Abstract
Purpose
Atrial arrhythmias are common after non-cardiac thoracic surgery. We tested the hypothesis that TEA reduces the risk of new-onset atrial arrhythmias after pulmonary resection.
Methods
We evaluated patients who had pulmonary resection. New-onset atrial arrhythmias detected before hospital discharge was our primary outcome. Secondary outcomes included other cardiovascular complications, pulmonary complications, time-weighted average pain score over 72 h, and duration of hospitalization. Patients with combination of general anesthesia and TEA were matched on propensity scores with patients given general anesthesia only. The matched groups were compared by use of logistic regression, linear regression, or Cox proportional hazards regression, as appropriate.
Results
Among 1,236 patients who had pulmonary resections, 937 received a combination of general anesthesia and TEA (TEA) and 299 received general anesthesia only (non-TEA). We successfully matched 311 TEA patients with 132 non-TEA patients. We did not find a significant association between TEA and postoperative atrial arrhythmia (odds ratio (95 % CI) of 1.05 (0.50, 2.19), P = 0.9). TEA was not significantly associated with length of hospital stay or postoperative pulmonary complications (odds ratio (95 % CI) of 0.71 (0.22, 2.29), P = 0.47). TEA patients experienced fewer postoperative cardiovascular complications; although the association was not statistically significant (odds ratio (95 % CI) of 0.30 (0.06, 1.45), P = 0.06). Time-weighted average pain scores were similar in the two groups.
Conclusion
TEA was not associated with reduced occurrence of postoperative atrial arrhythmia. Although postoperative pulmonary complications were similar with and without TEA, TEA patients tended to experience fewer cardiovascular complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atrial arrhythmia is a common complication after non-cardiac thoracic surgery [1, 2]. Although usually self-limited, the occurrence of atrial arrhythmia has been associated with increased costs, prolonged hospital stay, and higher mortality [3–5]. Although the cause of arrhythmia after thoracic surgery is unclear, and probably multifactorial, several underlying mechanisms have been suggested. First, injury to the cardiac parasympathetic nerves as a result of surgical manipulations causes relative sympathotonic status and can precipitate arrhythmias [6–8]. It has also been suggested that increased pulmonary vascular resistance caused by reduced pulmonary vascular bed after lung resection, and resulting increased right heart pressure, is a risk factor for tachyarrhythmias after thoracic surgery [1, 9]. Furthermore, neuroendocrine responses to surgical stimuli and inflammation could also be mechanisms of postoperative atrial arrhythmia, because anti-inflammatory drugs reduce its occurrence after cardiac surgery [10, 11].
Thoracic epidural analgesia (TEA) is widely used, intra and post-operatively, for thoracic surgery. Cardiac sympathetic nerve (T1–T4) blockade by epidurally administered local anesthetics attenuates sympathotonic status after pulmonary resection, and even when a high thoracic level of block is not achieved, it blocks the sensory input to the spinal cord and reduces neuroendocrine response to surgical pain. TEA directly reduces pulmonary vascular resistance in pulmonary hypertension [12]. The effect is also advantageous in reducing right heart strain caused by reduced pulmonary vascular bed. Recent meta-analysis indicates that TEA significantly reduces the occurrence of atrial arrhythmia during cardiac surgery [13]. However, the protective effect of TEA against atrial arrhythmia during non-cardiac thoracic surgery remains controversial [14–18].
We thus proposed testing the primary hypothesis that the occurrence of postoperative atrial arrhythmia in pulmonary resection is less frequent with combined general anesthesia and TEA than with general anesthesia alone. Our secondary hypotheses were that patients who received combined general anesthesia and TEA have fewer pulmonary complications and cardiovascular complications, require shorter length of hospital stay, and have lower postoperative pain score than those who received general anesthesia alone.
Materials and methods
This analysis was approved by the Cleveland Clinic Institutional Review Board.
Subject selection
We obtained data, from the Society of Thoracic Surgeons Adult Cardiac Surgery Database, for 2,085 unique patients who had thoracic surgery at Cleveland Clinic between January 2005 and September 2012. Demographic and baseline data obtained from the registry were augmented with manually-encoded additional clinical data obtained from eligible patients’ electronic medical records.
We excluded patients who had permanent atrial fibrillation and/or atrial flutter (ICD-9 diagnosis codes 427.31 and 427.32), lumbar or sacral epidural analgesia (CPT code 62319), intraoperative placement of intercostal nerve block (CPT codes 64420 or 64421), or paravertebral block (CPT code 64520) for intraoperative and/or postoperative analgesia, and patients with epidural catheters for whom epidural anesthesia medication was not started before the end of surgery. We also excluded emergency and urgent cases, lung-transplant surgery, and bilateral thoracic surgery. We also excluded patients for whom outcome or key baseline details, including potential confounding factors, were missing (Fig. 1).
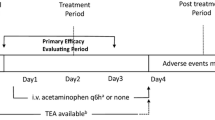
Our primary outcome was postoperative atrial arrhythmia (atrial fibrillation or atrial flutter) from the end of the surgery until hospital discharge. Our secondary outcomes were pulmonary complications (i.e. pneumonia, ARDS, bronchopleural fistula, empyema, postoperative mechanical ventilation >48 h, reintubation, tracheostomy), cardiovascular complications other than atrial arrhythmia (i.e., myocardial infarction, ventricular arrhythmia, deep vein thrombosis, pulmonary embolism), length of hospital stay, and postoperative pain scores.
Statistical analysis
Patients given combined general anesthesia and TEA were matched, on the basis of propensity scores, with control patients who had general anesthesia only, in a 3:1 ratio [19]. Propensity scores (i.e., the estimated the probability of receiving TEA on the basis of demographic and baseline characteristics) were estimated for each patient by use of logistic regression; all the pre-specified potential confounding variables listed in Table 1, except surgical approach, were used in this model. After randomly ordering the observations in the dataset, we used a sequential distance matching algorithm to match, each patient given only general anesthesia with as many as three patients given TEA, restricting successful matches to those with a common surgical approach and those for whom the propensity scores did not differ by more than 0.01 units. This subset of matched patients was used for all subsequent analyses.
Balance on potential confounding variables between matched TEA patients and patients receiving only general anesthesia was evaluated by using standard univariable summary statistics and absolute standardized difference scores (absolute value of difference in means, mean ranking, or proportions, divided by a combined estimate of standard deviation among the two groups). Potential confounding variables with an absolute standardized difference score of 0.20 \(\left({\rm i.e.,}\,1.96\; \times \sqrt {\frac{311 + 132}{311\; \times 132}}\right)\) or greater in absolute value were used for adjustment in all subsequent analysis [20].
Standard model-based Wald tests for regression coefficients were used to test all hypotheses. The Bonferroni correction for multiple comparisons was applied, to constrain overall type I error for the four secondary hypotheses to 5 %; thus, the nominal significance criterion for secondary hypotheses was P < 0.0125.
SAS statistical software version 9.3 (SAS Institute, Cary, NC, USA) for 64-bit Microsoft Windows and R statistical software version 2.15.2 for the 64-bit Unix operating system (The R Foundation for Statistical Computing, Vienna, Austria) were used for all statistical analysis.
Primary outcome
A logistic regression model was developed for estimation of the relationship between TEA and occurrence of postoperative atrial arrhythmia, adjusting for the potential confounding variables that remained inadequately balanced after matching. The odds of postoperative atrial arrhythmia were compared for matched patients with and without TEA.
To evaluate the sensitivity of our results for primary outcome to the method of controlling for covariates, we repeated the analysis for primary outcome among all 1,236 patients meeting inclusion and exclusion criteria, using standard multivariable logistic regression adjustment to estimate the treatment effect.
Secondary outcomes
Matched patients with and without TEA were compared for pulmonary and cardiovascular (other than atrial arrhythmia) complications by use of logistic regression models and accounting for any imbalanced potential confounding variables as specified above for the primary analysis.
Multivariable Cox proportional hazards regression models for time-to-event endpoints were used to assess the relationship between TEA use and duration of hospitalization [21]. The survival model was used to account for censoring as a result of death in hospital (in addition to controlling for imbalanced potential confounders). Hospital stays for patients who died in hospital and in the ICU were censored at the longest observed time until live discharge for the sample.
A multivariable linear regression model was developed for estimation of the difference between mean time-weighted average pain scores for matched patients with and without TEA. A time-weighted average algorithm was used to estimate a patient’s mean 72 h postoperative pain score, taking into account the levels of the pain and the potentially irregular time durations between consecutive pain measurements.
Power considerations
Because our study was observational in nature, our sample size was fixed. We thus a priori estimated the effect size for which we had 90 % power to detect at the 0.05 significance level. Given an expected incidence of atrial arrhythmia of 9 % for patients who received only general anesthesia and a sample size of 443, we expected having 90 % power to detect an odds ratio of 2.6 or greater by comparing the two study groups on postoperative atrial arrhythmia.
Results
Query of the Society of Thoracic Surgeons Adult Cardiac Surgery Database revealed 2,085 unique patients undergoing thoracic surgery at Cleveland Clinic between January 2005 and September 2012. After applying exclusion criteria and eliminating patients with missing baseline or outcome measurements 1,236 patients remained, including 937 (76 %) who received combined TEA and general anesthesia and 299 (24 %) who received general anesthesia alone (Fig. 1). Then, on the basis of demographic and baseline characteristics, we successfully matched, in a 3:1 ratio, 311 patients receiving a combination of TEA and general anesthesia (33 % of the total TEA patients) with 132 non-TEA patients receiving only general anesthesia (i.e. a total of 443 patients).
Baseline characteristics of patients with and without TEA before and after propensity score matching are shown in Table 1. As is apparent from the left of Table 1, baseline characteristics of patients receiving TEA were somewhat different from those of patients not receiving TEA: patients receiving TEA had slightly lower BMI, lower creatinine, higher albumin, were more likely to have lung cancer, tended to have longer surgery, tended to undergo thoracotomy more frequently than thoracoscopy, and tended to have lobectomy or complete pneumonectomy more frequently than segmental resection. Furthermore, they were more likely to have mediastinal lymph node dissection and less likely to have wedge resection. After matching (Table 1, right panel), most of the variables were well balanced (absolute value of standardized difference <0.20). Only surgical approach and duration of surgery remained imbalanced, in accordance with our pre-specified criteria; these factors were used for adjustment in all models comparing outcomes.
Although a relatively small proportion (33 %) of TEA patients were successfully matched (and thus used in the final analysis), these matched patients seemed to be very similar to the total sample and to non-matched patients (Appendix 1).
The primary and secondary outcomes are summarized in Table 2. Using matched patients and adjusting for imbalanced confounders we did not find a significant association between TEA and postoperative atrial arrhythmia (Wald test P = 0.90). The results of sensitivity analysis which investigated multivariable regression adjustment instead of matching was consistent with the results from the primary model.
We did not find an association between TEA use and any of the secondary outcomes (Table 2). Four matched patients died before discharge from the hospital and were censored for our Cox regression model for duration of hospitalization.
Discussion
We did not find a difference in the incidence of postoperative atrial arrhythmia between matched patients who had TEA for postoperative analgesia or general anesthesia alone. Furthermore, TEA was not significantly associated with shortened hospital stay or fewer postoperative pulmonary complications. TEA patients tended to experience fewer postoperative cardiovascular complications, although the association was not statistically significant. Finally, pain scores were similar for those who received TEA and those who did not.
Kopeika et al. [15] showed TEA provided superior postoperative pain control than intramuscular opioid administration after pulmonary resection, and found a tendency of less frequent postoperative atrial fibrillation among those who received TEA. Oka et al. [17] compared TEA with bupivacaine and TEA with morphine for postoperative analgesia for pulmonary resection and found that occurrence of atrial fibrillation and supraventricular tachycardia within 3 days after surgery was less for TEA with bupivacaine. However, in that study [17] patients in the bupivacaine group received a higher dose of indomethacin than those in the morphine group. Groban et al. [18] found occurrence of atrial fibrillation, atrial flutter, and supraventricular tachycardia increased after the TEA catheter was removed. However, TEA was continued only until 2.7 days after surgery, which is the time of frequent occurrence of atrial arrhythmia [22], and the occurrence of atrial arrhythmia after discontinuation of TEA could be just coincidence rather than a causal relationship. Jiang et al. [14] compared the incidence of supraventricular arrhythmia (supraventricular ectopic beats, supraventricular tachycardia, and atrial fibrillation) within 48 h after pulmonary resection between patients having TEA with a combination of local anesthetic and opioid for intra and post-operative analgesia and those who received intravenous patient-controlled analgesia with opioids. These authors observed significantly less supraventricular tachycardia and a tendency of less frequent atrial fibrillation among patients who received intravenous patient-controlled analgesia. Ahn et al. [23] compared intravenous patient-controlled analgesia with fentanyl plus ketorolac vs TEA for postoperative analgesia among esophageal surgery patients and found that occurrence of arrhythmia until 3 days after surgery was similar between the groups. Apart from differences in the populations and the specific analgesic regimens studied, differences in the way arrhythmia was diagnosed, duration of observation after the surgery, and use of non-steroidal anti-inflammatory drugs, which are potentially protective against atrial arrhythmia, could be possible explanations of conflicting outcomes between the studies.
In our study, 0.1 % bupivacaine plus fentanyl 2 mcg/ml solution was started during the surgery and continued postoperatively at a rate of 5 ml/h. Intraoperative management of TEA was otherwise at the discretion of the anesthesia provider and was not standardized. Therefore, we could not guarantee blockade of cardiac sympathetic fibers (T1–T4) among our patients. Another possible explanation for lack of protective effect against atrial arrhythmia by TEA in our study could be that relatively high sympathetic tone may not be a major cause of postoperative atrial arrhythmia, rather other factors, for example neuroendocrine responses characterized by increases in cytokines and corticosteroids, which are not suppressed by epidural analgesia after major surgery [24], or local damage of tissue with electrical properties in pulmonary veins during surgical manipulation might have major effects in mechanism of development of postoperative atrial arrhythmia. Further, liberal use of ketorolac to manage shoulder pain for both TEA and non-TEA patients might have diluted the effect of TEA.
In our study, occurrence of postoperative cardiovascular complications other than atrial arrhythmia was almost three times more frequent among non-TEA patients than among TEA patients, although the difference failed to reach statistical significance. Sympathetic blockade by TEA reduces myocardial oxygen demand and improves myocardial oxygen supply by coronary dilatation [25–27]. TEA directly reduces pulmonary vascular resistance in pulmonary hypertension [12]. The outcome of cardiovascular complication is in accordance with theoretical protective effects of epidural analgesia.
Epidural analgesia restores pulmonary function after thoracotomy [28] and reduces the incidence of postoperative pneumonia [29]. Our non-TEA patients received intravenous patient-controlled analgesia with opioids as analgesic regimen postoperatively, which provided pain relief similar to that of epidural analgesia. Comparative pain control between the groups might be the reason we did not observe a difference in occurrence of pulmonary complications in our study.
Use of TEA was not randomly assigned; it was, instead, selected at the discretion of attending anesthesiologists. It is likely that their choices were affected by the physical status and perceived risk of epidural-related complications. For example, epidural analgesia was presumably avoided for patients with low preoperative platelet counts, coagulation abnormalities, or who took antiplatelet or anticoagulation medications. To reduce selection bias, we used propensity score match on 40 potential confounding factors. Furthermore, confounding factors which remained slightly imbalanced after propensity matching were included in our multivariable models. But, of course, our retrospective analysis remains subject to selection bias and confounding by unobserved variables, some of which may have been important.
Results may differ at other centers or even for subtly different populations. We cannot exclude limited sample size as a reason we did not identify statistically significant differences in the primary and secondary outcomes between groups. And, finally, as with all observational studies, the associations we report may or may not indicate causal relationships between use of TEA and the outcomes.
In summary, we did not find a significant difference in the odds of postoperative atrial arrhythmia between patients who were given TEA compared to those who were not. Likewise TEA was not associated with prolonged hospital stay and postoperative pain score. Pulmonary and cardiovascular complications were not significantly associated, but a decreased trend of cardiovascular complications was observed with TEA use.
References
Amar D, Roistacher N, Burt M, Reinsel RA, Ginsberg RJ, Wilson RS. Clinical and echocardiographic correlates of symptomatic tachydysrhythmias after noncardiac thoracic surgery. Chest. 1995;108:349–54.
Harpole DH, Liptay MJ, DeCamp MM Jr, Mentzer SJ, Swanson SJ, Sugarbaker DJ. Prospective analysis of pneumonectomy: risk factors for major morbidity and cardiac dysrhythmias. Ann Thorac Surg. 1996;61:977–82.
Amar D, Burt M, Reinsel RA, Leung DH. Relationship of early postoperative dysrhythmias and long-term outcome after resection of non-small cell lung cancer. Chest. 1996;110:437–9.
Polanczyk CA, Goldman L, Marcantonio ER, Orav EJ, Lee TH. Supraventricular arrhythmia in patients having noncardiac surgery: clinical correlates and effect on length of stay. Ann Intern Med. 1998;129:279–85.
Sekine Y, Kesler KA, Behnia M, Brooks-Brunn J, Sekine E, Brown JW. COPD may increase the incidence of refractory supraventricular arrhythmias following pulmonary resection for non-small cell lung cancer. Chest. 2001;120:1783–90.
Asamura H, Naruke T, Tsuchiya R, Goya T, Kondo H, Suemasu K. What are the risk factors for arrhythmias after thoracic operations? A retrospective multivariate analysis of 267 consecutive thoracic operations. J Thorac Cardiovasc Surg. 1993;106:1104–10.
Kimura T, Komatsu T, Takezawa J, Shimada Y. Alterations in spectral characteristics of heart rate variability as a correlate of cardiac autonomic dysfunction after esophagectomy or pulmonary resection. Anesthesiology. 1996;84:1068–76.
Oka T, Ozawa Y. Correlation between intraoperative hemodynamic variability and postoperative arrhythmias in patients with pulmonary surgery. Masui. 1999;48:118–23.
Lindgren L, Lepantalo M, von Knorring J, Rosenberg P, Orko R, Scheinin B. Effect of verapamil on right ventricular pressure and atrial tachyarrhythmia after thoracotomy. Br J Anaesth. 1991;66:205–11.
Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, Barash PG, Hsu PH, Mangano DT. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–9.
Patti G, Chello M, Candura D, Pasceri V, D’Ambrosio A, Covino E, Di Sciascio G. Randomized trial of atorvastatin for reduction of postoperative atrial fibrillation in patients undergoing cardiac surgery: results of the ARMYDA-3 (Atorvastatin for Reduction of MYocardial Dysrhythmia After cardiac surgery) study. Circulation. 2006;114:1455–61.
Armstrong P. Thoracic epidural anaesthesia and primary pulmonary hypertension. Anaesthesia. 1992;47:496–9.
Svircevic V, van Dijk D, Nierich AP, Passier MP, Kalkman CJ, van der Heijden GJ, Bax L. Meta-analysis of thoracic epidural anesthesia versus general anesthesia for cardiac surgery. Anesthesiology. 2011;114:271–82.
Jiang Z, Dai JQ, Shi C, Zeng WS, Jiang RC, Tu WF. Influence of patient-controlled i.v. analgesia with opioids on supraventricular arrhythmias after pulmonary resection. Br J Anaesth. 2009;103:364–8.
Kopeika U, Taivans I, Udre S, Jakusenko N, Strazda G, Mihelsons M. Effects of the prolonged thoracic epidural analgesia on ventilation function and complication rate after the lung cancer surgery. Medicina (Kaunas). 2007;43:199–207.
Neustein SM, Krellenstein D, Cohen E. Arrhythmias after video assist thoracoscopy. Anesth Analg. 2002;94:1372.
Oka T, Ozawa Y, Ohkubo Y. Thoracic epidural bupivacaine attenuates supraventricular tachyarrhythmias after pulmonary resection. Anesth Analg. 2001;93:253–9.
Groban L, Dolinski SY, Zvara DA, Oaks T. Thoracic epidural analgesia: its role in postthoracotomy atrial arrhythmias. J Cardiothorac Vasc Anesth. 2000;14:662–5.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Cox DR. Regression Models and Life-Tables. J R Stat Soc Series B Methodol. 1972;34:187–220.
Roselli EE, Murthy SC, Rice TW, Houghtaling PL, Pierce CD, Karchmer DP, Blackstone EH. Atrial fibrillation complicating lung cancer resection. J Thorac Cardiovasc Surg. 2005;130:438–44.
Ahn HJ, Sim WS, Shim YM, Kim JA. Thoracic epidural anesthesia does not improve the incidence of arrhythmias after transthoracic esophagectomy. Eur J Cardiothorac Surg. 2005;28:19–21.
Yokoyama M, Itano Y, Katayama H, Morimatsu H, Takeda Y, Takahashi T, Nagano O, Morita K. The effects of continuous epidural anesthesia and analgesia on stress response and immune function in patients undergoing radical esophagectomy. Anesth Analg. 2005;101:1521–7.
Kirno K, Friberg P, Grzegorczyk A, Milocco I, Ricksten SE, Lundin S. Thoracic epidural anesthesia during coronary artery bypass surgery: effects on cardiac sympathetic activity, myocardial blood flow and metabolism, and central hemodynamics. Anesth Analg. 1994;79:1075–81.
Blomberg S, Emanuelsson H, Ricksten SE. Thoracic epidural anesthesia and central hemodynamics in patients with unstable angina pectoris. Anesth Analg. 1989;69:558–62.
Blomberg S, Emanuelsson H, Kvist H, Lamm C, Ponten J, Waagstein F, Ricksten SE. Effects of thoracic epidural anesthesia on coronary arteries and arterioles in patients with coronary artery disease. Anesthesiology. 1990;73:840–7.
Brichon PY, Pison C, Chaffanjon P, Fayot P, Buchberger M, Neron L, Bocca A, Verdier J, Sarrazin R. Comparison of epidural analgesia and cryoanalgesia in thoracic surgery. Eur J Cardiothorac Surg. 1994;8:482–6.
Popping DM, Elia N, Marret E, Remy C, Tramer MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: a meta-analysis. Arch Surg. 2008;143:990–9.
Acknowledgments
Supported by departmental funds.
Conflict of interest
No conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
See Table 3.
About this article
Cite this article
Komatsu, R., Makarova, N., Dalton, J.E. et al. Association of thoracic epidural analgesia with risk of atrial arrhythmias after pulmonary resection: a retrospective cohort study. J Anesth 29, 47–55 (2015). https://doi.org/10.1007/s00540-014-1865-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1865-z