Abstract
Purpose
Knowledge of the cumulative balance of sodium (CBS) is important for the diagnosis of salt disorders and water homeostasis and has the potential to predict hypovolemic status in acute neurological patients. However, an extensive application of the use of CBS is still lacking in the intensive care setting, where salt and water homeostasis represents a priority.
Methods
Records of consecutive series of acute neurological patients admitted to a neurointensive care unit over a 6-month period were retrospectively reviewed. CBS was calculated at the admission to the Emergency Department. Discrimination between cerebral salt-wasting syndrome (CSWS) and the syndrome of inappropriate antidiuretic hormone secretion (SIADH) was performed on the basis of the classical criteria. Additionally, we used the findings of a negative CBS exceeding 2 mEq/kg for the diagnosis of CSWS. Two independent clinicians who were blinded to the CBS results performed diagnosis of the causes of hyponatremia and estimated the daily volemic status of the patients on the basis of clinical parameters. Logistic regression analysis was used to determine the independent prognostic factors of hypovolemia.
Results
Thirty-five patients were studied for a total of 418 days. Four patients (11.4 %) fitted the criteria of CSWS and three patients (8.5 %) had SIADH. The unavailability of the CBS led to a wrong diagnosis in three of the eight hyponatremic patients (37.5 %). The risk of developing hypovolemia in patients with negative CBS was 7.1 times higher (CI 3.86–13.06; p < 0.001). Multivariate analysis revealed that negative cumulative fluid balance, negative CBS >2 mEq/kg, and CVP ≤5 cmH2O were independent prognostic factors for hypovolemia.
Conclusions
CBS is likely to be a useful parameter in the diagnosis of CSWS and a surrogate parameter for estimating hypovolemia in acute neurological patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Critically ill adult neurologic patients have a high incidence of salt and water homeostasis disorders [1]. Hyponatremia is one of the most common of these disorders, and when associated with hypotonicity can cause or increase cerebral edema and intracranial hypertension, thus worsening the neurological outcome [2].
The syndrome of inappropriate antidiuretic hormone secretion (SIADH) and cerebral salt-wasting syndrome (CSWS) are historically considered the two pivotal causes of hyponatremia in neurologic patients [1, 3–6]. The distinction between these two disorders is important since they require different treatments: fluid restriction in SIADH and sodium and volume replacement in CSWS [1, 3]. Up till now the differentiation between these two disorders has been made by measuring extracellular fluid volume (ECF), which is expanded or normal in SIADH, and decreased in CSWS [1, 5–7]. Many parameters are routinely used to evaluate ECF, however, these variables have limited sensitivity and specificity. Even the variables obtained more invasively may be misleading or not continuously available at the bedside, hence distinction between CSWS and SIADH might be difficult [8–11].
In a review published in 2002, Singh et al. [11, 12] emphasized that the clinical diagnosis of CSWS requires a true deficit of sodium evaluated by mass balances, suggesting that a deficit of sodium exceeding 2 mmol/kg body weight implies a contracted ECF volume. Stressing this concept, a diagnosis of CSWS could theoretically be obtained by a negative cumulative balance of sodium (CBS) exceeding 2 mmol/kg body weight given that no other physiological or pathological reasons for sodium excretion are found [11]. Although intriguing, a widespread application of this method in the intensive care setting is still lacking.
The primary purpose of the present study is to investigate the use of CBS to discriminate SIADH from CSWS in critically ill adult neurologic patients by applying the Singh et al. criteria and using a true deficit of sodium as principal parameter for diagnosing. The secondary purpose of this study is to compare the role of the daily sodium mass balance and cumulative balance of sodium with other surrogate markers of hypovolemia in patients admitted to a neurointensive care unit.
Materials and methods
After approval of the study by our hospital’s ethics committee (December 2012), we retrospectively reviewed the records of a consecutive series of patients admitted to the neurointensive care unit of our hospital over a previous 6-month period (March–September). In this period we introduced the practice of calculating the daily balance of sodium in patients with critical neurologic or neurosurgical diseases admitted to our ICU.
Inclusion criteria were: the direct admission from an emergency department, age >14 years, the availability of clinical and laboratory data from the admission to the emergency department until the 14th day in the intensive care unit (ICU), and ICU length of stay (LOS) longer than 48 h. Exclusion criteria were: patients with a history of adrenal gland disease or glucocorticoid therapy within the last year, acute renal failure defined by the specific criteria introduced by the Acute Kidney Injury Network (rapid time course, reduction in urine output defined as <0.5 ml/kg/h for more than 6 h, absolute increase in serum creatinine of ≥0.3 mg/dl or percentage increase in serum creatinine of ≥50 %) [13], chronic renal failure in stage IV, V or VI as defined by the international guideline of the Kidney Disease Improving Global Outcomes group (patients with a glomerular filtration rate of <30 ml per min) [14], and acute or chronic heart failure (AMI <3 months, NYHA III–IV) [15].
The evaluation of these patients began at the 1st day of admission to the emergency department, was continued in the ICU and ended at the 14th day in ICU or earlier if the patient was discharged from the ICU or died. Age, sex, simplified acute physiology score II (SAPS II) [16], post-resuscitation GCS score, hospital LOS, and ICU and hospital mortality were recorded.
Sodium balance
Natremia, urinary sodium concentration, plasma and urinary osmolality were recorded from the daily routine laboratory data. Blood and urine samples were sent at room temperature to the clinical laboratory of our hospital and analyzed immediately by the indirect potentiometry method (Advia 2400, Siemens Healthcare Diagnostics, Germany). Sodium excretion was measured in 24-h urine samples. Daily sodium balance was evaluated by analysis of intake and output of sodium, whereas the cumulative sodium balance was calculated from all the daily sodium balances. All the volumes, including the infusion solutions, medications as well as nutrition, were considered for the balances. Loss of sodium in sweat and feces was not included in the calculation of sodium balance. Cumulative sodium balance was identified as “negative” when the loss of sodium was higher than 2 mEq/kg [11, 12]. Hyponatremia was identified as a plasma sodium concentration <135 mEq/l, hypo-osmolality as a plasma osmolality <280 mOsm/kg, increased urinary sodium output as a urine sodium concentration greater than 20 mEq/l, increased urinary osmolality as a urine osmolality greater than 100 mOsm/kg, and hypernatremia was defined as a serum sodium level higher than 145 mEq/l [11, 12].
CSWS and SIADH diagnosis
In order to diagnose and distinguish CSWS from SIADH we followed the algorithm described in Fig. 1. The first step of analysis was the identification of patients with acute central nervous system disease in accordance with the inclusion criteria. The second step was the differentiation of patients according to the diagnosis of SIADH or CSWS by applying the diagnostic criteria as shown in Table 1 [11]. The third and final step was the assessment of natremia in patients with CSWS. Based on this algorithm, we identified four groups of patients: patients with SIADH, patients with CSWS and hyponatremia, patients with CSWS without hyponatremia, and patients without any of these diagnoses. Differences between the groups of patients with and without hypo-osmolar hyponatremia regarding demographics, medical history, ICU and hospital lengths of stay (LOS), mortality, fluid and sodium intake were evaluated.
Clinical evaluation of hypovolemia and CBS
The evaluation of the cumulative balance of sodium as a single surrogate marker of hypovolemia was performed by comparing it with five clinical signs derived from the retrospective revision of the patientsʼ charts. According to previous reports and guidelines, the five variables explored were central venous pressure (CVP), mean arterial pressure, hemoglobin and hematocrit values, balance volume and the use of catecholamines [17]. A central venous catheter was placed through the internal jugular vein or subclavian vein and the position of the catheter tip was placed within the right atrium. Hypovolemia was defined as accumulated fluid balance of <60 ml/kg per day or a CVP of 5 mmHg or less, while anemia was defined as a hematocrit level of <33 % [17]. Two independent expert anesthesiologists, blinded to the results of the daily balance of sodium and cumulative balance of sodium, reviewed the five aforementioned clinical signs and assessed the daily volemic status of the patient as euvolemic or hypovolemic. A hypovolemic state was declared only if both the anesthesiologists agreed.
In cases of hyponatremia, the two expert anesthesiologists independently performed a presumptive diagnosis of the causes of hyponatremia.
Statistical analysis
Data are expressed as a mean, with standard deviations for continuous variables and frequencies for categorical variables. In order to make univariate comparisons between normal and hyponatremic groups of patients, Pearson’s chi-squared test was used for categorical variables, a t-test for continuous variables and a Wilcoxon–Mann–Whitney for non-parametric variables. Agreement between physicians on the presence or absence of signs of hypovolemia was assessed by the kappa measurement of agreement. Standard formulas were used to calculate sensitivity, specificity, and positive and negative predictive value for each of the clinical parameters.
Clinical signs and parameters evaluated by mass balances rather than excretion rates of sodium (negative cumulative balance, negative fluid balance, use of catecholamine, use of diuretics, CVP ≤5 mmHg, excretion of urinary sodium <25 mEq/l, fractional sodium excretion <1 %, Hb <11.5 g/dl, Htc <33.5 %, MAP >87 mmHg) were collected for primary comparison. In order to make univariate comparisons between hypovolemic subgroups and the presence of one of the variables, logistic regression models were constructed using hypovolemia as the dependent variable and the presence or absence of a possible variable which could explain hypovolemia as the independent variable. Clinical factors found to have a p value of <0.20 in the univariate analysis were entered into stepwise multiple logistic regression analysis to determine which were independent prognostic factors for hypovolemia. Effects of selected factors were expressed in terms of odds ratios (OR), along with their 95 % confidence intervals (CI). Goodness-of-fit of the model was assessed using the Akaike information criterion (AIC) and McFadden’s pseudo R 2 measure [18, 19]. Statistical analyses were computed by R, R Development Core Team [20]. All statistical tests were considered significant for p values of <0.05.
Results
Over a 7-month period, a total of 277 consecutive patients were identified. Of these, 242 patients did not meet the inclusion criteria or were excluded because they did not present with an acute brain lesion, or because they had a stay in ICU shorter than 48 h. Thirty-five patients fulfilled the inclusion criteria and were followed for a total of 418 days. Patient characteristics at admission are presented in Table 2. Nineteen subjects were male (54.3 %), the median age was 51 years and head injury was the main cause of admission to ICU (40 %). Only thirteen (37 %) patients maintained eunatremia during the ICU observation period. Eight patients (22.8 %) developed hypo-osmolar hyponatremia, while ten patients (28.6 %) developed hypernatremia. In the group of eu-hypernatremic patients, five patients (14.3 %) developed a CSWS without hyponatremia.
Hyponatremic patients: CSWS and SIADH
Eight patients (22.8 %) developed a mild hypo-osmolar hyponatremia. These patients were heterogeneous for primary diagnosis at admission, demographics and severity of illness at presentation (Tables 2, 3). One of them developed iatrogenic hyponatremia (2.8 %) due to administration of osmotic therapy, while four patients (11.4 %) fitted the criteria of diagnosis of hyponatremic CSWS, and three patients (8.5 %) the diagnosis of SIADH (Table 3). A wrong diagnosis in three of the eight hyponatremic patients (37.5 %) was made by the two expert anesthesiologists because of the unavailability of the CBS.
In all of the eight patients, hyponatremia was rapidly identified, probably due to the frequent check-ups performed during their stay in ICU. The cumulative fluid and balance of sodium values were the main difference between CSWS and SIADH patients. Although fluid restriction or administration was guided by the cumulative balance of salts and fluids (Table 3), the main strategy adopted both for CSWS and SIADH patients was the administration of sodium, which was performed as soon as possible in order to avoid brain damage. The presence of the daily and cumulative balance of sodium, however, simplified the diagnosis and allowed adoption of the best treatment for every patient (Table 3). Figure 2 shows an example of one of the patients with CSWS without hyponatremia, who would have been misdiagnosed by the conventional methods.
There were no significant differences found between the SIADH patients (group 1) and the hyponatremic CSWS patients (group 2) compared to the other two groups [patients with CSWS without hyponatremia (group 3) and the patients without the aforementioned disorders (group 4)], except for the main daily intake of sodium and creatinine clearance, which was higher in groups 1 and 2; and duration in ICU, which was lower in groups 3 and 4 (Table 2). Five patients (14.3 %), all belonging to either group 3 or 4, died in ICU.
Kappa test results
Of the 418 evaluated days, the two physicians agreed only on 235 (56.2 %), which were 78 days (18.7 %) of hypovolemic status and 157 days (37.6 %) of euvolemic and hypervolemic statuses of the patients, respectively. The kappa measurement of agreement was 0.116 (CI 0.025–0.206; p < 0.05) for the presence or absence of hypovolemia, indicating a poor agreement between physicians for the diagnosis of volemic status of the patients.
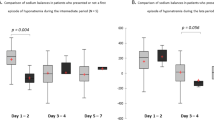
The risk of having hypovolemia was 1.86 times higher in patients with a negative daily balance of sodium (CI 1.01–3.02; p = 0.02), and 8.05 times higher in patients with a negative cumulative balance of sodium >2 mEq/kg (CI 3.77–17.18; p < 0.001).
Univariate logistic regression analysis
Variables that had p values of <0.05 for the development of hypovolemia were: the use of catecholamines (OR 0.47; CI 0.28–0.79), CVP ≤5 mmHg (OR 9.63; CI 5.21–17.78), MAP >87 mmHg (OR 2.28; CI 1.12–4.64), negative cumulative balance of sodium (OR 7.1; CI 3.86–13.05), negative daily balance of sodium (OR 1.82; CI 1.09–3.02), negative cumulative balance of sodium >2 mEq/kg (OR 8.05; CI 3.8–17.2), negative cumulative fluid balance (OR 14.65; CI 7.87–27.30), and negative daily fluid balance (OR 5.82; CI 3.33–10.17) (Table 4).
Multivariate logistic regression analysis
Clinical factors found to have a p value of <0.2 were put in a stepwise multivariate logistic regression for the determination of statistically significant independent prognostic factors for the development of hypovolemia. These factors were: negative cumulative balance of sodium >2 mEq/kg, use of catecholamines, use of diuretics, CVP ≤5 mmHg, MAP >87 mmHg, and negative cumulative fluid balance.
Multivariate analysis revealed prognostic factors for the development of hypovolemia negative cumulative fluid balance (OR 6.7; CI 3.4–13.28), negative cumulative balance of sodium >2 mEq/kg (OR 2.74; CI 1.04–7.19), and CVP ≤5 mmHg (OR 5.24; CI 2.75–9.99). Evaluation of the full and final model after stepwise inclusion or exclusion of variables showed pseudo R 2 values of 0.30 and 0.29, respectively (Table 5), indicative of a reasonable fit to the data.
Discussion
Our study demonstrates that assessments by bedside observation as to whether hyponatremia is associated with SIADH or CSWS, and evaluation of volemic status of the patients by clinical signs, still remains a dilemma for physicians and intensivists [8, 17]. In the intensive care setting, physicians usually pay particular attention to concentrations of electrolytes and plasma osmolality, checking them frequently. The brain edema consequent to a hypo-osmolar hyponatremia could worsen the outcome of patients with acute neurological disease, therefore normal or hypertonic saline are the most used saline infusions [2, 4]. The frequent usage of this kind of infusion can explain the high mean daily intake of sodium, the high presence of hypernatremic patients (28 %), and the presence of only mild hyponatremia. However, in our study, hyponatremia was found in 22.8 % of the patients admitted to the neurocritical care unit and seems to be related to a longer length of stay, as in accordance with previous reports [2, 21]. Even though the hyponatremia was mild, the incidence is impressive because it demonstrates the persistence of the syndromes even in a highly controlled environment such as a dedicated intensive care unit.
Cerebral salt-wasting syndrome with or without hyponatremia represents the most frequent disturbance of salt and water homeostasis in our population, in contrast to other recent findings [22–24]. Although diagnostic criteria for CSWS and SIADH have been clearly defined since the first reports, the greatest part of the studies on distinguishing between these two syndromes have focused on the difference in ECF. Nevertheless, parameters routinely used to evaluate ECF have limited sensitivity and specificity and may be misleading [8–11]. Specialized laboratory tests, such as isotopic red blood cell (RBC) volume measurement or measurement of renin activity in plasma, are not available when the clinical diagnosis of CSW or SIADH has been considered and decisions concerning therapy must be made. Moreover, the majority of the studies show that clinicians use unreliable data such as hyponatremia and the concentration of sodium in urine to conclude if there is salt wasting urine. Electrolytes are not usually measured in patients during the first days of recovery in the ICU, therefore balance data would not be available when the patient manifests hyponatremia [9, 11, 25].
In our study, we were only able to observe a small group of patients. Nonetheless, our study has the merit of exploring the discriminative diagnosis between CSWS and SIADH from a different point of view, performing accurate mass balances of sodium of the patients from admission to the ED until referral to the ICU. The advantage of knowing the sodium status of patients allows clinicians to apply the best treatment in cases of hyponatremia (Fig. 2; Table 3). Moreover, knowledge of the CBS can add information about the volemic status of the patient. To our knowledge, only the study by Carlotti et al. [12] has tried to explore mass balances for sodium accurately during the first 10 days of recovery in 10 children and 12 adults admitted for 10 days to an ICU. However, in none of these patients was the cumulative balance of sodium found to be negative [12]. By studying the sodium balance and changes in plasma volume by using the isotope dilution technique during the 5 days preceding hyponatremia, Wijdicks et al. [26] demonstrated a negative cumulative sodium balance, hyponatremia, and a plasma volume decrease of more than 10 % in 6 of the 21 patients with subarachnoid hemorrhage. In our study, we found nine patients with acute cerebral lesions and negative cumulative mass of sodium exceeding 2 mEq/kg. Four of those patients had a consequent hypo-osmolar hyponatremia suggestive for the diagnosis of CSWS. Our results support the findings by Wijdicks et al. [26] as mentioned above. Furthermore, the step-wise multivariate logistic regression analysis found that the cumulative balance of sodium >2 mEq/kg, the cumulative balance of fluids, and CVP ≤5 mmHg are independently related to hypovolemia.
The major limit of our study is its retrospective nature. Additionally, the procedure of determining the cumulative balance of sodium is time consuming. However, in our opinion, the understanding of mass balance of sodium is essential in the diagnosis of CSWS and SIADH [11]. Besides, it could be a useful parameter which could add information about the volemic status of the patient in the clinical setting of the ICU, where its evaluation may be difficult even for expert anesthesiologists. Our results encourage the idea of refining these findings with further prospective studies, where the main efforts may show mass balance of sodium and water in real time and continuously. It may allow clinicians to evaluate not only the state of salt and water but also to speculate on the volemic status of the patient.
Conclusions
In critical neurology and neurosurgical patients, the use of cumulative balance of sodium is likely to be a simple, economical and efficient tool which may help clinicians to distinguish CSWS from SIADH diagnosis and to improve the comprehension of the volemic status of patients.
References
Tisdall M, Crocker M, Watkiss J, Smith M. Disturbances of sodium in critically ill adult neurologic patients: a clinical review. J Neurosurg Anesthesiol. 2006;18:57–63.
Diringer MN, Zazulia AR. Hyponatremia in neurologic patients: consequences and approaches to treatment. Neurologist. 2006;12:117–26.
Sherlock M, O’Sullivan E, Agha A, Behan LA, Owens D, Finucane F, Rawluk D, Tormey W, Thompson CJ. Incidence and pathophysiology of severe hyponatraemia in neurosurgical patients. Postgrad Med J. 2009;85:171–5.
Schwartz WB, Bennett W, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med. 1957;23:529–42.
Peters JP, Welt LG, Sims EA, Orloff J, Needham J. A salt-wasting syndrome associated with cerebral disease. Trans Assoc Am Physicians. 1950;63:57–64.
Harrigan MR. Cerebral salt wasting syndrome: a review. Neurosurgery. 1996;38(152–160):23.
Hoorn EJ, Halperin ML, Zietse R. Diagnostic approach to a patient with hyponatremia: traditional versus physiology-based options. Q J Med. 2005;98:529–40.
McGee S, Abernethy WB, Simel DL. The rational clinical examination. Is this patient hypovolemic? JAMA. 1999;281:1022–9.
Shippy CR, Appel PL, Shoemaker WC. Reliability of clinical monitoring to asses blood volume in critically ill patients. Crit Care Med. 1984;12:107–12.
Jones JG, Wardrop CAJ. Measurement of blood volume in surgical and intensive care practice. Br J Anaesth. 2000;84:226–35.
Singh S, Bohn D, Carlotti AP, Cusimano M, Rutka JT, Halperin ML. Cerebral salt wasting: truths, fallacies, theories, and challenges. Crit Care Med. 2002;30(2575–2579):24.
Carlotti AP, Bohn D, Rutka JT, Singh S, Berry WA, Sharman A, Cusimano M, Halperin ML. A method to estimate urinary electrolyte excretion in patients at risk for developing cerebral salt wasting. J Neurosurg. 2001;95:420–4.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A, Acute Kidney Injury Network. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31.
Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, De Zeeuw D, Hostetter TH, Lameire N, Eknoyan G. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005;67:2089–100.
The Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Boston: Little, Brown & Co; 1994. p. 253–6.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Stéphan F, Flahault A, Dieudonné N, Hollande J, Paillard F, Bonnet F. Clinical evaluation of circulating blood volume in critically ill patients—contribution of a clinical scoring system. Br J Anaesth. 2001;86:754–62.
Burnham KP, Anderson DR. Multimodal inference: understanding AIC and BIC in model selection. Sociol Methods Res. 2004;33:261–304.
McFadden D. Conditional logit analysis of qualitative choice behavior. In: Zarembka P, editor. Frontiers in econometrics. New York: Academic Press; 1974. p. 105–42.
R: a language and environment for statistical computing. R foundation for statistical computing, Vienna. ISBN 3-900051-07-0. http://www.R-project.org.
Sherlock M, O’Sullivan E, Agha A, Behan LA, Rawluk D, Brennan P, Tormey W, Thompson CJ. The incidence and pathophysiology of hyponatraemia after subarachnoid haemorrhage. Clin Endocrinol (Oxf). 2006;64:250–4.
Oh MS, Carroll HJ. Cerebral salt-wasting syndrome: we need better proof of its existence. Nephron. 1999;82:110–4.
Maesaka JK, Gupta S, Fishbane S. Cerebral salt-wasting syndrome: does it exist? Nephron. 1999;82:100–9.
Brimioulle S, Orellana-Jimenez C, Aminian A, Vincent JL. Hyponatremia in neurological patients: cerebral salt wasting versus inappropriate antidiuretic hormone secretion. Intensive Care Med. 2008;34(125–31):26.
Harrigan MR. Cerebral salt wasting syndrome. Crit Care Clin. 2001;17:125–38.
Wijdicks EF, Vermeulen M, ten Haaf JA, Hijdra A, Bakker WH, van Gijn J. Volume depletion and natriuresis in patients with a ruptured intracranial aneurysm. Ann Neurol. 1985;18:211–6.
Acknowledgments
We would like to thank Dr Benvenuto Antonini, from the Anesthesia and Intensive Care Department of Manerbio Hospital, Brescia. The authors wish to dedicate this work to Nicola Motterlini, outstanding researcher and statistician, gentle and brave man.
Conflict of interest
The authors have no funding or conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Gritti, P., Lanterna, L.A., Rotasperti, L. et al. Clinical evaluation of hyponatremia and hypovolemia in critically ill adult neurologic patients: contribution of the use of cumulative balance of sodium. J Anesth 28, 687–695 (2014). https://doi.org/10.1007/s00540-014-1814-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1814-x