Abstract
Functional imaging methods, including positron emission tomography (PET) and functional magnetic resonance imaging (fMRI), have become important tools for studying how anesthetic drugs act in the human brain to induce the state of general anesthesia. Recent imaging studies using fMRI and PET techniques have demonstrated the regional effects of propofol on the brain. However, the pharmacological mechanism of the action of propofol in the intact human central nervous system is unclear. To explore the possible action targets of propofol in the human brain, a systematic review of the literature was performed. The literature search was performed with limiting factors of “propofol,” “functional imaging,” “positron emission tomography”, and “functional magnetic resonance imaging” from 1966 to July 2013 (using Medline, EMBASE, CINAHL and hand searches of references). Studies meeting the inclusion criteria were reviewed and critiqued for the purpose of this literature research. Eighteen researches meeting the inclusion criteria were reviewed in terms of the appropriateness of valuation technique. In the unconscious state, propofol sharply reduces the regional glucose metabolism rate (rGMR) and regional cerebral blood flow (rCBF) in all brain regions, particularly in the thalamus. However, GMR, such as in the occipital, temporal, and frontal lobes, was obviously decreased at a sedative dosage of propofol, whereas, changes in the thalamus were not obvious. Using fMRI, several studies observed a decrease of connectivity of the thalamus versus an increase of connectivity within the pons of the brainstem during propofol-induced mild sedation. During deep sedation, propofol preserves cortical sensory reactivity, the specific thalamocortical network is moderately affected, whereas the nonspecific thalamocortical network is severely suppressed. In contrast, several recent fMRI studies are consistent on the systemic decreased effects of propofol in the frontoparietal network. Accumulating evidence suggest that propofol-induced unconsciousness is associated with a global metabolic and vascular depression in the human brain and especially with a significant reduction in the thalamocortical network and the frontoparietal network.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional imaging methods are a comprehensive, non-invasive diagnostic imaging technique. To show in vivo biochemical, metabolic, and functional changes, these methods can be used combined with more traditional anatomical imaging techniques [1]. These methods, including positron emission tomography (PET) and functional magnetic resonance imaging (fMRI), have become important tools for studying how to induce the state of general anesthesia for anesthetic drugs acting in the human brain [2]. Using PET first and fMRI thereafter, recent imaging studies have demonstrated regional effects of many anesthetic agents on the brain. Using PET, researchers measured propofol-induced changes in regional glucose metabolism rate (rGMR) [3–6] and regional cerebral blood flow (rCBF) [6–10]. fMRI studies have taken the alternative approach of measurement of changes in stimulus-induced activity within specific sensory or cognitive systems during general anesthesia [11–18].
Propofol is a potent intravenous anaesthetic agent with a rapid onset and a short duration of action. It is widely used both for induction and maintenance of anaesthesia, as well as for sedation in the intensive care unit [19]. Despite the prevalence of its use, the fundamental question of what is the functional target of propofol in the human brain remains unanswered. Previous studies have been mainly focused on molecular and cellular targets of propofol. It is now well accepted that propofol produces its hypnotic effects by a positive modulation of the inhibitory function of the neurotransmitter GABA through GABAA receptors, and via presynaptic mechanisms of GABAergic transmission [20, 21]. However, in the intact central nervous system, especially in human beings during anesthesia, the pharmacological mechanism of propofol in the brain is still a mystery. Whether it acts on the cortex or thalamus is still controversial [22].
The objective of this paper was to provide a review on anesthetic effects of propofol in the brain revealed by functional imaging, to present an inventory of current researches, and to suggest the directions for future research.
Materials and methods
Search criteria
Relevant literature search was performed using the most common database of medical literature as shown below:
Medline (Through Pubmed; 1966 to July 2013),
EMBASE (1980–2013 week 21),
and CINAHL (1982 to July week 1 2013).
The search was performed with limiting factors of “propofol,” “functional imaging,” “positron emission tomography”, and “functional magnetic resonance imaging”. Some papers and the reference lists of articles selected for review were found by manual methods. Additional literature identified from these references that contained relevant supporting information were then included.
Inclusion/exclusion criteria
After excluding identical papers, we carried out a selection of peer-reviewed articles to include in our study. The selected articles were to meet the following criteria:
-
The papers that focused on anesthetic effects of propofol in the brain revealed by functional imaging were selected.
-
All subjects in the selected articles were healthy right-handed adult volunteers.
-
In the selected articles, only propofol in different concentration was given by intravenous infusion.
-
The letters to the editor, the papers contained no primary data, or the single case reports or abstracts were excluded.
Results
After a screening of abstracts, eighteen articles underwent further analysis. There were two reports published before 2000, five papers published between 2000 and 2009, and nine papers in the 2010s. There were four papers mainly focused on propofol-induced changes in rCBF, five studies on propofol-induced changes in rGMR, and seven articles on anesthetic effects of propofol in the brain revealed by fMRI.
Propofol-induced changes on rGMR and rCBF
There were four and five studies focused on propofol-induced changes in rGMR [3–6] and rCBF [6–10], respectively. Most of their data were similar, the detailed data and the different data were listed in Tables 1 and 2, separately.
In the unconscious state, propofol sharply reduces rGMR and rCBF in all brain regions, particularly in the thalamus. GMR, such as occipital, temporal and frontal lobe, was obviously decreased at a sedative dosage of propofol. However, changes in the thalamus were not obvious.
Anesthetic effects of propofol in the brain revealed by fMRI
There were eight studies focused on propofol-induced changes using fMRI: Mhuircheartaigh et al. [11], Boveroux et al. [12], Zhang et al. [13], Stamatakis et al. [14], Schrouff et al. [15], Schröter et al. [16], Liu et al. [17], and Gili et al. [18]. The most detailed data and the different data are listed in Table 3.
Several studies have observed both preservation and alteration of corticocortical connectivity during sedation and anesthesia. Some researchers reported a decrease of connectivity of the thalamus versus an increase of connectivity within the pons of the brainstem during propofol-induced mild sedation. During deep sedation, propofol preserves cortical sensory reactivity, the specific thalamocortical network is moderately affected, and the nonspecific thalamocortical network is severely suppressed. In contrast, several recent fMRI studies are consistent on the effect of propofol that having systemic decreases in the frontoparietal network.
Discussion
Since the pioneering work of Jasper [23] and Moruzzi [24], the thalamus and the brainstem reticular formation have been known to play a critical role in the regulation of consciousness levels. In particular, GABAergic cells of the reticular thalamic nucleus seem to control bursting activity of the thalamocortical neurons and, in turn, to modulate cortical activity [25]. Therefore, most previous studies on the effects of propofol on the human central nervous system have identified the thalamus as a key target.
Anesthetic effects of propofol in the brain revealed by PET
PET is based on the intravenous administration of molecules that are labeled by positron-emitting isotopes. It is a novel method capable of producing quantitative high-resolution data from the whole brain and enables three-dimensional (3D) metabolic and flow studies in the living human brain [26]. Depending on the administered molecule and according to changes in brain state, PET measures rCBF distribution across the brain (15O labeled water), glucose uptake (18F labeled glucose), and neurotransmission system activities [27]. Neuronal activation in the brain is assumed to be coupled by parallel changes in rGMR and rCBF [28].
Propofol-induced changes on rGMR
Recent evidence suggest that rGMR more directly reflects fluctuating neuronal activity than the regional oxygen consumption during local activation [28]. Many studies focused on rGMR with PET to measure propofol-induced changes.
In the unconscious state, propofol markedly reduced GMR in all brain regions [3–6]. Cerebral glucose metabolism in the thalamus, cerebral cortex, hippocampus, and cerebrum was decreased, particularly in the thalamus [5], indicating that the thalamus might be the target region for propofol to induce unconsciousness [5, 6]. However, cortical glucose metabolism, such as in the occipital lobe, temporal lobe, and frontal lobe, was obviously reduced at a sedative dosage of propofol, but changes in subcortical regions like the thalamus were not obvious [5]. Based on the data, it may be deduced that the sedative function of propofol is probably induced by direct inhibition of the higher central cortical neurons that control consciousness and mental actions rather than inhibition of the ascending reticular activating system.
Moreover, it is well-known that the hippocampus and cingulate gyrus are important structures of the limbic system that are involved in autonomic nervous system regulation of the visceral, cardiovascular, and endocrine systems [29]. Under the propofol-induced unconsciousness state, the reduced blood pressure and respiratory rate found in the present study might be related to neuronal actions in the hippocampus region and cingulated gyrus.
Propofol-induced changes on rCBF
As blood flow and neuronal activity are tightly coupled under normal conditions, changes in blood flow are accurate markers of changes in activity. In addition to a generalized decrease in global CBF induced by propofol [6–10, 26], an important contribution of the early studies was to reveal that propofol-induced unconsciousness is consistently associated with a reduction in the medial thalamus, orbitofrontal region, and the medial parietoocciptal cortex, including the cuneus and precuneus, and the posterior cingulate, and right angular gyri [7, 8, 26, 30]. Moreover, there was a strong negative correlation between rCBF in the medial thalamus and propofol concentration. The changes in CBF are linked to the specific effects of propofol on neuronal activity and are not the result of a nonspecific regional effect on CNS vasculature [7].
Propofol may influence neurovascular coupling. Although propofol has depressive effects on respiration during anesthesia, it has been shown that autoregulation of cerebral vasculature is intact at sedative concentrations [7], and the drug does not appear to affect the regional cerebral blood flow response to brain activity [10].
The results provide strong evidence that reductions in rCBF in the thalamus is functionally related to propofol-induced unconsciousness independently of non-specific effects of propofol. These observations confirm that the thalamus is a key element in understanding how propofol causes unconsciousness and how patients wake up from anaesthesia. Furthermore, they are consistent with the notion that propofol-induced unconsciousness is associated with reduced cholinergic activation [31].
Anesthetic effects of propofol in the brain revealed by fMRI
The fMRI provides an effective nontraumatic method for observing the structural and functional changes of the human brain [32]. Compared with PET, the advantages of fMRI are more excellent in temporal and spatial resolution [33]. One scan could get the anatomical and functional image in fMRI without the need for tracer agents or exposure to radiation [34].
In recent years, increasing attention has been paid to coherent spontaneous blood-oxygen-level-dependent (BOLD) in the low frequency range as observed by fMRI. A BOLD signal change is based on hemodynamic changes in the CNS, which is a direct consequence of alterations in neuronal activity [35]. Intrinsic brain activity, as reflected in spontaneous slow fluctuations in BOLD signals in fMRI, has been proposed to provide important clues about brain organization [36] and mapping of its spatiotemporal correlation structure. It seems a promising approach to assess basic properties of brain function [37]. To date, more and more researches have revealed the effects of anesthesia on BOLD signal response to chemical or sensory stimulation.
Thalamus as a “switch” or “read-out” of propofol-induced unconsciousness
Is thalamus a “switch” or a “read-out” of propofol-induced unconsciousness [21, 38]? In recent years, the thalamic “switch” hypothesis was based on human neuroimaging studies, which identified thalamic depression as a common feature of intravenous anesthesia [7]. In contrast, some studies demonstrated the cortex was the site mediating anesthetic-induced unconsciousness. Therefore, a subsequent depression of the thalamus might reflect a “read-out” of diminished cortical activity [39]. In the literature, there is still a debate on the question whether anesthesia-induced hypnosis results primarily from the action on the thalamus [16, 17, 40, 41] or on the cortex [11–16, 39]. Several studies have observed both preservation and alteration of cortico-cortical connectivity during sedation and unconsciousness. However, results may depend on the agent studied and the degree of sedation. Propofol has many interesting properties for its effects varying as a function of concentration [21]. These properties will be described at length in a later paper.
The thalamus and propofol-induced unconsciousness
The most consistent regional effect produced by propofol at loss of consciousness is a reduction of thalamic metabolism and blood flow. In a previous study using PET imaging, the researchers observed in the subcortical regions that the decrease of rGMR was greatest in the thalamus [5]. Therefore, several authors have proposed that thalamic activity could act as a consciousness switch, allowing cortical arousal [40]. Revealed by fMRI, Gili and coworkers [18] observed a decrease of connectivity of the thalamus versus an increase of connectivity within the pons of the brainstem during propofol-induced mild sedation. Specifically, the thalamus is out of touch with a widespread set of cortical and subcortical regions, and then the thalamus centrality decreases. Consistent with their observations of thalamic functional disconnection from a wide range of cortical and subcortical areas and with electrophysiological measurements [40], a functional disconnection between structurally distinct cortical regions and the thalamus has been suggested to be the cause of anesthesia-induced hypnosis [41].
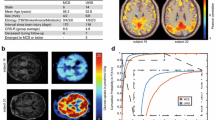
Recently, Liu et al. [17] unlocked the vault of the thalamus by fMRI to differentiate the role of specific and nonspecific thalamocortical systems in propofol-induced unconsciousness. The thalamocortical system is a bilateral structure and has two thalamic nuclei, the specific and nonspecific divisions, and they may play the roles of mediating the relay of peripheral information to a particular area of sensory cortex and mediating multimodal integration of information, respectively [38]. The thalamocortical connectivity at baseline was dominantly medial and bilateral frontal and temporal for the specific system, and it was medial frontal and medial parietal for the nonspecific system. However, during loss of consciousness, propofol preserves cortical sensory reactivity [42]. The specific thalamocortical network is moderately affected, while the nonspecific thalamocortical network is severely suppressed and subsequently reactivated after recovery of consciousness (Fig. 1).
The center median-parafascicular complex is made up of the centromedian and the parafascicolar. It is the important component group in the thalamus intralaminar lamina. It was used as a seed to calculate nonspecific thalamocortical connectivity. The rest of the thalamus was used as a seed for calculating specific thalamocortical connectivity
The cortex connectivity and propofol-induced unconsciousness
Are some cortical areas more significant than the thalamus for propofol-induced unconsciousness? Propofol has traditionally been considered to decrease activity in a widespread bilateral frontoparietal brain structures [13, 22]. Several recent fMRI researchers are consistent about the effect of propofol decreasing systemically in subcorticocortical and corticocortical connectivity [11–16]. Regionally, the connectivity of the thalamus [16], putamen [11, 16], posterior cingulate [14], hypothalamus [13], and several multimodal associative and sensory cortices are also reduced (Fig. 2).
Propofol and consciousness networks
It is worth mentioning that the definition of “intrinsic connectivity networks” [43] brings about a further step to comprehend the possible action targets of propofol anesthesia. These networks consist of the medial frontoparietal default mode network (DMN) [44], the dorsolateral frontoparietal executive control network (ECN) [45], and the visual and auditory networks [46]. They are higher-order information processing networks to support the emergence of mental content and of the inner self [27].
In recent years, several fMRI studies have suggested that propofol disturbs cerebral connectivity and stereotypical patterns of brain responses [22]. During deep sedation, propofol largely and significantly reduces but does not abolish corticocortical and thalamocortical connectivity in frontoparietal segregation (DMN and ECN) in large-scale brain networks [12, 15] (Fig. 1). These findings showed that coherent integration among frontoparietal cortices is important in the generation of conscious perception [15, 47, 48]. Furthermore, when propofol produces loss of consciousness, a negative correlation was identified between thalamic and cortical activity in these networks. In contrast, connectivity was globally preserved in low-level sensory cortices (visual and auditory networks) [12, 15, 16].
Conclusion
Functional imaging studies have provided essential progress for exploring propofol-altered consciousness. Propofol and the state of unconsciousness is associated with a significant reduction on rCBF and rGMR in most cortical areas and the thalamus. It decreases the activity of the nonspecific thalamocortical network or the most frontoparietal network. Nevertheless, although much published data has accumulated about the effective role of consciousness networks in the emergence of the conscious experience, supplementary evidence should still be required to further verify other mechanisms of propofol-altered consciousness.
References
Ziegler SI. Positron emission tomography: principles, technology, and recent developments. Nucl Phys A. 2005;752:679–87.
Purdon PL, Pierce ET, Bonmassar G, Walsh J, Harrell PG, Kwo J, Deschler D, Barlow M, Merhar RC, Lamus C, Mullaly CM, Sullivan M, Maginnis S, Skoniecki D, Higgins HA, Brown EN. Simultaneous electroencephalography and functional magnetic resonance imaging of general anesthesia. Ann N Y Acad Sci. 2009;1157:61–70.
Alkire MT, Haier RJ, Barker SJ, Shah NK, Wu JC, Kao YJ. Cerebral metabolism during propofol anesthesia in humans studied with positron emission tomography. Anesthesiology. 1995;82:393–403.
Jeong YB, Kim JS, Jeong SM, Park JW, Choi IC. Comparison of the effects of sevoflurane and propofol anaesthesia on regional cerebral glucose metabolism in humans using positron emission tomography. J Int Med Res. 2006;34:374–84.
Sun X, Zhang H, Gao C, Zhang G, Xu L, Lv M, Chai W. Imaging the effects of propofol on human cerebral glucose metabolism using positron emission tomography. J Int Med Res. 2008;36:1305–10.
Schlünzen L, Juul N, Hansen KV, Cold GE. Regional cerebral blood flow and glucose metabolism during propofol anaesthesia in healthy subjects studied with positron emission tomography. Acta Anaesthesiol Scand. 2012;56:248–55.
Fiset P, Paus T, Daloze T, Plourde G, Meuret P, Bonhomme V, Hajj-Ali N, Backman SB, Evans AC. Brain mechanisms of propofol-induced loss of consciousness in humans: a positron emission tomographic study. J Neurosci. 1999;19:5506–13.
Bonhomme V, Fiset P, Meuret P, Backman S, Plourde G, Paus T, Bushnell MC, Evans AC. Propofol anesthesia and cerebral blood flow changes elicited by vibrotactile stimulation: a positron emission tomography study. J Neurophysiol. 2001;85:1299–308.
Veselis RA, Reinsel RA, Feshchenko VA, Dnistrian AM. A neuroanatomical construct for the amnesic effects of propofol. Anesthesiology. 2002;97:329–37.
Veselis RA, Feshchenko VA, Reinsel RA, Beattie B, Akhurst TJ. Propofol and thiopental do not interfere with regional cerebral blood flow response at sedative concentrations. Anesthesiology. 2005;102:26–34.
Mhuircheartaigh RN, Rosenorn-Lanng D, Wise R, Jbabdi S, Rogers R, Tracey I. Cortical and subcortical connectivity changes during decreasing levels of consciousness in humans: a functional magnetic resonance imaging study using propofol. J Neurosci. 2010;30:9095–102.
Boveroux P, Vanhaudenhuyse A, Bruno MA, Noirhomme Q, Lauwick S, Luxen A, Degueldre C, Plenevaux A, Schnakers C, Phillips C, Brichant JF, Bonhomme V, Maquet P, Greicius MD, Laureys S, Boly M. Breakdown of within- and between-network resting state functional magnetic resonance imaging connectivity during propofol-induced loss of consciousness. Anesthesiology. 2010;113:1038–53.
Zhang H, Wang W, Zhao Z, Ge Y, Zhang J, Yu D, Chai W, Wu S, Xu L. The action sites of propofol in the normal human brain revealed by functional magnetic resonance imaging. Anat Rec (Hoboken). 2010;293:1985–90.
Stamatakis EA, Adapa RM, Absalom AR, Menon DK. Changes in resting neural connectivity during propofol sedation. PLoS One. 2010;5:e14224.
Schrouff J, Perlbarg V, Boly M, Marrelec G, Boveroux P, Vanhaudenhuyse A, Bruno MA, Laureys S, Phillips C, Pélégrini-Issac M, Maquet P, Benali H. Brain functional integration decreases during propofol-induced loss of consciousness. Neuroimage. 2011;57:198–205.
Schröter MS, Spoormaker VI, Schorer A, Wohlschläger A, Czisch M, Kochs EF, Zimmer C, Hemmer B, Schneider G, Jordan D, Ilg R. Spatiotemporal reconfiguration of large-scale brain functional networks during propofol-induced loss of consciousness. J Neurosci. 2012;32:12832–40.
Liu X, Lauer KK, Ward BD, Li SJ, Hudetz AG. Differential effects of deep sedation with propofol on the specific and nonspecific thalamocortical systems. Anesthesiology. 2013;108:59–69.
Gili T, Saxena N, Diukova A, Murphy K, Hall JE, Wise RG. The thalamus and brainstem act as key hubs in alterations of human brain network connectivity induced by mild propofol sedation. J Neurosci. 2013;33:4024–31.
Vasileiou I, Xanthos T, Koudouna E, Perrea D, Klonaris C, Katsargyris A, Papadimitriou L. Propofol: a review of its non-anaesthetic effects. Eur J Pharmacol. 2009;605:1–8.
Ishizawa Y. Mechanisms of anesthetic actions and the brain. J Anesth. 2007;21:187–99.
Vanlersberghe C, Camu F. Propofol. Handb Exp Pharmacol. 2008;182:227–52.
Alkire MT, Hudetz AG, Tononi G. Consciousness and anesthesia. Science. 2008;322:876–80.
Jasper H. Diffuse projection systems: the integrative action of the thalamic reticular system. Electroencephalogr Clin Neurophysiol. 1949;1:405–19.
Moruzzi G, Magoun HW. Brain stem reticular formation and activation of the EEG. Electroencephalogr Clin Neurophysiol. 1949;1:455–73.
Steriade M, McCormick DA, Sejnowski TJ. Thalamocortical oscillations in the sleeping and aroused brain. Science. 1993;262:679–85.
Kaisti KK, Metsähonkala L, Teräs M, Oikonen V, Aalto S, Jääskeläinen S, Hinkka S, Scheinin H. Effects of surgical levels of propofol and sevoflurane anesthesia on cerebral blood flow in healthy subjects studied with positron emission tomography. Anesthesiology. 2002;96:1358–70.
Bonhomme V, Boveroux P, Hans P, Brichant JF, Vanhaudenhuyse A, Boly M, Laureys S. Influence of anesthesia on cerebral blood flow, cerebral metabolic rate, and brain functional connectivity. Curr Opin Anaesthesiol. 2011;24:474–9.
Fox PT, Raichle ME, Mintun MA, Dence C. Nonoxidative glucose consumption during focal physiologic neural activity. Science. 1988;241:462–4.
Mintun MA, Lundstrom BN, Snyder AZ, Vlassenko AG, Shulman GL, Raichle ME. Blood flow and oxygen delivery to human brain during functional activity: theoretical modeling and experimental data. Proc Natl Acad Sci U S A. 2001;98:6859–64.
Franks NP, Lieb WR. Molecular and cellular mechanisms of general anaesthesia. Nature. 1994;367:607–14.
Xie G, Deschamps A, Backman SB, Fiset P, Chartrand D, Dagher A, Plourde G. Critical involvement of the thalamus and precuneus during restoration of consciousness with physostigmine in humans during propofol anaesthesia: a positron emission tomography study. Br J Anaesth. 2011;106:548–57.
Becerra L, Harter K, Gonzalez RG, Borsook D. Functional magnetic resonance imaging measures of the effects of morphine on central nervous system circuitry in opioid-naive healthy volunteers. Anesth Analg. 2006;103:208–16.
Harel N, Uğurbil K, Uludağ K, Yacoub E. Frontiers of brain mapping using MRI. J Magn Reson Imaging. 2006;23:945–57.
Heinke W, Schwarzbauer C. Subanesthetic isoflurane affects task-induced brain activation in a highly specific manner: a functional magnetic resonance imaging study. Anesthesiology. 2001;94:973–81.
Matthews PM, Jezzard P. Functional magnetic resonance imaging. J Neurol Neurosurg Psychiatry. 2004;75:6–12.
Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci. 2007;8:700–11.
Biswal BB, Mennes M, Zuo XN, Gohel S, Kelly C, Smith SM, Beckmann CF, Adelstein JS, Buckner RL, Colcombe S, Dogonowski AM, Ernst M, Fair D, Hampson M, Hoptman MJ, Hyde JS, Kiviniemi VJ, Kötter R, Li SJ, Lin CP, Lowe MJ, Mackay C, Madden DJ, Madsen KH, Margulies DS, Mayberg HS, McMahon K, Monk CS, Mostofsky SH, Nagel BJ, Pekar JJ, Peltier SJ, Petersen SE, Riedl V, Rombouts SA, Rypma B, Schlaggar BL, Schmidt S, Seidler RD, Siegle GJ, Sorg C, Teng GJ, Veijola J, Villringer A, Walter M, Wang L, Weng XC, Whitfield-Gabrieli S, Williamson P, Windischberger C, Zang YF, Zhang HY, Castellanos FX, Milham MP. Toward discovery science of human brain function. Proc Natl Acad Sci U S A. 2010;107:4734–9.
Mashour GA, Alkire MT. Consciousness, anesthesia, and the thalamocortical system. Anesthesiology. 2013;118:13–5.
Velly LJ, Rey MF, Bruder NJ, Gouvitsos FA, Witjas T, Regis JM, Peragut JC, Gouin FM. Differential dynamic of action on cortical and subcortical structures of anesthetic agents during induction of anesthesia. Anesthesiology. 2007;107:202–12.
Franks NP. General anaesthesia: from molecular targets to neuronal pathways of sleep and arousal. Nat Rev Neurosci. 2008;9:370–86.
Alkire MT, Haier RJ, Fallon JH. Toward a unified theory of narcosis: brain imaging evidence for a thalamocortical switch as the neurophysiologic basis of anesthetic-induced unconsciousness. Conscious Cogn. 2000;9:370–86.
Liu X, Lauer KK, Ward BD, Rao SM, Li SJ, Hudetz AG. Propofol disrupts functional interactions between sensory and high-order processing of auditory verbal memory. Hum Brain Mapp. 2012;33:2487–98.
Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, Reiss AL, Greicius MD. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56.
Damoiseaux JS, Rombouts SA, Barkhof F, Scheltens P, Stam CJ, Smith SM, Beckmann CF. Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci U S A. 2006;103:13848–53.
Mason MF, Norton MI, Van Horn JD, Wegner DM, Grafton ST, Macrae CN. Wandering minds: the default network and stimulus-independent thought. Science. 2007;315:393–5.
Boly M, Phillips C, Balteau E, Schnakers C, Degueldre C, Moonen G, Luxen A, Peigneux P, Faymonville ME, Maquet P, Laureys S. Consciousness and cerebral baseline activity fluctuations. Hum Brain Mapp. 2008;29:868–74.
Boly M, Phillips C, Tshibanda L, Vanhaudenhuyse A, Schabus M, Dang-Vu TT, Moonen G, Hustinx R, Maquet P, Laureys S. Intrinsic brain activity in altered states of consciousness: how conscious is the default mode of brain function? Ann N Y Acad Sci. 2008;1129:119–29.
Dehaene S, Changeux JP, Naccache L, Sackur J, Sergent C. Conscious, preconscious, and subliminal processing: a testable taxonomy. Trends Cogn Sci. 2006;10:204–11.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Song, Xx., Yu, Bw. Anesthetic effects of propofol in the healthy human brain: functional imaging evidence. J Anesth 29, 279–288 (2015). https://doi.org/10.1007/s00540-014-1889-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1889-4