Abstract
Background
Although femoral nerve block provides good analgesia after total knee arthroplasty (TKA), residual posterior knee pain may decrease patient satisfaction. We compared the efficacy of periarticular infiltration analgesia (PIA) and sciatic nerve block (SNB) for posterior knee pain.
Methods
Forty-nine patients scheduled for TKA were prospectively randomized into the PIA group (n = 25) or SNB group (n = 24) and received general anesthesia with ultrasound-guided femoral nerve block (FNB). In the PIA group, 60 ml 0.5 % ropivacaine and 0.3 mg epinephrine were injected intraoperatively into the periarticular soft tissue before inserting the components. In the SNB group, patients received ultrasound-guided SNB with 20 ml 0.375 % ropivacaine and periarticular infiltration with 20 ml normal saline and 0.3 mg epinephrine. We evaluated postoperative pain scores, posterior knee pain, frequency of rescue analgesics for 36 h, and performance time of PIA and SNB.
Results
Visual analogue pain scores at 12–24 h were significantly lower in the PIA group than in the SNB group (p < 0.05). The majority of patients had no posterior knee pain. There were no significant differences between the groups in frequency and time of first administration of rescue analgesics and in side effects. Time for performance of periarticular infiltration was significantly shorter than that for SNB (p < 0.05). The dose of intraoperative remifentanil was significantly lower in the SNB group than in the PIA group (p < 0.001).
Conclusions
The combination of FNB and PIA provides sufficient analgesia after TKA. The rapid and convenient periarticular infiltration technique could be a good alternative to SNB.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known that total knee arthroplasty (TKA) causes severe postoperative pain. Femoral nerve block (FNB), which provides analgesia at the anterior aspect of the knee, shows higher quality of postoperative status after TKA [1] because there are fewer side effects, such as neurological complications, urinary retention, dizziness, sedation, pruritus, nausea, vomiting, and inhibition of motor function in the non-operated limb, than does epidural analgesia [2–4] or patient-controlled analgesia (PCA) with morphine [3, 5]. However, residual posterior knee pain may decrease the patient’s satisfaction. Thus, sciatic nerve block (SNB) in addition to FNB has been suggested to provide better analgesia around the operated knee than FNB alone [6, 7]. Still, the intense motor blockade by SNB may decrease satisfaction with anesthesia.
A possible alternative to peripheral nerve block is the local infiltration analgesia technique. Recently, a convenient local infiltration analgesia technique was developed to reduce postoperative pain [8]. This simple technique is usually performed during surgery by orthopedic surgeons. Although it has been reported that the efficacy of this technique is comparable to that of other analgesic methods including epidural [9], FNB [10], and intrathecal morphine [11], posterior knee pain after TKA has not been investigated.
We hypothesized that periarticular infiltration analgesia (PIA) would be effective for posterior knee pain after TKA, as well as SNB. In this study, we assessed the analgesic effect of PIA around the posterior knee, compared with SNB in patients in whom FNB was performed. Our primary outcome was postoperative pain scores within 36 h. Secondary outcome was existence of posterior knee pain, frequency of rescue analgesics for 36 h, time for performance of each analgesic technique, and dose of intraoperative remifentanil.
Methods
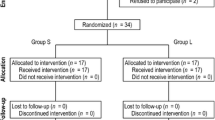
Ethical approval for the study was provided by the Ethics Committee of Obihiro Kyokai Hospital (Obihiro, Japan). All patients provided written informed consent before enrollment in the study. Forty-nine patients with osteoarthritis, who were more than 20 years old, of American Society of Anesthesiologists (ASA) physical status 1–2, and scheduled for elective unilateral TKA under general anesthesia were enrolled. Exclusion criteria were allergy or intolerance to one of the study drugs, renal insufficiency, language difficulty, mental illness, and dementia. Using computerized random number tables and sealed opaque envelopes, subjects were prospectively randomized into the PIA group (n = 25) or SNB group (n = 24).
Preparation
Standard monitoring was used throughout the procedure, including noninvasive arterial pressure, electrocardiogram, and pulse oximetry. Peripheral nerve blocks were performed using an ultrasound device (S-ICU; Sonosite, Bothell, WA, USA) with a high-frequency, 6–13 MHz, linear array transducer. A short-bevel, 22-gauge insulated nerve block needle (Stimuplex D Plus; Braun, Melsungen, Germany) was used for nerve blocks (50 mm for the femoral nerve and 120 mm for the sciatic nerve). A nerve stimulator was not used for these blocks. All blocks and general anesthesia were performed by the same anesthesiologist.
Anesthesia
Before the operation, all patients received ultrasound-guided FNB with 20 ml 0.375 % ropivacaine. In the inguinal region, after identifying the femoral nerve under the fascia iliaca, local anesthetic solution was injected circumferentially around the nerve by the in-plane technique. Success of FNB was defined by loss of cold sensation at the knee by alcohol-wet cotton. General anesthesia was induced with 2 mg/kg propofol and maintained with 1–2 % sevoflurane and 40 % oxygen via an endotracheal tube. Rocuronium 0.8 mg/kg was administered to facilitate tracheal intubation. Intravenous remifentanil was added if surgical anesthesia was deemed inadequate during the surgery. Our criteria for possibly insufficient anesthesia were a heart rate that exceeded preinduction values by 15 % and/or a systolic arterial blood pressure that exceeded baseline values by 20 % for at least 1 min. The total remifentanil dose given throughout the case was recorded. Other opioids were not administered. Patients were divided into two groups (PIA group and SNB group).
PIA group
Periarticular infiltration was performed by the same surgeon after all bony cuts and before cementing the components. A solution containing 0.5 % ropivacaine 60 ml with 0.3 mg epinephrine was injected into the posterior capsule of the knee around the attachment of the posterior cruciate ligament (Fig. 1). Injections were not performed in the anterior part of the knee including subcutaneous tissue.
Periarticular infiltration. Before implantation of the knee replacement system, surgeons injected 60 ml 0.5 % ropivacaine containing 0.3 mg epinephrine in the periarticular infiltration analgesia (PIA) group and 20 ml normal saline containing 0.3 mg epinephrine in the sciatic nerve block (SNB) group into the posterior capsule of the knee
SNB group
Patients received ultrasound-guided SNB by the subgluteal approach before FNB was performed. In the subgluteal region, after identifying the sciatic nerve underneath the gluteus muscle, 20 ml 0.375 % ropivacaine was injected by the in-plane technique. Effect of SNB was confirmed by loss of cold sensation in the lateral part of the lower leg. During surgery, periarticular infiltration was also performed with a solution containing 20 ml normal saline and 0.3 mg epinephrine by the same procedure as that used in the PIA group. In this group, epinephrine was administered to decrease bleeding at the request of the surgeons (in particular, the region around the attachment of the posterior cruciate ligament bleeds easily).
Surgery
All operations were performed using a minimally invasive technique [12]. All patients received the Vanguard Complete Knee System (Biomet, Warsaw, IN, USA). A thigh tourniquet with a pressure of 300 mmHg was used to minimize blood loss from the skin incision and was released after wound closure. A drain tube was left in the knee joint to drain blood after the operation. Antithrombotic therapy with low molecular weight heparin, enoxaparin sodium, was started on the day after surgery and was given for 2 weeks.
Postoperative pain management
All patients were postoperatively medicated with 60 mg oral loxoprofen sodium every 8 h. When necessary, rescue analgesics were given with 50 mg intravenous flurbiprofen or 50 mg suppository diclofenac.
Recordings and measurements
We measured the performance time of periarticular infiltration and ultrasound-guided SNB. We also recorded total remifentanil dose consumption during surgery. The time for performance of ultrasound-guided SNB was defined as the time from the start of needle insertion to completion of administration of local anesthetics. Performance time of PIA was defined from insertion of the needle to completion of injection. The frequency and time of the first administration of rescue analgesics were also recorded for 36 h after the operation. Nurses in the ward, who did not know the group of each patient, evaluated postoperative pain score. The worst pain score during each period of 0–12, 12–24, and 24–36 h postoperatively was estimated by a visual analogue scale (VAS: 0 mm = no pain, 100 mm = worst imaginable pain). The number of patients who had posterior knee pain was also recorded. Incidences of nausea and other adverse effects were recorded on the first postoperative day. Physical therapists, who did not know the group of each patient, assisted with rehabilitation and assessed knee range of motion (ROM) at extension and flexion and Barthel index [13] (daily function score of the activities of daily living and mobility) preoperatively and at discharge. The first postoperative day that the patient started walking and length of postoperative hospital stay were also recorded.
Our primary outcome was postoperative pain scores within 36 h. Secondary outcome was existence of posterior knee pain, frequency of rescue analgesics for 36 h, performance time for each analgesic technique, and dose of intraoperative remifentanil.
Statistics
Power analysis based on detecting a 10-mm difference in VAS scores estimated that 24 patients were required in each group [14]. We therefore included 49 patients in this study. Data were analyzed using the unpaired t test for demographic data, Mann–Whitney U test for comparison of nonparametric data between groups, and Wilcoxon signed-rank test for comparison of pre- and postoperative values within each group. The chi-squared test or Fisher’s exact test was used for other categorical data, and the log-rank significance test was used for the time of first administration of rescue analgesics. A p value < 0.05 was considered to be statistically significant.
Results
Patient characteristics in the two groups were similar (Table 1). There were no major surgical complications from adverse reactions to peripheral nerve blocks or local anesthetic infiltration. Visual analogue pain scores at 12–24 h were significantly lower in the PIA group than in the SNB group (p < 0.05). Only a few patients had posterior knee pain within 2 h after surgery (4.3 % in the PIA group vs. 8.7 % in the SNB group), and most patients had no posterior knee pain (76 % in the PIA group and 73 % in the SNB group) during the period of 36 h after the operation (p = 0.68). Kaplan–Meier analysis of survival curves for patients who did not require rescue analgesia showed no significant difference between the groups (p = 0.078, Fig. 2). Performance time in the PIA group was significantly shorter than that in the SNB group (p = 0.023, Table 2). The dose of intraoperative remifentanil was significantly lower in the SNB group than in the PIA group. There was no significant difference between the two groups in postoperative nausea and vomiting or frequency of rescue analgesics. There were no significant differences in knee ROM and Barthel index after the operation, postoperative physical status, and length of postoperative hospital stay between the groups.
Discussion
TKA consistently results in severe postoperative pain. Although FNB definitely eases post-TKA pain, 80–90 % of patients still experience pain that requires supplemental treatment in the immediate postoperative period [15, 16]. This pain is usually attributed to the sciatic or obturator nerves innervating the knee joint. This study showed that SNB was effective for reducing the amount of intraoperative opioids. To the best of our knowledge, this is the first study to compare the PIA technique with SNB in TKA performed with FNB. Periarticular infiltration decreased postoperative pain to a level comparable to that with SNB. This easy technique provides sufficient postoperative analgesia in the posterior side of the knee.
The posterior knee pain in post-TKA patients cannot be ignored. The benefit of the addition of SNB to FNB is still controversial [1, 17–19]. Three previous randomized controlled trials provided positive evidence that addition of SNB to FNB decreased pain score [6, 19], supplemental opioid requirements [6, 7, 19], and opioid-related adverse effects [6]. As this study has shown, SNB are effective during the operation and significantly decreased intraoperative remifentanil dose. However, there are several disadvantages of SNB. First, the combination of FNB and SNB causes intense paralysis and it is often unacceptable not only for patients but also orthopedic surgeons, who require immediate estimation of lower extremity function after TKA [6, 7]. Second, accurate ultrasound-guided SNB is time consuming regardless of operator skill or insertion technique [20]. Moreover, possible risks of hematoma or nerve injury by needle puncture or catheterization sometimes narrow the indication of SNB [21, 22], especially for patients with coagulation abnormalities. PIA, a convenient technique that has become popular, is easy to perform and takes much less time than SNB. Following initial reports of success using periarticular infiltration of high-volume local anesthetics in TKA [23], recent open and randomized studies have confirmed that this technique significantly reduced the intensity of postoperative pain and consumption of rescue analgesics [8, 24, 25]. This simple technique can always provide a reliable effect, whereas effects of peripheral nerve blocks might depend on the technique and experience of the anesthesiologist. PIA affects only the sensory nerve around the infiltrated area without motor dysfunction and has indication for patients with anticoagulant disorders or antithrombotic therapy, even in cases in which deep peripheral nerve blocks should be avoided. Our data indicate that PIA and SNB provided similar quality of pain relief after TKA in cases combined with FNB. Although the dose of intraoperative remifentanil was significantly lower in the SNB group than in the PIA group, the quality of postoperative analgesia was similar. It is reasonable that SNB was more effective during the operation, because SNB was performed before the operation.
The PIA technique for TKA in previous studies was performed in almost all parts around the knee including the capsule incision, quadriceps tendon, infrapatellar ligament, and subcutaneous tissue [11, 26], or vastus intermedius and lateralis [10]. In the present study, local anesthetics were injected only into the posterior capsule and the attachment of the posterior cruciate ligament because sufficient analgesia at the anterior part of the knee was assumed to be provided by FNB. Within 2 h after surgery, more than 90 % of the patients in the PIA group had no popliteal pain, and analgesic quality and side effects in those patients were the same as those in the SNB group. There has been no focus on “popliteal pain” with each analgesic method in studies on TKA. Our results suggest that local infiltration in the dorsal side of the knee provides sufficient analgesia and is an alternative to SNB.
Several types of drugs have been administered for PIA. The long-acting local anesthetics ropivacaine and levobupivacaine are useful as local infiltration analgesics [23, 25, 27, 28]. Ketorolac, a nonsteroidal anti-inflammatory drug (NSAID), is administered systemically and has recently been shown to be an effective adjuvant to local anesthetic drugs [27, 29]. Spreng et al. [30] reported that local administration of ketorolac and morphine had significantly stronger effects on postoperative pain than did intravenous administration. However, it is not clear whether local administration of NSAIDs or opioids can improve postoperative pain. Tissue damage caused by local administration of NSAIDs is also uncertain. It is known that NSAIDs and opioids are effective by systemic administration; however, it is still controversial how these drugs have effects when administrated locally.
There are some limitations in our study. First, we used 300 mg ropivacaine (in 60 ml) for the local infiltration technique. However, the local infiltration technique is limited to the posterior part of the knee, and the total amount of ropivacaine could be reduced. Although the plasma concentration of ropivacaine seems to be below a systematic toxic level when high-volume PIA is used [31], it should be noted that there is a risk of local anesthetic toxicity as a possible adverse effect of the combination of peripheral nerve block and PIA. Further studies are needed to determine optimal dose and volume of local anesthetics. Second, the effect of additional epinephrine injected with saline in SNB group is uncertain. It might have had some effects on postoperative pain scores. Third, NSAIDs administration might not be sufficient for postoperative pain management after TKA. Although frequency of rescue analgesics is not our primary outcome, further investigation is needed for precise evaluation of postoperative analgesia.
In conclusion, the combination of FNB and PIA provides sufficient analgesia after TKA. Although SNB could decrease opioid consumption during the operation, PIA using ropivacaine and epinephrine could provide sufficient analgesia in the posterior part of the knee with potentially the same analgesic effect as that of SNB. This study suggests that the rapid and convenient periarticular infiltration technique could be a good alternative to SNB. Further studies should be performed to clarify optimal dose and a better drug combination for local infiltration.
References
Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A, Murthy Y. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113:1144–62.
Zaric D, Boysen K, Christiansen C, Christiansen J, Stephensen S, Christensen B. A comparison of epidural analgesia with combined continuous femoral-sciatic nerve blocks after total knee replacement. Anesth Analg. 2006;102(4):1240–6.
Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998;87:88–92.
Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d’Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;91:8–15.
Raj PP, Knarr DC, Vigdorth E, Denson DD, Pither CE, Hartrick CT, Hopson CN, Edström HH. Comparison of continuous epidural infusion of a local anesthetic and administration of systemic narcotics in the management of pain after total knee replacement. Anesth Analg. 1987;66:401–6.
Pham Dang C, Gautheron E, Guilley J, Fernandez M, Waast D, Volteau C, Nguyen JM, Pinaud M. The value of adding sciatic block to continuous femoral block for analgesia after total knee replacement. Reg Anesth Pain Med 2005;30:128–133
Morin AM, Kratz CD, Eberhart LH, Dinges G, Heider E, Schwarz N, Eisenhardt G, Geldner G, Wulf H. Postoperative analgesia and functional recovery after total-knee replacement: comparison of a continuous posterior lumbar plexus (psoas compartment) block, a continuous femoral nerve block, and the combination of a continuous femoral and sciatic nerve block. Reg Anesth Pain Med. 2005;30:434–45.
Andersen LO, Husted H, Otte KS, Kristensen BB, Kehlet H. High-volume infiltration analgesia in total knee arthroplasty: a randomized, double-blind, placebo-controlled trial. Acta Anaesthesiol Scand. 2008;52:1331–5.
Andersen KV, Bak M, Christensen BV, Harazuk J, Pedersen NA, Søballe K. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop 2010;81(5):606–610
Affas F, Nygårds EB, Stiller CO, Wretenberg P, Olofsson C. Pain control after total knee arthroplasty: a randomized trial comparing local infiltration anesthesia and continuous femoral block. Acta Orthop. 2011;82(3):441–7.
Essving P, Axelsson K, Åberg E, Spenner H, Gupta A, Lundin A. Local infiltration analgesia versus intrathecal morphine for postoperative pain management after total knee arthroplasty: a randomized controlled trial. Anesth Analg 2011;113(4):926–933
Reid JB 3rd, Guttmann D, Ayala M, Lubowitz JH. Minimally invasive surgery-total knee arthroplasty. Arthroscopy. 2004;20(8):884–9.
Mahoney FI, Barthel DW. The Barthel index. Md State Med J. 1965;14:61–5.
Ward M, Minto G, Alexander-Williams JM. A comparison of patient-controlled analgesia administered by the intravenous or intranasal route during the early postoperative period. Anesthesia. 2002;57:48.
Ilfeld BM, Le LT, Meyer RS, Mariano ER, Vandenborne K, Duncan PW, Sessler DI, Enneking FK, Shuster JJ, Theriaque DW, Berry LF, Spadoni EH, Gearen PF. Ambulatory continuous femoral nerve blocks decrease time to discharge readiness after tricompartment total knee arthroplasty: a randomized, triple-masked, placebo-controlled study. Anesthesiology. 2008;108:703–13.
Ilfeld BM, Mariano ER, Girard PJ, Loland VJ, Meyer RS, Donovan JF, Pugh GA, Le LT, Sessler DI, Shuster JJ, Theriaque DW, Ball ST. A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedic wards. Pain. 2010;150:477–84.
Abdallah FW, Brull R. Is sciatic nerve block advantageous when combined with femoral nerve block for postoperative analgesia following total knee arthroplasty? A systematic review. Reg Anesth Pain Med 2011;36(5):493–498.
Fischer HB, Simanski CJ, Sharp C, Bonnet F, Camu F, Neugebauer EA, Rawal N, Joshi GP, Schug SA, Kehlet H, PROSPECT Working Group. A procedure-specific systematic review and consensus recommendations for postoperative analgesia following total knee arthroplasty. Anaesthesia. 2008;63:1105–23.
Wegener JT, Dijk NV, Hollmann MW, Preckel B, Stevens MF. Value of single-injection or continuous sciatic nerve block in addition to a continuous femoral nerve block in patients undergoing total knee arthroplasty: a prospective, randomized, controlled trial. Reg Anesth Pain Med. 2011;36:481–8.
Mariano ER, Cheng GS, Choy LP, Loland VJ, Bellars RH, Sandhu NS, Bishop ML, Lee DK, Maldonado RC, Ilfeld BM. Electrical stimulation versus ultrasound guidance for popliteal-sciatic perineural catheter insertion: a randomized controlled trial. Reg Anesth Pain Med. 2009;34:480–5.
Ilfeld BM. Continuous peripheral nerve blocks: a review of the published evidence. Anesth Analg 2011;113(4):904–925
Brull R, McCartney CJ, Chan VW, El Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104:965–74.
Kerr DR, Kohan L. Local infiltration analgesia: a technique for the control of acute postoperative pain following knee and hip surgery: a case study of 325 patients. Acta Orthop. 2008;79:174–83.
Vendittoli PA, Makinen P, Drolet P, Lavigne M, Fallaha M, Guertin MC, Varin F. A multimodal analgesia protocol for total knee arthroplasty. A randomized, controlled study. J Bone Joint Surg Am. 2006;88:282–9.
Busch CA, Shore BJ, Bhandari R, Ganapathy S, MacDonald SJ, Bourne RB, Rorabeck CH, McCalden RW. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006;88:959–63.
Carli F, Clemente A, Asenjo JF, Kim DJ, Mistraletti G, Gomarasca M, Morabito A, Tanzer M. Analgesia and functional outcome after total knee arthroplasty: periarticular infiltration vs. continuous femoral nerve block. Br J Anaesth. 2010;105(2):185–95.
Brill S, Plaza M. Non-narcotic adjuvants may improve the duration and quality of analgesia after knee arthroscopy: a brief review. Can J Anaesth. 2004;51:975–8.
Murphy TP, Byrne DP, Curtin P, Baker JF, Mulhall KJ. Can a periarticular levobupivacaine injection reduce postoperative opiate consumption during primary hip arthroplasty? Clin Orthop Relat Res. 2012;470:1151–7.
Rømsing J, Møiniche S, Ostergaard D, Dahl JB. Local infiltration with NSAIDs for postoperative analgesia: evidence for a peripheral analgesic action. Acta Anaesthesiol Scand. 2000;44(6):672–83.
Spreng UJ, Dahl V, Hjall A, Fagerland MW, Ræder J. High-volume local infiltration analgesia combined with intravenous or local ketorolac + morphine compared with epidural analgesia after total knee arthroplasty. Br J Anaesth. 2010;105(5):675–82.
Essving P, Axelsson K, Kjellberg J, Wallgren O, Gupta A, Lundin A. Reduced morphine consumption and pain intensity with local infiltration analgesia (LIA) following total knee arthroplasty. Acta Orthop 2010;81(3):354–360.
Acknowledgments
No external funding or conflicts of interest are declared.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Gi, E., Yamauchi, M., Yamakage, M. et al. Effects of local infiltration analgesia for posterior knee pain after total knee arthroplasty: comparison with sciatic nerve block. J Anesth 28, 696–701 (2014). https://doi.org/10.1007/s00540-014-1793-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1793-y