Abstract
There is no optimal treatment for symptomatic degenerative disc disease which affects millions of people worldwide. One novel approach would be to form a patch or tissue replacement to repair the annulus fibrosus (AF) through which the NP herniates. As the optimal scaffold for this has not been defined the purpose of this study was to determine if porous silk scaffolds would support AF cell attachment and extracellular matrix accumulation and whether chemically decorating the scaffold with RGD peptide, which has been shown to enhance attachment for other cell types, would further improve AF cell attachment and tissue formation. Annulus fibrosus cells were isolated from bovine caudal discs and seeded into porous silk scaffolds. The percent cell attachment was quantified and the cell morphology and distribution within the scaffold was evaluated using scanning electron microscopy. The cell-seeded scaffolds were grown for up to 8 weeks and evaluated for gene expression, histological appearance and matrix accumulation. AF cells attach to porous silk scaffolds, proliferate and synthesize and accumulate extracellular matrix as demonstrated biochemically and histologically. Coupling the silk scaffold with RGD-peptides did not enhance cell attachment nor tissue formation but did affect cell morphology. As well, the cells had higher levels of type II collagen and aggrecan gene expression when compared to cells grown on the non-modified scaffold, a feature more in keeping with cells of the inner annulus. Porous silk is an appropriate scaffold on which to grow AF cells. Coupling RGD peptide to the scaffold appears to influence AF cell phenotype suggesting that it may be possible to select an appropriate scaffold that favours inner annulus versus outer annulus differentiation which will be important for tissue engineering an intervertebral disc.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The intervertebral disc (IVD) is composed of three interrelated tissues which include the nucleus pulposus (NP), annulus fibrosus (AF) and the cartilage endplate (CEP) [7]. Together, the components of the IVD anchor adjacent vertebral bodies and by doing so allow for spinal stabilization, load bearing, and movement. The AF surrounds the NP and is composed mainly of collagen fibers which form layers called lamellae. The lamellae are oriented at approximately 60° to each other [8]. This organization is critical to the proper biomechanical functioning of the AF. The AF in conjunction with the NP can sustain loads that the AF could not withstand on its own [7].
Degenerative disc disease (DDD) affects millions of people worldwide and can be associated with low back pain. The pathogenesis of DDD has yet to be fully delineated, however, it is thought that trauma, mechanical forces, aging, impaired nutrition, and genetic predisposition contribute to the initiation and progression of the disease process [4, 6, 37]. The NP undergoes changes which include a loss of proteoglycan content, a decrease in cellularity and an increase in the amount of collagen. These changes reduce the ability of the NP to retain water making it less resilient to compression [1, 16]. The AF is forced to support more of the compressive forces than under normal conditions and this increase in loading of the AF causes biochemical and structural changes [19]. The lamellae become disorganized and as such reduces the ability of the AF to resist tensile and torsional forces [17]. The loss of structural integrity over time can lead to tears in the AF and protrusion and/or herniation of the NP contributing to the development of low back pain [32]. Herniated disc tissue can be surgically removed when it impinges on adjacent nerves causing disability and pain. There is usually no disc reconstruction performed during these surgical procedures and recurrent disc prolapse is seen in 10–20% of all patients treated, most commonly at the original site of injury, i.e. where the annular structure has been disrupted [21]. One novel approach to treating these AF defects would be to create a tissue replacement patch consisting of an AF cell seeded-scaffold to fill in and integrate with the tissue adjacent to the defect, or perhaps to replace the entire disc with a biological tissue engineered IVD.
One biomaterial that may be appropriate to use in this setting would be silk fibroin, a protein polymer made by silkworms, which is the strongest known natural fiber and displays resistance to failure in compression. The stability of the silk fibers is a result of the extensive hydrogen bonding, the hydrophobic nature of the protein and the high degree of crystallinity resulting from the β-sheet organization [3]. Bombyx mori (silkworm) silk fibers have been used for many years as suture material. After removal of sericin, the major immunogenic component, the silk fibers elicit little immune response post implantation [22]. Silk has been used for tissue engineering scaffolds as it can be processed into many different formats including porous scaffolds, the rate of degradation can be controlled, and it has both mechanical strength and toughness. For example the ultimate tensile strength of silk fibers are an order of magnitude greater than cross-linked collagen [3, 18, 27]. Degradation rates of silk in vivo will vary depending on the processing method, the animal model used, and the site of implantation [3]. In general, silk fibers lose the majority of their tensile strength within 1 year in vivo, and can be completely degraded within 2 years [3]. These scaffolds have been used successfully to generate a variety of tissues such as cartilage or bone by human mesenchymal stem cells [23, 24].
There are several benefits to using silk as a scaffold to support AF bioengineering. As a result of its compressive and tensile properties silk scaffolds will exhibit mechanical properties during tissue formation which is important for the disc which is always loaded to some degree in vivo. In addition, the silk scaffold would degrade at a sufficiently slow rate to allow for proper tissue development [14]. Another benefit of silk is that peptides can be covalently coupled to it thereby allowing for modification of the scaffolds to potentially enhance cell attachment [10]. A particular peptide of interest is RGD (arginine–glycine–aspartic acid) which is a cell attachment domain found in extracellular matrix proteins, such as fibronectin and collagen, present in the AF [32]. This sequence is recognized by integrins and is known to promote cell attachment for different cell types [10, 15, 31, 34]. Integrins are cell surface receptors that facilitate extracellular matrix-induced cell signaling and when activated have been shown to be important for cell survival for cells such as chondrocytes [15, 31]. AF cells express integrins, including α1, α5, and β1, β3, and β5 [28]. The role of integrins in AF tissue is not known. Hayes et al. [13] showed that in early development, α5β1 integrins are expressed throughout the AF tissue in a lattice-like pattern similar to the distribution of fibronectin. This suggests that matrix-integrin interactions may play a role in AF tissue development and perhaps cell phenotype.
The aims of this study were to determine if porous silk fibroin scaffolds would support AF cell attachment and extracellular matrix accumulation and whether chemically decorating the silk scaffolds with RGD peptide would enhance AF cell attachment and tissue formation.
Materials and methods
Preparation of silk scaffold
The porous silk fibroin scaffolds were produced as described previously [3, 27]. Briefly cocoons were boiled for 30 min in 0.02 M Na2CO3 and then rinsed with water to extract sericin. The silk was dissolved in 9.3 M LiBr solution at room-temperature yielding a 7–8% (w/v) solution, which was dialyzed in water using Slide-a-Lyzer dialysis cassettes (Pierce, MWCO 3500) and then lyophilized. The silk fibroin was dissolved in hexafluoroiso-propanol (HFIP, 17% w/v), granular sodium chloride (particle size 150–250 μm) was added and the solvent was allowed to evaporate at room temperature. The composite of silk/porogen was immersed in alcohol (1-butanol) for 30 min to induce a β-sheet structure and then placed into cold water for 24 h to extract the salt. The porous silk scaffolds were dried. Biopsy punches were used to create scaffolds measuring 4 mm in diameter and 2 mm in height which were subsequently sterilized by autoclaving. The scaffolds were placed in tygon tubing to aid in cell retention during seeding.
For some experiments, silk scaffolds were modified by covalent coupling of RGD peptides using methods previously described [10]. Briefly, after hydration of silk matrices in PBS (pH 6.5) for 1 h, the carboxyl groups of aspartatic acid and glutamic acid amino acids were activated by reaction with 0.5 mg/ml 1-ethyl-3-dimethylaminopropyl carbodiimide hydrochloride (EDC) and 0.7 mg/ml N-hydroxysuccinimide (NHS) solution (Pierce) in PBS for 15 min at room temperature. The silk scaffolds were rinsed to remove excess EDC/NHS and then reacted with the glycine–arginine–glycine–aspartate–serine (GRGDS) peptide (Sigma, St Louis, MO, 0.1 mg/ml) in PBS for 2 h at room temperature, then rinsed in distilled water and air dried.
Cell culture
Bovine caudal spines (6–9 months of age) were harvested aseptically; the AF dissected out and placed in Ham’s F12 and care was taken to avoid inclusion of NP and cartilage tissue. Tissues from five discs obtained from one caudal spine were combined to obtain sufficient cells for each experiment. Separate caudal spines were used for each set of experiments. The AF tissue was minced and underwent sequential enzymatic digestion with 0.5% protease (Sigma, St Louis, MO) for 1 h at 37°C, followed by 0.2% collagenase A (Roche, Laval, QC, Canada) overnight at 37°C. The cell suspension was washed, filtered through a sterile mesh, and resuspended in Ham’s F12 supplemented with 10% fetal bovine serum (FBS). An aliquot of cells (5 × 105 cells/20 μl) was applied to the top surface of the silk scaffold every 30 min for a total of four seedings. The cell-seeded scaffolds were maintained in Ham’s F12 supplemented with 10% FBS and the tubing was removed after 48 h. After 5 days, the FBS concentration was increased to 20% and ascorbic acid (100 μg/ml final concentration) was added to the medium starting at day 7. The medium was changed every 2–3 days and fresh ascorbic acid was added with each change. Cultures were harvested at various times up to 8 weeks. Each experiment was repeated at least 3 times.
Scanning electron microscopy (SEM)
Twenty-four hours or 14 days after seeding, cell-seeded scaffolds were harvested and fixed in 2% glutaraldehyde. The samples underwent sequential ethanol dehydration, critical point drying and sputter coating with gold. After critical point drying, representative constructs were fractured in half along the long axis to assess the extent of cell infiltration in the scaffold. All samples were evaluated using SEM (XL30 ESEM, FEI, Toronto, ON).
Cellularity
At various times, the entire cell-seeded scaffolds were harvested and papain digested (Sigma; 40 μg/ml, 20 mmol/l ammonium acetate, 1 mmol/l EDTA, and 2 mmol/l dithiothreitol) for 48 h at 65°C. The DNA content of the tissues was determined from aliquots of the papain digest using the Hoechst 33258 dye binding assay (Polysciences, Warrington, PA) and fluorometry (emission wavelength 365 nm, excitation wavelength 458 nm) as previously described [39]. A standard curve was generated using calf thymus DNA (Sigma). To determine the percent cell attachment to the scaffold the DNA content of the cell-seeded scaffolds at 24 h was divided by the DNA content of the cell aliquot used to seed the scaffold.
Quantification of proteoglycan and collagen synthesis
To quantify matrix synthesis, tissues at 3 or 14 days of culture were incubated in the presence of both [35S]-SO4 (4 uCi/construct) and [3H]-proline (4 uCi/construct) for an additional 24 h to label proteoglycans and collagen, respectively [36]. The radiolabeled tissues were harvested and washed 3 times in PBS to remove unincorporated isotope. The tissues were papain digested as described above. The proteoglycans in the media were precipitated with 100% ethanol, resuspended in 4 M guanidinium hydrochloride (in 50 mmol/l sodium acetate pH 5.8 containing 0.1 M 6-amino-hexanoic-acid, 50 mmol/l benzamidine HCl, 10 mmol/l EDTA, and 5 mmol/l N-ethylmaleimide). Collagen was precipitated from the culture media with 70% ammonium sulfate, washed and resuspended in 10% sodium dodecyl sulfate. The amounts of newly synthesized proteoglycan and collagen were determined by quantifying radioisotope incorporation using a β-liquid scintillation counter and total synthesis determined by combining the counts in the tissue and the culture medium.
RT-PCR
Seventy-two hours after seeding, total RNA was isolated from the cells using Trizol® (Gibco BRL, Rockville, MD) extraction following disruption of the tissue by mortar and pestle in liquid nitrogen. Total RNA (0.5 μg) was reverse transcribed (Superscript First Strand Synthesis System, Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions. Relative gene expression was examined by semi-quantitative PCR using Taq Polymerase (Quiagen, Mississauga, ON) and sequence-specific primers in reactions designed to amplify the template sequence of interest within the linear range as described previously (Eppendorf Mastercycler PCR machine) (Table 1) [36]. The PCR products were run on a 1.5%-agarose gel and stained with ethidium bromide. Band intensity was quantified by densitometry using LabWorks software (V4.0, Media Cybernectics). Gene expression was normalized by the housekeeping gene 18S rRNA. Each time point was done in triplicate and each experiment was repeated 3 times.
Histological evaluation
The cell-seeded silk scaffolds were harvested at various times, fixed in 10% formalin and paraffin-embedded. Five μm sections were cut and stained with either hematoxylin and eosin or trichrome.
Determination of proteoglycan and collagen contents
The proteoglycan content of the tissue was determined by measuring the amount of sulfated glycosaminoglycans in the papain-digested tissue using the dimethylmethylene blue dye binding assay and spectrophotometry at 525 nm as previously described [39]. The standard curve was generated using bovine chondroitin sulfate (Sigma).
Collagen content was determined by measuring the hydroxyproline content in aliquots of the papain digest following hydrolysis in 6 N HCl for 18 h at 110°C. The hydroxyproline content was determined using the chloramine-T/Ehrlich’s reagent assay and spectrophotometry at 560 nm [39, 40]. The standard curve was generated using l-hydroxyproline (Sigma). The collagen content was determined by assuming that hydroxyproline constitutes approximately 10% of the weight of collagen [40].
Statistical analysis
Results were pooled and expressed as the mean ± standard error of the mean (SEM) of three separate experiments. One-way analysis of variance with Tukey’s multiple comparison test was used to compare the in vitro-formed AF tissue over different time points. Comparison of two different conditions at the same time point was analyzed by a t-test. Significance was assigned at P < 0.05.
Results
Tissue cellularity over time
At 24 h, 35 ± 4.1% (mean ± SEM) of the cells seeded into the non-modified silk scaffold had attached as determined by quantifying DNA content. Figure 1 shows that although there was a trend toward increasing DNA content over time, a significant increase in cellularity was only detected by day 56, at which time there was approximately a twofold increase in DNA content compared to day 1 of culture (P < 0.05).
Effect of RGD-modified silk scaffold on cell attachment and cellularity over time
To determine if cell attachment could be enhanced, RGD peptide was chemically coupled to the silk scaffolds. The presence of RGD peptides did not enhance seeding efficiency as only 28.9 ± 2.5% cells attached to scaffold. Cell attachment was significantly decreased as this represented 72 ± 21.7% (mean ± SEM) of the number of cells that had attached to the non-modified scaffold (P < 0.05) (Fig. 2). Although the cellularity of the scaffolds appeared to be increasing on the RGD-coupled scaffolds similarly to that of the non-modified scaffolds, they did not attain the number of cells detected on the non-modified scaffolds. Cell-seeded RGD-coupled scaffolds achieved only 87.2 ± 10.71% (mean ± SEM) of the cellularity of cell-seeded non-modified scaffolds at the end of the 8 weeks of culture (Fig. 2).
DNA content of cell-seeded RGD-modified silk scaffolds relative to non-modified scaffolds at various times in culture up to 56 days. Each time point was done in triplicate and three separate experiments were performed (n = 9) and the results pooled and expressed as mean ± SEM. *P < 0.05 relative to cellularity on non-modified scaffold at that timepoint
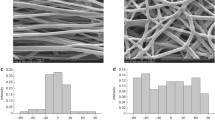
Appearance of cell-seeded silk scaffolds by scanning electron microscopy
The scaffolds, both non-modified and modified by coupling with RGD-peptide, were examined 1 and 14 days after seeding (Fig. 3). AF cells had attached predominately to the outer surface of the silk scaffolds and there appeared to be more cells on the non-modified scaffolds. At 24 h, there was a mixture of both round and flattened cells on both scaffolds (Fig. 3a–d). However, there appeared to be greater prevalence of rounded cells on the surface of the non-modified scaffold compared to the RGD-modified scaffolds. The cells on the non-modified scaffolds appeared spiky and were more polygonal than the cells on the RGD-modified scaffolds which were flat and smooth. There was very little extracellular matrix observed at this time on either type of scaffolds.
By 14 days, tissue was seen covering the scaffolds (Fig. 3e–h). Where cells could be delineated at the surface they appeared flattened although occasional round cells were still present. However there was still an observable difference in the surface roughness as cells on the non-modified scaffolds had spiky surfaces while cells on the RGD-modified scaffolds were smooth.
Extracellular matrix synthesis by AF cells
To evaluate matrix synthesis and accumulation over time AF cells were incubated with 3H-proline and 35SO4. By day 4 the cells were accumulating approximately one third of the newly synthesized collagen (Fig. 4a) and this increased significantly as by day 15 approximately three-quarters of the collagen was being retained. There was no significant difference in the amount of collagen synthesized between the cells on the two different scaffolds at either time point (data not shown).
a Percent retention of newly synthesized collagens at 4 or 15 days after seeding on either non-modified (non-mod) or RGD-modified scaffolds (RGD-mod). b Percent retention of newly synthesized proteoglycans at 4 and 15 days after seeding on either non-modified (non-mod) or RGD-modified scaffolds (RGD-mod). Each time point was done in triplicate and three separate experiments were performed (n = 9) and the results pooled and expressed as mean ± SEM. *P < 0.05 indicating a significant difference compared to day 4
Similarly there were no differences in the amount of proteoglycans synthesized by the cells at each time point on the two different scaffolds (data not shown). However the amount of proteoglycans that accumulated decreased about eightfold between 4 and 15 days for both the non-modified and RGD-modified scaffolds (Fig. 4b). (Retention of newly synthesized proteoglycans (mean ± SEM): non-modified scaffolds = 77 ± 4% at day 4 and 13 ± 3% at day 15; RGD-coupled scaffolds = 80 ± 1% at day 4 and 9 ± 1% at day 15, P < 0.05).
Gene expression of the AF cells grown on the silk scaffold
The gene expression of the major matrix molecules, known to be synthesized by AF cells, was examined after 72 h of culture. The cells grown on the silk scaffolds expressed both type I and type II collagens and aggrecan. The expression of collagen type I was similar in cells grown on the non-modified and RGD-modified scaffolds. However there was a significant increase in collagen type II and aggrecan gene expression levels (1.6-fold and a 1.9-fold, respectively), in cells grown on the RGD-modified scaffolds when compared to cells grown on the non-modified scaffolds (P < 0.05), (Fig. 5).
a Representative agarose gel showing gene expression of 2 representative cell cultures grown on either non-modified (non-mod) or RGD-modified silk scaffolds (RGD-mod). 18S rRNA represents the housekeeping gene. b Densitometry of collagen type I (Col I) or II (Col II) or aggrecan gene expression normalized to 18S rRNA. The data represents the mean ± SEM of 3 separate experiments. (*P < 0.05 relative to gene expression in cells grown on non-modified scaffold)
Extracellular matrix accumulation over time
To determine if cells grown on silk scaffolds can form tissue the amount of extracellular matrix that accumulated was quantified. Figure 6 shows that the cells grown on the silk scaffold accumulated collagen and proteoglycans over time. A significant increase in collagen content was detected within 14 days when compared to day 1 cultures and by 56 days there was over a tenfold increase in collagen. There were no significant differences in the amount of collagen at any time point between cells grown on the RGD-modified scaffolds and the non-modified scaffolds. As would be expected for AF tissue only small amounts of proteoglycan were accumulated and a significant increase in proteoglycan content relative to day 1 was only observed by 28 days. The amount of proteoglycans for the RGD-modified and non-modified scaffolds, on the first day of culture, were comparable but by day 14 significantly more proteoglycans had accumulated on the RGD-modified scaffolds. However, by 8 weeks, although there were slightly more proteoglycans in the tissue formed on the RGD-modified scaffolds, it was not significantly different from tissues formed on the non-modified scaffolds.
a AF cells were seeded on either non-modified or RGD-modified silk scaffolds and the collagen content determined and normalized for cellularity as described under the Materials and methods for various times up to 56 days. (*P < 0.05 relative to day 1 on relevant scaffold). b AF cells were seeded on either non-modified or RGD-modified silk scaffolds and the glycosaminoglycan content determined and normalized for cellularity as described under the Materials and methods for various times up to 56 days. (*P < 0.05 relative to day 1 on respective scaffold; a P < 0.05 between non-modified and RGD-modified scaffolds)
Histological evaluation of the cell-seeded silk scaffolds
To assess tissue morphology over time the scaffolds were harvested at various times up to 8 weeks and processed for histological evaluation. At 2 weeks cells were seen predominately on the surface of the scaffold and only a few scattered cells were seen within the scaffold. There were areas of the scaffolds that were devoid of any cells. There was no obvious difference observed between the two types of scaffolds. There appeared to be an increase in tissue over time. By 8 weeks a layer of tissue could be seen surrounding the entire outer surface of either scaffold and more cells were seen within the scaffold. The cellular morphology and tissue formation by cells grown on RGD-modified scaffolds were similar to that seen in the unmodified scaffolds (Fig. 7).
Discussion
The results of this study demonstrated that AF cells adhere to porous silk scaffolds and synthesize collagen and proteoglycans after attachment. The cells proliferate and accumulate extracellular matrix as demonstrated biochemically and histologically. Coupling the silk scaffold with RGD-peptides did not further enhance cell attachment, collagen accumulation, or tissue formation as determined histologically. AF cells have been grown in vitro on a variety of materials including agarose, alginate, atelocollagen, and collagen/glycosaminoglycan scaffolds and similar to our findings these cells did not form properly organized AF tissue [2, 5, 11, 20, 33, 35, 38]. Cells grown in or on these biomaterials for example, showed limited retention of matrix molecules [2] and/or patchy distribution of cells [11]. The one method that resulted in tissue formation consisted of seeding AF cells into a polyglycolic acid scaffold and implanting the cell-seeded construct into nude mice [25]. However, even under these conditions, the AF tissue only attained approximately 50% of the collagen content of native AF [26]. It is not clear why it is difficult to bioengineer AF tissue with a collagen content that mimics the in vivo tissue, however, other weight bearing tissues such as cartilage [39] experience similar limitations suggesting that tissue formation under static conditions may be a contributing factor. Clearly there is a need to identify a more appropriate method to form AF tissue in vitro if the goal is to form an organized and mechanically functional tissue.
It is not clear why decorating the silk scaffold with RGD peptides did not appear to improve cell attachment or distribution of cells throughout the scaffold. The formulation utilized in this study has been shown to improve cell attachment, spreading, proliferation and ECM production by stem cells and ligament fibroblasts seeded onto silk scaffolds in previous studies so it may be a cell-specific response [10, 23, 24]. Alternatively, it is possible that the AF cells did not express the appropriate integrins as it has been shown that integrins can be differentially expressed between species [28]. To ensure that this was not the cause of the negative results in this study, we determined that the cells expressed both α5β1 and αvβ3 integrins by immunostaining and confocal microscopy (data not shown). However as it has been shown that the amount, type (ring vs. linear peptide) and distribution of the RGD peptide on the scaffold may influence cell response it is possible that the optimal concentration or formulation of the peptide for AF cells was not selected [9, 29]. However, this is considered less likely for three reasons. Firstly, the presence of the RGD peptide appeared to inhibit cell attachment as significantly less cells attached to this scaffold. Interaction with RGD has been shown to inhibit epithelial cell attachment and cell proliferation, so this effect has been observed by others [30]. Secondly, the AF cells attached to the non-modified scaffold had a different appearance when compared to cells adherent to the RGD-modified scaffold, a feature that appeared to be maintained even at 14 days of culture. Thirdly, the cells grown on the RGD-modified scaffolds showed differential gene expression as there was significantly greater collagen type II and aggrecan gene expression at 72 h when compared to cells growing in the non-modified scaffold. Interestingly the genotypic differences observed when cells were grown on the RGD-modified scaffold are more in keeping with cells of the inner rather than outer AF [32] suggesting that the AF cell interaction with RGD may not enhance cell attachment but may play a role in influencing cell differentiation. This is not entirely unexpected as integrins are likely involved in development in vivo as they have been detected in the embryonic AF [12]. Furthermore, RGD-coupled silk scaffolds have been shown to aid in differentiation of mesenchymal stem cells [23, 24]. However, additional experiments, to evaluate the effect of varying the concentration and localization of RGD peptide on the scaffold, are necessary to confirm that RGD peptides do not influence AF cell attachment. As well, it is possible that a combination of receptors such as annexin V or CD44 in addition to integrins are needed to regulate cell attachment and that is why coupling the scaffold with RGD peptides was insufficient to effect cell attachment.
In keeping with the increased gene expression of aggrecan core protein in cells grown on RGD-modified scaffolds the cells accumulated significantly more proteoglycans than the cells grown on the non-modified silk scaffold. This occurred despite the observation that the cells on both scaffolds did not differ in the total amount of proteoglycans synthesized and/or retained on the two different scaffolds at the two time points examined (days 4 and 15). This raises the possibility that other factors such as changes in the levels of degradative enzymes may be contributing to the overall proteoglycan content and may explain why proteoglycan retention was lower at 15 days compared to 4 days. This requires further study. There were no significant differences in the amount of collagens synthesized and retained within the two different scaffolds. The cells on both types of scaffolds showed similar increase in retention of newly synthesized collagen with time. It is likely that the increased type II collagen gene expression in cells grown on the RGD-modified scaffold compared to the non-modified scaffold was insufficient to result in a change in collagen protein content that could be detected biochemically. A spectrophotometric method was used to quantify the amount of collagen, so it is possible that the assay was not sufficiently sensitive to detect small differences in the amounts of collagen. The assay also cannot differentiate between the different types of collagen produced [40].
In summary, porous silk scaffolds support AF cell attachment and tissue formation. It may be possible to use these scaffolds to also modulate the phenotype of the AF cells. This will be important for tissue engineering an AF that mimics the native tissue with inner transition and outer zones. Although tissue engineering AF tissue remains a challenge, our data suggests that silk scaffolds are appropriate to use based on these studies and the known biocompatibility and mechanical properties of this biomaterial. Further studies to optimize cell seeding and tissue formation are ongoing.
References
Adams MA, Roughley PJ (2006) What is intervertebral disc degeneration, and what causes it? Spine 31(18):2151–2161
Alini M, Li W, Markovic P, Aebi M, Spiro RC, Roughley PJ (2003) The potential and limitations of a cell-seeded collagen/hyaluronan scaffold to engineer an intervertebral disc-like matrix. Spine 28(5):446–454
Altman GH, Diaz F, Jakuba C, Calabro T, Horan RL, Chen J et al (2003) Silk-based biomaterials. Biomaterials 24(3):401–416
Anderson DG, Tannoury C (2005) Molecular pathogenic factors in symptomatic disc degeneration. Spine J 5(6 Suppl):S260–S266
Baer AE, Wang JY, Kraus VB, Setton LA (2001) Collagen gene expression and mechanical properties of intervertebral disc cell-alginate cultures. J Orthop Res 19(1):2–10
Battie MC, Videman T (2006) Lumbar disc degeneration: epidemiology and genetics. J Bone Joint Surg Am 88(Suppl 2):3–9
Bogduk N (1997) The inter-body joints and the intervertebral discs. In: Bogduk N (ed) Clinical anatomy of the lumbar spine and sacrum. Churchill Livingstone, New York, pp 13–31
Broberg KB (1983) On the mechanical behaviour of intervertebral discs. Spine 8(2):151–165
Carman CV, Springer TA (2003) Integrin avidity regulation: are changes in affinity and conformation underemphasized? Curr Opin Cell Biol 15(5):547–556
Chen J, Altman GH, Karageorgiou V, Horan R, Collette A, Volloch V et al (2003) Human bone marrow stromal cell and ligament fibroblast responses on RGD-modified silk fibers. J Biomed Mater Res A 67(2):559–570
Gruber HE, Leslie K, Ingram J, Norton HJ, Hanley EN (2004) Cell-based tissue engineering for the intervertebral disc: in vitro studies of human disc cell gene expression and matrix production within selected cell carriers. Spine J 4(1):44–55
Hayes AJ, Benjamin M, Ralphs JR (1999) Role of actin stress fibres in the development of the intervertebral disc: cytoskeletal control of extracellular matrix assembly. Dev Dyn 215(3):179–189
Hayes AJ, Benjamin M, Ralphs JR (2001) Extracellular matrix in development of the intervertebral disc. Matrix Biol 20(2):107–121
Horan RL, Antle K, Collette AL, Wang Y, Huang J, Moreau JE et al (2005) In vitro degradation of silk fibroin. Biomaterials 26(17):3385–3393
Hynes RO (2002) Integrins: bidirectional, allosteric signaling machines. Cell 110(6):673–687
Iatridis JC, Maclean JJ, Roughley PJ, Alini M (2006) Effects of mechanical loading on intervertebral disc metabolism in vivo. J Bone Joint Surg Am 88(Suppl 2):41–46
Iatridis JC, MaClean JJ, Ryan DA (2005) Mechanical damage to the intervertebral disc annulus fibrosus subjected to tensile loading. J Biomech 38(3):557–565
Kim UJ, Park J, Li C, Jin HJ, Valluzzi R, Kaplan DL (2004) Structure and properties of silk hydrogels. Biomacromolecules 5(3):786–792
Klein JA, Hickey DS, Hukins DW (1983) Radial bulging of the annulus fibrosus during compression of the intervertebral disc. J Biomech 16(3):211–217
Kluba T, Niemeyer T, Gaissmaier C, Grunder T (2005) Human anulus fibrosis and nucleus pulposus cells of the intervertebral disc: effect of degeneration and culture system on cell phenotype. Spine 30(24):2743–2748
Martin G (1980) Recurrent disc prolapse as a cause of recurrent pain after laminectomy for lumbar disc lesions. NZ Med J 91(656):206–208
Meinel L, Hofmann S, Karageorgiou V, Kirker-Head C, McCool J, Gronowicz G et al (2005) The inflammatory responses to silk films in vitro and in vivo. Biomaterials 26(2):147–155
Meinel L, Hofmann S, Karageorgiou V, Zichner L, Langer R, Kaplan D et al (2004) Engineering cartilage-like tissue using human mesenchymal stem cells and silk protein scaffolds. Biotechnol Bioeng 88(3):379–391
Meinel L, Karageorgiou V, Hofmann S, Fajardo R, Snyder B, Li C et al (2004) Engineering bone-like tissue in vitro using human bone marrow stem cells and silk scaffolds. J Biomed Mater Res A 71(1):25–34
Mizuno H, Roy AK, Vacanti CA, Kojima K, Ueda M, Bonassar LJ (2004) Tissue-engineered composites of anulus fibrosus and nucleus pulposus for intervertebral disc replacement. Spine 29(12):1290–1297
Mizuno H, Roy AK, Zaporojan V, Vacanti CA, Ueda M, Bonassar LJ (2006) Biomechanical and biochemical characterization of composite tissue-engineered intervertebral discs. Biomaterials 27(3):362–370
Nazarov R, Jin HJ, Kaplan DL (2004) Porous 3-D scaffolds from regenerated silk fibroin. Biomacromolecules 5(3):718–726
Nettles DL, Richardson WJ, Setton LA (2004) Integrin expression in cells of the intervertebral disc. J Anat 204(6):515–520
Ochsenhirt SE, Kokkoli E, McCarthy JB, Tirrell M (2006) Effect of RGD secondary structure and the synergy site PHSRN on cell adhesion, spreading and specific integrin engagement. Biomaterials 27(20):3863–3874
Oharazawa H, Ibaraki N, Ohara K, Reddy VN (2005) Inhibitory effects of Arg–Gly–Asp (RGD) peptide on cell attachment and migration in a human lens epithelial cell line. Ophthalmic Res 37(4):191–196
Pulai JI, Del Carlo M Jr, Loeser RF (2002) The alpha5beta1 integrin provides matrix survival signals for normal and osteoarthritic human articular chondrocytes in vitro. Arthritis Rheum 46(6):1528–1535
Roberts S, Evans H, Trivedi J, Menage J (2006) Histology and pathology of the human intervertebral disc. J Bone Joint Surg Am 88(Suppl 2):10–14
Rong Y, Sugumaran G, Silbert JE, Spector M (2002) Proteoglycans synthesized by canine intervertebral disc cells grown in a type I collagen-glycosaminoglycan matrix. Tissue Eng 8(6):1037–1047
Ruoslahti E (1996) RGD and other recognition sequences for integrins. Annu Rev Cell Dev Biol 12:697–715
Sato M, Kikuchi M, Ishihara M, Ishihara M, Asazuma T, Kikuchi T et al (2003) Tissue engineering of the intervertebral disc with cultured annulus fibrosus cells using atelocollagen honeycomb-shaped scaffold with a membrane seal (ACHMS scaffold). Med Biol Eng Comput 41(3):365–371
Seguin CA, Pilliar RM, Roughley PJ, Kandel RA (2005) Tumor necrosis factor-alpha modulates matrix production and catabolism in nucleus pulposus tissue. Spine 30(17):1940–1948
Setton LA, Chen J (2006) Mechanobiology of the intervertebral disc and relevance to disc degeneration. J Bone Joint Surg Am 88:(Suppl 2):52–57
Thonar EJ, An H, Masuda K (2002) Compartmentalization of the matrix formed by nucleus pulposus and annulus fibrosus cells in alginate gel. Biochem Soc Trans 30:874–878
Waldman SD, Grynpas M, Pilliar RM, Kandel RA (2002) Characterization of cartilagenous tissue formed on calcium polyphosphate substrates in vitro. J Biomed Mater Res 62(3):323–330
Woessner JF Jr (1961) The determination of hydroxyproline in tissue and protein samples containing small proportions of this imino acid. Arch Biochem Biophys 93:440–447
Acknowledgments
We thank Mr. Harry Bojarski and Ryding-Regency Meat Packers, Toronto, Canada for providing the tissues and Marie Maguire for secretarial support. This work was supported by NIH grant R21AR052801-02.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chang, G., Kim, HJ., Kaplan, D. et al. Porous silk scaffolds can be used for tissue engineering annulus fibrosus. Eur Spine J 16, 1848–1857 (2007). https://doi.org/10.1007/s00586-007-0364-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-007-0364-4