Abstract
Spine surgery may be associated with profuse intraoperative bleeding that often requires blood transfusions. In recent years several techniques have been developed to avoid allogenic transfusions and their potential complications to surgical patients. In this study we review and analyse the role of preoperative recombinant human erythropoietin (rHuEPO) administration in spine surgery as a blood conservation strategy. Between 1998 and 2002, a total of 250 patients scheduled for spine surgery were included in our blood-sparing program: 114 patients (group 1), operated on before rHuEPO approval (2000), underwent preoperative autologous blood donation (ABD) alone, and 136 patients operated on after rHuEPO approval (groups 2 and 3) received rHuEPO while undergoing ABD. Adding rHuEPO to ABD resulted in higher haemoglobin and haematocrit values the day of surgery, more ABD units retrieved per patient and, consequently, reduced allogenic transfusion requirements. The effectiveness of rHuEPO as the only preoperative blood conservation technique was evaluated in ten patients with a predicted blood loss of less than 30% of their total volume, scheduled for lumbar surgery. Data from these patients were matched with those from a similar group of patients who had undergone ABD. Patients receiving rHuEPO alone had higher haemoglobin levels the day of surgery than did patients in the ABD program. Neither group required allogenic transfusions. Conclusions: preoperative rHuEPO is useful for reducing allogenic blood requirements in elective spine surgery. In patients with an expected blood loss of around 50% of blood volume, rHuEPO improves ABD, minimising preoperative anaemia and increasing the number of ABD units collected. In patients with expected blood loss below 30% of total volume, rHuEPO administration may replace ABD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery for spinal deformities or degenerative lumbar disease may be associated with blood loss ranging from 30% to 100% of the patient’s total blood volume [18, 26, 68, 79, 85, 87]. This loss of blood is related to the complexity of the procedure, duration of surgery, number of fused levels, anaesthetic technique and the patient’s comorbid conditions [18, 26, 68, 76, 79, 85, 87]. Extensive bleeding may lead to rapid fatal consequences and to risks associated with allogenic blood transfusion [4, 8, 36, 40, 81]. Measures should be taken to minimise these risks [18, 26, 50, 58, 64, 65, 66, 68, 79].
Over the last 30 years, considerable efforts have been made to develop new blood-conservation strategies that will avoid allogenic transfusion. The most common include drug therapy (desmopressin [2, 58], aprotinin [25, 85], tranexamic acid [27, 65], hypotensive anaesthesia [59, 83], and autotransfusion techniques, such as normovolemic acute hemodilution [14, 19, 56, 67], perioperative salvage [3, 28, 56], postoperative salvage and autologous blood donation (ABD) [39, 49, 57, 64, 80, 88]. During the 1990s a new drug, recombinant human erythropoietin (rHuEPO), was added to the repertory of blood-conservation techniques [6, 9, 32, 33, 73]. This hormone plays a major role in patients undergoing elective surgery in which moderate or profuse blood loss is expected [22, 48, 74]. However, despite its approval for this purpose more than 3 years ago, very little information is available on its effectiveness in elective spine surgery [76, 77, 79, 86].
Erythropoietin
Erythropoietin (EPO) is a hormone that regulates erythropoiesis, acting on erythroid-colony-forming units by stimulating progenitor cell differentiation in the bone marrow. EPO accelerates maturation of proerythroblasts to reticulocytes, stimulates the synthesis of haemoglobin (Hb), and promotes the release of reticulocytes to the circulation and their differentiation into mature red blood cells [10, 20].
Erythropoietin is a 165-amino-acid glycoprotein with a molecular weight of 30,400 dalton. Approximately 90% is produced in the interstitial peritubular cells of the kidney. Normal plasma levels range 5–30 mU/ml and are regulated by tissue hypoxia and the various factors that influence oxygen availability in peripheral tissues [10, 20]. The human gene for erythropoietin is present as a single copy on chromosome 7 (q11–q22) and is comprised of 5 exons (582 base pairs) [10, 20, 48].
Recombinant human erythropoietin (rHuEPO) is a biosynthetic form of the natural hormone having the same biochemical structure and biological effect [12, 13, 20]. There are two types of rHuEPO: the alpha type and the beta type, presented in lyophilised form and reconstituted with saline solution [12, 13, 73].
Erythropoietin in surgery
Based on its success in the treatment of anaemia associated with chronic renal failure and chemotherapy [45, 52, 60], rHuEPO was contemplated for use in surgical patients to elevate preoperative haemoglobin values and facilitate the predeposit of autologous blood, thereby decreasing the need for allogenic blood transfusions. This hypothesis was confirmed in several studies involving orthopaedic surgery, [9, 16, 22, 23, 30, 53, 74], and this led to the registration of rHuEPO for clinical practice in Spain in October, 2000. It is now also used in cardiac, prostate and oncologic surgery for this purpose [52, 71, 73].
Dosing
Recombinant human erythropoietin can be administered intravenously or subcutaneously. It reaches peak plasma concentration faster by the intravenous route, although the half-life is shorter (5–10 h) [73]. Availability is lower with subcutaneous administration, but the half-life is longer (12–18 h) [73], and this route is usually recommended for the management of perioperative anaemia [12, 13, 48, 73].
Initially, the recommended dose was 300 IU/kg/day during 15 days [15]. However, Goldberg et al. [30] demonstrated that a weekly dose of 600 IU/kg starting 3 weeks before the procedure achieved a higher increase in haemoglobin (1.44g/dl vs 0.73 g/dl) with comparable safety and efficacy, and lower cost.
Current recommended dosage is 600 IU/kg of subcutaneous rHuEPO weekly, given over 3 weeks (days 21, 14, and 7 before the surgical procedure) and on the day of surgery. In practice, administration of a 40,000 IU vial weekly is recommended in adults with a mean weight of around 65 kg. The 40,000 IU dose is authorised exclusively for preoperative rHuEPO treatment. When haemoglobin levels reach 15 g/dl at any of the preoperative analyses, rHuEPO administration is interrupted indefinitely [6, 12, 13, 22, 23, 48, 82].
The dosing regimen for patients in the ABD program is somewhat different. Recommended dosage in these patients is 600 IU/kg (or a 40,000 IU vial), twice a week during the period that blood is being collected [5, 22, 23,24, 30, 41, 74, 82]. Again, when haemoglobin reaches levels above 15 g/dl, the dose is not administered.
Blood levels of ferritin, folic acid and vitamin B12 should be checked before initiating rHuEPO therapy. When concentrations of these blood components are low, additional treatment to recover adequate levels is essential before administration of rHuEPO. Oral administration of 200–300 mg/day of iron is necessary to compensate for the expenditure of ferritin reserves, due to the increasing erythrocyte mass in response to rHuEPO [6, 22, 51]. If possible, iron supplementation should be started at least 1 month before rHuEPO therapy to achieve adequate reserves and assure the efficacy of the hormone [29, 73].
Side effects
Recombinant human erythropoietin is considered to be a safe drug, although some side effects, such as headache, flu-like states and higher blood pressure levels in hypertensive patients have been observed [13, 21, 35].
Hemostasis studies in patients treated with rHuEPO have demonstrated a minimum effect on the coagulation cascade. No changes have been found in thrombin time, prothrombin time or activated partial thromboplastin time. A transient increase in platelet values, without exceeding normal limits, has been described [16, 31, 35].
With regard to increases in blood viscosity as the haematocrit rises, most authors agree that there is only a risk when the haematocrit exceeds 51% [13, 16, 31, 35, 51]. Analysis of the rHuEPO safety profile in 619 patients treated before orthopaedic surgery showed that the use of this hormone does not increase the risk of thromboembolic events [16, 31, 82].
Role of rHuEPO in preoperative autologous blood donation
Increasing awareness of the risks linked with transfusion of allogenic blood products has led to much more widespread use of preoperative autologous blood donation [72]. Nevertheless, ABD may involve certain problems inherent to the process, such as anaemia or adverse reactions on the part of the patient during donation, wastage of blood units due to delayed surgery, or clerical errors in blood labelling and storage [1, 4, 38, 74, 84]. Moreover, in certain circumstances it may be difficult to collect sufficient blood to cover the estimated loss during surgery [7, 17, 41, 43, 48, 70].
Even with the availability of anticoagulant preservation solutions, it is still necessary to perform blood withdrawal within a maximum of 42 days before the operation. For this reason, a considerable percentage of patients following an ABD program reach surgery with a lower haemoglobin value than when they entered the program [1, 37, 39, 42, 46, 61, 63], and when this value is significantly lower, their transfusion requirements increase [7, 11, 33, 43, 44, 48].
The interval between donations should not be less than 3 days, and the final collection should be performed at least 72 h before the operation [38, 72]. Patients with a moderate degree of anaemia (Hb 10–13 g/dl) and requiring a predeposit of more than 4 units will have serious difficulties providing sufficient autologous blood [17, 42, 46, 61, 62]. Erythropoiesis stimulation with rHuEPO can be very beneficial in these patients [17, 23, 41, 61, 71, 72, 84].
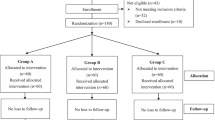
Since 1998, 250 patients have participated in the program of blood-sparing techniques in our spinal surgery unit. Candidates for this program include all patients undergoing spinal surgery whose expected blood loss is greater than or equal to 20% of their total blood volume and who have no contraindications for ABD. The exclusion criteria are urgent surgery, or predicted perioperative blood loss of less than 20% of the total volume. Approval of rHuEPO use in October 2000 resulted in changes in the treatment protocols for patients included in the program.
The 114 patients participating between 1998 and 2000 (group 1), 39 men and 75 women, were managed with ABD exclusively. The large majority had scoliosis or degenerative lumbar disease. Between 2001 and 2002, 136 patients were included in the program. These were divided into two groups according to their preoperative diagnosis and expected blood loss. Group 2 included 88 patients, 31 men and 57 women, with multilevel (two or more lumbar segments) degenerative lumbar disease and an expected perioperative blood loss of around 50% of the total volume. Group 3 comprised 48 patients, 10 men and 38 women, with idiopathic or degenerative adult scoliosis, or complex adult deformities and an expected blood loss of nearly 100% of the total volume. Demographic data from these groups are detailed in Table 1.
All patients followed a standard ABD program consisting of serial blood collection every 7 days (provided that haemoglobin levels remained above 10 g/dl) and 525 mg of ferric sulphate 3 times daily, starting approximately 2 months before surgery. Groups 2 and 3 additionally received subcutaneous rHuEPO at a dose of 40,000 IU, according to the above-described dosing regimen.
The baseline haemogram showed no major differences among the patient populations, although baseline haemoglobin levels were slightly higher in group 1 than in groups 2 and 3. A gradual decrease in haemoglobin was observed in group 1 as patients underwent serial blood collection (Table 2). In groups 2 and 3, haemoglobin levels remained constant at around 12.5 g/dl after the second collection and up to the day of surgery. The effect of rHuEPO on haemoglobin levels and the haematocrit in the three groups is shown in Figures 1a and 1b.
Haemogram values during the study. Haemoglobin a and haematocrit b were determined at the beginning of the study (baseline), before each rHuEPO administration and/or ABD and on the day of surgery. Groups 2 (●) and 3 (■) underwent up to five ABD and five rHuEPO administrations; and group 1 (◆) underwent ABD only
Table 3 summarises the proportion of patients meeting ABD previsions for each study group. The percentage of patients able to donate the anticipated required units was 83.9% in group 1, 100% in group 2 and 98% in group 3.
Recombinant human erythropoietin administration resulted in a higher number of donated autologous blood units (Tables 4 and 6), with a mean of 1.57 units per patient in group 1, 2.96 units per patient in group 2 and 4.19 units per patient in group 3 (Table 6). In groups 2 and 3 (ABD plus EPO), 50% of patients gave more than 3 units, whereas only 37.5% of patients in group 1 (ABD alone) were able to donate more than 3 units (Table 4). In group 3, which included patients with complex spinal deformities, expected blood loss of nearly 100% of total volume, and actual average blood loss of 3,408 cc (Table 5), 5 units were obtained in 18.4% of patients. This meant that 24 patients (50%) arrived at surgery with the anticipated coverage. In contrast, only 1.8% of patients in group 1 were able to provide 5 units.
In terms of effectiveness and waste, rHuEPO provides evident advantages in blood-sparing programs. First, it increases the efficacy of ABD by reducing the number of allogenic blood units required. With a similar mean blood loss in groups 1 and 2 (Table 5), transfusion of allogenic blood was necessary in 14 patients in group 1 (12.28%) and only two patients in group 2 (2.27%) (Table 6). Only seven patients (14.58%) in group 3 required allogenic blood, even though two of these seven patients had withdrawn from rHuEPO treatment during the study. A third patient in this group suffered a major complication during surgery (massive bleeding from vascular injury and loss of 16 l of blood). Excluding these three exceptional cases, the efficacy of ABD plus rHuEPO in this complex group would be 91.7%.
Autologous blood-donation waste, reflected in the number of non-transfused autologous blood units, was 16 ABD units in group 3 (8.12%), 45 ABD units (17.30%) in group 2 and 35 units (19.44%) in group 1 (Table 6).
Some of the patients in the program did not receive all of the rHuEPO anticipated, since their haemoglobin values exceeded 15 g/dl. In addition, the mean rHuEPO doses administered in both the treated groups were lower than those recommended [31]. In group 2, with a mean of 2.96 ABD units per patient, mean rHuEPO received was 3.28 doses per patient. In group 3, with 4.19 ABD units per patient, the number of rHuEPO doses was 4.75.
No adverse events were recorded in any of the patients receiving rHuEPO. Two patients from group 3 decided to stop rHuEPO treatment after the second blood collection, one because she was not convinced of the efficacy of this measure and the other because of general fatigue.
On the fifth postoperative day and at hospital discharge, all the patients studied presented haemoglobin levels and haematocrit within the normal range (Figures 2a and 2b).
Role of preoperative rHuEPO in elective surgery as the only blood-sparing technique
Various clinical trials have assessed the usefulness of rHuEPO as the only blood-sparing technique used in elective orthopaedic surgery (other than spine surgery) [15, 23, 24, 30, 55, 74, 82]. In several randomised, placebo-controlled trials, preoperative rHuEPO administration significantly reduced transfusion requirements. Treated patients present higher haemoglobin levels than controls on the day of surgery. This effect is evident in procedures where blood loss is expected to be approximately 30% of the patient’s total calculated volume [23, 53, 55, 74, 78]. Generally, this degree of blood loss is typical in primary, unilateral hip or knee arthroplasty.
A number of clinical trials [15, 22, 23, 24, 30, 31]have been conducted to determine the ideal preoperative dosing regimen for rHuEPO and the type of patient that can most benefit from this treatment. These studies included a total of 824 patients undergoing scheduled orthopaedic surgery, mainly arthroplasty of the hip, knee or shoulder, in which moderate blood loss (900–1800 ml or 25%–30% of total volume) was anticipated. Two different doses of rHuEPO (100 IU/kg or 300 IU/kg, subcutaneously) were used, beginning administration 10 days before surgery and ending 4 days after (15 doses) [15, 22, 23, 24, 30, 31].
The results of these studies suggest that a preoperative haemoglobin value greater than 13 g/dl is a good indicator that transfusion will not be needed [24]. Patients with haemoglobin levels of 10 to 13 g/dl at the beginning of treatment benefit the most from the effect of rHuEPO, with reductions in allogenic transfusions of 50% to 70% [15, 30, 31, 69]. In moderately anaemic patients approaching scheduled orthopaedic surgery, rHuEPO as a first-line treatment is well-tolerated and is associated with a shorter hospital stay [15]. As mentioned above, the recommended regimen nowadays is four doses of 600 IU/kg/week, beginning 3 weeks before surgery [31].
Using this dosing schedule, Stowell et al. [82] performed an open, randomised, multicenter study with parallel groups comparing the safety and efficacy of rHuEPO treatment (600 IU/kg on days −21, −14, −7 and 0) with that of standard ABD (2 predonated units). The study included 490 patients scheduled for total hip or knee arthroplasty, with baseline haemoglobin values of 10 to 13 g/dl. Haemoglobin levels over the entire preoperative period were higher in the rHuEPO group than in the ABD group. Mean haemoglobin values on the day of surgery were 13.8 g/dl in the patients receiving rHuEPO and 11.1 g/dl in the ABD patients. These differences resulted in a lower total transfusion rate (12.9% in rHuEPO vs 74.4% in ABD) and a lower rate of allogenic blood transfusion (12.9% in rHuEPO vs 19.2% in ABD). These data suggest that in patients with haemoglobin values greater than 13 g/dl, this type of surgery can be performed with lower transfusion requirements.
This technique has been applied in orthopaedic surgery in which the typical bleeding risk is around 30% of the total blood volume [24, 30, 33, 70, 82]. The characteristics of this type of surgery are similar to those of lumbosacral procedures.
Table 6 shows that there is a high percentage of wasted units of autologous blood in groups 1 and 2 of our series (19.4% and 17.3%, respectively). These two groups (particularly group 2) are comprised of patients who underwent lumbosacral surgery with blood losses (1,862 cc for group 1 and 1,793 cc for group 2) of around 30% of the total volume. We hypothesised that this type of patient could be managed without ABD, if haemoglobin values were above 13 g/dl at the day of surgery.
To investigate this idea we designed a case-control study comparing rHuEPO administration with ABD as single blood-sparing approaches in patients undergoing lumbosacral surgery, with expected blood losses of 30% of the total blood volume. The study included 20 patients scheduled for surgery to treat degenerative lumbar spine disease. Ten patients (EPO group) received treatment with 40,000 IU of rHuEPO in four separate doses given 21, 14 and 7 days before surgery and on the day of surgery. Data from these patients were cross-matched with data from patients managed with ABD alone (ABD Group). We identified 10 patients with diagnoses and surgical procedures similar to those of the EPO group, from whom an average of 2.8 units of autologous blood had been retrieved preoperatively.
As is shown in Table 7, the duration and type of surgery were similar in the two groups (p=0.1), although perioperative blood loss was significantly higher (p=0.03) in those who received rHuEPO. Baseline haemoglobin values were also comparable in the two groups (EPO group’s 12.9 g/dl vs ABD group’s 13.05 g/dl, p>0.1). Nevertheless, whereas in the EPO group haemoglobin had increased to 14.2 g/dl on the day of surgery, in the ABD patients haemoglobin had dropped to 10.7 g/dl (p=0.004). Haemoglobin levels on the day after surgery were still higher in the EPO group (11.9 g/dl vs 8.8 g/dl, p=0.005), but similar values were recorded on discharge from the hospital (EPO group’s 11.1 g/dl vs ABD group’s 11.1 g/dl, p>0.1). None of the patients in either group required allogenic blood transfusion.
In summary, the group treated with rHuEPO presented higher preoperative haemoglobin levels than those of the ABD group. Despite significantly greater intraoperative bleeding, none of the rHuEPO patients required allogenic blood transfusions and, upon discharge, haemoglobin levels were similar to those of the ABD group. Our results suggest that lumbosacral surgery with estimated blood losses lower than 30% of total blood volume can be performed without the need for allogenic blood if preoperative haemoglobin concentrations are higher than 13 g/dl. Recombinant human erythropoietin therapy is a safe, effective method to reach these levels.
Discussion
Autologous blood donation has become the gold standard for blood conservation in elective spine surgery. Nevertheless, this technique has some limitations, one of the most important being the anaemia caused by repeated blood collection, which can limit the number of units recovered and, in some cases, lead to clearly insufficient haemoglobin levels at the time of surgery [38, 41, 43, 47, 48, 57, 64]. Addition of rHuEPO therapy to the predonation program allows patients to undergo surgery with haemoglobin levels and haematocrit similar to those present before starting the program [74, 77, 79, 86]. Blood retrieval is not recommended in patients with haemoglobin levels lower than 11 g/dl. By maintaining adequate haemoglobin concentrations during repeated blood collection, it is possible to reduce the interval between donations and retrieve a larger number of autologous blood units, thereby covering the predicted requirements [17, 22, 23, 41, 50, 61]. The fact that patients approach surgery with high levels of haemoglobin despite autologous donation reduces transfusion requirements and confers important benefits with regard to postoperative recovery [23, 24, 69, 70, 71].
Blood management is most difficult in adult patients with complex deformities requiring very aggressive surgery with circumferential approaches and long spinal instrumentation. These patients, comprising group 3 of our series, can present blood losses equal to their total blood volume [79, 85]. Shapiro et al. [79] published a randomised controlled trial analysing the effect of rHuEPO treatment on patients in an ABD program. The patients had been scheduled for complex spinal reconstruction and were very similar to the patients in group 3 of our series in terms of type and duration of surgery, blood loss and number of days of hospitalisation. All those in the group treated with rHuEPO were able to comply with the foreseen perioperative autotransfusions, as compared to 78% of patients in the control group. Moreover, only 24% of patients receiving rHuEPO required allogenic transfusions, as compared to 83% in the control group. Our experience yielded findings similar to those reported in this study. In our complex patients, 98% complied with ABD estimations and only 14.6% required allogenic blood transfusion.
In patients with less aggressive surgery (group 2) and a predicted blood loss of around 50% of total volume, nearly 97% did not require allogenic transfusions when rHuEPO treatment was associated with the ABD program. However, a significant percentage of autologous donation units were not used (17.3%) in this group, whereas only 8.2% of donated units went wasted in the complex surgery group. Typically, 10% to 25% of autologous blood units are wasted in less aggressive surgery [32, 33, 34, 36, 47, 64, 81, 84].
The total recommended rHuEPO dose for ABD support is 3,600 IU/kg [31, 70, 82]. Our results show, however, that equally satisfactory results are obtained with lower doses: Group 2 received a total of around 1,900 IU/kg and group 3 received 2,800 IU/kg. Our data concur with those of Lee et al. [54], who reported improved performance in the ABD program (3 predeposit units) with administration of 1,200 to 1,500 IU/kg to patients scheduled for lumbosacral surgery. We believe it is advisable to adjust the total rHuEPO dose according to the haemogram. The total recommended dose can be decreased while maintaining the efficacy of the treatment. This will reduce the high cost of rHuEPO use, which is one of the disadvantages of this therapy.
In lumbar surgery with blood loss at around 30% of the total volume, the use of blood conservation strategies is questionable. Systematic application of ABD will lead to a high rate of wasted blood units, since it is difficult to estimate the autotransfusion requirements. Our results suggest that surgery in these patients can be carried out without recurring to transfusion, when the patient’s haemoglobin levels on the day of surgery are greater than 13 g/dl. This type of surgery would be equivalent to other orthopaedic techniques [6, 22, 24, 30, 70]. With rHuEPO administration, the required haemoglobin levels can be attained quickly and safely.
There were no adverse incidents associated with rHuEPO administration in our series. The high level of satisfaction indicated by the patients during the entire process was remarkable and contrasted with the discomfort associated with repeated blood collection. However, it is important that rHuEPO administration be individualised. Periodic haemograms must be performed to monitor both the haemoglobin levels and the haematocrit. The earliest response showing the effectiveness of rHuEPO administration is an increase in the number of reticulocytes, occurring between day 3 and day 10. The treatment should be withdrawn if haemoglobin levels exceed 15 g/dl [22, 30, 48]. This was the case in three out of ten patients who received treatment with rHuEPO alone, without ABD.
We conclude that surgery involving blood losses under 30% of the patient’s total volume can be accomplished without the need for allogenic transfusion, if the baseline haemoglobin level is greater than 13 g/dl. Recombinant human erythropoietin administration is very effective for attaining this level and can be used as the only blood-sparing technique in these patients.
When the expected blood loss is around 50% of the total volume, ABD is the standard technique applied. Addition of rHuEPO to ABD in these patients improves haemoglobin levels and facilitates retrieval of the autologous blood units required. This combination can avoid allogenic transfusion in 95% of the patients.
When surgery is associated with a predicted blood loss close to the patient’s total blood volume, the combined blood-sparing technique should always be used. Despite the complexity and aggressiveness of the procedure, with the combination of ABD and rHuEPO, more than 80% of the patients operated will not require allogenic transfusions.
References
Abildgaard L, Aaro S, Lisander B (2001) Limited effectiveness of intraoperative autotransfusion in major back surgery. Eur J Anaesthesiol 18:823–828
Alanay A, Acaroglu E, Ozdemir O, Ercelen O, Bulutcu E, Surat A (1999) Effects of deamino-8-D-arginin vasopressin on blood loss and coagulation factors in scoliosis surgery. A double-blind randomized clinical trial. Spine 24:877–882
Anand N, Idio FG Jr., Remer S, Hoppenfeld S (1998) The effects of perioperative blood salvage and autologous blood donation on transfusion requirements in scoliosis surgery. J Spinal Disord 11:532–534
Audet AM, Goodnough LT, Parvin CA (1996) Evaluating the appropriateness of red blood cell transfusions: the limitations of retrospective medical record reviews. Int J Qual Health Care 8:41–49
Beris P (1996) Epoetin alfa as an adjuvant to autologous blood donation. Semin Hematol 33:27–29
Beris P (1996) Epoetin alfa: new directions in orthopedic surgery. Semin Hematol 33:60–62
Beris P, Mermillod B, Levy G, Laubriat M, Soulier-Lauper M, Tullen E, Hugli A, Miescher PA (1993) Recombinant human erythropoietin as adjuvant treatment for autologous blood donation. A prospective study. Vox Sang 65:212–218
Blumberg N (1997) Allogeneic transfusion and infection: economic and clinical implications. Semin Hematol 34:34–40
Bose WJ (1996) The potential use of human recombinant erythropoietin in orthopedic surgery. Orthopedics 19:325–328
Browne JK, Cohen AM, Egrie JC, Lai PH, Lin FK, Strickland T, Watson E, Stebbing N (1986) Erythropoietin: gene cloning, protein structure, and biological properties. Cold Spring Harb Symp Quant Biol 51 Pt 1:693–702
Cha CW, Deible C, Muzzonigro T, Lopez-Plaza I, Vogt M, Kang JD (2002) Allogeneic transfusion requirements after autologous donations in posterior lumbar surgeries. Spine 27:99–104
Cheung W, Minton N, Gunawardena K (2001) Pharmacokinetics and pharmacodynamics of epoetin alfa once weekly and three times weekly. Eur J Clin Pharmacol 57:411–418
Cheung WK, Natarajan J, Sanders M, Vercammen E (2000) Comparative pharmacokinetics, safety, and tolerability after subcutaneous administration of recombinant human erythropoietin formulated with different stabilizers. Biopharm Drug Dispos 21:211–219
Copley LA, Richards BS, Safavi FZ, Newton PO (1999) Hemodilution as a method to reduce transfusion requirements in adolescent spine fusion surgery. Spine 24:219–222
de Andrade JR, Jove M, Landon G, Frei D, Guilfoyle M, Young DC (1996) Baseline hemoglobin as a predictor of risk of transfusion and response to Epoetin alfa in orthopedic surgery patients. Am J Orthop 25:533–542
de Andrade JR, Frei D, Guilfoyle M (1999) Integrated analysis of thrombotic/vascular event occurrence in epoetin alfa-treated patients undergoing major, elective orthopedic surgery. Orthopedics 22:s113–s118
de Pree C, Mermillod B, Hoffmeyer P, Beris P (1997) Recombinant human erythropoietin as adjuvant treatment for autologous blood donation in elective surgery with large blood needs (>or=5 units): a randomized study. Transfusion 37:708–714
Dorsey AT, Schwartz RE, Stayer SA, Pasquariello CA (1993) Scoliosis surgery: determinants of blood loss. Anesth Analg 76:684–685
Du TG, Relton JE, Gillespie R (1978) Acute haemodilutional autotransfusion in the surgical management of scoliosis. J Bone Joint Surg Br 60:178–180
Egrie JC, Strickland TW, Lane J, Aoki K, Cohen AM, Smalling R, Trail G, Lin FK, Browne JK, Hines DK (1986) Characterization and biological effects of recombinant human erythropoietin. Immunobiology 172:213–224
Eschbach JW, Egrie JC, Downing MR, Browne JK, Adamson JW (1991) The safety of epoetin-alpha: results of clinical trials in the United States. Contrib Nephrol 88:72–80
Faris P (1996) Use of recombinant human erythropoietin in the perioperative period of orthopedic surgery. Am J Med 101:28S-32S
Faris PM, Ritter MA, Abels RI (1996) The effects of recombinant human erythropoietin on perioperative transfusion requirements in patients having a major orthopaedic operation. The American Erythropoietin Study Group. J Bone Joint Surg Am 78:62–72
Faris PM, Spence RK, Larholt KM, Sampson AR, Frei D (1999) The predictive power of baseline hemoglobin for transfusion risk in surgery patients. Orthopedics 22:s135–s140
Feeley TW, Rinsky LA (1993) Use of aprotinin to reduce intraoperative bleeding. West J Med 159:189–192
Fievez E, Schultze-Balin C, Herbaux B, Dalmas S, Scherpereel P (1995) [A study of blood loss during surgery for scoliosis. Posterior approach in 319 adolescents]. Cah Anesthesiol 43:425–433
Florentino-Pineda I, Blakemore LC, Thompson GH, Poe-Kochert C, Adler P, Tripi P (2001) The Effect of epsilon-aminocaproic acid on perioperative blood loss in patients with idiopathic scoliosis undergoing posterior spinal fusion: a preliminary prospective study. Spine 26:1147–1151
Gaudiche O, Loose JP, Egu JF, Dubousset J, Saint-Maurice C (1988) [Autotransfusion using Cell Saver III. Experience with 90 cases of surgery of the spine in childhood and adolescence]. Cah Anesthesiol 36:451–457
Goldberg MA (1995) Erythropoiesis, erythropoietin, and iron metabolism in elective surgery: preoperative strategies for avoiding allogeneic blood exposure. Am J Surg 170:37S–43S
Goldberg MA (1997) Perioperative epoetin alfa increases red blood cell mass and reduces exposure to transfusions: results of randomized clinical trials. Semin Hematol 34:41–47
Goldberg MA, McCutchen JW, Jove M, Di Cesare P, Friedman RJ, Poss R, Guilfoyle M, Frei D, Young D (1996) A safety and efficacy comparison study of two dosing regimens of epoetin alfa in patients undergoing major orthopedic surgery. Am J Orthop 25:544–552
Goodnough LT (1990) Erythropoietin as a pharmacologic alternative to blood transfusion in the surgical patient. Transfus Med Rev 4:288–296
Goodnough LT (1993) The role of recombinant growth factors in transfusion medicine. Br J Anaesth 70:80–86
Goodnough LT (1994) The implications of cost-effectiveness for autologous blood procurement. Arch Pathol Lab Med 118:333–334
Goodnough LT (1994) The safety of recombinant human erythropoietin therapy in autologous blood donors. J Lab Clin Med 124:17–18
Goodnough LT (1996) Current red blood cell transfusion practices. AACN Clin Issues 7:212–220
Goodnough LT, Brecher ME (1998) Autologous blood transfusion. Intern Med 37:238–245
Goodnough LT, Brittenham GM (1990) Limitations of the erythropoietic response to serial phlebotomy: implications for autologous blood donor programs. J Lab Clin Med 115:28–35
Goodnough LT, Marcus RE (1992) Effect of autologous blood donation in patients undergoing elective spine surgery. Spine 17:172–175
Goodnough LT, Shuck JM (1990) Risks, options, and informed consent for blood transfusion in elective surgery. Am J Surg 159:602–609
Goodnough LT, Rudnick S, Price TH, Ballas SK, Collins ML, Crowley JP, Kosmin M, Kruskall MS, Lenes BA, Menitove JE, (1989) Increased preoperative collection of autologous blood with recombinant human erythropoietin therapy. N Engl J Med 321:1163–1168
Goodnough LT, Wasman J, Corlucci K, Chernosky A (1989) Limitations to donating adequate autologous blood prior to elective orthopedic surgery. Arch Surg 124:494–496
Goodnough LT, Price TH, Rudnick S, Soegiarso RW (1992) Preoperative red cell production in patients undergoing aggressive autologous blood phlebotomy with and without erythropoietin therapy. Transfusion 32:441–445
Goodnough LT, Price TH, Friedman KD, Johnston M, Ciavarella D, Khan N, Sacher R, Vogler WR, Wissel M, Abels RI (1994) A phase III trial of recombinant human erythropoietin therapy in nonanemic orthopedic patients subjected to aggressive removal of blood for autologous use: dose, response, toxicity, and efficacy. Transfusion 34:66–71
Goodnough LT, Strasburg D, Riddell J, Verbrugge D, Wish J (1994) Has recombinant human erythropoietin therapy minimized red-cell transfusions in hemodialysis patients? Clin Nephrol 41:303–307
Goodnough LT, Verbrugge D, Marcus RE, Goldberg V (1994) The effect of patient size and dose of recombinant human erythropoietin therapy on red blood cell volume expansion in autologous blood donors for elective orthopedic operation. J Am Coll Surg 179:171–176
Goodnough LT, Vizmeg K, Verbrugge D (1994) The impact of autologous blood ordering and blood procurement practices on allogeneic blood exposure in elective orthopedic surgery patients. Am J Clin Pathol 101:354–357
Goodnough LT, Monk TG, Andriole GL (1997) Erythropoietin therapy. N Engl J Med 336:933–938
Hansen E, Pollwein B, Martin E, Heim MU, Horst S, Matzen KA, Peter K (1987) [Autologous transfusion in scoliosis operations: preoperative autologous blood donations and intraoperative mechanical autotransfusion]. Z Orthop Ihre Grenzgeb 125:262–267
Keating EM, Meding JB (2002) Perioperative blood management practices in elective orthopaedic surgery. J Am Acad Orthop Surg 10:393–400
Keating M, Faris P, Ritter M (1998) Erythropoietin use. Orthopedics 21:13–14
Kosmadakis N, Messaris E, Maris A, Katsaragakis S, Leandros E, Konstadoulakis MM, Androulakis G (2003) Perioperative erythropoietin administration in patients with gastrointestinal tract cancer: prospective randomized double-blind study. Ann Surg 237:417–421
Laupacis A (1996) Effectiveness of perioperative epoetin alfa in patients scheduled for elective hip surgery. Semin Hematol 33:51–53
Lee JH, Lee SH, Oh JH (2003) Minimal effective dosage of recombinant human erythropoietin in spinal surgery. Clin Orthop 71–76
Levine EA, Gould SA, Rosen AL, Sehgal LR, Egrie JC, Sehgal HL, Levine HD, Moss GS (1989) Perioperative recombinant human erythropoietin. Surgery 106:432–437
Lisander B, Jonsson R, Nordwall A (1996) Combination of blood-saving methods decreases homologous blood requirements in scoliosis surgery. Anaesth Intensive Care 24:555–558
MacEwen GD, Bennett E, Guille JT (1990) Autologous blood transfusions in children and young adults with low body weight undergoing spinal surgery. J Pediatr Orthop 10:750–753
McCall RE, Bilderback KK (1997) Use of intravenous Premarin to decrease postoperative blood loss after pediatric scoliosis surgery. Spine 22:1394–1397
McNeill TW, DeWald RL, Kuo KN, Bennett EJ, Salem MR (1974) Controlled hypotensive anesthesia in scoliosis surgery. J Bone Joint Surg Am 56:1167–1172
Mercuriali F, Inghilleri G (1998) [Blood transfusion in oncologic surgery: the role of recombinant human erythropoietin (rHuEPO)]. Tumori 84:S3–14
Mercuriali F, Zanella A, Barosi G, Inghilleri G, Biffi E, Vinci A, Colotti MT (1993) Use of erythropoietin to increase the volume of autologous blood donated by orthopedic patients. Transfusion 33:55–60
Mercuriali F, Inghilleri G, Biffi E, Colotti MT, Vinci A, Scalamogna R, Zanella A (1994) Erythropoietin treatment to increase autologous blood donation in patients with low basal hematocrit undergoing elective orthopedic surgery. Clin Investig 72:S16–S18
Mercuriali F, Inghilleri G, Biffi E (2000) New approach to preoperative autologous blood donation (PABD). Int J Artif Organs 23:221–231
Murray DJ, Forbes RB, Titone MB, Weinstein SL (1997) Transfusion management in pediatric and adolescent scoliosis surgery. Efficacy of autologous blood. Spine 22:2735–2740
Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM (2001) A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg 93:82–87
Nuttall GA, Horlocker TT, Santrach PJ, Oliver WCJ, Dekutoski MB, Bryant S (2000) Predictors of blood transfusions in spinal instrumentation and fusion surgery. Spine 25:596–601
Olsfanger D, Jedeikin R, Metser U, Nusbacher J, Gepstein R (1993) Acute normovolaemic haemodilution and idiopathic scoliosis surgery: effects on homologous blood requirements. Anaesth Intensive Care 21:429–431
Phillips WA, Hensinger RN (1988) Control of blood loss during scoliosis surgery. Clin Orthop 88–93
Price TH, Goodnough LT, Vogler WR, Sacher RA, Hellman RM, Johnston MF, Bolgiano DC, Abels RI (1996) Improving the efficacy of preoperative autologous blood donation in patients with low hematocrit: a randomized, double-blind, controlled trial of recombinant human erythropoietin. Am J Med 101:22S–27S
Price TH, Goodnough LT, Vogler WR, Sacher RA, Hellman RM, Johnston MF, Bolgiano DC, Abels RI (1996) The effect of recombinant human erythropoietin on the efficacy of autologous blood donation in patients with low hematocrits: a multicenter, randomized, double-blind, controlled trial. Transfusion 36:29–36
Quirt I, Robeson C, Lau CY, Kovacs M, Burdette-Radoux S, Dolan S, Tang SC, McKenzie M, Couture F (2001) Epoetin alfa therapy increases hemoglobin levels and improves quality of life in patients with cancer-related anemia who are not receiving chemotherapy and patients with anemia who are receiving chemotherapy. J Clin Oncol 19:4126–4134
Rosencher N, Conseiller C (2001) [Autologous blood transfusion]. Rev Prat 51:1328–1331
Rosencher N, Ozier Y (2003) [Peri-operative use of EPO]. Transfus Clin Biol 10:159–164
Rosencher N, Woimant G, Ozier Y, Conseiller C (1999) [Preoperative strategy for homologous blood salvage and peri-operative erythropoietin]. Transfus Clin Biol 6:370–379
Rosencher N, Kerkkamp HE, Macheras G, Munuera LM, Menichella G, Barton DM, Cremers S, Abraham IL (2003) Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion 43:459–469
Roye DP Jr (1999) Recombinant human erythropoietin and blood management in pediatric spine surgery. Orthopedics 22:s158–s160
Roye DP Jr, Rothstein P, Rickert JB, Verdisco L, Farcy JP (1992) The use of preoperative erythropoietin in scoliosis surgery. Spine 17:S204–S205
Sculco TP (1995) Blood management in orthopedic surgery. Am J Surg 170:60S–63S
Shapiro GS, Boachie-Adjei O, Dhawlikar SH, Maier LS (2002) The use of epoetin alfa in complex spine deformity surgery. Spine 27:2067–2071
Siller TA, Dickson JH, Erwin WD (1996) Efficacy and cost considerations of intraoperative autologous transfusion in spinal fusion for idiopathic scoliosis with predeposited blood. Spine 21:848–852
Stehling L, Luban NL, Anderson KC, Sayers MH, Long A, Attar S, Leitman SF, Gould SA, Kruskall MS, Goodnough LT (1994) Guidelines for blood utilization review. Transfusion 34:438–448
Stowell CP, Chandler H, Jove M, Guilfoyle M, Wacholtz MC (1999) An open-label, randomized study to compare the safety and efficacy of perioperative epoetin alfa with preoperative autologous blood donation in total joint arthroplasty. Orthopedics 22:s105–s112
Sum DC, Chung PC, Chen WC (1996) Deliberate hypotensive anesthesia with labetalol in reconstructive surgery for scoliosis. Acta Anaesthesiol Sin 34:203–207
Thomas MJ, Gillon J, Desmond MJ (1996) Consensus conference on autologous transfusion. Preoperative autologous donation. Transfusion 36:633–639
Urban MK, Beckman J, Gordon M, Urquhart B, Boachie-Adjei O (2001) The efficacy of antifibrinolytics in the reduction of blood loss during complex adult reconstructive spine surgery. Spine 26:1152–1156
Vitale MG, Stazzone EJ, Geljins AC, Moskowitz AJ, Roye DP Jr (1998) The effectiveness of preoperative erythropoietin in averting allogenic blood transfusion among children undergoing scoliosis surgery. J Pediatr Orthop B :166–172
Vitale MG, Levy DE, Park MC, Choi H, Choe JC, Roye DP, Jr. (2002) Quantifying risk of transfusion in children undergoing spine surgery. Spine J 2:166–172
Viviani GR, Sadler JT, Ingham GK (1978) Autotransfusions in scoliosis surgery. Review of 20 Harrington fusions. Clin Orthop 74–78
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Colomina, M.J., Bagó, J., Pellisé, F. et al. Preoperative erythropoietin in spine surgery. Eur Spine J 13 (Suppl 1), S40–S49 (2004). https://doi.org/10.1007/s00586-004-0754-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-004-0754-9