Abstract
Spinal surgery in adults can vary from simple to complex and can also have variable anticipated surgical blood loss. There are several factors that can put patients at increased risk for greater intraoperative blood loss. These factors, including a review of the literature, will be discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
With an increasing number of spinal operations—more and more complex—being performed, there is mounting awareness of the effects of blood loss on the patients’ outcomes. From the most simplistic standpoint, greater blood loss means greater transfusion needs, exposure to more blood products and the potential for disease transmission or transfusion reactions. Significant blood loss also results in greater fluid shifts, which can affect cardiac, pulmonary and renal status, or even, in the extreme example, lead to transfusion-related acute lung injury (TRALI) [25]. Increasing data suggests that blood products may impair the immune system and, therefore, increase the infection rate after surgery [5, 19, 28]. A significant blood loss can lead to coagulopathy or even disseminated intravascular coagulation (DIC), which may lead to postoperative hematoma and potential neurologic compromise or increase the risk of infection.
There are a number of reasons, certainly known to most spine surgeons, that can cause surgical blood loss that can be considerable even in routine cases. The exposure of the spine, with stripping of muscle off bone, leaves exposed surfaces of muscle and bone that can bleed, unless they are coagulated. While young patients usually have thick periosteum and have less bleeding during exposure, older patients can have thin periosteum, and osteoporotic bone with wider vascular channels. Patients with neuromuscular scoliosis—children, and adults with their osteoporotic bone—also have increased blood loss. When a patient needs decompression, laminectomy can result in epidural bleeding.
Adult patients have stiffer spines than children and adolescents, and they can have arthritic facet joints that may require osteotomy. These osteotomies will increase the bleeding from exposed bone. Adults are more likely to need more vertebral segments fused, especially in deformity surgery, since their compensatory curves may have become structural and may require inclusion to maintain truncal balance. Adult spine patients also have a higher rate of revision surgery, which has a greater risk of increased bleeding [31].
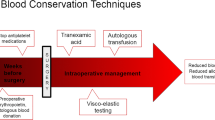
Intraoperative management from the anesthesiologist’s standpoint can be challenging. While controlled hypotension can be used in many pediatric cases, adults with medical comorbidities such as hypertension, cardiac or carotid disease often cannot tolerate decreased perfusion to critical organs. Some patients have taken analgesics such as non-steroidal antiinflammatories, which can decrease platelet function if not discontinued a week or two prior to surgery. Herbal or naturalistic supplements, notably ginseng, ginkgo, and vitamin E among others, can also increase bleeding. Oftentimes, patients do not think to tell their physicians about their non-prescription medications.
In general, most spine surgeons have found a low likelihood of needing transfusions for patients undergoing laminectomy alone [6], with patients who auto-donate blood prior to laminectomy not using their donated blood in 80% of cases. By comparison, patients who had fusions who pre-donated decreased their risk of receiving allogeneic blood by 75% for non-instrumented fusions, and 50% for instrumented fusions. The estimated blood loss (EBL) for these two groups was 674 ml (+/-443 ml) and 1,257 ml (+/-793 ml), respectively. Surgeons fused up to three levels in this patient population, although most of their patients only had one level fused.
Surgical blood loss for lumbar fusion surgery can vary, averaging over 800 ml (range 100–3,100 ml) for non-instrumented fusions to 1,517 ml (range 360–7,000 ml) for instrumented fusions in one study [18]. Other studies have shown comparable findings [2, 4, 7]. Hur et al. [13] looked at a wide range of spinal fusion surgeries and found the average total blood loss to be 1,122 ml, but had one patient whose total blood loss was 3,000 ml for a two-stage surgery.
With increasing numbers of adult deformity surgery being performed, and with greater numbers of levels of fusion required, reports of blood loss in the literature have ranged from less than 1 liter to 3 liters [1, 3, 12, 24, 27, 30] for posterior procedures, with similar results with anterior instrumented procedures [16, 23], but greater blood loss when osteotomies through prior fusions are performed, ranging from 325 to 4,700 ml [8, 14, 17].
Autologous blood donation has become increasingly common for elective spine surgery patients and can lead to a decrease in the likelihood of homologous blood exposure [10]. Use of erythropoietin in patients auto-donating for elective orthopedic surgery, in conjunction with iron sulfate supplements, can increase the number of autologous units the patients are able to donate [11]. This study had one patient who was randomized to receive erythropoietin and who developed a peripheral arterial thrombosis. The safety of use of erythropoietin in elective spine patients, particularly if they are to undergo anterior spinal surgery that incurs a higher risk of thromboembolic disease, is not yet established.
Intraoperative blood salvage is another method of decreasing use of homologous blood transfusion during surgery. Simpson et al. [26] found that, for their pediatric and young adult population who also donated autologous blood prior to surgery, this method was efficacious only if the estimated blood loss was greater than 2,000 cc. This group only represented about 10% of their patient population. They did not analyze their patients for risk factors for this greater blood loss.
Nuttall et al. [21] reviewed their experience in adult patients, including an average of over four levels fused (SD+/-4) and found several factors that resulted in a greater risk of allogeneic blood transfusion, including low preoperative hemoglobin, tumor surgery, increased number of posterior levels fused, history of pulmonary disease, and decreased amount of autologous blood available. In an accompanying article [22], they applied a “surgical blood order equation” to help the surgical team decide how much blood to order preoperatively. This was an attempt to decrease an excessive setting aside of blood for an individual patient’s surgery. They found that the most important preoperative variables were preoperative hemoglobin and whether the patient had had a surgical diagnosis of a tumor.
Zheng et al. [31] looked at revision lumbar spinal fusions and found that intraoperative blood loss rose statistically in proportion to increasing fusion levels, preoperative hemoglobin, and body weight. They also found male gender, higher body mass index and the presence of degenerative scoliosis to correlate with greater blood loss. Johnson et al. found that instrumentation, multilevel fusion, and combined approaches increased the intraoperative blood loss for lumbar fusions [15].
Looking at complex adult reconstructive surgery that requires sequential anterior and posterior spinal fusion, Urban et al. [29] found an average intraoperative EBL of 3,556 ml, although he did not give ranges. The average number of levels fused in this study was seven anteriorly and 13 posteriorly. This prospective, randomized study specifically looked at efficacy of the antifibrinolytics Amicar (epsilon-aminocaproic acid [EACA], Lederle, Philadelphia) versus aprotinin (Transylol, Bayer, West Haven, CT, USA) on perioperative blood loss. Although both study groups had less perioperative blood loss than the control group, only in patients receiving aprotinin did this reach statistical significance. Duration of surgery was also correlated with blood loss. Murray, in an accompanying point of view, noted that this decrease was only 20% overall, and the cost of Aprotinin for an 8-h infusion would be $1,000. In addition, aprotinin has been associated with sensitization and anaphylaxis after exposure [9].
The issues of exposure to allogeneic blood products are certainly a reason to strive to decrease perioperative blood loss. However, there are other consequences of greater surgical blood loss that raise the impact of decreasing EBL. Nahtoma-Shick et al. [20] demonstrated that higher EBL, increased crystalloid administration and total blood administration were all factors that led to increased crystalloid infusion and increased length of stay in the ICU in their patient populations. Additional predictors were age, ASA physical status, surgical procedure (decompression alone, decompression and fusion, complex procedures, and combined anterior/posterior procedures), and total intraoperative crystalloid/platelet administration. Their EBL for patients who stayed in the ICU more than 1 day was 2,702+/-1,771 ml compared with 612+/-480 ml for those who did not require ICU stay.
In summary, spinal fusion surgery can result in significant intraoperative blood loss, with some risk factors predicable and others not. With increasing magnitude and complexity of spinal surgery, surgeons and anesthesiologists should anticipate greater potential blood loss. Although the risks of disease transmission with transfusion have decreased with better testing, greater exposure to homologous blood may increase the length of ICU care. The risk of increased infection, immune system compromise or of transfusion-related acute lung injury may be relatively small, but should be considered important in these patients.
References
Allen BL, Ferguson RL (1988) The Galveston experience with L-rod instrumentation for adolescent idiopathic scoliosis. Clin Orthop 229:59–69
Ani N, Keppler L, Biscup RS, Steffee AD (1991) Reduction of high-grade slips with VSP instrumentation. Spine 16(6S): S203–310
Boachie-Adjei O, Bradford DS (1991) The Cotrel-Dubousset system—results in spinal reconstruction. Early experience in 47 patients. Spine 16:1155–1160
Boachie-Adjei O, Do T, Rawlins BA (2002) Partial lumbosacral kyphosis reduction, decompression and posterior lumbosacral transfixation in high-grade isthmic spondylolisthesis. Spine 27:E161–E168
Carson JL, Altman DG, Duff A et al (1999) Risk of bacterial infection associated with allogenic blood transfusion among patients undergoing hip fracture repair. Transfusion 39:694–700
Cha CW, Deible C, Muzzonigro T et al (2002) Allogeneic transfusion requirements after autologous donations in posterior lumbar surgeries. Spine 27:99–104
Chang KW, McAfee PC (1989) Degenerative spondylolisthesis and degenerative scoliosis treated with a combination segmental rod-plate and transpedicular screw instrumentation system. J Spinal Disord 1:247–256
Danisa OA, Turner D, Richardson WJ (2000) Surgical correction of lumbar kyphotic deformity: posterior reduction “eggshell’ osteotomy. J Neurosurg [Suppl 1] 92:50–56
Dietrich W, Spath P, Zuhlsdorf M et al (2001) Anaphylactic reactions to aprotinin reexposure in cardiac surgery. Anesthesiology 95:64–71
Goodnough LT, Marcus RE (1992) Effect of autologous blood donation in patients undergoing elective spine surgery. Spine 17:172–175
Goodnough LT, Rudnick S, Price TH et al (1989) Increased preoperative collection of autologous blood with recombinant human erythropoietin therapy. N Engl J Med 321:1163–1168
Gurr KR, McAfee PC (1988) Cotrel-Dubousset instrumentation in adults: a preliminary report. Spine 13:510–519
Hur SR, Huizenga BA, Major M (1992) Acute normovolemic hemodilution combined with hypotensive anesthesia and other techniques to avoid homologous transfusion in spinal fusion surgery. Spine 17: 867–870
Islam NC, Wood KB, Transfeldt EE et al (2001) Extensions of fusions to the pelvis in idiopathic scoliosis. Spine 26:166–173
Johnson RG, Murphy M, Miller M (1989) Fusions and transfusions: an analysis of blood loss and autologous replacement during lumbar fusions. Spine 14:358–362
Kaneda K, Fujiya N, Satoh S (1986) Results with Zielke instrumentation for idiopathic thoracolumbar and lumbar scoliosis. Clin Orthop 205:195–203
Lagrone MO, Bradford DS, Moe JH et al (1988) Treatment of symptomatic flatback after spinal fusion. J Bone Joint Surg Am 70: 569–580
Möller H, Hedlund R (2000) Instrumented and noninstrumented posterolateral fusion in adult spondylolisthesis. Spine 25:1716–1721
Murphy P, Heal JM, Blumberg N et al (1991) Infection or suspected infection after hip replacement surgery with autologous or homologous blood transfusions. Transfusion 31:212–217
Nahtomi-Shick O, Kostuik JP, Winters BD et al (2001) Does intraoperative fluid management in spine surgery predict intensive care unit length of stay? J Clin Anesth 13:208–212
Nuttall GA, Horlocker TT, Santrach PJ et al (2000) Predictors of blood transfusion in spinal instrumentation and surgery. Spine 25:596–601
Nuttall GA, Horlocker TT, Santrach PJ et al (2000) Use of the surgical blood order equation in spinal instrumentation and fusion surgery. Spine 25:602–605
Ogiela DM, Chan DP (1986) Ventral derotation spondylodesis. Spine 11:18–22
Ponder RC, Dickson JH, Harrington PR, Erwin ED (1975) Results of Harrington instrumentation and fusion in the adult idiopathic scoliosis patient. J Bone Joint Surg Am 57: 797–801
Popovsky M, Davenport RD (2001) Transfusion-related acute lung injury: femme fatale? Transfusion 41:312–315
Simpson MB, Georgopolous G, Eilert RE (1993) Intraoperative blood salvage in children and young adults undergoing spinal surgery with predeposited autologous blood: efficacy and cost effectiveness. J Pediatr Orthop 13:777–780
Swank S, Lonstein JE, Moe JH et al (1981) Surgical treatment of adult scoliosis. J Bone Joint Surg Am 63: 268–287
Triulzi DJ, Vanek K, Ryan DH et al (1992) A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion 32:517–524
Urban MD, Beckman J, Gordon M, Urquart B, Boachie-Adjei O (2001) The efficacy of antifibrinolytics in the reduction of blood loss during complex adult reconstructive spine surgery. Spine 26:1152–1157
Winter RB, Lonstein JE (1989) Adult idiopathic scoliosis treated with Luque or Harrington rods and sublaminar wiring. J Bone Joint Surg Am 71: 1308–1313
Zheng F, Cammisa FP, Sandhu HS et al (2002) Factors predicting hospital stay, operative time, blood loss and transfusion in patients undergoing revision posterior lumbar spine decompression, fusion and segmental instrumentation. Spine 27:818–824
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hu, S.S. Blood loss in adult spinal surgery. Eur Spine J 13 (Suppl 1), S3–S5 (2004). https://doi.org/10.1007/s00586-004-0753-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-004-0753-x