Abstract
The aim of this study was to assess the diagnostic value of combining single photon emission computerised tomography (SPECT) with reverse gantry computerised tomography (rg-CT) in the investigation of spondylolysis. Patient characteristics and imaging results in 118 patients, aged 8–44 years, with low back pain (LBP) were analysed. SPECT showed increased scintigraphic uptake in 80 patients, and spondylolysis was identified on rg-CT in 53. The Cohen Kappa ratio of 0.362 (95% CI: 0.198–0.526) suggests only fair agreement for the result of increased scintigraphic activity with the finding of spondylolysis on rg-CT. We conclude that these investigations give mutually exclusive information, which leads to four diagnostic categories. When there was increased scintigraphic activity on SPECT, 58.8% (95% CI: 48.0–69.5%) of patients had spondylolysis on rg-CT. With rest from provoking activities, these lesions may heal. We interpret the findings of increased scintigraphic activity, but no spondylolysis demonstrated on rg-CT as indicating a bone stress response. These also require rest from provoking activity to prevent a stress fracture developing. In this study, 84.2% (95% CI: 72.67–95.8%) of those patients without increased activity on SPECT had no spondylolysis identified on rg-CT. These patients may need further investigations such as magnetic resonance imaging (MRI) to diagnose pathology, which typically does not involve the posterior elements—but rest from sport may not be so important. There were five patients in our study, without increased scintigraphic activity, but in whom bilateral chronic-appearing (wide separation, smooth sclerotic bone margins) spondylolyses were identified at L5. These all were anticipated from previous plain radiographs or MRI. This group will almost certainly not heal, and if the spondylolyses are the cause of pain these vertebrae will need stabilisation by surgery if physiotherapy fails.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pathology in the pars interarticulares is common in young athletes presenting with low back pain (LBP). The pars interarticularis is that portion of the neural arch which lies at the junction of the pedicle, articular facets and lamina. Spondylolysis is defined as a separation in the neural arch and usually occurs in the pars interarticularis. The separation was described as dysplastic by Wiltse [35], but is now generally thought to be due to a stress fracture [36]. These stress fractures may be complete or incomplete. Healing of such pars defects has been documented with conservative management such as rest from provocative activities, bracing and exercise programmes [24, 26, 33, 36]. If the lesion fails to heal, the spondylolysis may remain painful and surgery may be indicated [7, 8]. High-standard athletes need to return to training as soon as possible to minimise deterioration in performance. The attending physician requires good evidence to justify recommending a period of relative rest longer than the pain alone would dictate.
This study aims to assess the diagnostic value of information provided by a combination of single photon emission computerised tomography (SPECT) and reverse gantry computerised tomography (rg-CT) in the investigation of young people with LBP, and particularly aims to consider the hypothesis that it is unnecessary to follow a normal SPECT with a rg-CT. Each investigation has financial implications and subjects patients to radiation risks. It is therefore important to demonstrate the added value of using two investigations to diagnose these problems. Furthermore, an exploration of the characteristics of groups of patients with the various possible combinations of results from SPECT and computerised tomography (CT) can provide insight into the evolution of spondylolysis.
Methods
Patients presenting to the Sports Medicine Centre or Spinal Unit of Queens Medical Centre (QMC), Nottingham, UK between 1 January 1995 and 31 December 2000 with LBP related to activity and pain exacerbated by lumbar extension were investigated by planar bone scintigraphy and SPECT. Planar bone scintigraphy and SPECT imaging was performed after the injection of 600 MBq technetium-99m methylene diphosphonate (MDTP) intravenously. Sixty-four images of the lumbar region were acquired with a dual-headed gamma camera using a low-energy ultra-high resolution collimator over a 360° circular orbit. The images were reconstructed by filtered back projection with pre-filtering. The images were viewed interactively in axial, sagittal and coronal planes on-screen by a senior radiologist (author RWK) and selected images were hard-copied. Scintigraphic activity was graded subjectively as being normal or increased with respect to the activity in adjacent vertebral bodies and posterior elements. Where abnormal, the level, side and specific location were determined.
Following this, CT scans were obtained with a reverse gantry angle (aligned from a lateral scout view to lie between the superior and inferior articular processes of the relevant level, with a maximum angulation of 25°) through all posterior elements with increased scintigraphic activity found on SPECT and occasionally through L5 or L4 despite negative SPECT. The sections were of 2 mm thickness, obtained at 2 mm intervals (3 mm sections were obtained in a small number of earlier cases), and multiplanar reformats were produced in most cases. An experienced musculoskeletal radiologist (author RWK) reviewed hard and soft copy images. The integrity or non-integrity of the pars interarticularis and other posterior element structures were reported, as well as abnormalities of size, sclerosis, and the size and margins of any osseous defect. The scintigraphic findings were available when the CT scans were reported.
We investigated 213 patients for LBP with SPECT and rg-CT in this period; however, those having a greater interval than 30 days between SPECT and rg-CT were excluded from this retrospective analysis. All patients were suffering from LBP at the time of investigation. The findings from these scans might have resulted from different stages in the evolution of spondylolysis. Thus, an analysis of the results of 118 patients is presented. Results were stored in Microsoft Access (Redland, WA, USA).
The characteristics of the following groups of patients are discussed: (1) Group A: scintigraphic activity was increased in posterior elements of the lumbar spine and spondylolysis was observed on rg-CT; (2) Group B: scintigraphic activity was increased in posterior elements of the lumbar spine, but no spondylolysis was observed on rg-CT; (3) Group C: scintigraphic activity was not increased in posterior elements of the lumbar spine, but spondylolysis was observed on rg-CT; (4) Group D: scintigraphic activity was not increased in posterior elements of the lumbar spine, and no spondylolysis was observed on rg-CT.
The characteristics considered were gender, age at onset of pain, and interval between onset of pain and date of investigations. Other investigations performed and subsequent diagnosis and management are also detailed. The degree of concordance of SPECT and rg-CT in sorting these patients into diagnostic groups is measured as Cohen’s Kappa ratio. Confidence intervals for sensitivity and specificity were calculated using the Wilson method using the Confidence Interval Analysis (CIA) Microcomputer Program Manual [13].
Results
The median age of the patients when LBP started was 17.6 (range 8.0–44.0) years. There were 85 male and 33 female patients. Sport was recorded as the activity provoking LBP in 104 of these patients—with most being cricketers (29), followed by 21 soccer players, 7 gymnasts, 7 field hockey players and 6 rugby football players. The median interval between the onset of LBP and the SPECT scan was 376.0 days (range 25–6,531 days). The CT scan was performed 3.0 (median) days after the SPECT scan (range: 18 days before to 30 days after). There were areas of increased scintigraphic activity on SPECT scans in 80 of these patients (67.8%) and spondylolysis was identified on rg-CT in 53 (44.9%). These results are summarised in Table 1.
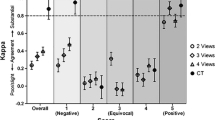
The degree of concordance between the result of increased scintigraphic activity on SPECT and the finding of a spondylolysis on rg-CT is indicated by Cohen’s Kappa ratio of 0.362 (95% CI: 0.198–0.526). This indicates a fair strength of agreement [19]. In this study, increased scintigraphic activity was found in 88.7% (95% CI: 80.1–97.2%) of patients who had a spondylolysis identified on rg-CT. Though SPECT had high sensitivity in this situation, its specificity was not so high. A negative SPECT scan occurred in only 49.2% (95% CI: 37.1–61.4%) of those patients who did not have spondylolysis identified on rg-CT. Increased scintigraphic uptake was associated with a finding of spondylolysis on rg-CT in 58.8% (95% CI: 48.0–69.5%), whilst a negative SPECT scan was associated with the rg-CT finding of no fracture in 84.2% (95% CI: 72.67–95.8%).
Characteristics of Group A
There were 47 patients in whom SPECT showed increased scintigraphic activity and spondylolysis was diagnosed on rg-CT. The most commonly reported sporting involvement in these patients was cricket in 20, soccer in 14, gymnastics in 2, rugby in 2, and racquet sports in 2; but 2 were involved in a combination of sports. Involvement in sport was not recorded in 2 of the patients, and one patient stated that they were not involved in any sport. The characteristics of this group are detailed in Table 2. Significantly more patients were male (40) than female (7) (χ2; p <0.001).
This group included 18 patients with incomplete fractures, of which three had incomplete fractures at two lumbar levels. All but one incomplete fracture was associated with increased scintigraphic uptake in the region of the affected pars. Nineteen patients had bilateral spondylolysis and these lesions were all complete. The 5th lumbar level was the level of 16 bilateral lesions. One patient with bilateral L5 spondylolyses also had bilateral complete lesions at L4. Two patients had bilateral lesions at L4 and L3, whilst one had bilateral spondylolyses at L4 only.
In those with bilateral spondylolyses, at least one of the affected pars interarticulares was associated with increased scintigraphic activity. There were 8 patients with single unilateral complete spondylolyses, and the pars interarticularis involved had increased scintigraphic activity in all but one, in which the increased activity was in the contralateral pars. This pars looked sclerotic on rg-CT. One cricketer had unilateral lesions at L2, L3 and L4 all on the left. There were two lesions seen outside the pars: one was a fracture of the tip of the superior articular process of L3 and the other was a fracture extending from one pedicle to the contralateral articular process.
Characteristics of Group B
The characteristics of the 33 patients with increased scintigraphic activity, but no spondylolysis identified on rg-CT are given in Table 2. Significantly more patients were male (25) than female (8) ( p =0.003; χ2). Involvement in sports was recorded in all but three of this group. The most common sport was cricket with 5 players, then rugby with 4 players and there were 4 runners of which one competed over hurdles. There were 3 gymnasts and 3 involved in a combination of more than one sport.
Group B includes five patients with increased scintigraphic uptake localised to an area outside the lumbar pars interarticulares. One of these patients had increased uptake in the 11th thoracic vertebra, two had increased uptake around the sacroiliac joints and one had increased uptake at the lumbo-sacral junction. The fifth had midline increase in scintigraphic activity in the body of L4.
Sclerosis of the pars interarticularis was noted on rg-CT in nine of the patients in Group B. In one, the sclerosis was due to an osteoid osteoma centred on the pars. The two patients with increased scintigraphic uptake at the sacroiliac joint were noted to be sclerotic at these joints on CT. Coincidently an osteophyte on the superior articular process was identified contralateral to the site of increased scintigraphic activity of one 4th lumbar vertebrae. Rg-CT did not identify any other abnormality in the other 21 patients.
It is possible that a bone stress response indicated by increased activity on SPECT could pre-date a spondylolysis. Two patients from this group went on to have a second CT. One patient had entirely normal rg-CT scans on the first and the second occasion 26 months later. Sclerosis noted in the pars interarticularis on the first CT scan was also observed on second CT scans at 10 months in one patient, yet no spondylolysis had developed.
Characteristics of Group C
The characteristics of the group of six patients with spondylolysis identified on CT, but no increased scintigraphic activity found on SPECT are detailed in Table 2. There were 3 males and 3 females in this group. Five patients had bilateral lesions at L5 with smooth sclerotic bone margins and wide defects suggesting chronic lesions. Three had plain radiographs prior to CT and these had led to the suspicion of spondylolysis. Two had spondylolisthesis diagnosed on magnetic resonance imaging (MRI) prior to CT. One cricketer with a 5-year history of fast-bowling-related pain had an incomplete fracture at the junction of the pars with the pedicle of L4.
Characteristics of Group D
Although rg-CT did not reveal spondylolysis in 32 patients without increased scintigraphic activity, two were observed to have sclerotic pars suggestive of a bone stress response. Rg-CT identified one facet joint injury, one patient with facet joint arthrosis, one with a small bone fragment at the articular process and two patients with Schmorl’s nodes.
Twenty-two of these patients were investigated with MRI, and the final diagnosis for 11 was intervertebral disc degeneration. Various developmental anomalies were identified, such as a rudimentary disc at S1/2 of one patient and six lumbar vertebral segments in two patients. MRI diagnosed a haemangioma of the third lumbar vertebral body in one patient who subsequently underwent partial vertebrectomy and grafting. For one patient, clinicians made a final diagnosis of chronic pain syndrome.
No current involvement in sport was recorded for six patients of Group D. Five played hockey, 5 soccer and 3 cricket. Three were involved in equestrian sports, and these described pain commencing after falls from horses. Three patients in Group D were competing in more than one sport. There were 17 males and 15 females in Group D, and this was not statistically significant ( p =0.724; χ2).
Discussion
Traditionally, diagnosis of spondylolysis relied on plain radiography, but the pars lies oblique to all three orthogonal planes and therefore can escape detection unless angled projections are used. No consensus has been reached amongst the proponents of the various radiological techniques [1, 2, 11, 20, 21, 23, 28]. Additional oblique radiographs increase the exposure of patients to ionising radiation. Incomplete fractures almost invariably are radiologically occult and yet important to diagnose as rest from activities provoking pain may allow such lesions to heal. Plain radiographs do not form part of the usual investigative algorithm for patients with extension and activity-related LBP at our centre, and only three patients included in this study are known to have had plain radiographs before rg-CT. In these three cases, rg-CT confirmed spondylolysis first identified on plain radiographs, though SPECT had been negative.
MRI provides an alternative imaging modality without the risks of exposure to ionising radiation. MRI may be used to diagnose pars defects, though the sensitivity of MRI in the diagnosis of incomplete posterior element stress fractures is unknown. Established defects appear as a discontinuity of the cortex and marrow through the pars, best seen on T1-weighted sequences [14]. Nevertheless, these appearances are also possible with sclerosis of the neck of the pars, partial volume imaging of an osteophyte from the S1 superior facet and osteoblastic metastases of the pars [16]. MRI was found to have a sensitivity of 57–86%, specificity of 81–82%, positive predictive value of 14–18% and negative predictive value of 97–99% for the diagnosis of a pars defect in 50 patients. CT was used as the gold standard in this study [31]. Marrow oedema is sometimes seen in the pars when spondylolyses are present. This is analogous to the marrow oedema seen in stress fractures elsewhere in the body. Nevertheless, the sensitivity and specificity of MRI in this context is not known.
CT provides good images of the pars defects, but there are associated risks. A series of antero-posterior, lateral and oblique plain radiographs delivers a similar surface radiation dose as a single CT slice, but the CT scanning is more focussed and so the gonadal radiation is limited and nil in males [10]. The radiologist may scan only the most suspicious lumbar levels to further reduce radiation. Standaert concludes from a review of papers detailing the level of spondylolyses that 85–95% are at L5, 5–15% are at L4 and more proximal lesions are much less common [32]. However, if only L4 and L5 are scanned some higher lesions will be missed. Conventional CT slices are in the axial plane, which is parallel to the intervertebral disc. Congeni recommends rg-CT where the CT scanning plane is perpendicular to the usual fracture plane [10], and this technique was employed in our study.
Bone scintigraphy determines whether there is increased metabolic activity in sites of the lumbar spine. Planar bone scans cannot reliably distinguish between increased metabolic activity in the posterior neural arch and the underlying vertebral body. SPECT improves diagnostic localisation of bone by achieving separation of bony structures that overlap on standard planar images [9]. Bellah reported 71 patients with positive SPECT scans, of which no increase in activity was identified on the planar bone scan in 39 [6]. This suggests SPECT scanning may be more sensitive, but less specific than planar bone scanning.
Having noted the sites of increased scintigraphic activity, the radiologist may select specific lumbar levels to scan by CT. Ryan studied 34 patients with LBP: 27 were SPECT positive of which 18 had abnormalities on CT scan. At 43 sites (80%) of increased scintigraphic activity, an abnormality was found on CT. The investigations were performed within 3 weeks of each other. These patients were aged 18–70 years (median 44 years) [30]. We performed selective CT scanning in this study. All levels with increased scintigraphic activity were studied by rg-CT, and additionally adjacent levels were sometimes studied. Recognising that most spondylolyses described in the literature were at L5, we generally scanned this level even in the absence of increased scintigraphic activity and often scanned L4, which is the next most common level affected.
We recognise that bone scintigraphy and CT reflect different things. Bone scintigraphy reflects metabolic activity in bone, which may increase in response to physical stress. CT depicts anatomy and helps us visualise sites of pathology. Nevertheless, if the two investigations sorted the patients studied similarly into groups, there would be no advantage in doing both investigations. Cohen’s Kappa ratio of 0.362 indicates only fair agreement between the investigations. Thus we must decide whether one investigation is superior to the other and can be done alone or whether the combination offers the clinician added value. The radiologist reported the rg-CT without blinding to the result of the SPECT. This is usual clinical practice, but is a methodological weakness of our study and yet might have lead to greater concordance of results from the two investigations, if it were to influence them at all.
Congeni studied patients with LBP, negative radiographs but positive bone scans. Some were investigated with SPECT, but some with planar bone scans only. Pars fractures were found on CT scans performed within 10 weeks of the bone scan in 34 of 40 (85%) of these patients. Our study differs in including only those whose rg-CT was performed within 30 days of the SPECT. We found that 58.8% of those with increased scintigraphic activity had spondylolysis demonstrable on rg-CT (Group A). It is reasonable to infer that some of these fractures developed between 30 days and 10 weeks in sites of increased scintigraphic activity, though other design factors such as patient selection criteria may have differed, providing other explanations for the different figures.
Congeni et al. found six patients with increased scintigraphic uptake for whom no pars defect was demonstrated on CT and said to show various degrees of bone stress reaction. They conclude that nuclear medicine studies have a 15% false positive rate when CT scan is used as the standard to establish the diagnosis of spondylolysis [10]. We think it is unhelpful to use the term ‘false positive’ in this situation, as the finding of bone stress response, as indicated by increased scintigraphic activity yet no fracture found at this site on rg-CT, is important clinically.
Other studies suggest that increased bone scintigraphic activity can precede the development of radiographic [27] or surgical [34] evidence of spondylolysis. Such patients may be developing a stress fracture, which may be prevented by rest from activities which provoke LBP. This Group B comprises 41.2% of those with increased scintigraphic activity in our study. Only two of these had persistent symptoms, and these had repeat rg-CT. There was no radiological evidence of progression from a bone stress response to a spondylolysis. This probably indicates the success of our management strategy, though this strategy requires further research to corroborate this assumption. In our study, 8 of the 28 patients with increased scintigraphic activity confined to the posterior elements of the lumbar vertebrae also had the appearance of sclerosis within the affected pars interarticularis. This supports the notion that these are sites of bone stress response.
In our hands, the management of those with increased scintigraphic activity and a spondylolysis (Group A), whether complete or incomplete fracture, is similar to the bone stress response patients (Group B). We believe the increased scintigraphic activity indicates a potential for healing, which should be maximised. The patients are advised to rest from activities (usually sport) which provoke their LBP, and to engage in a programme of core stabilisation with our physiotherapists. Nevertheless, eight of Group A are known to have been surgically stabilised due to failure of this programme to resolve the patients’ back pain, which was threatening careers in sport.
In our study, the absence of increased scintigraphic activity on SPECT is associated with an 84.2% chance of not having spondylolysis identified on rg-CT. Thus it is reasonable to reassure the patient that they probably do not have a spondylolysis, without exposing them to a CT scan. We currently consider MRI as the next investigation for those with normal SPECT scans, as this can reveal pathology outside the posterior element that may cause LBP. This approach led to the diagnosis of intervertebral disc disease in 11 of the 32 patients in Group D. However, MRI was performed in only 22 of these patients. This information changes management, as there may be no need to avoid so strictly activities that have provoked pain. An example would be lumbar extension, which is used in some programmes to treat intervertebral disc prolapse.
There were six patients with spondylolysis identified in our study who had no increased activity on SPECT (Group C). Some of these may have been stress fractures that had become metabolically inactive with time [22, 34]. Indeed, this group had a relatively long history of LBP (median 376 days), though not as long as those of Group D (761.5 days). Also it should be noted that they were relatively young when LBP began (median age 14.5), compared to the median of the whole cohort (17.6 years). They have a similar incidence in males and females and there was no particular association with sports, though they often recalled a traumatic moment when pain began. This causes us to consider a different aetiology in this group. These lesions might be developmental and be the result of dysplasia [35]. Indeed, spondylolysis has been demonstrated by radiography in people without back pain. The prevalence of asymptomatic spondylolysis is approximately 4–6% in the general adult population [1, 3, 4, 5, 12, 17, 18, 25, 29, 37]. However, spondylolysis has never been recorded in newborns or infants, and this is evidence against the lesions ever being congenital. In Group C, five of six patients had lesions that were complete, had smooth sclerotic bone margins and were bilateral at L5. We assume these lesions do not have the potential to heal spontaneously, nevertheless some patients from this group have benefited from surgical stabilisation.
Among those in our study with increased scintigraphic activity, 12 had typical chronic-appearing lesions bilaterally at L5. We estimated a separation of between 2 mm and 6 mm between the smooth sclerotic bone margins. One patient had bilateral chronic-appearing lesions at L4 and L3. We also found six patients with chronic-appearing single spondylolyses all at L5. Four of these had evidence of contralateral pars bone stress response and one had increased scintigraphic activity at two higher levels (L3 and L4), though no increase at the site of spondylolysis. This raises the possibility that a chronic spondylolysis may lead to instability in the lumbar spine, which may become manifest as pain with evidence of bone stress response in another pars interarticularis and propensity to develop further spondylolyses with repeated activities of sport. Another possibility is that a chronic lesion may become painful if traumatised. Several patients of this series described trauma at the onset of pain. Of course the presence of spondylolysis may be entirely co-incidental and the pain source something else entirely.
The characteristics of Group A support the notion that spondylolyses may be the result of stress fractures. Significantly more of this group are males and the median age is 17.8 years. It is this age group and gender that we expect to be most extensively involved in sports. Within Group A, there are a high proportion of cricketers and soccer players. The latter may reflect only the popularity of playing this sport in our country, but the proportion of cricketers is higher and suggests a particular risk factor in this sport. All of these cricketers were fast bowlers and it is this activity that has previously been identified as a risk factor [15]. Alternatively, some of those in Group A may have had a chronic spondylolysis and their sporting activities may have provoked pain and a bone stress response in the lumbar posterior elements. In our study, incomplete fractures were usually associated with increased scintigraphic activity in the same pars—20 out of 22 (90.9%). This suggests that they form in response to stress in the bone and that they have potential for healing.
Conclusions
SPECT provides information about the metabolic activity of the bone of the pars in response to repeated stress of sporting activity. Rg-CT provides morphological information about the state of the pars interarticularis, and SPECT and CT together can indicate the stage reached in the evolution of a stress fracture. The data provided in this series of 118 patients investigated for spondylolysis supports the practice that SPECT should be the first line investigation for this condition.
Rg-CT best delineates the abnormal anatomy in those who have increased scintigraphic activity. This identifies those with bone stress response alone that may or may not be confirmed by abnormal sclerosis in the affected pars interarticularis, those further along the continuum who have developed an incomplete stress fracture and those who have complete fractures. These complete lesions may have chronic appearances of smooth sclerotic bone margins and may be separated by several millimetres. Such lesions are less likely to heal, and make other pars vulnerable to stress response by the instability arising in the lumbar spine.
Chronic lesions were identified in patients without increase in scintigraphic activity in this series, but had been already diagnosed by MRI or plain radiographs. We believe that it is not necessary to follow negative SPECT by rg-CT and that MRI may be better as it has the potential to diagnose pathology outside the posterior elements that may give rise to pain and may be differently managed.
References
Amato M, Totty WG, Gilula LA (1984) Spondylolysis of the lumbar spine: demonstration of defects and laminal fragmentation. Radiology 153:627–629
Appleby A, Stabler J (1969) A new sign of spondylolisthesis. Clin Radiol 20:315–319
Baker D, McHollick W (1967) Hereditary spondylolisthesis and spina bifida. J Bone Joint Surg Am 49A:507–513
Baker DR, McHollick WJ (1956) Spondylolschisis and spondylolisthesis in children. J Bone Joint Surg Am 38A:933–934
Barr JS (1955) Spondylolisthesis. J Bone Joint Surg Am 37A:878–880
Bellah RD, Summerville DA, Treves ST et al. (1991) Low-back pain in adolescent athletes: detection of stress injury to the pars interarticularis with SPECT. Radiology 180:509–512
Bradford DS, Iza J (1985) Repair of the defect in spondylolysis or minimal degrees of spondylolisthesis by segmental wire fixation and bone grafting. Spine 10:673–679
Buck JE (1970) Direct repair of defect in spondylolisthesis. J Bone Joint Surg Br 52B:432–437
Collier BD, Johnson RP, Carrera GF et al. (1985) Painful spondylolysis or spondylolisthesis studied by radiography and single-photon emission computed tomography. Radiology 154:207–211
Congeni J, McCulloch J, Swanson K (1997) Lumbar spondylolysis. A study of natural progression in athletes. Am J Sports Med 25:248–253
Dubowitz B, Friedman L, Papert B (1987) The oblique cranial tilt view for spondylolysis. J Bone Joint Surg Br 69:421
Fredrickson BE, Baker D, McHolick WJ et al. (1984) The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am 66:699–707
Gardner MJ, Gardner SB, Winter PD (1991) Confidence Interval Analysis. Version 1.1. Br Med J, London
Grenier N, Kressel HY, Schiebler ML et al. (1989) Isthmic spondylolysis of the lumbar spine: MR imaging at 1.5 T. Radiology 170:489–493
Hardcastle P, Annear P, Foster DH et al. (1992) Spinal abnormalities in young fast bowlers. J Bone Joint Surg Br 74:421–425
Johnson DW, Farnum GN, Latchaw RE et al. (1989) MR imaging of the pars interarticularis. Am J Roentgen 52:327–332
Jones DM, Tearse DS, el Khoury GY et al. (1999) Radiographic abnormalities of the lumbar spine in college football players. A comparative analysis. Am J Sports Med 27:335–338
Krenz J, Troup JD (1973) The structure of the pars interarticularis of the lower lumbar vertebrae and its relation to the etiology of spondylolysis, with a report of a healing fracture in the neural arch of a fourth lumbar vertebra. J Bone Joint Surg Br 55:735–741
Landis JR, Koch GC (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–74
Libson E, Bloom RA (1983) Anteroposterior angulated view. A new radiographic technique for the evaluation of spondylolysis. Radiology 149:315–316
Libson E, Bloom RA, Dinari G et al. (1984) Oblique lumbar spine radiographs: importance in young patients. Radiology 151:89–90
Lusins JO, Elting JJ, Cicoria AD et al. (1994) SPECT evaluation of lumbar spondylolysis and spondylolisthesis. Spine 19:608–612
Markwalder TM, Saager C, Reulen HJ (1991) “Isthmic” spondylolisthesis—an analysis of the clinical and radiological presentation in relation to intraoperative findings and surgical results in 72 consecutive cases. Acta Neurochir 110:154–159
Morita T, Ikata T, Katoh S et al. (1995) Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br 77:620–625
Nathan H (1959) Spondylolysis. J Bone Joint Surg Am 41A:303–320
O Sullivan PB, Phyty GD, Twomey LT et al. (1997) Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine 22:2959–2967
Papanicolaou N, Wilkinson RH, Emans JB et al. (1985) Bone scintigraphy and radiography in young athletes with low back pain. Am J Roentgen 145:1039–1044
Porter RW, Park W (1982) Unilateral spondylolysis. J Bone Joint Surg Br 64:344–348
Roche GG, Rowe MB (1952) The incidence of separate neural arch and coincident bone variations. J Bone Joint Surg Am 34A:491–494
Ryan PJ, Evans PA, Gibson T et al. (1992) Chronic low back pain: comparison of bone SPECT with radiography and CT. Radiology 182:849–854
Saifuddin A, Burnett SJ (1997) The value of lumbar spine MRI in the assessment of the pars interarticularis. Clin Radiol 52:666–671
Standaert CJ, Herring SA (2000) Spondylolysis: a critical review. Br J Sports Med 34:415–422
Steiner ME, Micheli LJ (1985) Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine 10:937–943
Van den Oever M, Merrick MV, Scott JH (1987) Bone scintigraphy in symptomatic spondylolysis. J Bone Joint Surg Br 69:453–456
Wiltse LL (1962) The etiology of spondylolisthesis. J Bone Joint Surg Am 44A:539–559
Wiltse LL, Widell EH, Jackson DW (1975) Fatigue fracture: the basic lesion is isthmic spondylolisthesis. J Bone Joint Surg Am 57:17–22
Yano T (1967) Familial incidence of spondylolysis. J Bone Joint Surg Br 49B:390
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gregory, P.L., Batt, M.E., Kerslake, R.W. et al. The value of combining single photon emission computerised tomography and computerised tomography in the investigation of spondylolysis. Eur Spine J 13, 503–509 (2004). https://doi.org/10.1007/s00586-004-0696-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-004-0696-2