Abstract
Remifentanil is a synthetic opioid derivative that was introduced into clinical practice in the United States in 1996. The unique modification of its chemical structure to include a methyl-ester ring allows its hydrolysis by non-specific plasma and tissue esterases. This molecular configuration results in its rapid metabolism thereby providing a rapid onset, easy titration by continuous infusion, and a short context-sensitive half-life with rapid elimination. These principles are stable and consistent across all age groups regardless of the infusion characteristics. Owing to these pharmacokinetic characteristics, it is an effective agent in the neonatal population allowing the provision of intense analgesia and anesthesia with a rapid recovery profile in various clinical scenarios. Here, we review the pharmacokinetics of remifentanil in neonates, discuss its clinical applications including intraoperative administration for anesthetic care, unique applications for procedural sedation including endotracheal intubation, and its potential use for sedation in the Intensive Care Unit setting during mechanical ventilation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Remifentanil is the newest of the piperidine synthetic opioid derivatives, being introduced into clinical practice in the United States in 1996. It has potent affinity for μ-opioid receptors but has less affinity for other opioid receptors (κ and σ) [1, 2]. No significant clinical effects have been demonstrated for non-opioid receptors. Its potency and respiratory depressant effect is generally considered to be twice that of fentanyl; however, its half-life is significantly shorter [1–3]. Modification of its chemical structure with the incorporation of a methyl-ester ring into the molecule allows its hydrolysis by non-specific plasma and tissue esterases. Its principle metabolite, GR90291, also binds to μ, κ and σ receptors, but has only 1/4,600th the potency of remifentanil as a μ-opioid agonist [4]. Unlike succinylcholine, its duration of action and elimination are unaffected by acquired or inherited deficiencies of the enzyme butyrylcholinesterase (pseudocholinesterase) [5].
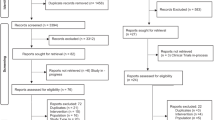
This molecular configuration and its rapid metabolism results in a unique pharmacokinetic and pharmacodynamic profile with a rapid onset, easy titration by continuous infusion, and a short context-sensitive half-life with rapid elimination across all age groups regardless of the infusion characteristics [6, 7]. Owing to its predictable characteristics, it has become an effective agent in the neonatal population allowing the provision of intense analgesia/anesthesia with a rapid recovery profile [8]. Here, we review the pharmacokinetics of remifentanil in neonates, discuss its clinical applications including intraoperative administration for anesthetic care, unique applications for procedural sedation including endotracheal intubation, and its potential use for sedation in the Neonatal Intensive Care Unit (NICU) setting during mechanical ventilation. The literature review included a Medline search (last updated in August 2015) with PubMed using the search terms ‘neonate’ and ‘remifentanil’. The search was limited to human studies in the English language. In addition, we also searched the reference lists of published studies for further potential articles. A published systematic review was also examined for references.
Pharmacodynamic properties
Remifentanil is metabolized by blood and tissue esterases and its principle metabolite is eliminated in the urine. Therefore, unlike other synthetic opioids, the metabolism of remifentanil is independent of both renal and hepatic function [9–11]. Given this non-organ-dependent elimination with sole dependence on plasma and tissue esterases, the pharmacodynamic parameters are similar across all age ranges including neonates. These pharmacokinetic principles and their resultant clinical effects were clearly demonstrated by early trials using intraoperative remifentanil in neonates and infants [12–14]. During general anesthesia with halothane in nitrous oxide and oxygen, remifentanil (5 µg/kg over 1 min) was administered to 42 pediatric patients [12]. The patients were divided into 6 groups based on age including young infants (<2 months), older infants (>2 months to <2 years), young children (2 to <7 years), older children (7 to <13 years), adolescents (13 to <16 years), and young adults (16 to <18 years). The volume of distribution (Vd) was largest in the youngest age group (young infants) at 453 ± 145 mL/kg) and decreased to 223 ± 31 mL/kg in the 13- to 16-year-old patients and 242.5 ± 109.2 mL/kg in young adults. Clearance (CL) was most rapid in the younger age at 90.5 ± 36.8 and 92.1 ± 25.8 mL/kg/min in the infants aged <2 months and those aged 2 months to 2 years, respectively. CL was lowest in the two oldest age groups (57.2 ± 21.1 and 46.5 ± 2.1 mL/kg/min.). Although a higher Vd and CL were noted in the younger age groups, the elimination half-life was similar among the groups with the mean varying from 3.4−5.7 min and the range varying from 3−8 min in all 42 patients. Given these data, the authors predicted that a higher infusion rate was needed to achieve the same target level with neonates compared to older children.
The clinical effect of this rapid metabolism is demonstrated by a two-part study evaluating the perioperative effects of an intraoperative remifentanil infusion [13, 14]. In this multicenter study, 60 infants with pyloric stenosis were randomized to receive either remifentanil with nitrous oxide and oxygen or halothane with nitrous oxide and oxygen as the maintenance anesthetic. No premedication was administered. Anesthesia was induced with atropine (10 µg/kg), propofol (2 mg/kg), and succinylcholine (2 mg/kg). After the trachea was intubated, cis-atracurium was administered as needed to maintain muscle relaxation and rectal acetaminophen was administered for postoperative pain relief. Intraoperative remifentanil dosing ranged from 0.39−1 µg/kg/min with an average infusion rate of 0.55 µg/kg/min. There were no significant differences in the hemodynamic values between the two groups at the various intraoperative points. Extubation time, post-anesthesia care unit discharge time, need for supplemental analgesic medications, and adverse events were similar for both groups. However, significant differences were noted when evaluating postoperative respiratory function. No patient anesthetized with remifentanil, who had a normal preoperative pneumogram, had an abnormal postoperative pneumogram (0 of 22), whereas 3 of 13 patients (23 %) with a normal preoperative pneumogram who were anesthetized with halothane had an abnormal postoperative study (p = 0.04). The authors of the study concluded that “Remifentanil was not associated with clinically observed postoperative respiratory depression, nor was remifentanil associated with a new onset of pneumogram abnormalities in the postoperative period. The use of ultra-short-acting opioids combined with nitrous oxide and oxygen seems to be a safe and appropriate anesthetic technique for infants less than 2 months old in whom tracheal extubation after surgery is anticipated”.
Clinical applications
Intraoperative administration
In addition to the above studies investigating the pharmacokinetic principles of remifentanil and its postoperative effects on respiratory function in neonates and infants, several other authors have described the intraoperative use of remifentanil in neonates and young infants during various surgical procedures. In a prospective study, 30 full-term infants were randomized to receive either 0.4 μg/kg/min of remifentanil infusion or 0.75 % inspired concentration of isoflurane for maintenance anesthesia following anesthetic induction and endotracheal intubation [15]. At the beginning of skin closure, the anesthetic agent (isoflurane or remifentanil) was discontinued and paracetamol (15 mg/kg) was administered. Although the intraoperative heart rate (HR) was lower in patients receiving remifentanil, the extubation time between the groups was similar.
Michel et al. reported their retrospective experience involving 65 infants presenting for abdominal surgery who received intraoperative anesthesia with endotracheal intubation and mechanical ventilation using sevoflurane and a remifentanil infusion [16]. The patients were separated into 3 groups—pre-term neonates (PTN, n = 21), full-term neonates (FTN, n = 24), and children aged <2 years (CUT, n = 20). The remifentanil infusion was initiated at 0.2 μg/kg/min and adjusted as needed. Neuromuscular blocking agents were not administered. There were no statistically significant differences between groups in length of anesthesia, surgery, duration of remifentanil infusion, and time between initiation of the remifentanil infusion and surgery. However, although not meeting statistical significance, the duration of surgery was 66.6 ± 43.4, 68.2 ± 45.0, and 109.0 ± 90.5 min in the PTN, FTN and CUT groups, respectively. The duration of anesthesia was likewise longer in the older age group (100.3 ± 50.2, 103.6 ± 34.0, and 144.7 ± 100.8 min, respectively). The authors reported that there was strong evidence for lower remifentanil-infused doses in the PTN and FTN groups than in the CUT group. The difference increased progressively with time as the dose requirements for remifentanil decreased during anesthesia in the PTN and FTN groups. In contrast, remifentanil dose requirements slowly increased during anesthesia in the CUT group. The longer duration surgery and the higher infusion requirements resulted in significantly higher total remifentanil requirements in the CUT group compared to the other two groups (17.7 ± 11.4, 19.7 ± 9.9, and 40.8 ± 37.7 μg/kg, respectively, p = 0.003). End-tidal sevoflurane concentrations were also higher in the CUT group than in the PTN and FTN groups.
When considering hemodynamic changes, there was no difference in HR and mean arterial pressure between the three groups. Episodes of hypotension occurred in 66.6 % of patients in the PTN group, 58.3 % in the FTN group, and 75.0 % in the CUT group. Despite the high incidence of hypotension, treatment was rarely required. Two neonates in the PTN group required treatment, one requiring 10 mL/kg of normal saline plus epinephrine (0.3 μg/kg/min) and the other requiring a normal saline bolus plus dopamine (15 μg/kg/min). In the FTN group, one neonate required normal saline and dopamine (10 μg/kg/min). For these 3 neonates, the vasoactive agent was discontinued within 4 h of tracheal extubation. No patient in the CUT group required treatment for hypotension. Bradycardia was noted (HR 96 beats/min) in one child in the PTN group; however, no therapy was required. The time from discontinuation of the remifentanil infusion to tracheal extubation was available for 26 patients of the study cohort. There was no difference among the 3 groups with mean times of 12.4, 10.5, and 10.0 min for the PTN, FTN and CUT groups, respectively. The authors concluded that “when administered along with sevoflurane, 0.25 μg/kg/min of remifentanil is effective and well-tolerated in neonates”.
Wee et al. prospectively evaluated an intraoperative anesthetic technique which involved the use of an intraoperative remifentanil infusion, isoflurane (0.5 %), and epidural anesthesia for major intra-abdominal procedures in 20 neonates aged <3 months [17]. There were 5 neonates aged <7 days (group A) and they were compared with 15 patients ranging in age from 7 days to 3 months (group B). Anesthesia was induced with intravenous thiopentone followed by endotracheal intubation facilitated by neuromuscular blockade using atracurium or vecuronium. Although, the initial study protocol included remifentanil (1 μg/kg bolus followed by an infusion rate of 1 μg/kg/min), this was adjusted down to 0.25 μg/kg/min without a bolus due to hypotension. The inspired concentration of isoflurane and the epidural infusion of ropivacaine were kept constant, while the remifentanil was titrated in the range of 0.05–0.25 μg/kg/min according to hemodynamic response. Isoflurane was discontinued at the beginning of skin closure and the remifentanil infusion was discontinued after the surgical dressing was applied. Despite a similar anesthesia time between the groups (166 vs 210 min), the time to eye opening (15 vs 4.2 min, p < 0.002) and tracheal extubation (21.2 vs 4.9 min, p < 0.002) were significantly longer in infants aged <7 days (group A) compared to those who were aged 7 days to 3 months (group B). Given the outcomes of previous studies showing rapid awakening with remifentanil even in neonates, the authors hypothesized that the longer recovery time was related to the prolonged effects of isoflurane or thiopentone.
A subsequent study evaluated the efficacy of remifentanil in providing analgesia during the tunneling phase of ventriculoperitoneal (VP) shunt insertion in pediatric patients including preterm neonates, term neonates, and infants [18]. Sixty-two pediatric patients including 8 ex-premature babies who were <60 weeks post-conceptual age, 13 neonates, 24 infants, and 25 children aged >1 year were anesthetized with 1 % isoflurane and nitrous oxide. They were randomized to receive remifentanil (1 μg/kg) (n = 33) or saline (n = 29) as a bolus over 1 min just prior to tunneling the VP shunt. In all age groups, there was a greater cardiovascular response and higher norepinephrine level in the saline group compared to the remifentanil group. However, the hemodynamic responses were not considered to be clinically important. Time to tracheal extubation, transfer to the recovery room, and discharge to the inpatient ward were similar between the remifentanil and the saline groups. The authors concluded that “remifentanil is safe and effective in this setting, in children of all ages”.
A final study regarding the intraoperative administration of remifentanil provides somewhat contradictory information to previous data demonstrating a lack of effect of remifentanil on postoperative respiratory function [19]. The study was influenced by their definition of apnea as a respiratory pause of >6 s. Bradycardia was defined as a HR <100 beats/min. The study cohort included 150 infants <60 weeks post-conceptual age (116 term and 34 preterm) undergoing herniorrhaphy. Anesthesia was induced with 6–8 % of sevoflurane and maintained with remifentanil infusion at 0.5 μg/kg/min with 60 % nitrous oxide. Postoperative apnea occurred in 31 infants (20.7 %), of whom 27 (18 %) had apnea in the recovery room and 4 (2.6 %) had apnea on the ward. In the 31 apneic patients, 5 (16.1 %) and 2 (6.4 %) had bradycardia in the recovery room and in the inpatient ward, respectively. Although the incidence of apnea (20.7 %) was high, paralleling that of other studies using volatile anesthetic agents, the authors’ definition of apnea was different (6 vs 20 s). Furthermore, apnea with bradycardia was uncommon, occurring in 6.4 % of patients. The authors recommended longer surveillance and monitoring in the recovery room and the inpatient ward or an ICU setting for infants at high risk of postoperative apnea.
Given its rapid metabolism, remifentanil’s major advantage over other synthetic opioids (fentanyl, sufentanil) lies in its ability to control the surgical stress response and provide intense analgesia during major surgical procedures and yet allow for early tracheal extubation. Although used most commonly during abdominal and thoracic procedures, its intense analgesic effects have led to it being used in combination with propofol as part of a total intravenous anesthetic technique for upper airway surgery using jet ventilation [20]. The caveat of such use is that given its rapid metabolism, some other form of analgesia (opioids or regional anesthesia) will be required during the immediate postoperative period. The studies to date reveal a limited risk of postoperative apnea or respiratory depression while intraoperative bradycardia and hypotension have been reported especially with higher doses and in preterm infants. These generally respond to decreasing the infusion rate or the administration of fluid. Given these effects, several other authors have reported anecdotal experience with the intraoperative administration of remifentanil in various clinical scenarios (Table 1) [21–32].
Procedural sedation
Advancements and developments in neonatal medicine have led to the survival of extremely premature infants, resulting in an increased number of these patients requiring invasive and non-invasive procedures. Although even preterm neonates have been shown to experience pain and react to painful stimuli therefore requiring analgesia for invasive procedures, healthcare providers may be reluctant to use opioids given their effects on respiratory function and the potential for post-procedural apnea. Given its rapid elimination, there may be a role for remifentanil in various painful procedures in this population.
Laser surgery for retinopathy of prematurity
One of the more common procedures required in this population is laser therapy to treat retinopathy of prematurity (ROP). Although many of these procedures are performed in the NICU to avoid transport-related risks such as hypothermia and hemodynamic instability, in many cases, endotracheal intubation and controlled ventilation are provided to eliminate the risks of apnea and hypoxemia. Sammartino et al. evaluated the efficacy of remifentanil infusion for 6 premature infants undergoing laser therapy in NICU for ROP [33]. The mean gestational age (GA) was 25.9 weeks, the mean post-conceptional age was 34.5 weeks, the mean birth weight was 640 g, and the mean weight at the time of surgery was 1,433 g. Prior to the start of the procedure, the trachea of the infants was intubated and ventilation provided using synchronized, intermittent mandatory ventilation. One hour prior to surgery, remifentanil infusion was initiated at 0.75–1 µg/kg/min and a bolus dose of midazolam (0.2 mg/kg) was administered. During the procedure, the infusion rate of the remifentanil infusion was increased quickly to 4 ± 2.1 µg/kg/min and then to a maximum dose of 10.3 ± 8.7 µg/kg/min as needed. In one patient, the dose was briefly (10 min) increased up to 20 µg/kg/min to control the hemodynamic response. The remifentanil infusion was discontinued at the end of surgery. Despite such high doses, the authors reported no adverse effect on hemodynamic function or concerns of chest wall rigidity. The minimum HR was 134.3 ± 3.4 beats/min with a minimum systolic blood pressure (sBP) of 83.6 ± 4.1 mmHg. There was a rapid postoperative recovery and return to baseline condition in all infants. The authors concluded that “a continuous infusion of remifentanil is efficient, reliable, and can be performed in the NICU, thus avoiding transportation of the preterm infants and minimizing the risk of hypothermia”.
A subsequent study revealed similar efficacy during laser therapy in neonates with ROP albeit with a much lower dose requirement [34]. The 64 neonates had a mean GA of 27.3 weeks and a post-conceptional age of 37.1 weeks. The mean body weight at birth and surgery were 965 and 1,913 g, respectively. After a bolus dose of midazolam (0.1 mg/kg), the tracheas were intubated and mechanical ventilation provided. During the procedure, remifentanil infusion was administered starting at 0.2 µg/kg/min and increased to 0.6 µg/kg/min to obtain to the desired level of anesthesia. The mean remifentanil infusion rate was 0.4 ± 0.1 µg/kg/min (range 0.2–0.6 µg/kg/min). Bradycardia and hypotension were noted in one patient each. Time to tracheal extubation was slightly longer in patients with a history of bronchopulmonary dysplasia (210 vs 151 min, p = 0.048). Although the patients with bronchopulmonary dysplasia had a longer time to tracheal extubation, there were no cases of extubation failure due to apnea or respiratory insufficiency.
Endotracheal intubation
Without effective analgesia, significant physiologic stress may occur including alterations in cerebral blood flow with the potential for intraventricular hemorrhage during endotracheal intubation. Using appropriate analgesia and sedation for endotracheal intubation can blunt not only the stress response, but facilitate the procedure thereby decreasing the time and difficulty of the procedure and reducing the potential for airway injury [35–37]. Remifentanil has been evaluated as a premedication for endotracheal intubation in both term and preterm neonates. These studies have evaluated the conditions for endotracheal intubation, the success rate, and the hemodynamic changes.
Badiee et al. prospectively evaluated the efficacy and safety of remifentanil as a premedication for elective endotracheal intubation in 40 preterm neonates with a GA of 25–37 weeks, comparing remifentanil to saline placebo [38]. Both groups received 10 µg/kg atropine followed by either 2 mL of normal saline or remifentanil (2 µg/kg over 2 min). Although they found that there was less pain in neonates who received remifentanil, there were no significant differences in the time for endotracheal intubation (20.8 ± 6 vs 22. 8 ± 7.3 s), the number of attempts for successful intubation, and oxygen desaturation between the two groups. They concluded that premedication with remifentanil had good analgesic effects for endotracheal intubation in premature infants with a stable hemodynamic pattern. Sixteen infants who received remifentanil had apnea for an average of 8.7 min and a maximum of 17 min. Although it did not occur in their study, they cautioned regarding the potential adverse effect of chest wall rigidity with remifentanil [39].
Crawford et al. performed a two-stage study using remifentanil for endotracheal intubation in neonates, comparing the dose–response in infants to children in a study that included 32 healthy infants (aged 2–12 months) and 32 children [40]. After the administration of glycopyrrolate (10 µg/kg) and propofol (4 mg), 1 of 4 doses of remifentanil (1.25, 1.50, 1.75, or 2.00 µg/kg) was administered to facilitate endotracheal intubation. Using logistic regression analysis, the ED50 and ED98 for remifentanil were 1.70 ± 0.1 and 2.88 ± 0.5 µg/kg, respectively. No difference was noted between neonates and children. In the second phase of their study, they noted no difference in the duration of apnea, conditions for endotracheal intubation, and hemodynamic changes when comparing propofol and succinylcholine (2 mg/kg) to propofol and remifentanil (3 µg/kg).
Other investigators have compared remifentanil with a combination of morphine and midazolam for endotracheal intubation [41]. The study population included 20 preterm neonates (GA 28–34 weeks) who required endotracheal intubation to treat respiratory failure due to respiratory distress syndrome (RDS). After preoxygenation with 100 % oxygen, midazolam (0.2 mg/kg) with either morphine 150 µg/kg (n = 10) or remifentanil 1 µg/kg (n = 10) was given over 1 min. Excellent conditions for endotracheal intubation condition were found in 6 patients who received remifentanil versus none in the morphine group (p = 0.0034). In the morphine group, 4 neonates required a second attempt at endotracheal intubation versus none in the remifentanil group. There were no significant differences between the groups regarding pain, stress levels and hemodynamic variables relating to endotracheal intubation. Avino et al. noted no significant differences when evaluating conditions for endotracheal intubation, changes of successful intubation on the first attempt, and time to successful intubation at the first attempt when comparing remifentanil (1 µg/kg) with a combination of morphine (100 µg/kg) and midazolam (50 µg/kg) [42]. Various other investigators have reported the use of remifentanil for endotracheal intubation (Table 2) [43–46]. In the majority of these studies, remifentanil was equivalent to or many times better than the comparison group. There were no adverse effects (hypotension or bradycardia) although atropine was administered prior to endotracheal intubation.
Tracheal intubation is also used for application of surfactant in the NICU. INSURE (intubate–surfactant–rapidly–extubate) is a procedure which combines endotracheal intubation for surfactant application followed by immediate or early extubation. For the procedure, optimal intubating conditions, adequate analgesia and sedation, maintenance of stable hemodynamic status, and a brief period of mechanical ventilation are essential. Welzing et al. evaluated intubating conditions, tracheal extubation times, and outcome in 21 preterm infants with moderate to severe respiratory distress receiving remifentanil as an induction agent for the INSURE procedure [47]. Atropine was followed by remifentanil (2 µg/kg) prior to endotracheal intubation. The conditions for endotracheal intubation were assessed as excellent or good in all cases. The average tracheal extubation time after surfactant administration was 16.9 min. The authors concluded “INSURE with remifentanil was associated with good intubating conditions and early extubation resulting in an excellent neonatal outcome”.
Placement of percutaneous intravenous central catheter
The other painful procedure that is performed on a daily basis in the NICU is percutaneous intravenous central catheter (PICC) placement. In a prospective trial, 54 preterm infants were randomly assigned to receive a low-dose remifentanil infusion (0.03 µg/kg/min) or placebo during PICC placement in addition to 0.3 mL of 12 % sucrose per os for non-nutritive sucking [48]. Eighteen of the 54 preterm infants were mechanically ventilated while the others were breathing spontaneously under nasal continuous positive airway pressure. Pain scores were lower in the remifentanil group. Although there was no difference in time to complete the procedure and the number of attempts, the cardiovascular and respiratory responses as well as body movements suggested improved analgesia with remifentanil. The authors concluded that low-dose remifentanil has a measurable analgesic effect in combination with non-nutritive sucking, but that it did not make PICC placement easier or quicker. A subsequent study in mechanically ventilated preterm infants suggested that although there were more respiratory events (apnea), a remifentanil infusion of 0.25 µg/kg/min was superior to 0.1 µg/kg/min for providing superior analgesia during PICC placement in preterm infants as assessed using the Premature Infant Pain Profile [49].
These preliminary trials demonstrate the potential use of remifentanil for procedural sedation. In addition to providing intense analgesia, the major pharmacokinetic advantage remains the short-half life and rapid recovery thereby allowing its effects to dissipate, resulting in the rapid return of spontaneous ventilation. Other anecdotal experience has also suggested that remifentanil may be used for radiologic imaging when brief periods of apnea are required to facilitate image acquisition and improve resolution such as computed tomography imaging of the lungs or intrathoracic vasculature [50]. For this scenario, ventilation can be assisted via an endotracheal tube or laryngeal mask airway as needed prior to and following image acquisition. With its rapid metabolism, the period of apnea will be limited thereby allowing the rapid return of spontaneous ventilation when the procedure is completed. Anecdotal experience also suggests its potential use as part of the sedation regimen during fiberoptic bronchoscopic examination of the upper and lower airway given the ability of opioids, including remifentanil, to blunt the cough reflex [51]. Regardless of the clinical scenario, given the potent respiratory depressant effects of all opioids especially in neonates, close monitoring of respiratory function is required with the consideration for control of ventilation in many scenarios.
Sedation during mechanical ventilation
Given its longer duration of action and the variation in its pharmacokinetics especially in preterm neonates, morphine may not be the ideal opioid for sedation of the preterm infant during mechanical ventilation [52, 53]. In a prospective trial, 20 premature neonates (GA 28–34 weeks) with RDS were randomized to receive either a continuous infusion of morphine or remifentanil during mechanical ventilation [54]. After terminating the infusion, the length of time until awakening and tracheal extubation was 18.9- and 12.1-fold longer in patients receiving morphine, respectively.
Similar efficacy was demonstrated in a prospective open-label trial using remifentanil infusion for 2–7 days for sedation during mechanical ventilation of 18 neonates with GA ≥32 weeks on mechanical ventilation [55]. The patients received a continuous infusion at a mean dose of 0.15 µg/kg/min for an average of 67 h. When compared with baseline, the HR decreased by approximately 20 %. After the infusion was discontinued, the mean time until tracheal extubation was 18 min. No adverse effects were noted.
In an effort to determine the minimal effective dose of remifentanil to provide sedation during mechanical ventilation, 48 preterm infants (average GA 28.5 weeks) requiring mechanical ventilation for respiratory failure were prospectively enrolled to receive remifentanil [56]. The remifentanil infusion was started at 0.075 µg/kg/min and increased as needed without bolus dosing. At 12 h after starting the remifentanil infusion, analgesia was adequate in 97 % of the patients with a dose of 0.094 ± 0.03 µg/kg/min. The time from discontinuation of remifentanil infusion to tracheal extubation was 36 ± 12 min despite a duration of 5.9 ± 5.7 days (range 1–20 days) of mechanical ventilation. The authors noted a short time to tracheal extubation after discontinuation of the remifentanil infusion despite an average of 5.9 days of mechanical ventilation. They also showed that the long-term infusion of remifentanil induces tolerance with the need to escalate the dose during prolonged infusions.
In a prospective, randomized trial, Welzing et al. compared remifentanil with fentanyl for sedation during mechanical ventilation in 23 neonates, ranging in age from 1−8 days [57]. Sedation was initiated with midazolam (50 µg/kg/h) and either remifentanil (9 µg/kg/h) or fentanyl (3 µg/kg/h). The opioid infusion was adjusted by 3 µg/kg/h of remifentanil or 1 µg/kg/h of fentanyl to achieve and maintain an adequate sedation level. The median time to tracheal extubation was significantly shorter in the remifentanil group (80.0 min, interquartile range [IQR] 15.0–165.0) compared to fentanyl (782.5 min, IQR 250.8–1,875.0, p = 0.005). When taken together, these 3 studies demonstrate not only the potential efficacy of remifentanil in providing sedation during mechanical ventilation, but also provide anecdotal proof of its primary advantage, i.e., rapid recovery with the potential for rapid tracheal extubation when the primary etiology of the respiratory failure has resolved.
Clinical concerns and adverse effects
Respiratory depression
As with any opioid, the primary concerns with the use of remifentanil include the potential for respiratory depression and hemodynamic effects. While not specifically demonstrated with remifentanil, for various developmental and physiologic reasons, neonates are more sensitive to the respiratory depressant effects of opioids [58, 59]. Remifentanil is a potent respiratory depressant with equivalent effects on respiratory function as other opioids when administered in equipotent doses. Although there are limited data in the neonatal population, the impact of remifentanil on respiratory function has been studied in the slightly older pediatric population [60, 61]. In a cohort of 32 children, ranging in age from 2−7 years, the apnea threshold was determined by slowing escalating the infusion rate of remifentanil during 1 % end-tidal sevoflurane in 60 % nitrous oxide [60]. The remifentanil infusion was started at 0.03 µg/kg/min after endotracheal intubation and increased every 10 min until the end-tidal CO2 was >70 mmHg, the oxygen saturation was <94 % with apnea of >5 s or the respiratory rate was <10 breaths/min. The median maximum infusion rate was 0.127 µg/kg/min (range 0.053–0.3 µg/kg/min) with the most frequent reason for discontinuing the infusion being apnea. In patients ranging in age from 6 months to 9 years, the respiratory depressant effects were less evident in those aged <3 years when compared to older patients [61]. The authors postulated that this was the result of a larger volume of distribution. Although it is not likely of clinical significance, the studies using remifentanil intraoperatively in neonates have demonstrated a slightly longer time to tracheal extubation in patients with a lower GA or the younger neonates [14–19]. Although remifentanil has a short context-sensitive half-life with rapid elimination even in neonates, especially premature neonates may still have a risk of respiratory depression postoperatively thereby suggesting that postoperative monitoring is necessary.
Hemodynamic effects
The hemodynamic responses to remifentanil (bradycardia and hypotension) are similar to those seen with other µ opioids. Despite fairly extensive experience in the neonatal population, there are limited concerns regarding significant hemodynamic effects that require anything more than decreasing the infusion rate or administering fluid. In one report, even with a relatively large bolus dose of 5 µg/kg, the decrease in HR and sBP averaged 9.0 beats/min and 12.1 % from baseline, respectively [12]. As the hemodynamic response to remifentanil is dose-dependent, the use of a large bolus dose or a high infusion rate should be avoided in patients with intravascular volume depletion or those with compromised myocardial function. Given its short context sensitive half-life, it can be effectively used intraoperatively by starting at a lower infusion rate and titrating up as needed [17, 62].
Chest wall rigidity
One adverse effect that is unique to the synthetic opioids when compared to other agents is chest wall/laryngeal rigidity [63]. The rigidity may be mediated in part by the modulation of gamma-aminobutyric acid pathways at the spinal cord and basal ganglia levels via fentanyl binding to μ1- and κ-opioid receptors [64]. Cerulospinal noradrenergic pathways have also been suggested to be involved [65]. Although chest wall rigidity occurs more commonly with large doses and rapid administration, it may occur with lower doses (0.5–1 µg/kg) even with gradual administration especially in neonates and infants [39]. Clinical manifestations may include coughing, hypoxemia with bradycardia, and difficult bag-valve-mask ventilation. While the end result is the same (inadequate ventilation with hypoxemia), the site of involvement remains controversial with ongoing debate as to whether this represents true chest wall/truncal rigidity or laryngeal involvement with rigidity and laryngospasm. In the studies reviewed using remifentanil as the sole premedication for neonatal endotracheal intubation, doses of 3, 2 and 1 µg/kg caused chest wall rigidity in 13 % (2/15), 10 % (4/40), and 6 % (2/36) of the cohorts, respectively [38, 42, 43]. However, other studies reported no such problems. Although chest wall rigidity can be treated with naloxone, should the inability to ventilation progress rapidly to hypoxemia, immediate airway management with endotracheal intubation may be necessary. As such the appropriate equipment and neuromuscular blocking agents should also be immediately available.
Hyperalgesia and tolerance
As remifentanil binds avidly to the µ-opioid receptor, clinical and animal studies have demonstrated the rapid development of tolerance with the need to increase the dose to achieve the desired level of analgesia [66–69]. In adults, the development of tolerance has been demonstrated after even brief infusions of <60–90 min, resulting in greater postoperative opioid requirements when remifentanil is used intraoperatively and the need to escalate doses rapidly when remifentanil is used for ICU sedation [67, 68]. To date, the majority of information regarding this phenomenon relates to patients outside of the neonatal period. Welzing et al. noted that during the administration of remifentanil infusion to 11 neonates for a median time of 71.7 h, the dose needed to be increased by 24 % to keep the infants adequately sedated during mechanical ventilation [70]. Although one neonate required methadone for withdrawal treatment, the authors concluded that remifentanil does not seem to be associated with an increased risk for withdrawal. However, the data remain sparse and more information is needed regarding this problem in the neonatal population.
Cost
Remifentanil-based anesthesia has been reported to be more expensive compared to other opioid-based anesthesia in the adult popuatlion [71, 72]. However, any cost analysis would need to consider not only acquisition cost of the medication, but also advantages regarding duration of mechanical ventilation, hospital stay, etc. To date, no such studies exist in the neonatal population. When simply comparing medication acquisition costs for the smallest available vials using data from August 2015 at our hospital (Nationwide Children’s Hospital, Columbus, OH, USA), remifentanil is the most expense with a cost of $45.52 for a 1,000 µg (1 mg). In comparison, morphine (2 mg) costs $1.69, fentanyl (100 µg) costs $0.92 and sufentanil (250 µg) costs $12.79.
Summary
Remifentanil has now been available for almost two decades in the United States as the newest of the synthetic opioid class. Because of the unique pharmacokinetic and pharmacodynamic profile including rapid onset, rapid metabolism and non-functional metabolite, remifentanil has found use in many clinical scenarios. Given its rapid metabolism, the major advantage of remifentanil lies in its ability to provide intense surgical anesthesia and control the stress response during major surgery, yet allow for rapid recovery. The pharmacokinetic principles are the same across all age ranges including neonates.
Although adverse hemodynamic effects are uncommon, high infusion rates or large bolus dosing should be avoided to prevent hemodynamic instability (bradycardia and hypotension) especially in preterm neonates, in the setting of intravascular volume depletion or in patients with compromised myocardial function. Should adverse hemodynamic effects occur, these are generally easily treated by the administration of fluid or decreasing the infusion rate. Following its introduction for intraoperative anesthesia, remifentanil has also found use in other clinical scenarios including sedation during endotracheal intubation, brief invasive procedures, or mechanical ventilation in the NICU.
References
Egan TD, Kern SE, Muir KT, White J. Remifentanil by bolus injection: a safety, pharmacokinetic, pharmacodynamic, and age effect investigation in human volunteers. Br J Anaesth. 2004;92:335–43.
Glass PS, Gan TJ, Howell S. A review of the pharmacokinetics and pharmacodynamics of remifentanil. Anesth Analg. 1999;89(4 Suppl):S7–14.
Gelberg J, Jonmarker C, Stenqvist O, Werner O. Intravenous boluses of fentanyl, 1 μg kg−1, and remifentanil, 0.5 μg kg−1, give similar maximum ventilatory depression in awake volunteers. Br J Anaesth. 2012;108:1028–34.
Hoke JF, Cunningham F, James MK, Muir KT, Hoffman WE. Comparative pharmacokinetics and pharmacodynamics of remifentanil, its principle metabolite (GR90291) and alfentanil in dogs. J Pharmacol Exp Ther. 1997;281:226–32.
Davis PJ, Stiller RL, Wilson AS, McGowan FX, Egan TD, Muir KT. In vitro remifentanil metabolism: the effects of whole blood constituents and plasma butyrylcholinesterase. Anesth Analg. 2002;95:1305–7.
Kapila A, Glass PS, Jacobs JR, Muir KT, Hermann DJ, Shiraishi M, Howell S, Smith RL. Measured context-sensitive half-times of remifentanil and alfentanil. Anesthesiology. 1995;83:968–75.
Egan TD, Minto CF, Hermann DJ, Barr J, Muir KT, Shafer SL. Remifentanil versus alfentanil. Comparative pharmacokinetics and pharmacodynamics in healthy adult male volunteers. Anesthesiology. 1996;84:821–33.
Welzing L, Roth B. Experience with remifentanil in neonates and infants. Drugs. 2006;66:1339–50.
Dershwitz M, Hoke JF, Rosow CE, Michałowski P, Connors PM, Muir KT, Dienstag JL. Pharmacokinetics and pharmacodynamics of remifentanil in volunteer subjects with severe liver disease. Anesthesiology. 1996;84:812–20.
Hoke JF, Shlugman D, Dershwitz M, Michałowski P, Malthouse-Dufore S, Connors PM, Martel D, Rosow CE, Muir KT, Rubin N, Glass PS. Pharmacokinetics and pharmacodynamics of remifentanil in persons with renal failure compared with healthy volunteers. Anesthesiology. 1997;87:533–41.
Kapila A, Glass PS, Jacobs JR, Muir KT, Hermann DJ, Shiraishi M, Howell S, Smith RL. Measured context-sensitive half-times of remifentanil and alfentanil. Anesthesiology. 1995;83:968–75.
Ross AK, Davis PJ. Dear Gd GL, Ginsberg B, McGowan FX, Stiller RD, Henson LG, Huffman C, Muir KT. Pharmacokinetics of remifentanil in anesthetized pediatric patients undergoing elective surgery or diagnostic procedures. Anesth Analg. 2001;93:1393–401.
Davis PJ, Galinkin J, McGowan FX, Lynn AM, Yaster M, Rabb MF, Krane EJ, Kurth CD, Blum RH, Maxwell L, Orr R, Szmuk P, Hechtman D, Edwards S, Henson LG. A randomized multicenter study of remifentanil compared with halothane in neonates and infants undergoing pyloromyotomy. I. Emergence and recovery profiles. Anesth Analg 2001;93:1380–6.
Lynn AM, Rabb MF, Yaster M, Henson LG, Blum R, Hechtman D, Maxwell L, Szmuk P, Orr R, Krane EJ, Edwards S, Kurth CD. A randomized multicenter study of remifentanil compared with halothane in neonates and infants undergoing pyloromyotomy. II. Perioperative breathing patterns in neonates and infants with pyloric stenosis. Anesth Analg. 2001;93:1387–92.
Ben Khalifa S, Blidi S, Trifa M, Skhiri A, Drira M, Regaya T, Fekih Hassen A. Time to extubation in infants undergoing pyloromyotomy—isoflurane inhalation vs remifentanil infusion. Middle East J Anaesthesiol 2009;20:277-80.
Michel F, Lando A, Aubry C, Arnaud S, Merrot T, Martin C. Experience with remifentanil-sevoflurane balanced anesthesia for abdominal surgery in neonates and children less than 2 years. Paediatr Anaesth. 2008;18:532–8.
Wee LH, Moriarty A, Cranston A, Bagshaw O. Remifentanil infusion for major abdominal surgery in small infants. Paediatr Anaesth. 1999;9:415–8.
Chambers N, Lopez T, Thomas J, James MF. Remifentanil and the tunnelling phase of paediatric ventriculoperitoneal shunt insertion. A double-blind, randomised, prospective study. Anaesthesia. 2002;57:133–9.
Gharavi-Fard M, Taghavi-Gilani M, Kazemi S, Razavi M. Apneas in infants with postconceptional age below 60 weeks undergoing herniorrhaphy. Iran J Pediatr. 2014;24:179–83.
Mausser G, Friedrich G, Schwarz G. Airway management and anesthesia in neonates, infants and children during endolaryngotracheal surgery. Paediatr Anaesth. 2007;17:942–7.
Eck JB, Lynn AM. Use of remifentanil in infants. Paediatr Anaesth. 1998;8:437–9.
Wee L, Stokes MA. Bladder exstrophy in a neonate at risk of transient myasthenia gravis: a role for remifentanil and epidural analgesia. Br J Anaesth. 1999;82:774–6.
Sommer M, Riedel J, Fusch C, Fetsge PA, Hachenberg T. Intravenous anaesthesia with remifentanil in a preterm infant. Paediatr Anaesth. 2001;2:252–4.
Fernández A, Jerez A, Falcone N. Anaesthetic management in a case of a type IV laryngotracheo-oesophageal cleft. Paediatr Anaesth. 2003;13:270–3.
Krosnar S, Baxter A. Thoracoscopic repair of esophageal atresia with tracheoesophageal fistula: anesthetic and intensive care management of a series of eight neonates. Paediatr Anaesth. 2005;15:541–6.
Koomen E, Poortmans G, Anderson BJ, Janssens MM. Jet ventilation for laryngotracheal surgery in an ex-premature infant. Paediatr Anaesth. 2005;15:786–9.
Guruswamy V, Roberts S, Arnold P, Potter F. Anaesthetic management of a neonate with congenital cyst adenoid malformation. Br J Anaesth. 2005;95:240–2.
Gerçek A, Dagcinar A, Ozek MM. Anesthetic management of a newborn with Mohr (oro-facial-digital type II) syndrome. Paediatr Anaesth. 2007;17:603–4.
Arai LR, Dicindio S, Cook SP, Davis DA. Anesthesia management of a patient with a laryngotracheo-esophageal cleft. Paediatr Anaesth. 2007;17:171–5.
Pickard A, Chen J. Petty syndrome–implications for anesthesia. Paediatr Anaesth. 2011;21:1274–6.
Sammartino M, Garra R, Sbaraglia F, De Riso M, Continolo N, Papacci P. Experience of remifentanil in extremely low-birth-weight babies undergoing laparotomy. Pediatr Neonatol. 2011;52:176–9.
Kim BR, Kim JH, Kim KW, Choe WJ, Park JS. Anesthetic management of a preterm neonate intracranial aneurysm clipping. Korean J Anesth. 2014;67:S85–6.
Sammartino M, Bocci MG, Ferro G, Mercurio G, Papacci P, Conti G, Lepore D, Molle F. Efficacy and safety of continuous intravenous infusion of remifentanil in preterm infants undergoing laser therapy in retinopathy of prematurity: clinical experience. Paediatr Anaesth. 2003;13:596–602.
Demirel N, Bas AY, Kavurt S, Celik IH, Yucel H, Turkbay D, Hekimoğlu E, Koc O. Remifentanil analgesia during laser treatment for retinopathy of prematurity: a practical approach in neonatal intensive care unit. Am J Perinatol. 2014;31:983–6.
Shah V, Ohlesson A. The effectiveness of premedication for endotracheal intubation in mechanically ventilated neonates: a systematic review. Clin Perinatol. 2002;29:535–54.
Aranda JV, Carlo W, Hummel P, Thomas R, Lehr VT, Anand KJ. Analgesia and sedation during mechanical ventilation in neonates. Clin Ther. 2005;27:877–99.
Cook-Sather SD, Tulloch HV, Cnaan A, Nicolson SC, Cubina ML, Gallagher PR, Schreiner MS. A comparison of awake versus paralyzed tracheal intubation for infants with pyloric stenosis. Anesth Analg. 1998;86:945–51.
Badiee Z, Vakiliamini M, Mohammadizadeh M. Remifentanil for endotracheal intubation in premature infants: A randomized controlled trial. J Res Pharm Pract. 2013;2:75–82.
Dewhirst E, Naguib A, Tobias JD. Chest wall rigidity in two infants after low-dose fentanyl administration. Pediatr Emerg Care. 2012;28:465–8.
Crawford MW, Hayes J, Tan JM. Dose-response of remifentanil for tracheal intubation in infants. Anesth Analg. 2005;100:1599–604.
Pereira e Silva Y, Gomez RS, Marcatto Jde O, Maximo TA, Barbosa RF, Simões e Silva AC. Morphine versus remifentanil for intubating preterm neonates. Arch Dis Child Fetal Neonatal Ed 2007;92:F293-4.
Avino D, Zhang WH, De Villé A, Johansson AB. Remifentanil versus morphine-midazolam premedication on the quality of endotracheal intubation in neonates: a noninferiority randomized trial. J Pediatr. 2014;164:1032–7.
Choong K, Al Faleh K, Doucette J, Gray S, Rich B, Verhey L, Paes B. Remifentanil for endotracheal intubation in neonates: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 2010;95:F80–4.
Penido MG, Oliveira Silva DF, Tavares EC, Silva YP. Propofol versus midazolam for intubating preterm neonates: a randomized controlled trial. J Perinatol. 2011;31:356–60.
Norman E, Wikström S, Hellström-Westas L, Turpeinen U, Hämäläinen E, Fellman V. Rapid sequence induction is superior to morphine for intubation of preterm infants: a randomized controlled trial. J Pediatr. 2011;159:893–9.
Norman E, Wikström S, Rosén I, Fellman V, Hellström-Westas L. Premedication for intubation with morphine causes prolonged depression of electrocortical background activity in preterm infants. Pediatr Res. 2013;73:87–94.
Welzing L, Kribs A, Huenseler C, Eifinger F, Mehler K, Roth B. Remifentanil for INSURE in preterm infants: a pilot study for evaluation of efficacy and safety aspects. Acta Paediatr. 2009;98:1416–20.
Lago P, Tiozzo C, Boccuzzo G, Allegro A, Zacchello F. Remifentanil for percutaneous intravenous central catheter placement in preterm infant: a randomized controlled trial. Paediatr Anaesth. 2008;18:736–44.
Shin SH, Kim HS, Lee J, Choi KY, Lee JH, Kim EK, Park MS, Choi JH. A comparative study of two remifentanil doses for procedural pain in ventilated preterm infants: a randomized, controlled study. Pediatr Crit Care Med 2014;15-5.
Joshi G, Tobias JD. Remifentanil to facilitate high-resolution computed tomography imaging of the chest or magnetic resonance imaging in infants. South Med J. 2009;102:1121.
Berkenbosch JW, Graff GR, Stark JM, Ner Z, Tobias JD. Use of a remifentanil-propofol mixture for pediatric flexible fiberoptic bronchoscopy sedation. Paediatr Anaesth. 2004;14:941–6.
Pereira e Silva Y, Gomez RS, Barbosa RF, Simões e Silva AC. Remifentanil for sedation and analgesia in a preterm neonate with respiratory distress syndrome. Paediatr Anaesth 2005;15:993–6.
Tobias JD. Remifentanil: Applications in the Pediatric ICU population. Amer J Pain Manage. 1998;8:114–7.
Pereirae Silva YP, Gomez RS, Marcatto J de O, Maximo TA, Barbosa RF, eSilva AC. Early awakening and extubation with remifentanil in ventilated premature neonates. Paediatr Anaesth 2008;18:176–83.
Stoppa F, Perrotta D, Tomasello C, Cecchetti C, Marano M, Pasotti E, Barbieri MA, Conti G, Pirozzi N. Low dose remifentanyl infusion for analgesia and sedation in ventilated newborns. Minerva Anestesiol. 2004;70:753–61.
Giannantonio C, Sammartino M, Valente E, Cota F, Fioretti M, Papacci P. Remifentanil analgosedation in preterm newborns during mechanical ventilation. Acta Paediatr. 2009;98:1111–5.
Welzing L, Oberthuer A, Junghaenel S, Harnischmacher U, Stützer H, Roth B. Remifentanil/midazolam versus fentanyl/midazolam for analgesia and sedation of mechanically ventilated neonates and young infants: a randomized controlled trial. Intensive Care Med. 2012;38:1017–24.
Howard RF, Lloyd-Thomas A, Thomas M, Williams DG, Saul R, Bruce E, Peters J. Nurse-controlled analgesia (NCA) following major surgery in 10,000 patients in a children’s hospital. Paediatr Anaesth. 2010;20:126–34.
Morton NS, Errera A. APA national audit of pediatric opioid infusions. Paediatr Anaesth. 2010;20:119–25.
Ansermino JM, Brooks P, Rosen D, Vandebeek CA, Reichert C. Spontaneous ventilation with remifentanil in children. Paediatr Anaesth. 2005;15:115–21.
Barker N, Lim J, Amari E, Malherbe S, Ansermino JM. Relationship between age and spontaneous ventilation during intravenous anesthesia in children. Paediatr Anaesth. 2007;17:948–55.
Weale NK, Rogers CA, Cooper R, Nolan J, Wolf AR. Effect of remifentanil infusion rate on stress response to the pre-bypass phase of paediatric cardiac surgery. Br J Anaesth 200;92:187–94.
Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia. 2007;62:1266–80.
Ellenbroek B, Schwarz M, Sontag KH, Jaspers R, Cools A. Muscular rigidity and delineation of a dopamine-specific neostriatal subregion: tonic EMG activity in rats. Brain Res. 1985;345:132–40.
Lui PW, Lee TY, Chan SH. The possible mechanism of fentanyl-induced muscle rigidity. Ma Zui Xue Za Zhi. 1991;29:542–7.
Anand KJ, Willson DF, Berger J, Harrison R, Meert KL, Zimmerman J, Carcillo J, Newth CJ, Prodhan P, Dean JM, Nicholson C. Tolerance and withdrawal from prolonged opioid use in critically ill children. Pediatrics. 2010;125:e1208–25.
Guignard B, Bossard AE, Coste C, Sessler DI, Lebrault C, Alfonsi P, Fletcher D, Chauvin M. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000;93:409–17.
Vinik HR, Kissin I. Rapid development of tolerance to analgesia during remifentanil infusion in humans. Anesth Analg. 1998;86:1307–11.
Crawford MW, Hickey C, Zaarour C, Howard A, Naser B. Development of acute opioid tolerance during infusion of remifentanil for pediatric scoliosis surgery. Anesth Analg. 2006;102:1662–7.
Welzing L, Link F, Junghaenel S, Oberthuer A, Harnischmacher U, Stuetzer H, Roth B. Remifentanil-induced tolerance, withdrawal or hyperalgesia in infants: a randomized controlled trial. RAPIP trial: remifentanil-based analgesia and sedation of paediatric intensive care patients. Neonatology. 2013;104:34–41.
Loop T, Priebe HJ. Prospective, randomized cost analysis of anesthesia with remifentanil combined with propofol, desflurane or sevoflurane for otorhinolaryngeal surgery. Acta Anaesthesiol Scand. 2002;46:1251–60.
Beers RA, Calimlim JR, Uddoh E, Esposito BF, Camporesi EM. A comparison of the cost-effectiveness of remifentanil versus fentanyl as an adjuvant to general anesthesia for outpatient gynecologic surgery. Anesth Analg. 2000;91:1420–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This review was not sponsored, and there are no conflicts of interests known at the time of submission.
About this article
Cite this article
Kamata, M., Tobias, J.D. Remifentanil: applications in neonates. J Anesth 30, 449–460 (2016). https://doi.org/10.1007/s00540-015-2134-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-015-2134-5