, 37, 54, 81].
Although the ideal stiffness of a cervical spine construct for a certain clinical situation and the number of corpectomy levels mandating combined anterior and posterior fixation is not known [46, 54, 58, 84], the fusion and complication rates at the anterior cervical spine have been shown to have a direct correlation to the mechanical stability of the fixation, and it seems that anterior plate length is predictive of failure [35, 41, 54, 61, 71]. On the other hand, posterior stabilization using posterior cervical pedicle screw (pCPS) fixation is the technique with highest primary stability [84]. The increased stability particularly gains importance in multilevel and severe traumatic three-column instabilities. In order to avoid additional posterior stabilization in patients who undergo anterior reconstructive surgery, an anterior cervical spine implant which offers higher primary stability in selected patients is desirable.
We performed an extended review of the literature concerning the superior biomechanical characteristics [45, 58, 59, 84], and clinical success of pCPS fixations [1–3, 50, 76, 107] with increasing safety utilizing CAS and ISO-C-3D fluoroscopy [42, 43, 57, 77]. Based on available anatomical data in the literature [10, 14, 17, 23, 24, 46, 49, 64, 68, 80, 95, 98] we investigated the requirements that would be necessary to develop a morphologically shaped design of a preclinical release prototype of an AnteriorTransPedicularScrew(ATPS)–plate system. Measuring specific anatomical parameters on fine CT scans, we conducted a quantitative evaluation of the morphology of the cervical spine regarding its feasibility for ATPS insertion. From data derived we calculated ‘Standard Spine Models’ resembling the anatomical general set-up for ATPS insertion and developed the concept for the first ATPS–plate system.
The anatomical feasibility and restrictions of ATPS insertion, as well as the biomechanical considerations, indications, and principales in designing implants accomodating ATPS are discussed the first time. With a quantitative understanding of the cervical pedicle and vertebral morphology at different spinal levels in light of ATPS, it should be possible to conduct further laboratory studies on this new field of cervical spine stabilization.
Methods
The cervical spine CT scans of 29 patients admitted to an emergency department (Katharinenhospital Stuttgart, Stuttgart, Germany) were evaluated as the basis of our study. There were 20 male and 9 female patients. Mean age was 44.8 years (18–81). The cervical spines were free from tumor, deformity, fracture and severe osteoporosis. CT scans with advanced degenerative changes were excluded. All studies were performed on the same CT scanner (LightSpeed Plus, General Electric, USA) using a 15- to 18-cm detail field of view, axial slice thickness of 1.0 mm, slice spacing of 1.25 mm, and pitch of 0.75. Coronal and sagittal reconstructions of the axial images were generated using standard algorithms and stored digitally. Using the cursor, digital CT measurements (0.1 mm increments) were performed with a customized shaped software (Escape Medical Viewer V3, Escape Thessaloniki, Greece). The parameters and distances used during the measuring process are illustrated in Fig. 1 and Table 1.
It is to be explained that in sagittal plane, the lsIP and rsIP, and in transverse plane, the ltIP and rtIP, respectively, resemble conceivable entry points for anterior transpedicular screws (ATPS) into the left and right pedicles, respectively. The entry points resemble the projection of the center of a corridor formed by the cervical pedicles onto the anterior vertebral cortex, both in coronal and sagittal plane. As with lsIP and rsIP, mean data of ltIP and rtIP at the levels C3–T1 were visualized to explain their meaning for insertion of ATPS (Fig. 2). At the axis body, the former parameters were not measured, as C2 is obviously not suitable for ATPS. The lsIP and rsIP at C2 resembling entry points for common vertebral body screws were arbitrarily set 10 mm above the axis endplate. The distances between sagittal intersection points were measured along the anterior cervical column and could be angled and interrupted at the superior and inferior corner of each vertebral body using a polygon measuring tool. Hence, the software used allowed us to take into account the lordotic curvature of the cervical spine. Regarding measurements of ltIP and rtIP, those pedicle axis which crossed the mid-sagittal line were scaled as ‘positive’ values, and those intersecting the anterior vertebral body lateral to mid-sagittal line were scaled as ‘negative’ values. Regarding measurements of lsPA and rsPA, values >90° direct cephalad in relation to the anterior vertebral body wall.
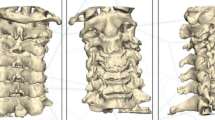
Computer model depicts projection of cervical pedicle axis with rsIP and rtIP on the anterior surface of vertebral bodies C3–C5 and C6–T1. The center cross from cephalad to caudad at C3–C5 and C6–T1 resembles mean data of rsIP and rtIP, and as such the conceivable entry points for ATPS into the right pedicles. The ellipsoid spots (blue, red, green) surrounding the center cross resemble the standard deviations for rsIP and rtIP
From axial and reconstructed images it is difficult to determine the real anatomical pedicle axis and to measure its length [14]. We measured the pedicle axis length (PAL) from the anterior border of the vertebral body through the center of the pedicle and lateral mass in transverse plane. The software used enabled tracking the PAL in different axial planes. Hence, the real PAL, e.g., at C6 slightly from postero-superior to antero-inferior in relation to the anterior vertebral cortex, could be measured closer to its real anatomical course (Fig. 4).
In order to discuss the clinical feasibility of ATPS insertion and to enable developing prototype designs of an ATPS-plate with its holes incorporating transpedicular screws, ‘Standard Spine Models’ were calculated from average data of all patients and interlevel distances between sagittal intersection points C2–T1 (DlsIPCx+Cx+1/DrsIPCx+Cx+1, see Table 1), respectively. These ‘Standard Spine Models’ mark the varying distances between sagittal intersection points, which resemble the entry points for ATPS and the center of a screw perforation at the ends of a plate to be designed, respectively. Calculations were performed for each conceivable combination of vertebrae to be instrumented between C2 and T1. The distance between sagittal intersection points at each level was added by 1 mm for the vertebral disc as a factor for the height restoring by use of a graft/cage. Based on the calculated ‘Standard Spine Models’ from average data of all patients, additionally four models according to ±1 and 2 SD for each conceivable combination of vertebrae to be instrumented were calculated. It should be noted that a conceivable ATPS-plate, at its ends, can incorporate cannulated ATPS unilateral, and a vertebral body screw triangulated adjacent but beneath the ATPS on the contralateral side (Fig. 4). Both the distances of the center of plate holes in sagittal plane, as well as the size and location of plate holes in frontal plane would have to respect the varying interlevel differences, which are evaluated in our study.
Descriptive statistics including mean values, standard deviations and ranges were used to summarize data. A repeated measures ANOVA was used in which the factor ‘cervical level’ with factor levels C2–T1 was measured on the same individual. Gender was used as ‘between-subjects’ factor to compare males and females. Post hoc comparisons were done to compare different factor levels. Categorized whisker plots with 95% confidence intervals for the means were constructed to illustrate the corresponding effects. P < 0.05 was considered statistically significant. All analyses were done with Statistica 6.1 (StatSoft, Inc., 2004, Tulsa, USA).
Results
Analysis of data showed homogenous results, in which only three individuals, one female and two male, depicted large anatomical dimensions on CT scans. The CT data pool comprised 203 cervical vertebrae. The process of measuring resulted in a total of 3,712 parameters which are described as mean, SD, and ranges in Tables 2, 3, 4, 5, 6 and 7.
There were no statistically significant interlevel differences in aVBH, VBD, and VBW between male and female patients, but between aVBH of C2 and C3 for both gender (P < 0.00001). There was an increase from C5 to T1 for aVBH and VBD, and from C4 to T1 for VBW, respectively (Table 2). Measurements of PAL showed statistically significant differences only between the levels C2 and C3 (P = 0.03). There was a slight decrease in magnitude of pedicle angulations in transverse plane from C4 to T1, whereas statistically significant differences of ltPA and rtPA calculated from merged data of all 29 patients existed between the levels C2 and C3 (P = 0.03), C3 and C4 (P = 0.03), and between C6 and C7 (P = 0.02) (Table 3). With the lsPA and rsPA C3–T1 there were no significant gender- or side-related, and no significant interlevel differences. From the anterior vertebral body cortex, the pedicle axis increased upwards from C3 to C6 (94°–111°) with a following slight decrease from C6 to T1 (111°–103°; Table 3).
Concerning outer pedicle width (OPW) of all patients, there were no significant differences between left and right sides (Table 4). However, merging left and right OPW, gender as well as vertebral level was proven as a statistically significant factor (P = 0.00035, P = 0.00001; Graph 1). With post hoc analyisis, OPW at T1 was shown to be significantly larger in males than in females (P = 0.028). The OPW showed the tendency to increase from cephalad C5 to caudad T1 in males, and from C4 to T1 in females (Graph 1). Significant differences in males were observed between OPW of C2 and C3 (P = 0.0003), C5 and C6 (P = 0.016), C6 and C7 (P = 0.00001), and C7 and T1 (P < 0.00001). In females significant differences were observed between the levels C2 and C3 (P = 0.01), C4 and C5 (P = 0.048), C6 and C7 (P = 0.027), and C7 and T1 (P < 0.00001). The frequency of OPW below 5 mm was 31.0% at C3, 39.7% at C4, 38.0% at C5, 20.7% at C6, 0% at C7 and T1. The frequency of OPW below 4 mm was 10.3% at C3, 5.2% at C4, 5.2% at C5, 0% at C6, C7 and T1. With OPH, all but one pedicle showed measurements larger than 5.0 mm
Concerning OPH of all patients, there were no significant differences between left and right sides, however gender was also proven as a statistically significant factor (P = 0.017, Table 5). Statistical analysis revealed significant differences in males between OPH of C2 and C3 (P = 0.08), C4 and C5 (P = 0.01), C6 and C7 (P = 0.00005), and C7 and T1 (P < 0.00001). In females significant differences were observed between C6 and C7 (P = 0.01), and C7 and T1 (P < 0.00001). Merging left and right OPH, there was a tendency towards a decrease of OPH from C2 to C5 in males and from C2 to C6 in females with a reversal increase in males from C5 to T1, and in females from C6 to T1.
There were no meaningful gender related differences (P = 0.195) in merged data of left and right interlevel distances between sagittal intersection points C2 to T1 (DlsIPCx+Cx+1 and DrsIPCx+Cx+1; Table 6). Significant differences between the interlevel distances of sagittal intersection points from cephalad to caudad C2–T1 existed between the levels C2–C3 and C3–C4 for both gender (P < 0.00001, Table 6) which was a factor of the determined starting point for measurements at C2. Statistically significant differences in males existed also between C6–C7 and C7–T1 (P = 0.0026), and in females between C4–C5 and C5–C6 (P = 0.006).
The sagittal intersection points resemble the projection of the center of the cervical pedicles onto the anterior vertebral cortex marking the theoretical entry points for 3.5 or 4.0 mm diameter cannulated ATPS (Fig. 2). Mean distances from adjacent disc spaces and cephalad endplates, respectively, to the sagittal intersection points are compiled in Table 7. In general, to ensure safe screw placement 0.5 mm of bone around each screw was determined as the critical value, and a safe entry point for placement of a 3.5 mm screw was assumed to be 2.25 mm (1.75 + 0.5 mm) [47] off. Accordingly, to select an entry point and to place a 3.5 or 4.0 mm ATPS with its head and the proximal outer rim of a plate (1 mm) close to, but beneath an adjacent disc space, at least an error margin of 3.25 and 3.5 mm, respectively, must be ensured. Using anatomical trajectories of pedicles axis for measuring the lsIP and rsIP, the frequency of those lsIP and rsIP with a distance below 4 mm to its adjacent cephalad disc space was 79.7% at C3, 58.6% at C4, 24.1% at C5, 5.2% at C7, and 1.7% at T1. These data has to be put into perspective to increased OPH compared to OPW. E.g., mean OPH of all C3- and C4-pedicles was both 7.3 mm. Mean sagittal angle of pedicle axis was 94.3° and 103.9° at C3 and C4, respectively. Hence, clinically there is a wider corridor in the sagittal plane to place a 3.5 or 4.0 mm pedicle screw inside the pedicles and sufficiently beneath adjacent disc spaces, as done with pCPS insertion [1].
Our calculations showed that measurements of DlsIP and DrsIP were not significantly different between male and female patients (Table 7). Therefore, we used the average data of all of our patients for designing the ‘Standard Spine Models’ (Table 8). Calculation of the ‘Standard Spine Models’ ±1 and 2 SD (five ‘Standard Spine Models’) according to the interlevel distances between sagittal intersection points in all 29 patients revealed that for, e.g., a static ATPS–plate system with fixed plate hole perforations, at least 105 different plates sizes would have to be designed. Derived from our data, in a conceivable ATPS–plate set (one- to six-level plates) designed according to the distances between the center of plate holes of the five calculated ‘Standard Spine Models’ for each conceivable plate length in between the levels C2–T1 to be instrumented, the remaining gap between two plate sizes next to each other (see Table 8, maximum of values in brackets) would be 3.2 mm in one-level plates, 5.8 mm in two-level plates, 8.4 mm in three-level plates, 10.8 mm in four-level plates, 12.9 mm in five-level plates, and 14.5 mm in six-level plates. But, using a screw–plate- and not a screw–rod-system, the holes of the plate would have to fit always exactly the given location of a placed k-wire and the following cannulated ATPS in transverse and sagittal plane in all individuals. Hence, only by using a translation mechanism could these these gaps be approximated. A plate design with a translation mechanism would have to compensate for the individual variations in interlevel distances.
If the axis vertebra is excluded from calculating the ‘Standard Spine Models’ ±1 and 2 SD, the differences between calculated distances of plate hole perforations for one-, two-, three-, four-, and five-level plates at C3–T1 vary only by 2 mm. Thus, the total number of anatomically shaped plates could be reduced. From this point of view, with a translation mechanism allowing for shifting of the ends of a plate towards each other and allowing for some overlap between different plate sizes, as well as including those individuals with smallest and largest distances between sagittal intersection points, a translation mechanism would have to enable translation of about 3 mm in one-level, 5.5 mm in two-level, 8 mm in three-level, 11 mm in four-level, and 13 mm in five-level plates for instrumentation between C3 and T1. Due to this, the number of plates need to accommodate ATPS fixation in all individuals would be 25 for instrumentations C3–T1, and 30 for C2–T1. When designing the length adjusted plates about 1–2 mm will need to be added at either end of a plate to accommodate the screw holes at the projected intersection points. Total plate length C x − Cx+(1–6) is the calculated distances between intersection points, plus 1 mm added to each vertebral disc as a factor for the height restoration caused by using an inter-body fusion cage device or graft, plus the 1–2 mm either end required for production of a stable plate, plus half the diameter of an ATPS plate hole perforation.
Measurement of distances between ltIP and rtIP referred to mid-sagittal line (DltIP and DrtIP, Table 7) demonstrated that the +95% confidence interval was highest at C4 with 3.63 mm and the −95% confidence interval lowest at C7 with −2.41 mm. Only three individuals showed their transverse intersection points more than 5 mm lateral to one side of the mid-sagittal line. For better understanding, means and SD for ltIP/rtIP and lsIP/rsIP are visualized in Fig. 2. The pedicle axes do not necessarily intersect each other in the anterior part of the vertebral body. Accordingly our data for DltIP and DrtIP (Table 7) showed averages of −0.67 to +2.77 mm, with a maximum ranging from −10.38 to +8.19 mm concerning all patients, and with a maximum ranging between −7.01 to +8.19 mm excluding one large individual. Although ranges tended to be large, there were no significant interlevel, male versus female, or left versus right differences detected. The mean distances measured between mid-sagittal line and ltIP/rtIP shifted slightly from contralateral to mid-sagittal line of the measured pedicle axis at C3–C6 and towards the ipsilateral side at C7–T1 (Fig. 2). Most often pedicle axes not crossing the mid-sagittal line at the anterior vertebral body wall were observed at the caudal levels C7–T1, whereas at C6 and C7 the maximum distances of ltIP and rtIP to mid-sagittal line were observed. Due to midline crossing of the pedicle axis, insertion of ATPS is possible (mainly) unilaterally. As ltIP and rtIP resemble the varying entry points for ATPS in transverse plane, a static or translational plate design, as well as a platform–rod-system [9], will have to respect the individual variations of entry points in transverse and sagittal plane, by adjustment of the hole geometry, as well as the distances between the center of plate hole perforations. Concerning the differences of DltIP and DrtIP in designing an anatomical shaped ATPS–plate system, its screw holes have to respect the aforementioned facts. This process of adaptation results in an asymmetrical location of oval holes in the horizontal plane at the cephalad and caudal ends (Fig. 3) according to the DltIP/DrtIP at each cervical level. Hence, one side of an ATPS-plate (the left or right one) will show a cephalad oval hole in transverse plane of about 10 mm lenght and a round plate hole perforation to accommodate an adjacent vertebral body screw. To place the plate with its longitudinal axis close to mid-sagittal line, its caudal transverse counterpart hole, oval in shape, will be situated more closely to the mid-sagittal line in those plates designed for instrumentation at C6–T1.
Computer model depicts a conceivable design of an ATPS–plate system with asymmetrical plate holes proximally and distally, respecting asymmetric entry points for ATPS at C3–T1. Here, a conceivable design of a four-level instrumentation, e.g., C4–T1, is depicted. At the end-levels, proximal oval hole perforations are located, e.g., more left sided for an ATPS directing rightwards, and circular and slightly oval holes proximal and distal, respectively, directing leftwards for triangulated anterior vertebral body screws. Midsection of the plate marks space for a conceivable translation mechanism. With the plate enabled to translate the proximal towards the distal plate holes according to given entry points of the ATPS will support its clinical feasibility. The insertion of 3.5–4.5 mm ATPS will follow the insertion of a k-wire placed albeit parallel to the endplates to be instrumented. Afterwards, an ATPS-plate is chosen adjusted to the length of levels to be instrumented and translation is performed. Due to the oval holes, the differing entry points of the k-wires cranially and caudally in transverse plane can be compensated due to translation of the plate more medially or laterally along the longitudinal axis
As in the study by Ugur et al. [99], female individuals were underdistributed in our series with a male to female ratio of 1:0.45. However, significant gender related differences in creating ‘Standard Spine Models’ for ATPS, which were our most important calculations, did not exist. We derived data from a population of European origin. Differences in specimen from other continents have to be taken into account when comparing our results.
Discussion
Indications for ATPS
There are worthwhile reasons for attempting to invent an immediately rigid technique of anterior fixation in the cervical spine [12]. Despite adequate intraoperative construct stability, some series concerning ACPS in subaxial traumatic instabilities report the incidence of re-displacement or loss of alignment at 19% [38], or 50% in patients with ankylosing spondylitis [28], the incidence of redo surgeries with 11–20% [16, 38], and the need for posterior supplemental stabilization with 10–15% [16, 103]. Hence, increased stability with anterior-only instrumentations would be advantageous in highly unstable cervical spine injuries. In turn, reconstruction of the multilevel decompressed cervical spine is required in degenerative disorders, infections and deformities, and tumor related instabilities [6, 18, 54, 72, 90]. If multilevel ACDF is not feasible, corpectomy plus adjacent level discectomies and discontinous corpectomies with retention of an intervening body, respectively, has been successfully performed at three or more motion segments [5, 13, 29, 54]. But, some cases demand multilevel corpectomies. Unfortunately, long strut grafts or cages used for reconstruction are known to be biomechanically inferior [89] and vulnerable to failure requiring revision [18, 19, 37, 79, 97]. Surgical complications and construct failures encountered with plated long-segment strut grafts increase with the number of corpectomized levels [9, 13, 18, 30, 62, 71, 78, 81, 93, 97, 101] and the literature provides evidence that anterior-only constructs particularly in more than two-level corpectomies [12, 18, 37, 82, 92, 101] do show a cause for concern regarding failure rates. A review of literature [54] showed that the rate of non-unions in multilevel ACDF and failure rates for long-length decompressions/corpectomies is as high as 20–50%, and up to 30–100%, respectively. About 30–50% of complications in multilevel cases are due to graft/cage and instrumentation related causes and carry a significant reoperation rate, which is reported as being between 10–50% [12, 36, 54]. Therefore, biomechanical studies [21, 32, 41, 52, 59, 69, 84, 88, 89] and clinical series [6, 65, 79, 85, 102] support the addition of posterior stabilization in multilevel procedures improving the early and long-term stability. Besides multilevel fusions for degenerative diseases, a body of clinical situations, including tumor related three-column instability, severe osteoporosis or ankylosing spondylits, call for combined anterior–posterior stabilization [6, 28, 54, 91, 100]. From the point of view of measuring techniques, combined antero-posterior stabilization leaves no doubts, particularly in long corpectomy cases [20, 32, 46, 52, 58, 84, 88], yielding fusion rate of 100% without construct failures for three- and four-level surgeries [54, 79, 85, 87, 102]. However, with the biomechanical advantage of supplemental posterior stabilization comes the addition of a second approach, added surgical risks, and a higher rate of infection. Posterior procedures with cervical dissection can cause significant myofascial pain due to the stripping of the musculature from the posterior elements and can be associated with significant postoperative axial symptoms and neck pain [5, 54, 66, 72, 87]. Hence, further development of the ATPS technique with an anterior-only treatment strategy could overcome the aformentioned drawbacks while serving the benefit of transpedicular construct anchorage. Part 1 of this article obviously depicts the field of clinical settings in which an ATPS–plate sytem would be a valuable tool. The ATPS technique is not sought as a replacement of common techniques for daily cervical spine surgery, but a technical adjunct for select cases. Due to transpedicular three-column fixation, the ATPS-technique could merge the biomechanical merits of current pCPS fixations with the surgical benefits of anterior-only procedures.
Morphological feasibility of ATPS
Morphometric measurements based on CT scans compared to manual calliper measurements are proven efficient to determine pedicle dimensions [14, 47, 49, 86]. CT scans avoid possible deviations by post mortem changes such as dehydration and altered tonus of the soft tissue that might change the disc height [48]. In our study, measurements of sagittal and transverse intersection points defining the possible entry points for ATPS were recorded, which is not possible using direct calliper measurements. Nevertheless, to put our data in perspective, one has to accept that morphometric measurements between different observers [64], techniques, and populations from different continents vary to some extent (see Table 9), and that qualitative inter- and intralevel changes in pedicle morphology, even along their axes, can alter results of measurements [70].
The anatomic feasibility of ATPS at C3–T1 is based on the multitude of studies considering the quantitative morphology of human cervical spine. The VBD determines the antero-posterior diameter for a vertebral body screw. In our study VBD of C2–T1 showed a mean of 16.8 mm in males and 16.2 mm in females (Table 2). Concerning in- and exclusion of C2 or T1 into calculations, the results are similar to those of Kwon et al. [60] for C3–C7 (17.1 and 15.2 mm, respectively) and those of Ebraheim et al. [25] for C2–C7 (15.5 and 14.7 mm, respectively). According to our measurements, intendend to enable designing an ATPS–plate system, unicortical vertebral body screws could be inserted triangularly with lengths of 16–18 mm.
For ATPS, the midbody VBW determines the anterior work-space in coronal plane for screw placement and restricts the width of a plate. Average VBW at C2–T1 in horizontal plane was 25.3 mm for males and 23.3 mm for females (Table 2). Data for C3–C7 were similar to those of Kwon et al. [60] (24.6 and 23.0 mm, respectively). To allow for plate positioning even lateral to the mid-sagittal line, the width of an ATPS-plate could be 16–18 mm. In our study mean aVBH at C3–T1 was 15.8 mm for males and 14.9 mm for females (Table 2), similar to data of Oh et al. [67]. The data depict sufficient work-space for insertion of an ATPS and an adjacent vertebral body screw into each vertebra to be instrumented at C3–T1 (Fig. 4).
Photo model depicts the principles of ATPS fixation. Left one depicts sagittal plane of C6 vertebra; right one depicts transverse plane of C6 vertebra from cryosections. Note transverse intersection point of ATPS with anterior vertebral body close to mid-sagittal line, insertion of ATPS albeit parallel to upper vertebral endplate in sagittal plane, and crossing configuration of ATPS and vertebral body screw in transverse plane, respectively. Asterisk marks vertebral artery. Cryosections with kindly permission from A. Kathrein, M.D., University of Innsbruck/Austria
Our means for OPW that based on CT-scan measurements are comparable to data previously published [14, 49, 80] using similar techniques. Excluding data from Ludwig et al. [64], direct measurements reported in literature are smaller. But, our mean OPW at C2 was smaller than in other studies reviewed [56] which refers to the varying definitions of the ‘surgical C2-pedicle’ used. As in the current study, there were no significant differences between left and right OPW and OPH, as reported in literature [10, 64, 70, 73] and the OPW was found to be larger in males than in females [14, 49, 70, 80]. But, the OPH was not consistently larger in males than in females. Panjabi et al. [68] noted that pedicle height was greater than its width for both left and right pedicles of each vertebra, resembling similar observations compared to our study and that of Kareikovic et al. [49]. The OPW was shown to slightly increase in males and females from cephalad (C3) to caudad (C7) [10, 26], whereas the most significant difference was found between OPW of C6- to T1-levels (5.8–8.6 mm) in our study. In addition to the overall mean of OPW, the frequency of the limiting transverse diameter of cervical pedicles for a pedicle screw insertion deserves attention: In a study of Chazono et al. [14] and Kareikovic et al. [49] the frequency of the OPW below 5 mm was 32.2 and 75.5% at C3, 30.1 and 35.8% at C4, 25.4 and 13.2% at C5, 15.9 and 13.2% at C6, and 1.6 and 6.6% at C7, respectively. Data of Chazono were roughly similar to our measurements, as it was the incidence of OPW with 3–4 mm in their study and that of Panjabi et al. [68]. Taking into account the means and calculating the frequencies depicts that ATPS fixation using 3.5–4.5 mm diameter screws would be appropriate at all levels only in selected patients, but feasible in most of the biomechanically challenged end-levels (C6–T1) of multilevel cervical constructs.
For the mean PAL, ranges were reported between 22 and 33 mm at C3–C7 [10, 49, 80]. In comparison, our mean PAL at each level was larger (Table 3). Notably, in comparison to previous studies [10, 49], our software enabled adapting the plane of transverse pedicle axis with respect to the cervical lordosis, which might explain that our PAL were larger. According to our data, ATPS for C3–T1 could show lengths of 20–40 mm, comparable to customized pCPS in use [75].
Measuring the tPA remains a concern, since determination of the pedicle axis is difficult especially with direct techniques [10, 49]. The tPA measured for pCPS insertion varies between a minimum mean of 36° for the male C7 pedicle to a maximum mean of 49° for the male C4 pedicle [49]. Our means for ltPA and rtPA were 2°–4° larger compared to previous studies [46, 49, 73]. Surgical recommendations for the angulation to be used in pCPS insertion at the C3 to C6 levels show a range of 40°–45° [44, 46, 64, 98]. Based on an ex vivo study of Sakamoto et al. [80], 50° was recommeneded as screws of 4.5 mm diameter would fit in all 120 vertebrae C3–C6 at 50° without violating the transverse foramen or spinal canal. We measured the tPA perpendicular to the diameter between transverse foramen and medial border of the pedicle. Our mean OPW were similar to that reported previously (Table 9), and the mean tPA was 48°. Hence, Sakamoto’s suggestion to choose a SAS-50° might be appropriate also for ATPS insertions.
We measured the lsPA and rsPA formed by the pedicle axis and a line drawn along the anterior vertebral body, as this angle would be that created between an ATPS and the anterior cervical plate. Our sagittal angulations measured are therefore not comparable to previous ones [10, 49, 68, 73], but correspond to those depicted in clinical practice with pCPS fixation [3, 75, 94]. Kareikovic et al. [49] found that C2 and C3 pedicles were directed superiorly compared with the inferior vertebral endplate, that C4 and C5 pedicles were parallel to it, and that C6 and C7 pedicles were inferiorly directed, sharing similar observations with other authors [14, 64, 68, 73]. However, clinically Abumi et al. [1] showed that paralleling the CPS according to the upper endplate in the sagittal plane is sufficient. In our study lsPA and rsPA were the lowest at the C3-level with a mean of 94°, that is an ATPS would to be directed slightly in cephalad direction in relation to the anterior vertebral cortex at C3. The associated lsIP and rIP showed a mean of 3 mm. As mentioned, the OPH height is mainly larger than the OPW. Therefore, a more steep cephalad directed trajectory for insertion of an ATPS is possible also at this level. Consecutively, the sagittal intersection points resembling the entry points of ATPS at these and other levels might be chosen more caudad in reference to the superior endplate of the instrumented vertebra if necessary. With the measurements of the distances of the sagittal and transverse intersections (lsIP and rsIP/ltIP and rtIP) the authors assessed the theoretical entry points for ATPS in to the vertebral bodies and pedicles, respectively. During insertion of ATPS using a manual, fluroroscipally assisted insertion technique, these data that can be derived from fine CT-scans to locate the starting points for a k-wire and cannulated screw, respectively.
The C2-morphology is not suitable for ATPS as mean lsPA and rsPA was 55.9° and 55.1° in an oral direction. An ATPS would have to be inserted transorally, which is not a realistic scenario when using an anterior retropharyngeal approach. We performed measurements including C2 to validate the whole data pool in comparison with data from literature (Table 9). Our results regarding the C2-pedicle dimensions (pars interarticularis of C2) are comparable to previous ones reviewed [56]. As with the use of common cervical plates, within a conceivable ATPS–plate-system the plate would accomodate vertebral body screws for insertion into C2 whilst allowing placement of ATPS at the caudad level. The reason why preferably one ATPS with an adjacent VBS at each level between C3 and T1 can be inserted with the ATPS technique is refered to the fact that in the horizontal plane and going from posterior to anterior the pedicles converge towards the midline with only the lower cervical levels (C6–T1) the pedicle axis intersecting anteriorly to the vertebral body or at its anterior edge [51, 55].
The authors measured the distance between the sagittal intersection points of the pedicle axis at the anterior vertebral cortex. These data have to be taken into calculation if one considers preclinical release prototyping of an ATPS-plate to evaluate biomechanical characteristics.
Biomechanical considerations for ATPS
Fusion rates in the spine have been shown to have a direct correlation to the mechanical stability of the fusion construct [35, 54, 61] with construct failure particularly in multilevel constructs most often occuring early during postoperative course [18, 54, 71]. Early failure depends on the immediate stability conferred by the construct [41] and relies on the mobility of the fused segments, screw purchase, alignment and load sharing achieved, the bone quality, and stabilizing potential of the construct [8, 32, 74]. With the ATPS-technique, enhanced screw anchorage by transpedicular fixation [45, 46, 59] would be of benefit to resist the axial pull-out forces that can compromise the screw–bone interfaces even with constrained screw–plate systems [83]. Serving for three-column pedicle screw fixation [11, 21] the ATPS technique would provide posterior column support but with use of an anterior-only approach. The current study on the OPW and OPH showed that all cervical pedicles from C6 to T1 would have been amenable to incorporate 4.5 mm diameter ATPS. In this context it is of note that the failure in multilevel ACDF or corpectomies is mostly observed at the end-levels of the constructs (the caudal more than the cephalad), where graft/cage subsidence and telescoping occurs, hardware fractures or levers off [4, 33, 39, 54, 69, 83, 104]. Up to 78% of multilevel fusions end at the CTJ (C7–T1) [40]. Boockvaar et al. [8] observed construct failures in 18% in fusions ending at the CTJ and pseudoarthrosis in 12%. Similarly, Wang et al. [104] observed a higher rate of graft migration in corpectomies involving a fusion ending at the C7 vertebral body. Conclusively, fusions ending at the lower cervical spine would in particular benefit from increased construct anchorage that would yielded by use of ATPS. Concerning an ATPS–plate-system, it is the author’s belief that two transpedicular constrained plate–screw fixations, proximally and distally, with two vertebral body screws will significantly increase construct stability in comparison to currently used screw–plate systems. This has the potentional of a clinical stability comparable to pCPS fixations, which in turn might reduce the incidence of postsurgical loss of alignment, construct failure, and diminish the need for postoperative orthotic wear in selected cases.
Surgical prerequisites for ATPS
The technique of CPS insertion was first described and further developed by Abumi et al. [1]. Since this time, increased usage and safety with cervical pedicle placement using manual and computer assisted techniques are documented in the spinal literature [105, 107]. The incidence of non-critical breaches was reported up to 100% and even though perforation of the transverse foramen occurs at times, the vertebral artery does not occupy the whole part of the foramen transversarium [56] with most pedicle wall perforations occurring non-critical [1, 50, 56, 94]. The cervical pedicles seem tolerant to some screw violations as many VA injuries go asymptomatic [2, 96, 106]. Nonetheless, with insertion of CPS and ATPS goes the risk of vertebral artery injury, which in turn can be fatal! But, as the use of CPS becomes more widespread with time and our knowledge base expands, the concerns regarding neurovascular injuries will be put into perspective. The issue of ATPS accuracy and savety will be further discussed in ‘Part 2’ of the ATPS-project.
Conclusion
The idea behind the ATPS–plate system lies in the desire to increase stability after reconstruction of highly unstable, particularly multilevel decompressed cervical spines in fractures, degenerative and neoplastic disorders. Before implementation of a new technique, the authors exposed and showed that the morphology of the cervical spine is feasible for ATPS insertion, suggesting that this technique is also clinically possible in selected vertebrae and patients. The authors also offered the anatomical template that enables preclinical release protoyping of an ATPS–plate system which in turn enables biomechancial testing of the whole construct prior to any clinical application. The surgical technique of ATPS and its accuracy will be evaluated with use of manual and computer-assisted insertion techniques. A three-column fixation device as with the ATPS–plate system could be a valuable tool with a biomechanical advantage in the surgeon’s armamentarium. Surgeons will have to consider the trade-off between the potential benefit of increased construct stability and avoiding added posterior surgery and the potential of neurovascular injury risk that goes with any cervical pedicle screw insertion technique.
Abbreviations
- ACP:
-
Anterior cervical plate(s)
- ACPS:
-
Anterior cervical plate stabilization
- ADD:
-
Adjacent disc degeneration
- ACDF:
-
Anterior (segmental) cervical decompression with fusion
- ATPS:
-
Anterior transpedicular screw(s)
- BMD:
-
Bone mineral density
- CAS:
-
Computer-assisted surgery
- CPS:
-
Cervical pedicle screw(s)
- CS-plate:
-
Constrained plate
- CTJ:
-
Cervicothoracic junction
- NC-plate:
-
Non-constrained plate
- SD:
-
Standard deviation
- VA:
-
Vertebral artery
References
Abumi K, Itoh H, Taneichi H, Kaneda K (1994) Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord 7:19–28
Abumi K, Shono Y, Ito M, Taneichi H, Kotani Y, Kaneda K (2000) Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine 25
Abumi K, Shono Y, Taneichi H, Itoh M, Kaneda K (1999) Correction of cervical kyphosis using pedicle screw fixation systems. Spine 24:2456–2462
Arnold PM, Eckard DA (1999) Four-level anterior cervical discectomy and fusion report of 18 cases with one-year follow-up. Presentation, Annual meeting CSRS-A
Ashkenazi E, Smorgick Y, Rand N, Millgram MA, Mirovsky Y, Floman Y (2005) Anterior decompression combined with corpectomies and discectomies in the management of multilevel cervical myelopathy: a hybrid decompression and fixation technique. J Neurosurg Spine 3:205–209
Bilsky MH, Boakye M, Collignon F, Kraus D, Boland P (2005) Operative management of metastatic and malignant primary subaxial cervical tumors. J Neurosurg Spine 2:256–264
Bolesta MJ, Rechtine DR II, Chrin AM (2000) Three- and four-level anterior cervical discectomy and fusion with plate fixation: a prospective study. Spine 25:2040–2056
Boockvaar JA, Philips MF, Telfeian AE, O’Rourke DM, Marcotte PJ (2001) Results and risk factors for anterior cervicothoracic junction surgery. J Neurosurg 94(Spine 1):12–17
Bose B (2003) Anterior cervical arthrodesis using DOC dynamic stabilization implant for improvement in sagittal angulation and controlled settling. J Neurosurg 98(Spine 1):8–13
Bozbuga M, Ozturk A, Ari Z, Sahinoglu K, Bayraktar B, Cecen A (2004) Morphometric evaluation of subaxial cervical vertebra for surgical application of transpedicular screw fixation. Spine 29:1876–1880
Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VKH, Papadopoulos SM, Crawford NR (2005) Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine 30:915–922
Brazenor GA (2007) Comparison of multisegment anterior cervical fixation using bone graft versus a titanium rod and buttress prosthesis. Spine 32:63–71
Casha S, Fehlings MG (2003) Clinical and radiological evaluation of the Codman semiconstrained load-sharing anterior cervical plate: prospective multicenter trial and independent blinded evaluation of outcome. J Neurosurg 99(Spine 3):264–270
Chazono M, Soshi S, Inoue T, Kida Y, Ushiku C (2006) Anatomical considerations for cervical pedicle screw insertion: the use of multiplanar computerized tomography reconstruction measurements. J Neurosurg Spine 4:472–477
Coe JD, Vaccaro C, Vaccaro AR (2004) Complications of anterior cervical plating. In: Clark CR (ed) The cervical spine, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 1147–1169
Daentzer D, Boeker D-K (2004) Operative stabilization of traumatic instabilities of the lower cervical spine. Experience with an angle unstable anterior plate–screw system in 95 patients. Unfallch 107:175–180
Datir SPD, Mitra SR (2004) Morphometric study of the thoracic vertebral pedicle in an indian population. Spine 29:1174–1181
Daubs MD (2005) Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine 30:1402–1406
DiAngelo DJ, Foley KT, Vossel KA, Rampersaud YR, Jansen TH (2000) Anterior cervical plating reverses load transfer in multilevel strut graft. Spine 25:2366–2376
Dmitriev AE, Kuklo TR, Lehman RA Jr, Rosner MK (2007) Stabilizing potential of anterior, posterior, and circumferential fixation for multilevel cervical arthrodesis. Spine 32:E188–E196
Do Koh Y, Lim TH, Won You J, Eck J, An HS (2001) A biomechanical comparison of modern anterior and posterior plate fixation of the cervical spine. Spine 26:15–21
Dorai Z, Morgan H, Cimbra C (2003) Titanium cage reconstruction after cervical corpectomy. J Neurosurg 99(Spine 1):3–7
Ebraheim NA, Fow J, Xu R, Yeasting RA (1998) The vertebral body depths of the cervical spine and its relation to anterior plate–screw fixation. Spine 23:2299–2302
Ebraheim NA, Xu R, Knight T, Yeasting RA (1997) Morphometric evaluation of lower cervical pedicle and its projection. Spine 22:1–6
Ebrahim NA, Fow J, Xu R, Yeasting RA (1998) The vertebral body depths of the cervical spine and its relation to anterior plate–screw fixation. Spine 23:2299–2302
Ebrahim NA, Xu R, Knight T, Yeasting RA (1997) Morphometric evaluation of lower cervical pedicle and its projection. Spine 22:1–6
Eichholz KM, Ryken TC (2003) Complications of revision spinal surgery. Neurosurg Focus 15, Article 1
Einsiedel T, Schmelz A, Arand M, Wilke HJ, Gebhard F, Hartwig E, Kramer M, Neugebauer R, Kinzl L, Schultheiss M (2006) Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine 5:33–45
Eleraky MA, Llanos C, Sonntag VKH (1999) Cervical corpectomy: report of 185 cases and review of literature. J Neurosurg 90(Spine 1):35–41
Elsaghir H, Bohm H (2000) Anterior versus posterior cervical plating in cervical corpectomy. Arch Orthop Trauma Surg 120:549–554
Epstein NE (2002) Reoperation rates for acute graft extrusion and pseudoarthrosis after one-level anterior corpectomy and fusion with an without plate instrumentation: etiology and corrective management. Surg Neurol 56:73–80
Foley KT, Di Angelo DJ, Rampersaud YR, Vossel KA, Jansen TH (1999) The in vitro effects of instrumentation on multilevel cervical strut-graft mechanics. Spine 24:2366–2376
Foley KT, Smith MM, Wiles DA (1997) Anterior cervical plating does not prevent strut graft displacement in multilevel cervical corpectomy. Presentation, Annual meeting CSRS-A, California
Fraser J, Diwan AD, Peterson M, O’Brien MF, Mintz DN, Khan SN, Sandhu HS (2002) Preoperative magnetic resonance imaging screening for a surgical decision regarding the approach for anterior spine fusion at the cervicothoracic junction. Spine 27:675–681
Greene DL, Crawford NR, Chamberlain RH, Park SC, Crandall D (2003) Biomechanical comparison of cervical interbody cage versus structural bone graft. Spine J 3:262–269
Greiner-Perth R, Allam Y, El-shagir H, Frank J, Boehm H (2006) Analysis of reoperations after surgical treatment of degenerative cervical spine disorders. A report on 900 cases. Eur Spine J 15(Suppl 4):S459
Hee HT, Majd ME, Holt RT, Whitecloud TS III, Pemkowski D (2003) Complications of multilevel cervical corpectomies and reconstruction with titanium cages and anterior plating. J Spinal Disord Tech 16:1–9
Henriques T, Olerud C, Bergman A, Jonsson Jr H (2004) Distractive flexion injuries of the subaxial cervical spine treated with anterior plate alone. J Spinal Disord Tech 17:1–7
Herrmann AM, Geisler FH (2004) Geometric results of anterior cervical plate stabilization in degenerative disease. Spine 29:1226–1234
Ikenaga M, Shikata J, Tanaka C (2005) Anterior corpectomy and fusion with fibular strut grafts for multilevel cervical myelopathy. J Neurosurg Spine 3:79–85
Isomi T, Panjabi MM, Wang JL, Vaccaro AR, Garfin SR, Patel T (1999) Stabilizing potential of anterior cervical plates in multilevel corpectomies. Spine 24:2219–2223
Ito H, Neo M, Yoshida M, Fujibayashi S, Yoshitomi H, Nakamura T (2006) Efficacy of computer-assisted pedicle screw insertion for cervical instability in RA patients. Rheumatol Int 27:567–574
Ito Y, Kai N, Haesgawa Y, Nakago K, Toda K, Yagata Y, Shibara M (2005) Cervical or thoracic instrumentation surgery with registration-free 3D-navigation. Eur Spine J 14 (Suppl 1). Abstract
Jeanneret B, Gebhard JS, Magerl F (1994) Transpedicular screw fixation of articular mass fracture-separation: results of an anatomical study and operative technique. Spine 19:2529–2539
Johnston LT, Karaikovic EE, Lautenschlager EP, Marcu D (2006) Cervical pedicle screws vs. lateral mass screws: uniplanar fatigue analysis and residual pullout strengths. Spine J 6:667–672
Jones EL, Heller JG, Silcox DH, Hutton WC (1997) Cervical pedicle screws versus lateral mass screws: anatomic feasibility and biomechanical comparison. Spine 22:977–982
Kandiziora F, Schulze-Stahl N, Khodadayan-Klostermann C, Schröder R, Mittlmeier T (2001) Screw placement in transoral atlantoaxial plate systems. J Neurosurg 30(Spine 1):80–87
Kantelhardt SR, Oberle J, Derakhsani S, Kast E (2005) The cervical spine and its relation to anterior plate-screw fixation: a quantitative study. Neurosurg Rev 28:308–312
Karaikovic EE, Daubs MD, Madsen RW, Gaines RW Jr (1997) Morphologic characteristics of human cervical pedicles. Spine 22:493–500
Karaikovic EE, Yingsakmongkol W, Gaines RW (2001) Accuracy of cervical pedicle screw placement using the funnel technique. Spine 26:2456–2462
Karaikovic EE, Yingsakmongkol W, Griffiths HJ, Gaines RW (2002) Possible complications of anterior perforation of the vertebral body using cervical pedicle screws. J Spinal Disord Tech 15:75–78
Kirkpatrick JS, Levy JA, Carillo J, Moeini SR (1999) Reconstruction after multilevel corporectomy in the cervical spine. A sagittal plane biomechanical study. Spine 24:1186–1191
Koller H, Daniaux H, Gruber H, Blauth M, Kathrein A (2004) The unstable traumatic spondylolisthesis C2/C3. Akt Traumatol 35:183–202
Koller H, Hempfing A, Ferraris L, Meier O, Metz-Stavenhagen P (2006) 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J, E-Pub 2007
Koller H, Acosta F, Fox M, Tauber M, Hudelmaier M, Forstner R, Augat P, Penzkofer R, Pirich C, Kässmann H, Resch H, Hitzl W (2008) Cervical anterior transpedicular screw fixation (ATPS) - Part II. Accuracy of manual insertion and pull-out strength of ATPS. Eur Spine J. (in press) [E-pub ahead of print]
Koller H Kammermeier V, Ulbricht D, Assuncao A, Karolus S, v-d Berg B, Holz U (2006) Anterior retropharyngeal fixation C1–2 for stabilization of atlantoaxial instabilities. Study of feasibility, technical description and preliminary results. Eur Spine J 15:1326–1338
Kotani Y, Abumi K, Ito M, Minami A (2003) Improved accuracy of computer-assisted cervical pedicle screw insertion. J Neurosurg 99(Spine 3):257–263
Kotani Y, Cunningham BW, Abumi K, McAfee PC (1994) Biomechanical analysis of cervical stabilization systems. An assessment of transpedicular screw fixation in the cervical spine. Spine 19:2529–2539
Kothe R, Rüter W, Schneider E, Linke B (2004) Biomechanical analysis of transpedicular screw fixation in the subaxial cervical spine. Spine 29:1869–1875
Kwon BK, Song F, Morrison WB, Grauer JN, Beiner M, Vaccaro AR, Hilibrand AS, Albert TJ (2004) Morphologic evaluation of cervical spine anatomy with computed tomography. J Spinal Disord Tech 17:102–107
Kwon BK, Vaccaro AR, Grauer JN, Beiner JM (2007) The use of rigid internal fixation in the surgical management of cervical spondylosis. Neurosurgery 60(Suppl 1):S118–S127
Le H, Balabhadra R, Park J, Kim D (2003) Surgical treatment of tumors involving the cervicothoracic junction. Neurosurg Focus 15, Article 3
Lowery GL, McDonough RF (1998) The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine 23:181–186
Ludwig SC, Kramer DL, Balderston RA, Vaccaro AR, Foley KF, Albert TJ (2000) Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine 25:1655–1667
McAfee PC, Bohlmann HH, Ducker TB, Zeidman SM, Goldstein JA (1995) One stage anterior cervical decompression and posterior stabilization. J Bone Joint Surg 77A:1791–1800
Ohnari H, Sasai K, Akagi S, Iida H, Takanori S, Kato I (2006) Investigation of axial symptoms after cervical laminoplasty using questionnaire survay. Spine J 6:221–227
Oh SM, Perin NI, Cooper PRM (1996) Quantitative three-dimensional anatomy of the subaxial cervical spine: implication for anterior spinal surgery. Neurosurgery 38:1139–1144
Panjabi MM, Duranceau J, Goel V, Takata K (1991) Cervical human vertebrae. Quantitative three-dimensional anatomy of the middle and lower regions. Spine 16:861–869
Panjabi MM, Isomi T, Wang JL (1999) Loosening at the screw–vertebra junction in multilevel anterior cervical plate constructs. Spine 24:2383–2388
Panjabi MM Shin EK, Chen NC, Wang JL (2000) Internal morphology of human cervical pedicles. Spine 25:1197–1205
Paramore CG, Dickman CA, Sonntag VKH (1996) Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg 84:957–961
Rao RD, Gourab K, David KS (2006) Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg 88A:1619–1640
Reinhold M, Magerl F, Rieger M, Blauth M (2006) Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J 16:47–56
Resnick DK, Trost GR (2007) Use of ventral plates for cervical arthrodesis. Neurosurg 60(Suppl 1):112–117
Richter M (2005) Posterior instrumentation of the cervical spine using the Neon Occipito-Cervical System. Part 2: Cervical and cervicothoracic instrumentation. Oper Orthop Traumatol 6:579–600
Richter M, Amiot LP, Neller S, Kluger P, Puhl W (2000) Computer-assisted surgery in posterior instrumentation of the cervical spine: an in-vitro feasibility study. Eur Spine J 9:S65–S70
Richter M, Cakir B, Schmidt R (2005) Cervicle pedicle screws: conventioneal versus computer-assisted placement of cannulated screws. Spine 30:2280–2287
Riew KD, Hilibrand AS, Palumbo MA, Bohlmann HH (1999) Anterior cervical corpectomy in patients previously managed with a laminectomy: short-term complications. J Bone Joint Surg Am 81A:950–957
Rogers DE, McDonough P, Cortes Z, Delamarter R (2001) Combined anterior and posterior fusions in patients requiring 3 or more cervical vertebrectomies. Poster presentation, Annual Meeting CSRS-A
Sakamoto T, Neo M, Nakamura T (2004) Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine 22:2510–2514
Sasso RC (2006) Salvage of long strut graft failure following multilevel cervical corpectomy and arthrodesis. In: Clark CR (ed) The cervical spine, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 1212–1217
Sasso RC, Ruggiero RA Jr, Reilly TM, Hall PV (2003) Early reconstruction failures after multilevel cervical corpectomy. Spine 28:140–142
Schlenk RP, Stewart T, Benzel EC (2003) The biomechanics of iatrogenic spinal destabilization and implant failure. Neurosurg Focus 15(3), Article 2
Schmidt R, Wilke HJ, Claes L, Puhl W, Richter M (2003) Pedicle screws enhance primary stability in multilevel cervical corporectomies: biomechanical in vitro comparison of different implants including constrained and nonconstrained posterior instruments. Spine 16:1821–1828
Schultz KD Jr, McLaughlin MR, Haid RW Jr, Comey CH, Rodts GE Jr, Alexander J (2000) Single-stage anterior–posterior decompression and stabilization for complex cervical spine disorders. J Neurosurg 93(Spine 2):214–221
Senol U, Cubuk M,Sindel M,Yildirim F,Yilmaz S, Ozkaynak C, Luleci E (2001) Anteroposterior diameter of the vertebral canal in cervical region: comparison of anatomical, computed tomographic, and plain film measurements. Clin Anat 14:15–18
Sevki K, Mehmet T, Azmi H, Mercan S, Erkal B (2004) Results of surgical treatment for degenerative cervical myelopathy. Spine 29:2493–2500
Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS (2003) Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corporectomy of the cervical spine. Spine 28:2352–2357, 2358
Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS (2004) Enhancement of stability following anterior cervical corpectomy: a biomechanical study. Spine 29:845–849
Steinmetz MP, Kager C, Vaccaro AR, Benzel EC (2005) Kyphotic cervical deformity correction. In: Benzel EC (ed) Spine surgery, 2nd edn. Elsevier, Philadelphia, pp 788–795
Steinmetz MP, Kager CD, Benzel EC (2002) Ventral correction of postsurgical cervical kyphosis. J Neurosurg 97(Spine 2):1–7
Steinmetz MP, Warbel A, Whitfield M, Bingaman W (2002) Preliminary experience with the DOC dynamic cervical implant for the treatment of multilevel cervical spondylosis. J Neurosurg 97(Spine 3):330–336
Swank ML, Lowery GL, Bhat AL, McDonough RF (1997) Anterior cervical allograft arthrodesis and instrumentation: multiple interbody grafting or strut graft reconstruction. Eur Spine J 6:138–143
Takahashi J, Shono Z, Nakamura I, Hirabayashi H, Kamimura M, Ebara S, Kato H (2006) Computer-assisted screw insertion of cervical disorders in rheumatoid arthritis. Eur Spine J 16:485–494
Tan SH, Teo EC, Chua HC (2004) Quantitative three dimensional anatomy of cervical, thoracic and lumbar vertebrae of chinese Singaporeans. Eur Spine J 13:137–146
Taneichi H, Suda K, Kajino T, Kaneda K (2005) Traumatically induced vertebral artery occlusion associated with cervical spine injuries: prospective study using magnetic resonance angiography. Spine 30:1955–1962
Thongtrangan I, Balabhadra RSV, Kim DH (2003) Management of strut graft failure in anterior cervical spine surgery. Neurosurg Focus 15(3), Article 4
Ugur HC, Attar A, Uz A, Tekdemir I, Egemen N, Caglar S, Genc Y (2000) Surgical anatomic evaluation of the cervical pedicle and adjacent neural structures. Neurosurg 47:1162–1168. Comments 1168–1169
Ugur HC, Attar A, Uz A, Tekdemir I, Egemen N, Genc Y (2001) Thoracic pedicle: surgical anatomic evaluation and relations. J Spinal Disord 14:39–45
Ulrich C, Arand M, Nothwang J (2001) Internal fixation on the lower cervical spine—biomechanics and clinical practice of procedures and implants. Eur Spine J 10:88–100
Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, Garfin SR (1998) Early failure of a long segment anterior plate fixation. J Spinal Disord 11
Vanichkachorn JS, Vaccaro AR, Silveri CP, Albert TJ (1998) Anterior junctional plate in the cervical spine. Spine 23:2462–2467
Vecsei V, Fuchs M, Gäbler CH (1998) Indications for treatment of severe unstable injuries of the cervical spine by combined anterior and posterior internal fixation. Osteos Intern 6:121–128
Wang JC, Hart RA, Emery SE, Bohlmann (2003) Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine 28:1016–1021
Yoshida M, Neo M, Fujibayashi S, Nakamura T (2006) Comparison of the anatomical risk for vertebral artery injury associated with the C2-pedicle screw and atlantoaxial transarticular screw. Spine 31:E513–E517
Yoshimoto H, Sato S, Hyakumachi T, Yanagibashi Y, Masuda T (2005) Spinal reconstruction using a cervical pedicle screw system. Clin Orthop Relat Res 431:111–119
Yukawa Y, Kato F, Yoshirara H, Yanase M, Ito K (2006) Cervical pedicle screw fixation in 100 cases of unstable cervical injuries: pedicle axis views obtained using fluoroscopy. J Neurosurg 5:488–493
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koller, H., Hempfing, A., Acosta, F. et al. Cervical anterior transpedicular screw fixation. Part I: Study on morphological feasibility, indications, and technical prerequisites. Eur Spine J 17, 523–538 (2008). https://doi.org/10.1007/s00586-007-0572-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0572-y