Abstract
In this study, we investigated the effects of the memory-enhancing drugs piracetam, vincamine, and vinpocetine or the cholinesterase inhibitor donepezil on the development of oxidative stress, inflammation, and brain damage induced in rat brain by aluminum chloride (AlCl3). Saline (control), piracetam (100 or 300 mg/kg), vincamine (10 or 20 mg/kg), vinpocetine (10 or 20 mg/kg), piracetam 100 mg/kg plus vincamine 10 mg/kg, piracetam 100 mg/kg plus vinpocetine 10 mg/kg, or donepezil 5 mg/kg were administered once daily intraperitoneally for 45 days along with AlCl3 (10 mg/kg, intraperitoneally). Malondialdehyde (MDA), reduced glutathione (GSH), nitric oxide, acetylcholinesterase (AChE), butrylcholinesterase (BChE), paraoxonase (PON1) activities, and prostaglandin E2 (PGE2) concentrations were measured in brain. Histopathology and caspase-3 immunohistochemistry (an apoptotic marker) were also performed. Results indicated that (1) compared to controls, injection of AlCl3 significantly increased brain lipid peroxidation (MDA) and nitric oxide concentrations together with decreased GSH concentrations. PON1 activity in brain was significantly decreased, while AChE and BChE activities were significantly increased compared to control animals. Cortical atrophy, neuronal shrinkage, red neurons, surrounded by vacuolations with cytoplasmic neurofibrillary tangles, intense caspase-3 expression in degenerated neurons, and amyloid deposition were observed; (2) in AlCl3-treated rats, (i) lipid peroxidation was significantly decreased by the lower doses of piracetam, vincamine, and vinpocetine as well as by piracetam plus either vincamine or vinpocetine; (ii) nitric oxide was significantly decreased by the lower doses of piracetam, and vinpocetine, by both doses of vincamine, and by piracetam plus either vincamine or vinpocetine; (iii) nitric oxide also showed significant decrease after treatment with donepezil; (iv) both GSH and PON1 activity showed significant increase following the administration of the test drugs; (v) PGE2 significantly increased by the higher dose of piracetam, vincamine, vinpocetine, and piracetam plus either vincamine or vinpocetine; (vi) AChE and BChE activities decreased after treatment with the lower dose of piracetam, vinpocetine, and piracetam plus either vincamine or vinpocetine; (vii) AChE activity decreased following 20 mg/kg vincamine, and BChE activity decreased following 10 mg/kg vincamine; (viii) AChE but not BChE activity decreased after donepezil; (ix) on histopathology, the low dose of singly used drugs and donepezil had the best improvement in neuronal look, cortical thickness, and degree of vascular congestion. Rats treated with 10 mg/kg vinpocetine showed decreased capsase-3 immunoreactivity in brain and regenerating neurons. These results suggest that while the low therapeutic doses of the nootropic drugs piracetam, vincamine, and vinpocetine display anti-oxidant and neuroptotective effects, their high doses are likely to have prooxidant and proinflammatory properties.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pyrrolidine derivative piracetam, the Vinca minor alkaloid vincamine, and its synthetic derivative vinpocetine have widely been used for decades to treat memory dysfunction and cognitive impairment that occurs during normal aging, cerebrovascular disorders, or Alzheimer’s disease (Winblad 2005; Heckman et al. 2015). Piracetam (2-oxo-1-pyrrolidine-acetamide) was the first of the so-called “nootropic” drugs, a term that was introduced by Giurgea (1973) to denote this class of medications which protect memory processes against disruption by chemical or physical agents. In rodent experiments, the drug prevented memory changes caused by scopolamine (Chopin and Briley 1992) or morphine (Aksu et al. 1998). Clinically, it has been used in the treatment of aphasia following stroke (Kessler et al. 2000) and in cognitive impairment in the elderly (Waegemans et al. 2002). In stroke patients, the drug led to better recovery of cognitive impairment evaluated by event-related potentials compared to treatment with acetylsalicylic acid (Stahlhut et al. 2014). Piracetam also improved cognitive performance of patients undergoing coronary bypass surgery (Fang et al. 2014). The drug improved mitochondrial function and ATP production in models of amyloid beta (Aβ)-induced impairment of mitochondrial function (Kurz et al. 2010) or in PC12 cells subjected to oxidative stress (Keil et al. 2006). Piracetam resulted in increased cerebral blood flow in stroke (Kessler et al. 2000) and increased membrane fluidity of hippocampal membranes from Alzheimer’s disease patients and elderly controls (Eckert et al. 1999).
Vincamine, an extract of periwinkle, and its synthetic derivative vinpocetine (vinpocetine-ethyl apovincaminate) are both used in the treatment of cognitive decline due to cerebrovascular insufficiency (Fischhof et al. 1996; Hadjiev 2003). These agents increase cerebral blood flow and regional glucose uptake (Szilágyi et al. 2005; Jovanović et al. 2013). Vinpocetine is an inhibitor of cyclic GMP phosphodiesterase (Ahn et al. 1989), a potent ligand of peripheral benzodiazepine binding sites (Gulyás et al. 2005) and a blocker of NaV1.8 sodium channel activity (Zhou et al. 2003). Both vinpocetine and its main metabolite cis-apovincaminic acid (cAVA) exert neuroprotective effects (Nyakas et al. 2009; Tárnok et al. 2008). Vinpocetine in addition exerts an anti-inflammatory action inhibiting tumor necrosis factor-alpha (TNF-α)-induced nuclear factor-kappa B (NF-κB) activation, monocyte adhesion and chemotaxis, and the induction of proinflammatory mediators (Jeon et al. 2010). The drug reduces atherosclerotic lesion formation, oxidized low-density lipoprotein (LDL) uptake, and foam cell formation (Cai et al. 2013). These actions are likely to benefit patients with cerebrovascular insufficiency by preventing the progression of atherosclerosis.
There is an increasingly recognizable role for oxidative stress and neuroinflammation in the etiology of various brain disorders (Roth et al. 2005; Danielson and Andersen 2008; Sajdel-Sulkowska et al. 2008; Frank-Cannon et al. 2009; Abdel-Salam et al. 2015). Oxidative stress describes a state of ongoing oxidative damage to the cell that is caused by overwhelming reactive oxygen species or deficient protective mechanisms. Reactive oxygen metabolites are produced by the cell metabolic processes. Sources include the mitochondrial respiratory chain, the neutrophil enzymes NADPH oxidase and myeloperoxidase, and the enzyme xanthine oxidase. Within the cell, the ability of reactive oxygen metabolites to inflict damage to cell membranes, proteins, and DNA is counterbalanced by a number of molecules such as ascorbic acid, α-tocopherol, carotenes, the tripetide glutathione, and anti-oxidant enzymes, e.g., superoxide dismutases, catalases, and glutathione peroxidases (Sies 1991; Halliwell and Gutteridge 1989; McCord 2000). Under basal conditions, this balance is not so tight and a certain degree of oxidative stress is present. High levels of oxidative stress are associated with tissue damage and disease development (Halliwell 2001). Oxidative stress has been implicated in the pathogenesis of several neurodegenerative disorders, stroke, and aging and in the accompanying cognitive decline (Perry et al. 2007; Warner et al. 2004). Several factors are likely to account for the susceptibility of the brain tissue to oxidative stress. These include a high rate of oxygen utilization, rich content of polyunsaturated fatty acids, the presence of the redox-active transition metal ions Cu++ and Fe++, and decreased anti-oxidant enzymes (Halliwell 1992).
Aluminum, the most abundant metal in the Earth’s crust, has been implicated in accelerating brain aging and in the development of Alzheimer’s disease (Drago et al. 2007; Yumoto et al. 2009; Bondy 2014). The metal is widely used in building, construction, containers, packaging, electrical conductors, and many equipments. Aluminum can cross the blood–brain barrier and accumulate in the cortex, cingulate bundles, corpus callosum, hippocampus, and cerebellum (Xu et al. 1992; Struys-Ponsar et al. 1997; Yuan et al. 2012). It is found in glia, astrocytes, and neuronal cells (Golub et al. 1999; Lévesque et al. 2000). The neurotoxicity of aluminum involves enhancing lipid peroxidation (Esparza et al. 2003; Pallavi et al. 2008), altering axonal transport, and phosphorylation levels of neurofilaments (Exley 2004). Aluminum causes progressive memory deterioration, oxidative stress, hyperphosphorylated tau, and aggregation of β-amyloid, the major component of senile plaques (Walton 2007, Walton and Wang 2009). The latter are the main neuropathological features of Alzheimer’s disease (Castellani et al. 2006). The aluminum-based rodent model for Alzheimer’s disease can thus be used to study the pathogenetic mechanisms and the possible therapeutic interventions for Alzheimer’s disease (Kawahara 2005).
In the present study, the memory-enhancing drugs—piracetam, vincamine, and vinpocetine—used either singly or in combination were evaluated for their ability to reduce brain oxidative stress, inflammation, and neuronal damage evoked by systemic injection of aluminum chloride into rats. In addition, the effects of these drugs were compared to those of the acetylcholiesterase inhibitor donepezil, a commonly used drug for Alzheimer’s disease (Wilkinson et al. 2004).
Materials and methods
Animals
Adult male Sprague–Dawley rats, weighing 120–130 g (age 10–11 weeks), were used. Animals were obtained from the breeding colony maintained at the animal house of National Research Center (NRC, Cairo, Egypt). All animals were housed under conventional laboratory conditions throughout the period of experimentation at room temperature of 25 ± 2 °C, 60–70 % humidity, and 12-h light/dark cycle, fed standard laboratory pellets (20 % proteins, 5 % fats, 1 % multivitamins), and allowed free access to tap water. Animals were allowed at least 1 week of acclimatization before analyses. All animals received human care and followed the recommendations of the National Institutes of Health Guide for Care and Use of Laboratory Animals (Publication No. 85–23, revised 1985). Equal groups of seven rats each were used in all experiments.
Drugs and chemicals
Donepezil hydrochloride (Pfizer Egypt, Cairo, A.R.E.), piracetam (Pharco Pharmaceuticals, Alexandria, A.R.E.), vinpocetine (Amriya Pharmaceutical industries, Alexandria, A.R.E.), and vincamine (GlaxoSmithKline Pharmaceutical Co., Salam city, Cairo, A.R.E.) were used. Aluminum chloride (AlCl3) was obtained from Sigma (USA.) All drugs were dissolved in saline and freshly prepared immediately before use. Anti-caspase-3 antibody kit was obtained from Abcam plc. (Cambridge Science Park, Cambridge CB4 0FL, UK).
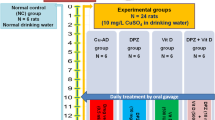
Experimental design
Rats were randomly assigned into 11 groups, with 7 rats each. Group 1 received the vehicle (saline). Group 2 received AlCl3 at the dose of 10 mg/kg. Groups 3 and 4 received AlCl3 in combination with piracetam (100 or 300 mg/kg). Groups 5 and 6 received AlCl3 in combination with vincamine (10 or 20 mg/kg). Groups 7 and 8 received AlCl3 in combination with vinpocetine (10 or 20 mg/kg). Group 9 received AlCl3 in combination with piracetam (100 mg/kg) plus vincamine (10 mg/kg). Group 10 received AlCl3 in combination with piracetam (100 mg/kg) plus vinpocetine (10 mg/kg). Group 11 received AlCl3 in combination with donepezil (5 mg/kg). Drugs were administered intraperitoneally daily for 45 days. Rats were euthanized 24 h following the last treatment by cervical dislocation under light ether anaesthesia, and the brain of each rat was rapidly excised, washed with ice-cold saline solution (0.9 % NaCl), immediately frozen on dry ice-cold glass plate, and stored at −80 °C for further determination of biochemical parameters. For biochemical studies, the brain was homogenized in ice-cold phosphate buffer to obtain 10 % homogenate. For histopathology and immunopathology studies, the brain of two to three rats, randomly selected from each group, was removed, rapidly rinsed in ice-cold saline solution, and placed in 10 % buffered formalin.
Biochemical studies
Determination of lipid peroxidation
Lipid peroxidation was assayed by measuring the level of malondialdehyde (MDA) in the brain homogenates. Malondialdehyde was determined by measuring thiobarbituric reactive species using the method of Ruiz-Larrea et al. (1994). In this assay, the thiobarbituric-acid-reactive substances react with thiobarbituric acid to produce a pink-colored complex having peak absorbance at 532 nm.
Determination of reduced glutathione
Reduced glutathione (GSH) was determined in brain tissue by Ellman’s method (1959). The procedure is based on the reduction of Ellman’s reagent by –SH groups of GSH to form 2-nitro-s-mercaptobenzoic acid; the nitromercaptobenzoic acid anion has an intense yellow color which can be determined spectrophotometrically. A mixture was directly prepared in a cuvette: 2.25 ml of 0.1 M K-phosphate buffer, pH 8.0; 0.2 ml of the sample; and 25 μl of Ellman’s reagent (10 mM 5,5′-dithio-bis-2-nitrobenzoic acid in methanol). After 1 min, the assay absorbance was measured at 412 nm and the GSH concentration was calculated by comparison with a standard curve.
Determination of butyrylcholinesterase activity
Butyrylcholinesterase activity in brain supernatant was determined by colorimetric method using butrylcholinesterase diagnostic kit (CHRONOLAB, Barcelona, Spain). The principle of the method is that cholinesterase hydrolyzes butrylcholinesterase to butyrate and thiocholine. The latter reacts with 5,5’-dithiobis-2-nitrobenzoic acid (DTNB) forming 5-mercapto-2-nitrobenzoic acid (5-MNBA). The rate of 5-MNBA formation, measured by spectrophotometer, is proportional to the enzymatic activity of cholinesterase in the sample.
Determination of acetylcholinesterase activity
The determination of cholinesterase activity in the brain was a modification of the method of Ellman et al. (1961) as described by Gorun et al. (1978). The principle of the method is the measurement of thiocholine produced when acetylcholine is hydrolyzed. The color was read immediately at 412 nm.
Determination of nitric oxide
Nitric oxide was determined in the brain homogenate according to the method described by Miranda et al. (2001).
Determination of paraoxonase activity
Arylesterase activity of paraoxonase was measured spectrophotometrically in supernatants using phenylacetate as a substrate (Higashino et al. 1972; Watson et al. 1995).
Determination of prostaglandin E2 concentration
Prostaglandin E2 concentration in rat brain supernatant was assayed by ELISA technique using prostaglandin E2 assay kit purchased from Glory Science Co., Ltd., TX, USA, according to the instructions provided. The parameter prostaglandin E2 (PGE2) immunoassay is a 3.5-h forward sequential competitive enzyme immunoassay designed to measure PGE2 in cell culture supernates.
Histopathology and immunopathology studies
For histopathological study, the brain was removed, placed in 10 % buffered formalin, dehydrated in graded alcohol, and embedded in paraffin. The paraffin blocks were serially sectioned at 5-μm thickness. Afterward, sections were mounted on glass slides and counter-stained with hematoxylin and eosin (Hx & E) for evaluation qualitatively under light microscope. Images were captured and processed using Adobe Photoshop version 8.0. For immunopathology, paraffin sections from each case were processed using caspase-3 antibodies. Caspase-3-stained sections were examined at high power for immunohistochemical expression and assessment of apoptosis and were divided into those that were negative (no immunoreactivity in any cells) and positive (membrane and/or cytoplasm immunoreactivity present).
Statistical analysis
Results are expressed as means ± SEM. Comparisons between means of different groups were carried out using one-way analysis of variance (ANOVA) test followed by Duncan multiple comparisons test. The level of significance was set at p < 0.05. SPSS software (SAS Institute Inc., Cary, NC) and Graph pad Prism software (Inc., San Diego, USA, version 5) were used to carry out all statistical tests.
Results
Oxidative stress
Compared with the saline-treated group, AlCl3 injection resulted in a significant increase in the level of MDA by 35.2 %, a decrease in the level of GSH by 72.9 %, and an increase in the level of nitric oxide by 74.21 % (Fig. 1a–c).
It was noted that treatment with the lower doses of piracetam, vincamine, or vinpocetine resulted in significant decrease in brain lipid peroxidation by 26.2 %, 33.5 %, and 23.6 %, respectively. In contrast, the higher dose of these agents failed to significantly alter brain MDA. A decrease in brain MDA was observed after treatment with 10 or 20 mg/kg vinpocetine (by 23.6 % and 18.1 %, respectively), low-dose piracetam plus vincamine (by 18.3 %), or low-dose piracetam plus vinpocetine (by 21.7 %). These figures, however, did not reach statistical significance. Meanwhile, no significant change in brain MDA was observed after treatment with donepezil (Fig. 1a).
The administration of the nootropic drugs piracetam, vincamine, vinpocetine, piracetam plus vincamine, piracetam plus vinpocetine, or donepezil 5 mg/kg almost reversed or restored the depleted brain glutathione (Fig. 1b).
Moreover, significant decrease in brain nitric oxide was observed after treatment with 100 mg/kg piracetam (by 45.8 %), 10 and 20 mg/kg vincamine (by 17.4 % and 17.2 %, respectively), 10 mg/kg vinpocetine (by 27.6 %), piracetam plus vincamine (by 16.8 %), piracetam plus vinpocetine (by 24.6 %), and donepezil (by 23.6 %). Thus, the high dose of piracetam or vinpocetine failed to significantly alter the raised brain nitric oxide in AlCl3-treatred rats (Fig. 1c).
Paraoxonase 1 activity
AlCl3 resulted in significantly decreased brain paraoxonase (PON1) activity by 54.6 %. Compared with the AlCl3 control group, a significant decrease in brain PON1 activity was observed after treatment with piracetam (by 21 % and 75 %), vincamine (by 187.6 % and 98.8 %), vinpocetine (by 42.3 and 80 %), piracetam plus vincamine (by 58.8 %), piracetam plus vinpocetine (by 75.7 %), and donepezil (by 95.2 %). Brain PON1 activity was almost restored to normal value by treatment with vincamine (Fig. 1d).
Acetylcholinesterase activity
In AlCl3-treated rats, brain acetylcholinesterase (AChE) activity was significantly raised by 50.6 % compared with the saline group. Brain AChE activity showed significant decrease after treatment with 100 mg/kg piracetam (by 29.8 %), 20 mg/kg vincamine (by 39.1 %), vinpocetine (by 25.6 % and 38.9 %), piracetam plus vincamine (by 74.3 %), piracetam plus vinpocetine (by 61.5 %), and donepezil (by 59.1 %; Fig. 2).
Butrylcholinesterase activity
In rats treated with AlCl3, butrylcholinesterase (BChE) activity in brain increased by 58.8 % compared with the saline group. BChE activity showed a significant decrease after treatment with 100 mg/kg piracetam (by 32.8 %), 10 mg/kg vincamine (by 42.8 %), vinpocetine (by 37.7 and 22.3 %), piracetam plus vincamine (by 37.9 %), piracetam plus vinpocetine (by 38.1 %), and donepezil (by 42.1 %). The administration of donepezil had no significant effect on BChE activity in AlCl3-treated rats (Fig. 3).
Prostaglandin E2
The administration of AlCl3 did not led to a significant change in brain PGE2 compared with the saline group (17.8 % increase, p > 0.05). In AlCl3-treated rats, however, brain PGE2 concentration increased by the high dose of piracetam (by 46.4 %), vincamine (by 39 %), vinpocetine (by 57.6 %), piracetam plus vincamine (by 27.1 %), and piracetam plus vinpocetine (by 21.3 %)(Fig. 4).
Histopathological results
Microscopic examination of the brain tissue from normal rats stained with Hx & E revealed regular normal-looking neurons with vesicular nuclei and prominent nucleoli with relatively pale-stained faint nuclear chromatin. The surrounding glial cells were evenly distributed and had small nuclei with densely stained condensed chromatin. The cerebral cortex was of average thickness, all indicative of normal cerebral tissue (Fig. 5a, b).
Hx & E stained sections showing the structure of the normal cerebral cortex (a, b): the innermost granular layer (red arrow) composed of many small cells; Purkinje cell layer, formed of large flask-shaped cells (blue arrow); and the outermost molecular layer that contains a few small nerve cells and many unmyelinated nerve fibers (red star) (Hx & E ×400)
Rats that received only AlCl3 showed atrophy of the cortex, shrinkage of the neuronal cell bodies, pyknosis of their nuclei, disappearance of the nucleoli, and loss of Nissl substance, with intense eosinophilia of the cytoplasm (red neurons), surrounded by vacuolations with cytoplasmic neurofibrillary tangles and associated with vascular congestion in the cortex and choroid plexus (Fig. 6a). Rats treated with AlCl3 along with piracetam (100 mg/kg) showed near average cortical thickness with mildly degenerated neurons. No neurofibrillary tangles were detected but there was still little vascular congestion (Fig. 6b). With the higher dose of the drug (300 mg/kg), cortical thickness was almost like the saline control with degenerated neurons surrounded by vacuolations. No neurofibrillary tangles were seen. Vascular congestion was still detected (Fig. 6c). In the group treated with AlCl3 along with donepezil at 5 mg/kg, there was average cortical thickness, mildly degenerated neurons, but no neurofibrillary tangles. Little vascular congestion was observed (Fig. 6d).
Hx & E stained sections of brain tissue of a AlCl3 (10 mg/kg)-treated rat showing wide neuronal degeneration and vacuolations with neurofibrillary tangles (arrowhead) (Hx & E ×100); b AlCl3 + piracetam (100 mg/kg) showing neuronal degeneration with surrounding vacuolations (note some healthy neurons) (Hx & E ×400); c AlCl3 + piracetam (300 mg/kg) showing congestion in the brain substance (Hx & E ×100); d AlCl3 + donepezil (5 mg/kg) showing neuronal regeneration (Hx & E ×200)
With vincamine treatment at 10 mg/kg, neuronal degeneration was evident but to a lesser extent than in the AlCl3 control group. No neurofibrillary tangles were detected, but vascular congestion was seen in both choroid plexus and brain substance (Fig. 7a). Rats treated with AlCl3 and vincamine at 20 mg/kg showed cortical neuronal degeneration with surrounding vacuolations. Average cortical thickness, scattered neurofibrillary tangles, and associated vascular congestion were observed (Fig. 7b).
Hx & E stained sections of brain tissue of a AlCl3 + vincamine (10 mg/kg) showing regenerating neurons. Note the restoration of nuclear roundness, appearance of nucleolus, and the open chromatin pattern (Hx & E ×400); b AlCl3 + vincamine (20 mg/kg) showing neuronal degeneration (Hx & E ×400); c AlCl3 + vinpocetine (10 mg/kg) showing congested choroid plexus (Hx & E ×100); d AlCl3 + vinpocetine (20 mg/kg) showing neuronal degeneration (Hx & E ×200)
Following vinpocetine treatment at 10 mg/kg, mild neuronal degeneration with occasional peri-neuronal vacuoles was seen. The cortical thickness was average. No neurofibrillary tangles were detected but mild congestion was seen (Fig. 7c). With vinpocetine treatment at 20 mg/kg, degenerative changes were seen in most of neurons with surrounding vacuolations but with normal cortical thickness. No neurofibrillary tangles were seen but mild vascular congestion was evident (Fig. 7d).
Brain sections of rats treated with piracetam (100 mg/kg) and either vincamine (10 mg/kg) or vinpocetine (10 mg/kg) showed cortical neuronal degeneration with surrounding vacuolations. Average cortical thickness, scattered neurofibrillary tangles, associated vascular congestion, and brain edema were seen (Fig. 8a, b).
Overall, the groups treated with low doses of singly used drugs and the donepezil-treated group had the best improvement in neuronal look, cortical thickness, and degree of vascular congestion, while the combined drugs in addition to evident previously mentioned parameters showed brain edema.
Caspase-3 immunoreactivity
Figure 9 shows brain sections stained with caspase-3 antibody from saline control rat (Fig. 9a, b) and after AlCl3, where degenerated neurons for caspase-3 were seen (Fig. 9c–e). Following treatment with vincamine at 10 mg/kg, degenerated neurons for caspase-3 were observed but with some regenerating neurons (Fig. 9f).
Brain sections stained with caspase-3 antibody from a, b saline control rat showing cytoplasmic staining neurons for caspase-3 (Hx & E ×100); c–e AlCl3 control showing cytoplasmic staining of degenerated neurons for caspase-3 (Hx & E ×100, 200, 400); f AlCl3 + vincamine (10 mg/kg) showing cytoplasmic staining of degenerated neurons for caspase-3. Note some regenerating neurons (black arrows) (Hx & E ×100)
Congo red staining
Sections from AlCl3 control rats stained with Congo red stain showed amyloid deposition in degenerated ganglionic cells (Fig. 10a, b). Figure 10c shows amyloid deposition in neurons after treatment with vincamine 20 mg/kg. Figure 10d–f shows amyloid deposition in neurons after treatment with piracetam 100 mg/kg + vincamine 10 mg/kg.
Brain sections stained with Congo red from a AlCl3 control rats showing amyloid deposition in degenerated ganglionic cells (arrowhead) (×200); b AlCl3 control rats showing neurofibrillary tangles and amyloid deposition (arrowhead) (×200); c AlCl3 + vincamine 20 mg/kg-treated group showing amyloid deposition in neurons (arrowhead) (×100); d, e AlCl3 + piracetam 100 mg/kg + vincamine 10 mg/kg-treated rats showing amyloid deposition in neurons (arrowhead) (×100 and ×200); f AlCl3 + piracetam 100 mg/kg + vincamine 10 mg/kg-treated rats showing homogenous structureless amyloid deposition (arrowhead) (×400)
Discussion
In this study, the repeated daily administration of AlCl3 for 45 days in rats was associated with increased brain oxidative stress. Malondialdehyde, a marker of lipid peroxidation, was increased (Gutteridge 1995), suggesting free radical attack on membrane lipids. Meanwhile, reduced glutathione, a major brain anti-oxidant and free radical scavenger (Bains and Shaw 1997; Dringen 2000), showed a marked decrease, possibly due to increased consumption by the increased free radicals. The intracellular tripeptide glutathione (glycyl–glutamic acid–cysteine) is the brain’s major redox buffer, and reduced levels have been detected in the brain from patients with neurodegenerative diseases such as Parkinson’s disease (Sofic et al. 1992; Sian et al. 1994) and Alzheimer’s disease (Ramassamy et al. 2000). The study also indicated increased nitric oxide levels in brains of AlCl3-treated rats. Nitric oxide is an important biological molecule involved in neurotransmission and vasodilatation. It is synthesized in vivo from L-arginine by the action of nitric oxide synthases (NOS), a family with four isoforms: endothelial, neuronal, inducible, and mitochondrial (Guix et al. 2005). It is nitric oxide which is generated in excess and for prolonged time by the inducible form of nitric oxide (iNOS) expressed following immunological or inflammatory stimulation in the immune and glial cells that evokes tissue damage (Guix et al. 2005; Förstermann and Sessa 2012). Nitric oxide neurotoxicity can be mediated via oxidative and nitrative stresses. The most important is the reaction of nitric oxide with superoxide (O2•−) which results in the formation of peroxynitrite (ONOO−), a highly reactive radical capable of damaging cellular macromolecules (lipids, proteins, DNA) (Boje 2004). The present findings are consistent with other studies showing elevated levels of oxidative stress (Yuan et al. 2012) and decreased reduced glutathione and glutathione reductase activity (Jacewicz et al. 2009) in rat brain following repeated administration of AlCl3. Although Al has a fixed oxidation number and therefore cannot undergo redox reactions, the metal can induce oxidative damage through multiple mechanisms, e.g., by altering iron homeostasis and stimulating iron-initiated free-radical-induced tissue damage (Gutteridge et al. 1985).
The present results also indicated decreased paraoxonase 1 (PON1) activity in the brain of AlCl3-treated rats. The paraoxonase family of enzymes is involved mainly with the detoxification of organophosphates and nerve agents (La Du 1992). PON1 has an anti-oxidant role (Watson et al. 1995; Rajkovic et al. 2011; Furlong 2008) and has recently been of much interest in view of a possible association with neurodegenerative disorders, e.g., Alzheimer’s disease and other dementias (Menini and Gugliucci 2013). In these patients, the level of the enzyme activity decreased in their sera (Wehr et al. 2009). A markedly decreased PON1 activity was also observed in an experimental model of multiple sclerosis (Abdel-Salam et al. 2012). The decline in PON1 activity in the present study is consistent with earlier observations using the same model (Abdel-Salam et al. 2014) and suggests inactivation of the enzyme by the increased level of oxidative stress and/or direct inhibition by AlCl3.
Several nootropic drugs, e.g., piracetam, vincamine, and vinpocetine, are being used to improve cognitive functions in the elderly with chronic cerebral hypo-perfusion or in those with devastating Alzheimer’s disease (Waegemans et al. 2002; Hadjiev 2003). In this study, these agents were evaluated for their ability to modulate the biochemical changes and neuronal injury caused by AlCl3. It was noted that treatment with the low doses of piracetam, vincamine, and vinpocetine resulted in significant decrease in brain lipid peroxidation and nitric oxide content, suggesting an anti-oxidant effect. In contrast, the higher dose of the agents were not effective in decreasing lipid peroxidation or brain nitric oxide although they lessened the decline reduced glutathione and PON1 activity induced by AlCl3. These findings suggest that the nootropic drugs piracetam, vincamine, and vinpocetine at high doses might increase oxidative stress.
Studies have reported anti-oxidant effects for piracetam and vinpocetine. In vitro, vinpocetine demonstrated hydroxyl radical scavenging capability near to that of vitamin E in the Fenton reaction (Oláh et al. 1990). The drug also showed marked anti-oxidant activity against free radicals generated by phenazine methosulphate. Piracetam showed anti-oxidant capacity only at concentrations 10 times higher than the therapeutic concentrations (Horvath et al. 2002). In rabbits with spinal cord ischemia/reperfusion injury, the drug displayed neuroprotective and anti-oxidant properties (decreasing malondialdehyde and xanthine oxidase level, while increasing glutathione peroxidase activity) (Kalkan et al. 2011). In rat primary cortical cells, subjected to oxygen and glucose deprivation, piracetam reduced neuronal damage and exerted anti-oxidant effects (He et al. 2014). Moreover, either piracetam (1 mM) or vinpocetine (0.1 μM) protected astrocytes against hypoxic injury in culture, by increasing intracellular ATP, and inhibiting caspase-3 activity. The higher concentration of vinpocetine (10 μM) was, however, detrimental in hypoxic conditions (Gabryel et al. 2002).
One possible explanation for the observed effects of the high doses of the nootropic drugs might be their ability to increase brain dopamine and/or dopaminergic neurotransmission (Rago et al. 1981; Stancheva et al. 1991; Budygin et al. 1996; Trejo et al. 2001). This might increase free radical generation due to increased dopamine metabolism, by monoamine oxidase, and/or dopamine autoxidation into reactive dopamine quinines with consequent attack on thiol compounds such as GSH and cysteinyl residues on proteins (LaVoie and Hastings 1999; Hermida-Ameijeiras et al. 2004). It is also possible that these drugs act as free radicals, and this explains sparing of reduced glutathione and PON1 activity. The present findings confirm previous observations in a demyelination model caused by intracerebral injection of ethidium bromide in rats. In that study, the increase in brain MDA decreased by treatment with vinpocetine at 1.5 mg/kg or piracetam at 150 mg/kg but increased by the higher dose of vinpocetine or piracetam (6 and 300 mg/kg, respectively) (Abdel-Salam et al. 2012).
Neuroinflammation is an important contributor in the pathogenesis of neurodegenerative diseases (Frank-Cannon et al. 2009). The arachidonic acid metabolite prostaglandin E2 (PGE2) is involved in the inflammatory responses following brain injury, bacterial or viral infections (Matsumura and Kobayashi 2004; Vasilache et al. 2015), and high levels have been found in neurodegenerative disorders such as Alzheimer’s disease (Hoozemans et al. 2001), prion’s disease (Pocchiari and Levi 2000), and autism (Brigandi et al. 2015). Moreover, selective inhibition of the EP2 receptor or EP2 receptor deletion was associated with decreased neuronal injury and improved functional recovery in experimental models of brain damage (Rojas et al. 2015; Leclerc et al. 2015). In this study, increased levels of PGE2 have been demonstrated in AlCl3-treated rats. Other researchers have indicated increased levels of PGE2, and other arachidonic acid metabolites in rat hippocampus following chronic aluminum gluconate administration. This occurred along with hippocampal neuronal injury and deficits in learning and memory (Wang et al. 2015). We also observed increased brain PGE2 concentrations after treatment with the high dose of piracetam, vincamine, and vinpocetine, as well as by the combined administration of the lower doses of piracetam plus either vincamine or vinpocetine. This finding is intriguing and might suggest an enhancing effect on the aluminum-induced brain inflammation by the high doses of the nootropic agents. In their study, Bhattacharya et al. (1989) reported significant increase in rat brain PGE2 and PGF2 alpha after treatment with 100 mg/kg piracetam.
Impaired central cholinergic neurotransmission is a key component of memory decline in disorders like Alzheimer’s disease (Coyle et al. 1983; Francis et al. 1999) and possibly in normal aging (Bartus et al. 1982). Consequently, boosting cholinergic activity through increasing available acetylcholine (ACh) with the use of centrally acting cholinesterase inhibitors like donepezil is a cornerstone of therapy and results in clinically measurable benefit in cognitive function, and behavior (Sugimoto et al. 2002; Wilkinson et al. 2004). In mammals, two cholinesterases exist in brain, predominantly acetylcholinesterase (AChE) (80 %), and butyrylcholinesterase (BChE) or pseudocholinesterase. Inhibiting AChE enhances cholinergic neurotransmission and increases the availability of acetylcholine. BChE found in neurons and glial cells is considered to play a minor role in regulating brain ACh levels (Greig et al. 2001; Giacobini 2001). There is, however, evidence that inhibition of BChE might find utility in treating advanced Alzheimer’s disease (Greig et al. 2001; Giacobini 2004). In the present study, AChE and BChE activities in brain increased following the repeated administration of AlCl3. Several studies reported alterations in AChE activity in rats chronically treated with aluminum. Mice treated orally with AlCl3 or aluminum lactate showed increased AChE activity in their brain homogenates (Zatta et al. 2002). Mice given AlCl3 (10 mg/kg/day) for 90 days also showed significant elevation of AChE activity in cerebral cortex and hippocampus and memory impairment (Yang et al. 2013). Kaizer et al. (2008) found increased AChE activity in striatum, and hypothalamus of rats following chronic treatment with AlCl3 (50 mg/kg/day). AChE activity in cerebellum, hippocampus, and cerebral cortex was, however, decreased by Al. Stevanović et al. (2009) reported a significant rise in AChE activity in the rat brain and serum following treatment with AlCl3. Gulya et al. (1990) suggested that the cholinotoxic effects of Al are likely the result of neurodegenerative effects. The authors found significant decrease in choline acetyltransferase activities but no change in AChE activity in the parietal cortex, the hippocampus, and the striatum of rats after chronic Al treatment. In vitro, low concentrations of Al slightly increased while high concentrations inhibited AChE activity.
In the present study, AChE and BChE activities showed significant and marked decrease after treatment with the lower dose of piracetam, vinpocetine, and piracetam plus either vincamine or vinpocetine. AChE activity decreased following 20 mg/kg vincamine, and BChE activity after decreased following 10 mg/kg vincamine. AChE but not BChE activity decreased after donepezil. The latter is an effective and selective inhibitor for AChE (Sugimoto et al. 2002). When given to rats, donepezil (2.5 mg/kg, p.o.), inhibited whole-brain AChE activity and increased the synaptic ACh concentration in the hippocampus (Kosasa et al. 1999). It is likely, however, that the observed changes in AChE and BChE activities in brain of AlCl3-treated rats following the lower doses of piracetam, vinpocetine, piracetam reflect neuroprotection.
Moreover, histopathological examination and caspase-3 immunolocalization in brain have shown that AlCl3 resulted in neuronal degeneration and induced apoptosis associated with the increase of caspase-3 expression in degenerated neurons. In the present study, the biochemical findings of decreased oxidative stress with the low doses of piracetam, vincamine, or vinpocetine in contrast to the effect of the high doses of these drugs in increasing brain PGE2 appear to correlate with the histopathological observations, where reduced neuronal degeneration and improved cortical thickness were seen only in the brain of AlCl3-treated rats after treatment with the low dose of singly used drugs.
References
Abdel-Salam OME, Khadrawy YA, Mohammed NA (2012) Neuroprotective effect of nitric oxide donor isosorbide-dinitrate against oxidative stress induced by ethidium bromide in rat brain. EXCLI J 11:125–141
Abdel-Salam OME, Youness ER, Mohammed NA, Abu Elhamed WA (2015) Nuclear factor-kappa B and other oxidative stress biomarkers in serum of autistic children. Open J Mol Integr Physiol 5:18–27
Abdel-Salam OME, Youness ER, Morsy FM, Mahfouz MM, Kenawy SA (2014) Study of the effect of antidepressant drugs and donepezil on aluminum-induced memory impairment and biochemical alterations in rats. Comp Clin Pathol. doi:10.1007/s00580-014-1994-7
Ahn HS, Crim W, Romano M, Sybertz E, Pitts B (1989) Effects of selective inhibitors on cyclic nucleotide phosphodiesterases of rabbit aorta. Biochem Pharmacol 38:3331–3339
Aksu F, Gültekin I, Inan SY, Baysal F (1998) The effects of piracetam on morphine-induced amnesia and analgesia: the possible contribution of central opiatergic mechanisms on the antiamnestic effect of piracetam. Inflammopharmacology 6:53–65
Bains JS, Shaw CA (1997) Neurodegenerative disorders in humans: the role of glutathione in oxidative stress-mediated neuronal death. Brain Res Brain Res Rev 25:335–358
Bartus RT, Dean RL 3rd, Beer B, Lippa AS (1982) The cholinergic hypothesis of geriatric memory dysfunction. Science 217:408–414
Bhattacharya SK, Upadhyay SN, Jaiswal AK, Bhattacharya S (1989) Effect of piracetam, a nootropic agent, on rat brain monoamines and prostaglandins. Indian J Exp Biol 27:261–264
Boje KMK (2004) Nitric oxide neurotoxicity in neurodegenerative diseases. Front Biosci 9:763–776
Brigandi SA, Shao H, Qian SY, Shen Y, Wu BL, Kang JX (2015) Autistic children exhibit decreased levels of essential fatty acids in red blood cells. Int J Mol Sci 16:10061–10076
Budygin EA, Gaĭnetdinov RR, Titov DA, Kovalev GI (1996) The effect of a low dose of piracetam on the activity of the dopaminergic system in the rat striatum. Eksp Klin Farmakol 59:6–8, Article in Russian
Cai Y, Li JD, Yan C (2013) Vinpocetine attenuates lipid accumulation and atherosclerosis formation. Biochem Biophys Res Commun 434:439–443
Castellani RJ, Lee HG, Zhu X, Nunomura A, Perry G, Smith MA (2006) Neuropathology of Alzheimer disease: pathognomonic but not pathogenic. Acta Neuropathol 111:503–509
Chopin P, Briley M (1992) Effects of four non-cholinergic cognitive enhancers in comparison with tacrine and galanthamine on scopolamine-induced amnesia in rats. Psychopharmacology 106:26–30
Coyle JT, Price DL, De Long MR (1983) Alzheimer’s disease: a disorder of cortical cholinergic innervation. Science 219:1184–1190
Danielson SR, Andersen JK (2008) Oxidative and nitrative protein modifications in Parkinson’s disease. Free Radic Biol Med 44:1787–1794
Drago D, Folin M, Baiguera S, Tognon G, Ricchelli F, Zatta P (2007) Comparative effects of Abeta(1-42)-Al complex from rat and human amyloid on rat endothelial cell cultures. J Alzheimers Dis 11:33–44
Dringen R (2000) Metabolism and functions of glutathione in brain. Prog Neurobiol 62:649–671
Eckert GP, Cairns NJ, Muller WE (1999) Piracetam reverses hippocampal membrane alterations in Alzheimer’s disease. J Neural Transm 106:757–761
Ellman GL, Courtney KD, Andreas V Jr, Feather-Stone RM (1961) A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharm 7:88–90
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem 82:70–77
Exley C (2004) The pro-oxidant activity of aluminum. Free Radic Biol Med 36:380–387
Bondy SC (2014) Prolonged exposure to low levels of aluminum leads to changes associated with brain aging and neurodegeneration. Toxicology 315:1–7
Esparza JL, Gomez M, Romeu M, Mulero M, Sanchez DJ, Mallol J, Domingo JL (2003) Aluminum-induced pro-oxidant effects in rats: protective role of exogenous melatonin. J Pineal Res 35:32–39
Fang Y, Qiu Z, Hu W, Yang J, Yi X, Huang L, Zhang S (2014) Effect of piracetam on the cognitive performance of patients undergoing coronary bypass surgery: a meta-analysis. Exp Ther Med 7:429–434
Fischhof PK, Möslinger-Gehmayr R, Herrmann WM, Friedmann A, Russmann DL (1996) Therapeutic efficacy of vincamine in dementia. Neuropsychobiology 34:29–35
Förstermann U, Sessa WC (2012) Nitric oxide synthases: regulation and function. Eur Heart J 33(7):829–837, 837a–837d
Francis PT, Palmer AM, Snape M, Wilcock GK (1999) The cholinergic hypothesis of Alzheimer’s disease: a review of progress. J Neurol Neurosurg Psychiatry 66:137–147
Frank-Cannon TC, Alto LT, McAlpine FE, Tansey MG (2009) Does neuroinflammation fan the flame in neurodegenerative diseases? Mol Neurodegener 4:47
Furlong CE (2008) Paraoxonases: an historical perspective. In: Mackness B, Mackness M, Aviram M, Paragh G (eds) The paraoxonases: their role in disease development and xenobiotic metabolism. Springer, Dordrecht, pp 3–31
Gabryel B, Adamek M, Pudełko A, Małecki A, Trzeciak HI (2002) Piracetam and vinpocetine exert cytoprotective activity and prevent apoptosis of astrocytes in vitro in hypoxia and reoxygenation. Neurotoxicology 23:19–31
Giacobini E (2001) Selective inhibitors of butyrylcholinesterase: a valid alternative for therapy of Alzheimer’s disease? Drugs Aging 18:891–898
Giacobini E (2004) Cholinesterase inhibitors: new roles and therapeutic alternatives. Pharmacol Res 50:433–440
Giurgea C (1973) The nootropic approach to the pharmacology of the integrative activity of the brain. Cond Reflex 8:108–115
Golub MS, Han B, Keen CL (1999) Aluminum uptake and effects on transferring mediated iron uptake in primary cultures of rat neurons, astrocytes and oligodendrocytes. Neurotoxicology 20:961–970
Gorun V, Proinov I, Baltescu V, Balaban G, Barzu O (1978) Modified Ellman procedure for assay of cholinesterases in crude enzymatic preparation. Anal Biochem 86:324–326
Greig NH, Utsuki T, Yu Q, Zhu X, Holloway HW, Perry T, Lee B, Ingram DK, Lahiri DK (2001) A new therapeutic target in Alzheimer’s disease treatment: attention to butyrylcholinesterase. Curr Med Res Opin 17:159–165
Gulya K, Rakonczay Z, Kása P (1990) Cholinotoxic effects of aluminum in rat brain. J Artic J Neurochem 54:1020–1026
Gulyás B, Halldin C, Vas A, Banati RB, Shchukin E, Finnema S, Tarkainen J, Tihanyi K, Szilágyi G, Farde L (2005) [11C]vinpocetine: a prospective peripheral benzodiazepine receptor ligand for primate PET studies. J Neurol Sci 229–230:219–223
Gutteridge JM (1995) Lipid peroxidation and antioxidants as biomarkers of tissue damage. Clin Chem 41:1819–1828
Gutteridge JM, Quinlan GJ, Clark I, Halliwell B (1985) Aluminium salts accelerate peroxidation of membrane lipids stimulated byiron salts. Biochim Biophys Acta 835:441–447
Guix FX, Uribesalgo I, Coma M, Muñoz FJ (2005) The physiology and pathophysiology of nitric oxide in the brain. Prog Neurobiol 76:126–152
Hadjiev D (2003) Asymptomatic ischemic cerebrovascular disorders and neuroprotection with vinpocetine. Ideggyogy Sz 56:166–172
Halliwell B (1992) Reactive oxygen species and the central nervous system. J Neurochem 59:1609–1623
Halliwell B (2001) Role of free radicals in the neurodegenerative diseases: therapeutic implications for antioxidant treatment. Drugs Aging 18:685–716
Halliwell B, Gutteridge JM (eds) (1989) Free radicals in biology and medicine, 2nd ed. Clarendon Press, Oxford, pp 22–85
He Z, Hu M, Zha YH, Li ZC, Zhao B, Yu LL, Yu M, Qian Y (2014) Piracetam ameliorated oxygen and glucose deprivation-induced injury in rat cortical neurons via inhibition of oxidative stress, excitatory amino acids release and P53/Bax. Cell Mol Neurobiol 34:539–547
Heckman PR, Wouters C, Prickaerts J (2015) Phosphodiesterase inhibitors as a target for cognition enhancement in aging and Alzheimer’s disease: a translational overview. Curr Pharm Des 21:317–331
Hermida-Ameijeiras A, Méndez-Alvarez E, Sánchez-Iglesias S, Sanmartín-Suárez C, Soto-Otero R (2004) Autoxidation and MAO-mediated metabolism of dopamine as a potential cause of oxidative stress: role of ferrous and ferric ions. Neurochem Int 45:103–116
Higashino K, Takahashi Y, Yamamura Y (1972) Release of phenyl acetate esterase from liver microsomes by carbon tetrachloride. Clin Chim Acta 41:313–320
Hoozemans JJ, Rozemuller AJ, Janssen I, De Groot CJ, Veerhuis R, Eikelenboom P (2001) Cyclooxygenase expression in microglia and neurons in Alzheimer’s disease and control brain. Acta Neuropathol (Berl) 101:2–8
Horvath B, Marton Z, Halmosi R, Alexy T, Szapary L, Vekasi J, Biro Z, Habon T, Kesmarky G, Toth K (2002) In vitro antioxidant properties of pentoxifylline, piracetam, and vinpocetine. Clin Neuropharmacol 25:37–42
Jacewicz M, CzapskiGA KI, Strosznajder RP (2009) Systemic administration of lipopolysaccharide impairs glutathione redox state and object recognition in male mice. The effect of PARP-1 inhibitor. Folia Neuropathol 47:321–328
Jeon KI, Xu X, Aizawa T, Lim JH, Jono H, Kwon DS, Abe J, Berk BC, Li JD, Yan C (2010) Vinpocetine inhibits NF-kappaB-dependent inflammation via an IKK-dependent but PDE-independent mechanism. Proc Natl Acad Sci U S A 107:9795–9800
Jovanović ZB, Pavlović AM, Pekmezović T, Mijajlović M, Covicković NS (2013) Transcranial Doppler assessment of cerebral vasomotor reactivity in evaluating the effects of vinpocetine in cerebral small vessel disease: a pilot study. Ideggyogy Sz 66:263–268
Kaizer RR, Corrêa MC, Gris LR, da Rosa CS, Bohrer D, Morsch VM, Schetinger MR (2008) Effect of long-term exposure to aluminum on the acetylcholinesterase activity in the central nervous system and erythrocytes. Neurochem Res 33:2294–2301
Kalkan E, Keskin F, Kaya B, Esen H, Tosun M, Kalkan SS, Erdi F, Unlü A, Avunduk MC, Cicek O (2011) Effects of iloprost and piracetam in spinal cord ischemia-reperfusion injury in the rabbit. Spinal Cord 49:81–86
Kawahara M (2005) Effects of aluminum on the nervous system and its possible link with neurodegenerative diseases. J Alzheimers Dis 8:171–182
Keil U, Scherping I, Hauptmann S, Schuessel K, Eckert A, Müller WE (2006) Piracetam improves mitochondrial dysfunction following oxidative stress. Br J Pharmacol 147:199–208
Kessler J, Thiel A, Karbe H, Heiss WD (2000) Piracetam improves activated blood flow and facilitates rehabilitation of poststroke aphasic patients. Stroke 31:2112–2116
Kosasa T, Kuriya Y, Matsui K, Yamanishi Y (1999) Effect of donepezil hydrochloride (E2020) on basal concentration of extracellular acetylcholine in the hippocampus of rats. Eur J Pharmacol 380:101–107
Kurz C, Ungerer I, Lipka U, Kirr S, Schütt T, Eckert A, Leuner K, Müller WE (2010) The metabolic enhancer piracetam ameliorates the impairment of mitochondrial function and neurite outgrowth induced by beta-amyloid peptide. Br J Pharmacol 160:246–257
La Du BN (1992) Human serum paraoxonase: arylesterase. In: Kalow W (ed) Pharmacogenetics of drug metabolism. Pergamon Press, New York, pp 51–91
LaVoie MJ, Hastings TG (1999) Dopamine quinone formation and protein modification associated with the striatal neurotoxicity of methamphetamine: evidence against a role for extracellular dopamine. J Neurosci 19:1484–1491
Leclerc JL, Lampert AS, Diller MA, Immergluck JB, Doré S (2015) Prostaglandin E2 EP2 receptor deletion attenuates intracerebral hemorrhage-induced brain injury and improves functional recovery. ASN Neuro 7: pii: 1759091415578713
Lévesque L, Mizzen CA, McLachlan DR, Fraser PE (2000) Ligand specific effects on aluminum incorporation and toxicity in neurons and astrocytes. Brain Res 877:191–202
Matsumura K, Kobayashi S (2004) Signaling the brain in inflammation: the role of endothelial cells. Front Biosci 9:2819–2826
McCord JM (2000) The evolution of free radicals and oxidative stress. Am J Med 108:652–659
Menini T, Gugliucci A (2013) Paraoxonase 1 in neurological disorders. Redox Rep 19:49–58
Miranda KM, Espey MG, Wink DA (2001) A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide 5:62–71
Nyakas C, Felszeghy K, Szabó R, Keijser JN, Luiten PG, Szombathelyi Z, Tihanyi K (2009) Neuroprotective effects of vinpocetine and its major metabolite cis-apovincaminic acid on NMDA-induced neurotoxicity in a rat entorhinal cortex lesion model. CNS Neurosci Ther 15:89–99
Oláh VA, Balla G, Balla J, Szabolcs A, Karmazsin L (1990) An in vitro study of the hydroxyl scavenger effect of Cavinton. Acta Paediatr Hung 30:309–316
Pallavi S, Amar J, Singh R, Hussain E, Sharma D (2008) Aluminium induced electrophysiological, biochemical and cognitive modifications in the hippocampus of aging rats. Neurotoxicology 29:1069–1079
Perry VH, Cunningham C, Holmes C (2007) Systemic infections and inflammation affect chronic neurodegeneration. Nat Rev Immunol 7:161–167
Pocchiari M, Levi G (2000) Increased brain synthesis of prostaglandin E2 and F2-isoprostane in human and experimental transmissible spongiform encephalopathies. J Neuropathol Exp Neurol 59:866–871
Rajkovic MG, Rumora L, Barisic K (2011) The paraoxonase 1, 2 and 3 in humans. Biochem Med (Zagreb) 21:122–130
Rago LK, Allikmets LH, Zarkovsky AM (1981) Effects of piracetam on the central dopaminergic transmission. Naunyn-Schmiedeberg’s Arch Pharmacol 318:36–37
Ramassamy C, Averill D, Beffert U, Theroux L, Lussier-Cacan S, Cohn JS et al (2000) Oxidative insults are associated with apolipoprotein E genotype in Alzheimer’s disease brain. Neurobiol Dis 7:23–37
Rojas A, Ganesh T, Lelutiu N, Gueorguieva P, Dingledine R (2015) Inhibition of the prostaglandin EP2 receptor is neuroprotective and accelerates functional recovery in a rat model of organophosphorus induced status epilepticus. Neuropharmacology 93:15–27
Roth AD, Ramírez G, Alarcón R, Von Bernhardi R (2005) Oligodendrocytes damage in Alzheimer’s disease: Beta amyloid toxicity and inflammation. Biol Res 38:381–387
Ruiz-Larrea MB, Leal AM, Liza M, Lacort M, de Groot H (1994) Antioxidant effects of estradiol and 2-hydroxyestradiol on iron induced lipid peroxidation of rat liver microsomes. Steroids 59:383–388
Sajdel-Sulkowska EM, Lipinski B, Windom B, Audhya T, McGinnis W (2008) Oxidative stress in Autism: elevated cerebellar 3-nitrotyrosine levels. Am J Biochem Biotechnol 4:73–84
Sian J, Dexter DT, Lees AJ, Daniel S, Agid Y, Javoy-Agid F, Jenner P, Marsden CD (1994) Alterations in glutathione levels in Parkinson’s disease and other neurodegenerative disorders affecting basal ganglia. Ann Neurol 36:348–355
Sies H (ed) (1991) Oxidative stress. Oxidants and antioxidants. Academic Press, New York
Sofic E, Lange KW, Jellinger K, Riederer P (1992) Reduced and oxidized glutathione in the substantia nigra of patients with Parkinson’s disease. Neurosci Lett 142:128–130
Stahlhut L, Grotemeyer KH, Husstedt IW, Evers S (2014) The impact of stroke on cognitive processing—a prospective event-related potential study. J Neurol Sci 339:157–163
Stancheva SL, Petkov VD, Hadjiivanova CI, Petkov VV (1991) Age-related changes of the effects of a group of nootropic drugs on the content of rat brain biogenic monoamines. Gen Pharmacol 22:873–877
Stevanović I, Jovanović M, Jelenković A, Bokonjić D, Čolić M, Stojanović I, Ninković M (2009) Effect of L-NAME on AlCl3-induced toxicity in rat brain. Acta Vet (Beograd) 59:133–146
Struys-Ponsar C, Kerkhofs A, Gauthier A, Soffié M, van den Bosch de Aguilar P (1997) Effects of aluminum exposure on behavioral parameters in the rat. Pharmacol Biochem Behav 56:643–648
Sugimoto H, Hiroo Ogura H, Arai Y, Iimura Y, Yamanishi Y (2002) Research and development of donepezil hydrochloride, a new type of acetylcholinesterase inhibitor. Jpn J Pharmacol 89:7–20
Szilágyi G, Nagy Z, Balkay L, Boros I, Emri M, Lehel S, Márián T, Molnár T, Szakáll S, Trón L, Bereczki D, Csiba L, Fekete I, Kerényi L, Galuska L, Varga J, Bönöczk P, Vas A, Gulyás B (2005) Effects of vinpocetine on the redistribution of cerebral blood flow and glucose metabolism in chronic ischemic stroke patients: a PET study. J Neurol Sci 229–230:275–284
Tárnok K, Kiss E, Luiten PG, Nyakas C, Tihanyi K, Schlett K, Eisel UL (2008) Effects of vinpocetine on mitochondrial function and neuroprotection in primary cortical neurons. Neurochem Int 53:289–295
Trejo F, Nekrassov V, Sitges M (2001) Characterization of vinpocetine effects on DA and DOPAC release in striatal isolated nerve endings. Brain Res 909:59–67
Vasilache AM, Qian H, Blomqvist A (2015) Immune challenge by intraperitoneal administration of lipopolysaccharide directs gene expression in distinct blood–brain barrier cells toward enhanced prostaglandin E2 signaling. Brain Behav Immun pii: S0889-1591(15)00021-5
Waegemans T, Wilsher CR, Danniau A et al (2002) Clinical efficacy of piracetam in cognitive impairment: a meta-analysis. Dement Geriatr Cogn Disord 13:217–224
Walton JR (2007) An aluminum-based rat model for Alzheimer’s disease exhibits oxidative damage, inhibition of PP2A activity, hyperphosphorylated tau, and granulovacuolar degeneration. Inorg Biochem 101:1275–1284
Walton JR, Wang MX (2009) APP expression, distribution and accumulation are altered by aluminum in a rodent model for Alzheimer’s disease. J Inorg Biochem 103:1548–1554
Wang H, Ye M, Yu L, Wang J, Guo Y, Lei W, Yang J (2015) Hippocampal neuronal cyclooxygenase-2 downstream signaling imbalance in a rat model of chronic aluminium gluconate administration. Behav Brain Funct 11:8
Warner DS, Sheng H, Batinic-Haberle I (2004) Oxidants, antioxidants and the ischemic brain. J Exp Biol 207:3221–3231
Watson AD, Berliner JA, Hama SY, La Du BN, Faull KF, Fogelman AM, Navab M (1995) Protective effect of high density lipoprotein associated paraoxonase. Inhibition of the biological activity of minimally oxidized low density lipoprotein. J Clin Invest 96:2882–2891
Wehr H, Bednarska-Makaruk M, Graban A, Lipczyńska-Łojkowska W, Rodo M, Bochyńska A, Ryglewicz D (2009) Paraoxonase activity and dementia. J Neurol Sci 283:107–108
Wilkinson DG, Francis PT, Schwam E, Payne-Parrish J (2004) Cholinesterase inhibitors used in the treatment of Alzheimer’s disease: the relationship between pharmacological effects and clinical efficacy. Drugs Aging 21:453–478
Winblad B (2005) Piracetam: a review of pharmacological properties and clinical uses. CNS Drug Rev 11:169–182
Yang WN, Han H, Hu XD, Feng GF, Qian YH (2013) The effects of perindopril on cognitive impairment induced by d-galactose and aluminum trichloride via inhibition of acetylcholinesterase activity and oxidative stress. Pharmacol Biochem Behav 114–115:31–36
Yuan CY, Lee YJ, Hsu GS (2012) Aluminum overload increases oxidative stress in four functional brain areas of neonatal rats. J Biomed Sci 19:5
Yumoto S, Kakimi S, Ohsaki A, Ishikawa A (2009) Demonstration of aluminum in amyloid fibers in the cores of senile plaques in the brains of patients with Alzheimer’s disease. J Inorg Biochem 103:1579–1584
Zatta P, Ibn-Lkhayat-Idrissi M, Zambenedetti P, Kilyen M, Kiss T (2002) In vivo and in vitro effects of aluminum on the activity of mouse brain acetylcholinesterase. Brain Res Bull 59:41–45
Zhou X, Dong XW, Crona J, Maguire M, Priestley T (2003) Vinpocetine is a potent blocker of rat NaV1.8 tetrodotoxin-resistant sodium channels. J Pharmacol Exp Ther 306:498–504
Xu N, Majidi V, Markesbery WR, Ehmann WD (1992) Brain aluminum in Alzheimer’s disease using an improved GFAAS method. Neurotoxicology 13:735–743
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abdel-Salam, O.M.E., Hamdy, S.M., Seadawy, S.A.M. et al. Effect of piracetam, vincamine, vinpocetine, and donepezil on oxidative stress and neurodegeneration induced by aluminum chloride in rats. Comp Clin Pathol 25, 305–318 (2016). https://doi.org/10.1007/s00580-015-2182-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00580-015-2182-0