Abstract
We investigated the osseointegration of solvent-preserved, xenogenous cancellous bone blocks in the treatment of unstable fractures of the thoracolumbar junction. In 22 patients, the anterior repair procedure was performed by thoracoscopy or minimally invasive retroperitoneal surgery. Twenty-two patients had undergone monosegmental anterior fusion and were surveyed prospectively. Solvent-preserved, bovine cancellous bone blocks were used in 11 patients; iliac crest bone graft was used in the others. Follow-up after 12 months included CT scans, which revealed successful osseointegration in eight out of 11 patients who had received autogenous iliac crest bone grafts, while three patients showed a partial integration. There were no graft fragmentations. In patients who had received solvent-preserved, xenogenous cancellous bone blocks, complete osseointegration was achieved at the graft–bone interface in only two out of 11 cases, after 1 year. Partial integration was found in three patients. In view of these results, autogenous iliac crest bone grafts are still the unrivalled standard for defect repair in spinal surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A large percentage of unstable vertebral fractures of the thoracolumbar spine involve a destruction of the anterior column. In burst fractures, imploded intervertebral disc material prevents osseous consolidation, so that posterior reduction and instrumentation frequently lead to unsatisfactory results. To achieve the treatment objective of anatomical reconstruction, it is frequently necessary to additionally revise and stabilize the anterior column.
Minimally invasive techniques are becoming more widespread, especially in anterior spinal surgery, due to improved technologies [3, 4, 5, 14, 16, 22, 24, 25, 29]. Stabilization plays an important role in spinal fracture treatment. Sophisticated systems like the Z-plate or the MACS TL system have been developed for endoscopic application [3, 16, 22, 24, 29]. Because of these improvements monosegmental fusion has become an alternative in the minimally invasive treatment of A 3.1 fractures [3, 4, 5, 16, 24, 29]. After removal of the disc, stabilization was performed with structural bone graft and overbridging monosegmental stabilization between the adjacent endplate and the impacted vertebral body, to prevent postoperative loss of correction and kyphotic deformity [16].
Due to these modern techniques, it was possible to minimize the approach-related trauma of the anterior procedure. However, donor site morbidity such as pain and dysesthesia at the iliac crest are becoming more important problems [2, 6].
The search for an alternative reconstruction material is still under way and ranges from the use of fibula via rib segments to titanium bodies for vertebral body replacement [7, 9, 11, 12, 17, 18, 20, 28, 30]. Problems include cost, lack of long-term results concerning osseointegration and sintering, loosening and mechanical failure of spacers.
Other alternatives include allogenous transplants, with the residual risk of transmitting infections and the necessity of cost-intensive bone-bank management.
With the introduction of bovine, solvent-preserved cancellous bone blocks (Tutoplast bovine cancellous bone block, Tutogen, Erlangen, Germany) a European Community-certified bone material is commercially available in standardized sizes. In vitro tests showed a high biomechanical resistance to axial loads, and osseointegration was observed in an animal model [10].
The aim of this study was the comparison of the osseointegration of autogenous iliac crest strut grafts or Tutoplast solvent-preserved, bovine cancellous bone blocks in monosegmental anterior fusion in the minimally invasive treatment of thoracolumbar fractures.
Material and methods
In 22 patients suffering from spine fractures, an endoscopic (T3–L1) or minimally invasive retroperitoneal monosegmental (L2–L4) fusion was performed [3, 4, 5, 16, 29].
Twenty-one fresh fractures and one old fracture were treated (Table 1). Mean age of the six female and 16 male patients was 39±14 years. Indications for operative treatment were restrictively evaluated according to the Magerl classification, after preoperative X-ray and CT scan, individually and independently from the technique of an anterior procedure [21].
According to the nature of the injury and AO (German acronym for “the working group on osteosynthesis”) classification, patients with type B and C distraction and/or rotation signs, or patients with a neurological deficit associated with higher-grade structural damage to the vertebral body, were stabilized by a combined anterior-posterior instrumentation. In some type A compression injuries only an anterior procedure with monosegmental stabilization was performed. Indications for an additional anterior procedure after a dorsal instrumentation were a significant narrowing of the spinal canal and/or the necessity of a reconstruction of the weight-bearing column because of higher-grade structural damage and anterior misalignment.
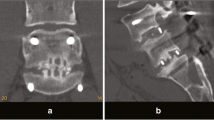
Most patients underwent posterior stabilization under emergency conditions, in the case of neurological deficits with laminectomy, using the Universal Spine System (USS, Stratec Medical, Umkirch, Switzerland) or the Compression Plate System (Litos, Hamburg, Germany) for posterior instrumentation (Fig. 2).
All patients were informed about the alternatives to the bone material to be implanted. Bone graft implantation was performed using a press-fit technique and a fixed-angle four-point implant was used anteriorly to achieve a high primary stability (MACS TL, Aesculap, Tuttlingen, Germany) or Z-Plate (Medtronic Sofamor Danek, Minneapolis, USA) in thoracoscopic or minimally invasive technique [29]. Autogenous grafts were obtained with chisels from the iliac crest as three-cortical structural grafts.
Solvent-preserved, bovine cancellous bone blocks were used in 11 of these patients (average age 40±12 years) (Tutoplast bovine, cancellous bone blocks, Tutogen, Erlangen, Germany); autologous, tricortical iliac crest strut grafts were used in the others (average age 39±16 years). Due to the given sizes (maximum height of 3 cm), we only used Tutoplast blocks (10 mm×10 mm×20 mm or 20 mm×20 mm×30 mm) for monosegmental fusion in this study. During the operative procedure, the material is easy to manipulate and can be adapted well. A high primary resistance to pressure was described by the manufacturer (153 kg/mm2).
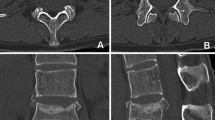
The radiological and clinical examination was performed after 6 months and 12 months according to the standard of the DGU (German Society of Trauma Surgery) working group on spine surgery, with the help of a typical spine score for evaluating pain symptoms and subjective overall assessment of level of activity, and radiological findings [18]. Conventional X-ray with anteroposterior and side view and CT scans were done with thin slices (1.5 mm) (Phillips MX 8000 IDT, Germany). Osseointegration was evaluated together with a radiologist in the proximal and distal regions of the graft bed via CT scan with sagittal, coronal and horizontal visualization. Complete osseointegration was considered radiologically as bony integration at the cranial and caudal endplates of the bone graft in the graft bed. Partial osseointegration was considered to exist if one of the two contact areas integrated. If no bony bridging occurred the graft was considered not integrated.
Results
All 22 patients were followed up. CT scans after 12 months revealed osseointegration in eight out of 11 patients who had received autogenous iliac crest grafts, while three patients showed a partial integration. There were no graft fractures.
In the Tutoplast group complete osseointegration was demonstrated in two cases at the contact areas (Fig. 1). In two patients, bridging ossifications along the anterior spinal ligament had formed, but the bone substitute was not integrated at the contact areas (Fig. 2). Partial integration of the cancellous bone block was found in another three patients (Fig. 3). No osseous integration at all was seen in four cases.
In four cases, graft morphology of the bovine material suffered fragmentation with consecutive sclerosing of the graft bed (Fig. 4).
In one of these patients, implant failure occurred ventrally, with a loss of correction of 30°, thus an operative revision was required. Clinical findings of an infection were established during the intervention; however, pathogens could not be identified (Fig. 5). After replacement with an autogenous iliac crest strut graft and stabilization, complete healing occurred within the next 6 months.
A median loss of correction of 5 was measured in both groups. The 90th percentiles ranged from +2° to −15 for the autogenous iliac crest strut graft and from −2° to −10 when Tutoplast material was used.
Discussion
The study compared the osseointegration of autogenous, tricortical iliac crest strut grafts and Tutoplast solvent-preserved, bovine cancellous bone blocks in monosegmental minimally invasive anterior fusion. After 12 months complete osseointegration was demonstrated in eight of 11 patients with autogenous grafts but only two of 11 with the bone substitute.
Since the introduction of minimally invasive procedures in spinal surgery, the approach-related trauma for anterior fusions has been considerably reduced in thoracolumbar fracture treatment. Monosegmental fusion of A 3.1 fractures is becoming more widespread, especially in thoracoscopically and minimally invasive spinal surgery, due to dedicated stabilization systems [3, 4, 5, 16, 22, 24, 29]. Fracture classification with regard to the existing ventral defect was comparable for all patients in this study, since only fractures eligible for monosegmental anterior repair were included. Instrumentation was mostly performed combined with angle-stable implants. Due to the minimally invasive technique, clinical outcome resulted in decreased approach-related pain.
Postoperative discomfort due to the harvesting of corticocancellous bone grafts from the iliac crest is an increasingly important problem [2, 4, 6, 16]. This fact and complication rates of up to 39% lead us to search for alternative ways to reconstruct the anterior column [2, 26]. This includes allogenous transplants, with the residual risk of transmitting infections and the necessity of a cost-intensive bone-bank management. Several spacers for vertebral body replacement are currently on the market. However, these are expensive alternatives, and there is a lack of long-term results considering the osseointegration of these spacers with mounted cancellous bone, sintering and loosening. For the most part, only primary stability tests have been presented [1, 7, 11, 12, 20, 23, 28]. Good long-term results with strut grafting and anterior stabilization were published only by Kaneda [15]. With the introduction of bovine, solvent-preserved cancellous bone blocks, there are European Community-certified bone materials available. There is no risk of transmission of infection by the material, due to the sterilization procedures performed [13]. Animal studies showed a proper osteogenous integration of the material [10]. However, to overcome the antigenicity of xenogenous tissues, the grafts are submitted to a chemical process that ensures their biotolerance, but also reduces their osteoinductive potential.
In our study, we investigated the integration behavior of solvent-preserved, bovine cancellous bone blocks compared to autogenous, tricortical iliac crest strut grafts. In contrast to the animal studies [10] the comparison of the integration behavior of the solvent-preserved, cancellous bone blocks showed a marked delay compared with autogenous iliac crest strut grafts.
Complete osseointegration was demonstrated only in two cases in the bone substitute group. Due to their primary stability, the bovine, solvent-preserved cancellous bone blocks tolerate the initial postoperative load bearing. However, the delayed bony ingrowth led to fragmentation and fissurations. Eventually, immunological processes may affect these reactions, thus leading to implant failure, as demonstrated in one case in this study (Fig. 5). The delayed ingrowth lead to anterior bony bridging along the anterior ligament in two cases, but no osseointegration was found at the contact area.
In the long term, the non-union rate of the solvent-preserved cancellous bone seems to be well above the reported values of 5–35% when using autogenous material [8]. The total number of patients in this study is limited, but due to the aforementioned results, the use of bovine cancellous bone blocks is not considered reliable for the spine, and, therefore, we have discontinued using this material altogether. It is well-known that similar problems may occur with autografts, however their failure rate appears significantly lower [19]. In view of the results obtained, the autogenous iliac bone graft has to be regarded as the standard technique for anterior reconstruction. The rate of donor site problems should not be disregarded, but rather their incidence should be minimized by an adequate operative technique, respecting anatomical structures and with a meticulous handling of the soft-tissue envelope [27].
References:
An HS, Lim TH, You JW, Hong JH, Eck J, McGrady L (1995) Biomechanical evaluation of anterior thoracolumbar spinal instrumentation. Spine 20(18):1979–1983
Banwart JC, Asher MA, Hassanein RS (1995) Iliac crest bone graft harvest donor site morbidity. A statistical evaluation. Spine 20:1055–1060
Beisse R, Potulski M, Temme C, Buhren V (1998) [Endoscopically controlled division of the diaphragm. A minimally invasive approach to ventral management of thoracolumbar fractures of the spine]. Unfallchirurg 101(8):619–627
Beisse R, Potulski M, Buehren V (2001) Endoscopic techniques for the management of spinal trauma. European Journal of Trauma 6:275–291
Buhren V, Beisse R, Potulski M (1997) [Minimally invasive ventral spondylodesis in injuries to the thoracic and lumbar spine]. Chirurg 68(11):1076–1084
Defino HL, Rodriguez-Fuentes AE (1999) Reconstruction of anterior iliac crest bone graft donor sites: presentation of a surgical technique. Eur Spine J (8):491–494
Dick JC, Brodke DS, Zdeblick TA, Bartel BD, Kunz DN, Rapoff AJ (1997) Anterior instrumentation of the thoracolumbar spine. A biomechanical comparison. Spine 22(7):744–750
Finkelstein JA, Chapman JR, Mirza S (1999) Anterior cortical allograft in thoracolumbar fractures. J Spinal Disord 12:424–429
Ghanayem AJ, Zdeblick TA (1997) Anterior instrumentation in the management of thoracolumbar burst fractures. Clin Orthop (335):89–100
Günther KP, Scharf HP, Pesch HJ, Puhl W (1996) Osteointegration lösungsmittelkonservierter Knochentransplantate im Tiermodell. Osteologie 5:4–12
Hitchon P GV, Rogge T, Grosland N, Torner J (1999) Biomechanical studies on two anterior thoracolumbar implants in cadaveric spines. Spine 24:213–218
Hitchon PW GV, Rogge TN, Torner JC, Dooris AP, Drake JS, Yang SJ, Totoribe BS, Totoribe K (2000) In vitro biomechanical analysis of three anterior thoracolumbar implants. J Neurosurg 93:252–258
Hofmann A, Hofmann C, Gotzen L (2000) [Effect of various bone disinfection and sterilization methods on osteoblast function. A comparative in vitro study]. Unfallchirurg 103:380–388
Huang TJ, Hsu RW, Liu HP, Hsu KY, Liao YS, Shih HN et al (1997) Video-assisted thoracoscopic treatment of spinal lesions in the thoracolumbar junction. Surg Endosc 11:1189–1193
Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M (1997) Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am 79:69–83
Khoo L, Beisse R, Potulski M (2002) Thoracoscopic-assisted treatment of thoracic and lumbar fractures: a series of 371 consecutive cases. Neurosurgery Nov (51):104–117
Kifune M, Panjabi MM, Liu W, Arand M, Vasavada A, Oxland T (1997) Functional morphology of the spinal canal after endplate, wedge, and burst fractures. J Spinal Disord 10:457–466
Knop C, Blauth M, Buhren V, Hax P, Kinzl L, Mutschler W et al (2000) [Surgical treatment of injuries of the thoracolumbar transition. 2: Operation and roentgenologic findings]. Unfallchirurg 103:1032–1047
Kossmann T, Ertel W, Platz A, Trentz O (1999) [Combined surgery for fractures of the thoraco-lumbar junction using the inlay-span method]. Orthopade 28:432–440
Kotani Y, Cunningham BW, Parker L, Kanayama M, McAfee P (1999) Static and fatigue biomechanical properties of anterior thoracolumbar instrumentation systems. A synthetic model. Spine 14:1406–1413
Magerl F, Aebi M, Gretzbein SD, Harms J, Nazarian S (1994) A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 3:184–201
Mayer HM (2000) Minimally invasive spine surgery. A surgical manual. Springer, Berlin Heidelberg New York
McAfee PC, Regan JR, Fedder IL, Mack MJ, Geis WP (1995) Anterior thoracic corpectomy for spinal cord decompression performed endoscopically. Surg Laparosc Endosc 5(5):339–348
Potulski M, Beisse R, Buhren V (1999) [Thoracoscopy-guided management of the “anterior column”. Methods and results]. Orthopäde 28:723–730
Regan JJ, Guyer RD (1997) Endoscopic techniques in spinal surgery. Clin Orthop 335:122–139
Sandhu HS, Grewal HS, Parvataneni H (1999) Bone grafting for spinal fusion. Orthop Clin North Am 30:685–698
Schnee CL, Freese A, Weil RJ, Marcotte PJ (1997) Analysis of harvest morbidity and radiographic outcome using autograft for anterior cervical fusion. Spine 22:2222–2227
Schultheiss M, Hartwig E, Kinzl L, Claes L, Wilke HJ (2003) Axial compression force measurement acting across the strut graft in thoracolumbar instrumentation testing. Clin Biomech (Bristol, Avon) 18:631–636
Schultheiss M, Kinzl L, Claes L, Wilke HJ, Hartwig E (2003) Minimally invasive ventral spondylodesis for thoracolumbar fracture treatment: surgical technique and first clinical outcome. Eur Spine J 12:618–624
Zdeblick TA, Shirado O, McAfee PC, deGroot H, Warden KE (1991) Anterior spinal fixation after lumbar corpectomy. A study in dogs. J Bone Joint Surg Am 73:527–534
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schultheiss, M., Sarkar, M., Arand, M. et al. Solvent-preserved, bovine cancellous bone blocks used for reconstruction of thoracolumbar fractures in minimally invasive spinal surgery—first clinical results. Eur Spine J 14, 192–196 (2005). https://doi.org/10.1007/s00586-004-0764-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-004-0764-7