Abstract
Background
Almost a quarter century has passed since the first nationwide survey on ulcerative colitis (UC) and Crohn’s disease (CD) was conducted in Japan. In this study, we used a nationwide survey to estimate the number of patients and prevalence of these diseases in Japan in 2014.
Methods
We conducted a mail-based survey targeting hospitals to estimate the annual numbers of patients with UC and CD in 2014. Respondents were asked to report the numbers of patients who met specific diagnostic criteria for these two conditions. A stratified random sampling method was used, and a total of 3712 departments (internal medicine, surgery, pediatrics, and pediatric surgery) were selected for analysis. The overall and sex-specific annual numbers of UC and CD patients were estimated. The corresponding prevalence rates per 100,000 population were calculated by dividing the number of patients with each disease by the mid-year population of Japan in 2014.
Results
The overall survey response rate was 56.7% (2016 departments). The estimated numbers of patients with UC and CD were 219,685 (95% confidence interval: 183,968–255,403) and 70,700 (56,702–84,699), respectively. The annual prevalence rates of UC and CD per 100,000 population were 172.9 (men: 192.3; women: 154.5) and 55.6 (men: 79.5; women: 33.1), respectively. These numbers are almost tenfold increase in comparing the previous survey (22,300 in UC and 7,400 in CD). The male-to-female ratios were 1.24 for UC and 2.40 for CD, and the UC-to-CD ratio was 3.11.
Conclusions
The prevalence of UC and CD in Japan has risen substantially over the past two decades, and their disease burden requires further examination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel diseases (IBDs), which include ulcerative colitis (UC) and Crohn’s disease (CD), refer to chronic inflammatory diseases of the gastrointestinal tract. Although these conditions are prevalent in North America, Western Europe, and Scandinavia, they are generally less common in Eastern Europe and Asia [1, 2]. However, recent epidemiological studies have suggested that IBD incidence is rising rapidly in South America, Eastern Europe, Asia, and Africa [3]. To determine the need for interventions and care programs for a disease, it is important to monitor its distribution and potential burden. This is especially important for diseases with unknown etiology, such as IBDs.
UC and CD are designated intractable diseases in Japan, and the majority of patients with such diseases are enrolled in a national registry [4]. Although this registry is not include all IBD patients, the data indicate that the number of IBD patients has increased over time in Japan, as in other Asian countries [3, 5, 6]. As Japan is one of the most westernized nations in Asia and IBD tends to be more prevalent in these countries [3], the apparent increase in IBD incidence in Japan has attracted much attention. Despite the need to confirm this disease trend, almost a quarter century has passed since the first nationwide survey was conducted in Japan to quantify the prevalence of UC and CD [7]. Here, we conducted a nationwide epidemiological survey to estimate the number of patients with UC and CD, as well as to measure the prevalence of these conditions throughout Japan in 2014.
Methods
In this study, we conducted a nationwide epidemiological survey targeting hospitals to estimate the number of patients with UC and CD in the Japanese population. This mail-based survey was performed in accordance with the standardized procedures proposed by the Research Committee on the Epidemiology of Intractable Diseases in Japan [8]. The survey, which used a self-administered questionnaire, was conducted between December 2014 and March 2015.
A stratified random sampling method was applied to estimate the annual numbers of IBD patients in Japan. When a complete survey is not possible, a sample survey such as a stratified random sampling is an efficient way to estimate the number of people in the population. In our study, we sampled medical departments from all hospitals in Japan, and a total of 3712 medical departments were selected for analysis. Stratified sampling was conducted based on (1) the type of medical department and (2) the number of beds and hospital type (i.e., university hospitals and specialized hospitals for treating inflammatory bowel diseases). For the type of medical department, the target hospitals were stratified into the following four categories: internal medicine, surgery, pediatrics, and pediatric surgery. For the number of beds and hospital type, the target hospitals were stratified into the following eight categories (with their respective sampling fractions): University hospitals (100%), specialized hospitals (100%), ≥ 500 beds (100%), 400–499 beds (80%), 300–399 beds (40%), 200–299 beds (20%), 100–199 beds (10%), and < 99 beds (5%). Total 32 categories, derived from the type of medical departments and beds numbers, were set to conduct this stratified random sampling survey.
To ensure the accuracy and standardization of patient diagnoses, we included specific diagnostic criteria for UC and CD [9, 10] in the questionnaire. The questionnaire was sent to each sampled department, and physicians in the department were asked to report the sex-specific numbers of patients with UC and confirmed CD during 2014. Reminder letters were sent to departments that had not returned the questionnaire within the study period.
The annual numbers of patients of each strata were estimated by multiplying the reported patient numbers, which was collected from the questionnaire, by the reciprocal of the survey response rate and sampling rate [11].
Overall and sex-specific annual prevalence rates in the Japanese population were estimated using national vital statistics in 2014 [12]. Specifically, the mid-year population was used to calculate prevalence rates per 100,000 population. The study protocol was approved (Approval Number: 27086) by the Ethics Committee of the Faculty of Medicine, Toho University (Tokyo, Japan).
Results
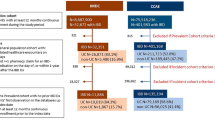
Table 1 shows the number of institutions that were sampled and the number that responded in this nationwide survey. A total of 3712 hospital departments were sampled through stratified random sampling (internal medicine: 1561; surgery: 1097; pediatrics: 841; and pediatric surgery: 213), and the overall response rate was 56.7% (2106/3712 departments). Among the bed number and hospital type categories, the response rate was highest in university hospitals (81.7%).
Table 2 presents the estimated numbers of patients with UC in 2014 according to the medical department type and the number of beds/hospital type. There were 219,685 UC patients (95% confidence interval [CI] 183,968–255,403), with 118,841 (99,792–137,890) men and 100,844 (83,886–117,803) women. Table 3 presents the estimated numbers of patients with CD in 2014 according to the medical department type and the number of beds/hospital type. There were 70,700 CD patients (95% CI 56,702–84,699), with 49,107 (38,937–59,277) men and 21,593 (17,687–25,500) women.
The estimated annual prevalence rates of UC and CD per 100,000 population based on the mid-year population of Japan in 2014 were 172.9 (192.3 in men and 154.5 in women) and 55.6 (79.5 in men and 33.1 in women), respectively (Table 4). The male-to-female ratios were 1.24 for UC and 2.40 for CD. The UC-to-CD ratio was 3.11 (172.9/55.6).
Discussion
Using a nationwide survey, we estimated that there were 219,700 patients with UC and 70,700 patients with CD throughout Japan in 2014. The first nationwide survey for IBD in Japan was conducted in 1991, of which the method they used was same as we used in the present study. This survey reported an estimated 22,300 patients with UC and 7400 patients with CD at that time [7]. This survey also showed that the overall and sex-specific prevalence rates of UC (1.95 (male: 2.23, female: 1.68) and CD (0.51 (male: 0.71, female: 0.32)). The results of these two surveys indicate an almost tenfold increase in patients with IBD over the span of 23 years. These surveys were conducted using a standardized protocol for intractable diseases that was developed by epidemiologists and biostatisticians [11], and which has been applied to estimate the annual prevalence of various intractable diseases [8, 13, 14]. The number of patients per medical institution, reported in Tables 2 and 3, indicated that the large amount of patients with UC and CD took medical care at the internal department of large hospitals such as University hospitals and specialized hospitals. UC and CD are designated intractable diseases and generally require specialized treatment and care. Accordingly, patients with these conditions are far more likely to be treated at larger hospitals with the required resources.
Japan has implemented a national registry for people with intractable diseases (including UC and CD), and registered patients are eligible to receive financial aid from the government [4]. According to a government report on public health administration and services in 2015, there were 166,085 registered patients with UC and 41,279 registered patients with CD [15]. These figures were substantially lower than those from our nationwide survey. We postulate that not all patients with IBD would enroll in the national registry. For example, wealthier individuals or those with other forms of financial support may not enroll in the registry as they have no need for the subsidies. In addition, patients with milder forms of IBD may have a lower registration rate. In contrast, our survey was based on patients who fulfilled the specified diagnostic criteria, irrespective of whether they were enrolled in the national registry. We believe that this approach provides a more accurate estimate of patients with these diseases.
In this study, the estimated annual prevalences of UC and CD per 100,000 population in 2014 were approximately 173 and 56, respectively. Although it is difficult to compare prevalences among countries due to inherent differences in target populations and epidemiological methods, a recent systematic review reported that the highest prevalences per 100,000 population were in Europe (UC: 505 in Norway; CD: 322 in Germany) and North America (UC: 286 in the USA; CD: 319 in Canada) [3]. In this review, range in prevalence of IBD per 100,000 population in Eastern Asia region was 1 (Taiwan) to 19 (Japan) in CD, and 5 (Taiwan) to 57 (Japan), respectively. The highest prevalences per 100,000 population in Asia region were 106 for UC (Beirut, Lebanon) and 53 for CD (Beirut, Lebanon) [3], which were slightly lower than the values reported in our survey.
The UC-to-CD ratio varies among geographic regions. For example, CD appears to be more dominant in the US and Canada, whereas there is a relatively higher incidence of UC in the Nordic countries [2, 16]. A study in the Asia–Pacific region found that the incidence ratio of UC to CD was approximately 2.0 in Asia and 0.5 in Australia [17]. However, the UC-to-CD ratio has been reported to decrease over time. In China, the ratio dropped from 41 in 1989–2003 to 15 in 2004–2007 [18]. In South Korea, the ratio also declined from 6.8 in 1986–1990 to 2.3 in 2001–2005 [19]. Based on the previous national survey [7] and our present analysis, the UC-to-CD ratio in Japan was found to have declined slightly from 3.82 in 1991 to 3.11 in 2014.
Studies from Western and Asian countries have reported generally similar sex distributions for UC [1, 20, 21]. In contrast, a male predominance for CD was observed in Asian countries (with male-to-female ratios ranging from 1.67 to 2.9), whereas a female predominance has been reported in Western countries [21]. We posit that smoking is a plausible risk factor for explaining this sex difference in CD prevalence. A meta-analysis has shown that while smoking is a risk factor for CD, it has a protective effect for UC [22]. These differential effects may influence the patterns of sex distribution between UC and CD. The variations in male-to-female ratios among different regions is interesting and may shed light on the etiology of CD, and should, therefore, be examined in more detail in the future.
This study has several limitations that should be considered when interpreting these findings. First, we did not consider possible duplicate counts of patients who sought care at multiple hospitals. In the previous survey conducted in 1991 [7], duplicate patients comprised only 0.9% of the sample and their influence appeared to be small. Second, the number of patients with IBD may have been underestimated as our survey did not include clinics (defined in Japan to be medical institutions with 19 or fewer beds). However, UC and CD are designated intractable diseases and generally require specialized treatment and care. As shown in Tables 2 and 3, patients with these conditions are far more likely to be treated at larger hospitals with the required resources. Therefore, we believe that the non-inclusion of clinics would not have a substantial effect on our CD findings. Third, our analysis estimated the prevalence of UC and CD, but not their incidence. Although the measurement of incidence is important from both the clinical and public health viewpoints, there are practical difficulties associated with the identification of new cases, especially in a nationwide survey. In addition, the prevalence of chronic diseases such as UC and CD represents an important indicator of overall disease burden. Fourth, our study did not show any age-specific information. Our study focused on a precise estimation of the overall number of IBD patients in Japan and an age-specific numbers was out of focus in this study. A conduct of an age-specific estimation is impracticable because fairly number of sample size and large budget for study are needed.
Despite these limitations, our study showed that UC and CD are currently more prevalent in Japan than 23 years ago. The exact reasons for this increase are unknown, but may be partially explained by a higher awareness of IBD in physicians, advancements in diagnostic methods (such as colonoscopies) and treatments, and changes in dietary habits in the Japanese population.
Conclusions
The estimated number of patients with UC and CD in Japan has risen substantially over the past 23 years. Further studies are needed to determine the clinical and economic burden of these conditions, and to ascertain the need for interventions or changes to resource allocation.
Change history
23 October 2019
The authors would like to correct the errors in the publication of the original article.
Abbreviations
- UC:
-
Ulcerative colitis
- CD:
-
Crohn’s disease
- IBD:
-
Inflammatory bowel disease
- CI:
-
Confidence interval
References
Ng SC. Epidemiology of inflammatory bowel disease: focus on Asia. Best Pract Res Clin Gastroenterol. 2014;28:363–72.
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–544.
Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390:2769–78.
Ministry of Health, Labour and Welfare. Annual Health, Labour and Welfare Report 2017. https://www.mhlw.go.jp/english/wp/wp-hw11/dl/02e.pdf. Accessed 9 Nov 2018.
Japan Intractable Disease Information Center. Ulcerative colitis. https://www.nanbyou.or.jp/entry/62. Accessed 9 Nov 2018 (in Japanese).
Japan Intractable Disease Information Center. Crohn’s disease. https://www.nanbyou.or.jp/entry/81. Accessed 9 Nov 2018 (in Japanese).
Morita N, Toki S, Hirohashi T, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995;30(Suppl 8):1–4.
Nakamura Y, Matsumoto T, Tamakoshi A, et al. Prevalence of idiopathic hypoparathyroidism and pseudohypoparathyroidism in Japan. J Epidemiol. 2000;10:29–33.
Ueno F, Matsui T, Matsumoto T; Guidelines Project Group of the Research Group of Intractable Inflammatory Bowel Disease subsidized by the Ministry of Health, Labour and Welfare of Japan and the Guidelines Committee of the Japanese Society of Gastroenterology. Evidence-based clinical practice guidelines for Crohn's disease, integrated with formal consensus of experts in Japan. J Gastroenterol. 2013;48:31–72.
Matsuoka K, Kobayashi T, Ueno, et al. Evidence-based clinical practice guidelines for inflammatory bowel disease. J Gastroenterol. 2018;53:305–53.
Hashimoto S, Fukutomi K, Nagai M, et al. A method of interval estimation for number of patients in the nationwide epidemiological survey on intractable diseases [in Japanese]. Nippon Koshu Eisei Zasshi. 1991;38:880–3.
Ministry of Health, Labour and Welfare. Vital statistics of Japan. Health. Tokyo, Japan: Labour and Welfare Statistics Association; 2014. p. 2016.
Mano H, Fujiwara S, Takamura K, et al. Congenital limb deficiency in Japan: a cross-sectional nationwide survey on its epidemiology. BMC Musculoskelet Disord. 2018;19:262.
Fukushima W, Fujioka M, Kubo T, et al. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res. 2010;468:2715–24.
Ministry of Health, Labour and Welfare. The report on public health administration and services 20https://www.e-stat.go.jp/stat-search/files?page=1&layout=datalist&toukei=00450027&tstat=000001031469&cycle=8&tclass1=000001090415&tclass2=000001090416&tclass3=000001090417&second2=1. Accessed 9 Nov 2018 (in Japanese).
Moum B, Vatn MH, Ekbom A, et al. Incidence of inflammatory bowel disease in southeastern Norway: evaluation of methods after 1 year of registration. Southeastern Norway IBD Study Group of Gastroenterologists. Digestion. 1995;56:377–81.
Ng SC, Tang W, Ching JY, et al; Asia-Pacific Crohn's and Colitis Epidemiologic Study (ACCESS) Study Group. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-pacific Crohn's and colitis epidemiology study. Gastroenterology. 2013;145:158–65.
Wang YF, Ouyang Q, Hu RW. Progression of inflammatory bowel disease in China. J Dig Dis. 2010;11:76–82.
Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: a KASID study. Inflamm Bowel Dis. 2008;14:542–9.
Asakura K, Nishiwaki Y, Inoue N, et al. Prevalence of ulcerative colitis and Crohn's disease in Japan. J Gastroenterol. 2009;44:659–65.
Thia KT, Loftus EV Jr, Sandborn WJ, et al. An update on the epidemiology of inflammatory bowel disease in Asia. Am J Gastroenterol. 2008;103:3167–82.
Mahid SS, Minor KS, Soto RE, et al. Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clin Proc. 2006;81:1462–71.
Acknowledgements
This work was supported by Health and Labour Sciences Research Grants for Research on Intractable Diseases from the Japanese Ministry of Health, Labour and Welfare (H26–28).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
All the authors declare that there are no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Murakami, Y., Nishiwaki, Y., Oba, M.S. et al. Estimated prevalence of ulcerative colitis and Crohn’s disease in Japan in 2014: an analysis of a nationwide survey. J Gastroenterol 54, 1070–1077 (2019). https://doi.org/10.1007/s00535-019-01603-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-019-01603-8