Abstract
The outcome assessment in instrumented lumbosacral fusion mostly focuses on clinical criteria, complications and scores, with a high variability of imaging means, methods of fusion grading and parameters describing degenerative changes, making comparisons between studies difficult. The aim of this retrospective evaluation was to evaluate the interest of quantified radiographic analysis of lumbar spine in global outcome assessment and to highlight the key biomechanical factors involved. Clinical data and Beaujon–Lassale scores were collected for 49 patients who underwent lumbosacral arthrodesis after prior lumbar discectomy (mean follow-up: 5 years). Sagittal standing and lumbar flexion-extension X-ray films allowed quantifying vertebral, lumbar, pelvic and kinematic parameters of the lumbar spine, which were compared to reference values. Statistics were performed to assess evolution for all variables. At long-term follow-up, 90% of patients presented satisfactory clinical outcomes, associated to normal sagittal alignment; vertebral parameters objectified adjacent level degeneration in four cases (8%). Clinical outcome was correlated (r = 0.8) with fusion that was confirmed in 80% of cases, doubtful in 16% and pseudarthrosis seemed to occur in 4% (2) of cases. In addition to clinical data (outcomes comparable to the literature), quantitative analysis accurately described lumbar spine geometry and kinematics, highlighting parameters related to adjacent level’s degeneration and a significant correlation between clinical outcome and fusion. Furthermore, criteria proposed to quantitatively evaluate fusion from lumbar dynamic radiographs seem to be appropriate and in agreement with surgeon’s qualitative grading in 87% of cases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The outcome assessment of lumbosacral fusion after prior discectomy mostly focuses on qualitative subjective criteria, such as fusion grading [6, 35]. Complications are also analysed, such as residual low back pain, pseudarthrosis, adjacent levels degeneration [1, 9, 11, 22, 29], hardware failure or recurrent herniation [5, 23, 30]. Difficulties arise from the lack of agreement in qualitative fusion grading [2, 13, 13, 28, 34] and in the choice of parameters describing degenerative changes of levels adjacent to the fused segment [9, 22, 29]. The choice of imaging means in the follow-up exams seems to be controversial as well. Some authors compared radiological data from X-ray films, MRI or CT and surgical findings [2, 13, 15, 32], without reaching an agreement, and accuracy of these measurements was not always documented [13]; computer-assisted tools for spine radiographic analysis were recently proposed [3, 4, 26, 27, 31] with extensive evaluation of measurement accuracy.
The aim of this study was to evaluate the interest of quantitative radiographic analysis of lumbar spine in assessing the global outcome of lumbosacral arthrodesis and to identify the key biomechanical factors involved.
Materials and methods
Clinical study
Clinical records were obtained (retrospectively) for 108 patients reoperated after lumbar discectomy by the senior surgeon (Ch.M.) between 1991 and 2000 at the Institut Mutualiste Montsouris, in Paris, France, and were registered in a specific database (ProFile®, Surgiview, Paris). From the files that contained both clinical and imaging records, a selection was made based on the criteria of instrumented lumbosacral fusion and a minimum radiological follow-up of 2 years.
The selected group was composed of 49 patients: 43% men and 57% women, aged from 29 to 73 years (average 47 years). Main reasons for reoperation were recurrent disc herniation (10 cases), epidural scar formation (4 cases) and incapacitating low back pain or sciatica, unresponsive to conservative care (35 cases).
All patients underwent posterolateral lumbosacral fusion with iliac crest autograft and dynamic instrumentation (Twinflex®, SpineNetwork, France) [12], the surgical technique being already presented elsewhere [21]. The following levels were involved: L3-sacrum in 25% of cases, L4-sacrum in 53% of cases and L5-sacrum for the other 22%, which means a total of 93 treated discs. Clinical data and scoring were collected. The Beaujon Lassale scoring system [17] was used to evaluate general and neurological condition of the patient. The relative gain was also calculated, as defined by Lassale et al.:
The follow-up period ranged from 2 to 10 years (average 5 years) and was divided into three periods, as follows: short term (up to 1 year), mid-term (1–3 years) and long term (3–5 years or more). Eight patients (16%) in this population did not reach the long-term follow-up.
Reoperations: During the follow-up, six patients were reoperated. In four cases, the reason was adjacent level degeneration (6–8 years after fusion), associated with screw breakage and pseudarthrosis in one case. In the two other cases active patients (intensive sports and physical activities) asked for the removal of the instrumentation (3 years after fusion).
Radiological study
For the 49 patients, 118 sagittal standing and 140 pairs of flexion-extension (dynamic) lumbar X-ray films were scanned and analysed by means of Spineview® 2.1 software (Surgiview, Paris, France). This analysis is based on vertebral bodies identification on the scanned image, allowing for automatic calculation of a large panel of parameters, with validity and reproducibility previously assessed and documented [3].
As the available radiological data was quite heterogeneous in this retrospective study, the type and numbers of patients’ X-ray films are presented in Table 1. Radiological follow-up was available at long-term exam for 38 patients, as eight patients did not reach this postoperative period and three other patients feeling well did not do X-ray exams any more.
Main evaluation was performed on dynamic radiographs, as sagittal standing X-ray films were not systematically prescribed at the same moment in time (to avoid patient irradiation). In spite of a heterogeneous distribution of these last exams (short and long term, mid- and long term or short and mid-term for a given patient), at least two postoperative sagittal standing X-ray films were available for each case and all patients had a postoperative sagittal standing radiograph at about 3 years (3 ± 0.5 years) after surgery.
Sagittal X-ray films analysis
-
1.
In order to evaluate lumbar and pelvic balance, the following parameters were calculated from sagittal X-ray films in standing position at different periods until the latest observation: L1S1 lordosis, measured from the upper endplate of L1 to the sacral plate; lumbar lordosis—angle formed by the upper and the lower endplates, respectively, of the most tilted vertebra of the lumbar curve; sacral slope—angle formed by the sacral plane with the horizontal [19]; pelvic version—angle formed by the vertical line and the straight line D meeting at the centre of the bicoxo-femoral axis and the centre of the sacral plate, and finally, the pelvic incidence—angle between the perpendicular to the sacral plane at its centre and the straight line D [19].The three previously described parameters are represented in Fig. 1.
-
2.
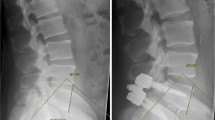
Adjacent levels degeneration was also investigated. Preoperative imaging exams (X-ray films and MRI) were used to evaluate pre-existent signs of degeneration. The presence of osteophytes and vertebral endplate sclerosis (graded from 1 to 4) and/or subjacent level stenosis were considered as qualitative criteria of degeneration [9, 22, 29]. Quantitative analysis focused on parameters calculated from sagittal standing X-ray films, such as upper endplate inclination, vertebral wedging, sagittal listhesis (Fig. 2), disc height [8], disc/vertebra height ratio and lordosis of the fused segment. Correlations were analysed between qualitative and quantitative criteria.
Lumbar kinematics
Lumbar kinematics was investigated on lumbar dynamic (flexion-extension) X-ray films. Ranges of motion (ROM) quantified the residual motion on instrumented levels and allowed to assess non-union, as described in the literature [20]. The following criteria were stated to interpret the results: not significant (0°–3°) intervertebral mobility might be assessed as solid fusion, low mobility (3°–5°) as doubtful fusion and, finally, mobility equal or superior to 5° as pseudarthrosis, in the hypothesis that fusion should be achieved after 1 year.
The Mean Centre of Rotation (MCR)[24, 25, 33] provides the location of the point around which the upper vertebra rotates with regard to the one below when passing from full flexion to full extension in a sagittal plane. As uncertainty of MCR location considerably increases when ROM are lower than 3° [3, 36], this parameter was not calculated in this situation. Therefore, results were classed in: MCR ‘not calculated’, “normal”—for a location within the obtained reference ranges, and ‘abnormal’, when MCR was calculated but location was out of reference ranges.
Analytical analysis and reference values
For all parameters, the measurement errors [3] presented in Table 2 represented the cut-off values used to evaluate significant changes in their evolution. Furthermore, in order to evaluate the influence of instrumentation on the fused segment, parameter values calculated from sagittal radiographs were compared to those corresponding to a group of 63 asymptomatic subjects (42% men, 58% women, mean age 43 ± 12 years) for whom full-spine sagittal X-ray films were available from previous studies [3]. Table 3 presents reference values obtained for vertebral parameters, as lordosis and pelvic parameters were already presented in the literature [3, 19, 38]. For dynamic analysis, reference values were obtained from 18 asymptomatic volunteers (11 men and 7 women, mean age 34 ± 10 years, available from previous studies); ROM are presented in comparison to literature in Fig. 3.
Statistics
Clinical scores were statistically analysed by one-way repeated measures of variance (ANOVA); a P-value inferior to 0.05 was considered to be significant. Furthermore, clinical data and biomechanical parameters were analysed using the following tests: ANOVA, regression and correlation tests by means of Statview 5.0® software (SAS Institute, Cary, NC, USA). Statistics were also used to compare fusion grading assessed by qualitative results, as found in senior surgeon’s notes (Ch.M.), and by quantified analysis, corresponding to the above-described protocol.
All measurements, statistics and data recording were performed in a blinded manner, by an independent observer, not related to the surgical team (SC).
Results
Clinical outcome
The evolution of Beaujon–Lassale scores (ranging from 0 to 20) is represented in Fig. 4. A significant difference (P = 0.03) was found between the score values calculated at different periods of time. Relative gains were: very good (71–100%) for 61%, good (41–70%) for 29% and fair (11–40%) for 10% of patients.
Postoperative complications were represented by residual pain (15%), adjacent level degeneration (8% at 5 years), hardware failure (6%) and pseudarthrosis (4%).
Radiological outcome
Sagittal X-ray films analysis
-
1.
Lumbar and pelvic balance. Statistical analysis showed no significant difference between values calculated at different follow-up exams for lordosis and pelvic parameters. Moreover, their values were within normal ranges [3, 19, 38] over time, except for three cases (6%), discussed hereafter. During all follow-up (including before surgery), low lordosis and pelvic parameters were observed in two patients, and high values of pelvic version and incidence in a third case, with no significant evolution.
-
2.
Adjacent levels degeneration. Globally, the rate of acquired adjacent level degeneration was 8% (4 cases) at 5 years and 18% (4 + 5 new cases) at 9 years follow-up, according to both qualitative and quantitative criteria; most significant findings are presented in the following.
In qualitative analysis, osteophytes and vertebral endplate sclerosis were associated with degenerative changes in 7/9 cases (except for two cases of stenosis).
The most significant quantitative parameters (P < 0.0001, Table 4) individually associated with disc degeneration were represented by the evolutive decrease of lordosis within the fused segment, significant changes in posterior disc height and the hypermobility of the adjacent level. Association of these parameters did not increase the degree of correlation.
Moreover, comparing to reference values, low lordosis of the fused segment was found in 5/49 patients in all exams (including preoperatory), but not associated with degenerative changes.
Lumbar flexion-extension analysis
The following paragraphs summarize the results of the analysis at each intervertebral level of ROM and location of mean centres of rotation (MCR) related to reference values that were found in agreement with the literature (Fig. 3 for ROM, [25, 36] for MCR).
-
1.
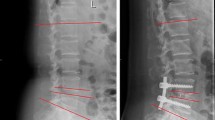
Analysis of the fused segment
ROM for the instrumented intervertebral segments were found between 0° and 5° during the follow-up, except for two patients presenting ROMs of respectively 5° and 6° at mid- and long-term exams. Similar values were obtained at 2 years, 5 years and last follow-up, as presented in Fig. 5.
Therefore, at last follow-up, instrumented segment mobility was:
-
Not significant (0°–3°) in 39 (80%) cases, for whom the clinical outcome was good and very good.
-
Low (3–5°) in eight cases (16%), having a good and fair clinical outcome associated with pain episodes and in 4/8 cases to late degenerative changes.
-
Significant of a pseudarthrosis (>5°) in 2 patients (4%), both presenting screw breakage and fair clinical outcome (revision surgery was needed in one case).
According to these results, long-term fusion was found in 80% of cases and a good correlation (r = 0.8) was noted between assessed fusion and clinical outcome. Furthermore, an agreement of 87% was noted between surgeon’s qualitative grading and our findings. The difference corresponds mainly to the cases assessed as doubtful fusion (16%) by our criteria. The pseudarthrosis rate results to be 4% in this series.
-
2. For the adjacent levels, mean mobility was quasi-constant during time. ROMs were between 0° and 19°, average 7° at short-term exam and 9° at mid- and long-term exams. However, a certain evolution was highlighted analytically: Table 5 shows the intervertebral mobility and location of MCR for the considered level in comparison to reference values at different periods of the follow-up. In addition, for the level above (adjacent +1) ROM was normal at long-term exam for 45% of patients, low in 48% of cases and high (comparing to reference values) in 7% of patients. MCR location was normal in 48% of these patients, abnormal for 20% and not calculated in 32% (ROM < 3°).
Discussion
Clinical outcome
The purpose of our study was to evaluate the interest of quantitative analysis in outcome assessment. A significant correlation (r = 0.8) was found between global clinical outcome (good and very good for 90% of patients) and fusion (rate 79% at mid-term and 80% at long term). These findings are in agreement with a meta-analysis of literature by Turner et al. [37], who evaluated the range of outcomes to 16–95% (mean 68%) and the fusion rate at 85.6% (56–100%), with a positive relation between fusion and satisfactory outcomes. Two studies evaluated a statistical relationship between fusion and clinical outcome: a slight correlation was observed by Diedrich et al. [7] (fusion rates 61.4% at mid-term and 77.8% at long term), while Wetzel et al. [39] found a good correlation, corresponding to a fusion rate of 61%. Though the fusion rates are similar to the former, our results seem to be more in agreement with the latter study and generally comparable to the literature.
Radiological outcome
Though quantitative analysis may seem complicated for the average spine surgeon, computer aided methods are rapid (average 10 min) and reproducible, helping in outcome assessment. Thus, a large panel of parameters was calculated in order to accurately describe lumbar spine geometry and kinematics during the follow-up. However, only some of them were relevant for patient’s postoperative evaluation and will be discussed in the following.
Sagittal X-ray films analysis
-
1.
Lumbar and pelvic parameters
Statistical analysis did not highlight any relevant evolution or abnormal values for these parameters. Furthermore, they were not correlated with the global outcome, in agreement with the studies of Lazennec et al. [18], who evaluated the possible correlation between pelvic parameters, L1S1 lordosis and postoperative pain, and of Korovessis et al. [16], who investigated on the role of sacral slope, lordosis and vertebral parameters in outcome assessment for posterior lumbar fusion.
-
2.
Adjacent levels degeneration
Solid fusion is believed to accelerate degeneration of the adjacent levels. Ghiselli et al. [9] announced a rate of symptomatic degeneration of 16.5% at 5 years and 36.1% at 10 years follow-up, which is superior to values observed in our population: i.e. 8% at 5 years and possibly 18% (out of 49 patients in our initial population) at 9 years follow-up. However, the last value (at 9 years) is to be interpreted with caution, because the 9 years radiological follow-up was not available in all patients. Moreover, it is generally difficult to determine if degenerative changes occurring 9 years after the surgery were strictly due to the surgery itself or to the ageing process, since there are no published studies clearly evaluating symptomatic disc degeneration related to ageing, which would allow a finer analysis.
Several clinical studies [5, 9, 11, 22, 29] reported adjacent level degeneration after lumbar fusion, investigating various factors as disc narrowing, progressive slippage of the vertebral body, osteophytes and vertebral endplate sclerosis but none could highlight their correlation. Comparing to a study of Okuda et al. [22], who hypothesized that adjacent level degeneration was related to laminar inclination that affects sagittal stability and abnormal rotation that increases tensile stress in the intervertebral disc, in our study vertebral parameters describing sagittal stability were not associated with degenerative changes, which were correlated (r = 0.6) with hypermobility only. Moreover, conversely to a study of Schlegel et al. [29], hypolordotic fixation of the fused segment (observed in five cases in our series) was not associated with adjacent level degeneration, as sagittal alignment was normal.
In this study, the quantitative parameters correlated to degenerative changes were the evolutive decrease of lordosis within the fused segment, the narrowing of posterior disc height and the hypermobility of the adjacent level. Conversely to the lordosis of the fused segment, significant changes in posterior disc height (or posterior disc/ vertebra height ratio, which is a more reliable evaluation of this parameter) were better correlated to degeneration than its decrease. These quantified signs of degeneration may be observed before a pronounced presence of osteophytes (beginning with grade 1–2), which means a possible early detection of risk of degeneration.
Lumbar flexion-extension analysis
Generally, difficulties arise from the absence of universally accepted imaging means [2, 3, 13, 15] or definitive criteria [20, 28] to assess the success of a posterolateral lumbar or lumbosacral fusion. A study of Christensen et al. [6] showed acceptable reliability (70%) in interpreting radiographic lumbar posterolateral fusion. Common criteria are qualitative and depending on observer’s experience [13]: i.e. the lack of motion on dynamic X-ray films and continuous bridging within the intervertebral space [8, 10, 15].
Tajima et al. [35] and Santos et al. [28] quantified the mobility of the fused segments and proposed a cut-off value of 2° for the residual motion, but this value does not take into account the measurement error (manual) which was not documented. A cut-off value of 5° was prescribed by The United States Food and Drug Administration [20]. Using this value, fusion rate in this series should be of 96%, which is within literature ranges [6, 7, 10, 15, 28, 35, 37]. In our study, a cut-off value of 3° was used to detect residual motion; as this threshold is higher than the uncertainty of angles measurements [3], it allowed quantifying low (3°–5°) residual motion that was associated with pain episodes and degenerative changes for our patients, classed as doubtful fusion, which should be further studied.
In this retrospective analysis, fusion rates obtained at mid- and long-term and last follow-up were quite similar (79% vs. 78% vs. 80% for ROM <3°), which encouraged us to consider their validity. Moreover, when comparing the qualitative notes of the senior surgeon (Ch. M.) and the results obtained with our criteria, an agreement was found in 87% of cases. Differences corresponded to the cases assessed as doubtful fusion. Given the variability in grading fusion by qualitative X-ray films analysis [13] and the good correlation between clinical outcome and fusion assessed for our population, the criteria stated to assess non-union seem to be appropriate. In spite of all these interesting findings, a prospective study on a larger population is necessary in order to fully validate this hypothesis in routine clinical practice.
The low mobility of adjacent segment could be explained for the early follow-up by postoperative diminished function due to postoperative pain; however, beginning with the mid term follow-up, it suggested an increased stiffness that might correspond to the ageing spine and/or to modified load distributions related to the dynamic instrumentation.
To summarize, clinical data outlined 90% of satisfactory results that are comparable to literature. In addition, quantitative analysis accurately described lumbar spine geometry and kinematics, highlighting 8% of adjacent level degeneration at 5 years follow-up, associated within this level with presence of osteophytes, hypermobility, narrowing of the posterior disc height and also with evolutive decrease of local lordosis within the fused segment. Moreover, accurate analysis of ROM allowed to test some criteria proposed to evaluate fusion from lumbar dynamic radiographs, which seem to be appropriate and in agreement with surgeon’s qualitative grading (in 87% of cases). They highlighted 4% of pseudarthrosis, a significant correlation between clinical outcome and fusion and a possible association between low residual motion on the fused segment, adjacent level degeneration and pain, leading to lower outcomes; however, all these findings need to be validated by further prospective studies on a larger scale.
Conclusion
This retrospective study offered a detailed insight into the outcome of posterolateral lumbosacral fusion with dynamic instrumentation, combining clinical outcome assessment with accurate quantitative evaluation of lumbar spine geometry and kinematics. Thus, in addition to clinical outcomes comparable to literature, 8% of adjacent level degeneration at 5 years follow-up could be detected, as well as residual motion of the fused segment, accurately interpreted in fusion grading, and some amount of adjacent levels long-term stiffness. These findings suggested that quantitative analysis may help in accurate outcome assessment and further comparison between studies.
References
Akamaru T, Kawahara N et al (2003) Adjacent segment motion after a simulated lumbar fusion in different sagittal alignments: a biomechanical analysis. Spine 28(14):1560–1566
Brodsky AE, Kovalsky ES, Khalil MA (1991) Correlation of radiologic assessment of lumbar spine fusions with surgical exploration. Spine 16(Suppl 6):S261–S265
Champain S, Benchikh K, Nogier A et al (2006) Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J 15(6):982–991
Cheung J, Wever DJ, Veldhuizen AG et al (2002) The reliability of quantitative analysis on digital images of the scoliotic spine. Eur Spine J 11:535–542
Chou WY, Hsu CJ, Chang WN et al (2002) Adjacent segment degeneration after lumbar spinal posterolateral fusion with instrumentation in elderly patients. Arch Orthop Trauma Surg 122(1):39–43
Christensen FB, Laursen M, Gelineck J et al (2001) Interobserver and intraobserver agreement of radiograph interpretation with and without pedicle screw implants: the need for a detailed classification system in posterolateral spinal fusion. Spine 26(5):538–543
Diedrich O, Perlick L, Schmitt O et al (2001) Radiographic characteristics on conventional radiographs after posterior lumbar interbody fusion: comparative study between radiotranslucent and radioopaque cages. J Spinal Disord 14(6):522–532
Frobin W, Brinckmann P, Leivseth G et al (1996) Precision measurement of segmental motion from flexion-extension radiographs of the lumbar spine. Clin Biomech 11(8):457–465
Ghiselli G, Wang JC, Hsu WK et al (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86-A(7):1497–1503
Godde S, Fritsch E, Dienst M et al (2003) Influence of cage geometry on sagittal alignment in instrumented posterior lumbar interbody fusion. Spin 28(15):1693–1699
Goto K, Tajima N, Chosa E et al (2003) Effects of lumbar spinal fusion on the other lumbar intervertebral levels (three-dimensional finite element analysis). J Orthop Sci 8(4):577–584
Graftiaux AG, Wattier B, Gentil P et al (1995) Biomechanical evaluation of different instrumentation for spinal stabilisation. Eur J Orthop Surg Traumatol 5:265–269
Hamill CL, Simmons ED (1997) Interobserver variability in grading lumbar fusions. J Spinal Disord 10(5):387–390
Hayes MA, Howard TC, Gruel CL et al (1989) Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine 14(3):327–331
Kant AP, Daum WJ, Dean SM et al (1995) Evaluation of lumbar spine fusion. Plain radiographs versus direct surgical exploration and observation. Spine 20:2313–2317
Korovessis P, Papazisis Z, Koureas G et al (2004) Rigid, semirigid versus dynamic instrumentation for degenerative lumbar spinal stenosis: a correlative radiological and clinical analysis of short-term results. Spine 29(7):735–742
Lassale B, Deburge A, Benoist M (1985) Résultat à long terme du traitement chirurgical des sténoses lombaires. Rev Rhum Mal Ostéoartic (52):27–33
Lazennec JY, Ramare S, Arafati N et al (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9(1):47–55
Legaye J, Hecquet J, Marty C et al (1993) Equilibre sagittal du rachis. Rachis 5(5):215–226
McAfee PC, Boden SD et al (2001) Symposium: a critical discrepancy —criteria of successful arthrodesis following interbody spinal fusions. Spine 26(3):320–334
Mazel Ch (1995) Instrumentation rachidienne flexible Twinflex dans les arthrodeses lombaires et lombosacrées—serie de 114 cas avec un recul minimal de 1 an. Eur J Orthop Surg Traumatol 5:271–277
Okuda S, Iwasaki M, Miyauchi A et al (2004) Risk factors for adjacent segment degeneration after PLIF. Spine 29(14):1535–1540
Ostermann H, Sund R, Seitsalo S et al (2003) Multiple reoperations after lumbar discectomy. Spine 28(6):621–627
Pearcy M, Portek I, Shepherd J (1984) Three-dimensional X-ray analysis of normal movements in the lumbar spine. Spine 9(3):582–587
Pearcy MJ, Bogduk N (1988) Instantaneous axes of rotation of the lumbar intervertebral joints. Spine 13(9):1033–1041
Rajnics P, Pomero V, De Guise J et al (2001) Computer-assisted assessment of spinal sagittal plane radiographs. J Spinal Disord 14:135–142
Rillardon L, Levassor N, Guigui P et al (2003) Validation of a tool to measure pelvic and spinal parameters of lumbar and pelvic balance. Rev Chir Orthop Reparatrice Appar Mot 89(3):218–227
Santos ER, Goss DG, Morcom RK, Fraser RD et al (2003) Radiologic assessment of interbody fusion using carbon fiber cages. Spine 28(10):997–1001
Schlegel JD, Smith JA, Schleusener RL (1996) Lumbosacral motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine 21:970–981
Schofferman J, Reynolds J, Herzog R et al (2003) Failed back surgery: etiology and diagnostic evaluation. Spine J 3:400–403
Shea KG, Stevens PM, Nelson M et al (1998) A comparison of manual versus computer-assisted radiographic measurement. Intraobserver measurement variability for Cobb angles. Spine 23:551–555
Siambanes D, Mather S (1998) Comparison of plain radiographs and CT scans in instrumented posterior lumbar interbody fusion. Orthopedics 21(2):165–167
Skalli W, Lavaste F (2002) Informatique et modélisation statique et dynamique du rachis. Cahiers d’enseignement de la Sofcot, Chirurgie orthopédique assistée par ordinateur 80:209–221
Stagnara P, De Mauroy JC, Dran G et al (1982) Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for evaluation of kyphosis and lordosis. Spine 7(4):335–342
Tajima N, Kawano K, Sera K et al (1989) Posterolateral fusion of the lumbar and lumbosacral spine—a review of long term results. Nippon Seikeigeka Gakkai Zasshi 63(4):262–268
Templier A, Skalli W, Diop A et al (1999) Evaluation radiographique quantitative des arthrodèses rachidiennes lombaires: protocole et analyse préliminaire d’une série multicentrique de 119 cas. Rachis 23–37
Turner JA et al (1992) Patient outcomes after lumbar spinal fusions. JAMA 268(7):907–911
Vialle R, Levassor N, Rillardon L et al (2005) Radiographic analysis of the sagittal alignement and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am 87(2):260–267
Wetzel FT, Brustein M, Phillips FM et al (1999) Hardware failure in an unconstrained lumbar pedicle screw system. A 2-year follow-up study. Spine 24(11):1138–1143
Acknowledgments
The authors wish to thank Mrs. C. Enout and IMM archives staff for their kind help and to SpineNetwork for their support (grant for a PhD project controlled by the National Agency for Technological Research (ANRT): CIFRE n° 677/2002).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Champain, S., Mazel, C., Mitulescu, A. et al. Quantitative analysis in outcome assessment of instrumented lumbosacral arthrodesis. Eur Spine J 16, 1241–1249 (2007). https://doi.org/10.1007/s00586-006-0302-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-006-0302-x