Abstract
Background
Patients with primary biliary cholangitis (PBC) frequently suffer from pruritus, which can severely impair their health-related quality of life (HRQOL). Nalfurafine hydrochloride, a selective κ-opioid receptor agonist, was recently approved in Japan for refractory pruritus in patients with chronic liver diseases, but it still remains unclear whether this treatment improves the patient-reported outcome (PRO) in PBC patients with refractory pruritus. Herein, we conducted a multicenter, post-marketing, single-arm prospective study to investigate the efficacy of nalfurafine in terms of PRO, and the associations of the efficacy with any clinical characteristics.
Methods
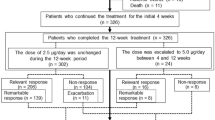
After screening for pruritus in 496 patients with PBC using PBC-40 and the visual analog scale (VAS), we identified 141 patients with moderate to severe pruritus; these were invited to participate in the study. The participants received 2.5 μg nalfurafine once daily for 12 weeks, and pruritus and HRQOL were assessed in week 12 of this treatment. Generic HRQOL, short form 36, blood chemistries, and serum autotaxin levels were also measured at baseline and at week 12.
Results
Forty-four patients participated in this study. The mean PBC-40 itch domain scores and VAS declined during the study period, from 8.56 to 7.63 (P = 0.041) and from 42.9 to 29.3 (P = 0.001) at baseline and at week 12, respectively, indicating a significant effect of nalfurafine. The other domains of PBC-40 and all domains of SF-36 were not significantly altered by this treatment. We failed to find any association between the change in VAS and PBC-40 itch scores and any clinical variable. Serum autotaxin levels were significantly increased during the study period.
Conclusions
This study demonstrated that nalfurafine improved pruritus in patients with PBC, independent of their clinical characteristics, but had a limited effect on the PRO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary biliary cholangitis (PBC) is a chronic cholestatic liver disease characterized by immune-mediated destruction of small and medium intrahepatic bile ducts [1, 2]. A substantial proportion of patients with PBC suffer from a variety of subjective symptoms. One of the most troubling of these is pruritus [3], which can severely impair health-related quality of life (HRQOL) [4,5,6]. Pruritus can occur at any stage of PBC in a local or generalized manner, and can significantly disturb daily life and disrupt sleep at night. The pathophysiologic mechanism underlying pruritus is largely unknown, although cholestasis definitely plays a key role [7]. Ursodeoxycholic acid (UDCA), a first-line therapeutic medication for PBC, does not ameliorate pruritus [8]. Bile sequestrants such as rifampicin and anti-histamines are used to alleviate pruritus. However, the efficacies of these therapeutic options are limited, and liver transplantation is required to address severe pruritus in some patients [2, 9, 10]. Therefore, new therapeutic approaches for the treatment of pruritus are strongly required.
Neurotransmission involving opioid receptors is known to play a significant role in pruritus. Serum levels of β-endorphin, an endogenous opioid, are elevated in patients with severe pruritus. Two opioid receptors are involved in pruritus signaling in the central nervous system; μ-receptors are stimulatory and κ-receptors are inhibitory. Antagonists of the μ-opioid receptor, such as naloxone or naltrexone, exhibited anti-pruritic effects in patients with cholestasis [11, 12]. Similarly, the use of κ-opioid receptor agonists could provide a rational approach to the treatment of pruritus.
Nalfurafine hydrochloride is a selective κ-opioid receptor agonist that has been approved as an anti-pruritic drug in hemodialysis patients with refractory pruritus [13]. The efficacy and safety of nalfurafine was previously investigated in a phase 3 randomized double-blind trial involving 318 patients with chronic liver diseases, including PBC [14]. Pruritus, measured using the visual analog scale (VAS), was significantly decreased by week 4 of oral nalfurafine administration, and the safety issues were acceptable [14]. However, although 87 patients with PBC were included in this study, only 30 patients were assigned to receive 2.5 μg daily, which is the usual dose of this compound. Furthermore, pruritus was measured by VAS only, and patient-reported outcomes (PRO) were not assessed using PBC-40 or the short form 36 (SF-36). Finally, these 30 patients were not analyzed in detail as a subgroup in this study, and it is therefore unclear whether the efficacy of nalfurafine is influenced by clinical characteristics such as age, sex, blood chemistry, and progression of PBC. Very recently, a large-scale, post-marketing study was published, demonstrating the efficacy of nalfurafine [15]. Although this study employed 673 patients with chronic liver diseases, only 38 patients with PBC were included and the details of these patients were obscure.
The current multicenter, post-marketing, single-arm prospective study aimed to clarify whether the PRO of PBC patients with moderate to severe pruritus, measured using PBC-40, SF-36, and VAS, were improved by treatment with nalfurafine. We also examined whether clinical variables were associated with any change in the level of pruritus following nalfurafine administration. In addition, we sampled serum from the study participants at baseline and investigated whether pruritus was associated with the level of autotaxin, which was previously reported to be associated with pruritus severity in patients with cholestasis [16].
Patients and methods
Screening of patients
We identified patients with PBC who were experiencing moderate to severe pruritus, and invited them to participate in the current study. The pruritus screening procedure was designed as a separate observational cross-sectional study, which was approved by the Ethics Committee of Teikyo University (approval no. 14-186); the results of this study have been described elsewhere [17]. In brief, we invited consecutive patients who presented with PBC at the outpatient clinics of each study center between July 1st, 2015, and October 31st, 2016. Diagnosis of PBC was made using established criteria, which required two or more of the following symptoms: chronic elevation of cholestatic liver enzymes, detectable anti-mitochondrial antibodies in sera, and compatible or diagnostic liver histology [10]. We asked patients to complete questionnaires to assess their symptoms and HRQOL (the Japanese version of PBC-40 and the SF-36), and assessed pruritus severity using the VAS. Patients were not invited to participate if they were being admitted to hospital, had a history of liver transplantation, had other liver diseases including autoimmune hepatitis, or had other comorbidities which were likely to affect their HRQOL. Consequently, 496 patients with PBC (male/female = 53/443; 66.0 ± 9.9 years old) agreed to complete the Japanese version of PBC-40 and SF-36.
Pruritus and HRQOL assessment tools
We employed the Japanese version of PBC-40 and SF-36 to assess symptoms and HRQOL in patients with PBC. PBC-40 is a patient-derived, disease-specific measure of symptoms and HRQOL that covers 6 domains: symptoms, itch, fatigue, cognition, social, and emotional. The acceptability, reliability, construct validity, and precision of this tool has been validated previously [18]. Participants were asked to select one of the following responses: never, rarely, sometimes, most of the time, or always, and these corresponded to scores of 1–5 points [19]. The itch domain included 3 items: Question 8, “Itching disturbed my sleep most of the time”; Question 9, “I scratched so much I made my skin raw”; and Question 10: “I felt embarrassed because of the itching”. The scores for the whole itch domain thus ranged from 3 to 15. Our screening process defined the severity of pruritus into the following four categories: “none” if the score was 0; “mild” if the score ranged from 1 to 5; “moderate” for scores between 6 and 10; and “severe” for scores between 11 and 15. This procedure classified 199, 156, 117, and 24 patients as “none”, “mild”, “moderate”, and “severe”, respectively; 141 patients were thus evaluated as experiencing moderate to severe pruritus, and were considered as potential candidates for nalfurafine treatment.
The SF-36 is a questionnaire used to measure general health status. In the SF-36, one item is designed to assess the perceived change in health status, and each of the remaining 35 items contributes to a score on one of eight scales: physical functioning; role-physical; bodily pain; general health perception; vitality; social functioning; role-emotional; and mental health [20]. The Japanese version of SF-36 was already established and has been validated previously [21, 22].
Nalfurafine intervention
We invited 141 patients with moderate to severe pruritus to participate in the current interventional study of nalfurafine (https://clinicaltrials.gov/ NCT02659696; UMIN000021681). This study was designed and conducted by the Japan PBC Study Group (JPBCSG), and approved by the Ethics Committee of Teikyo University (Approval no. 15-037) and other participating centers. Patients with moderate to severe pruritus who agreed to participate in the current study received once-daily oral nalfurafine (Toray Industries, Inc., Tokyo, Japan) at a dose of 2.5 μg for 12 weeks. Pruritus severity and HRQOL were evaluated again at week 12 using PBC-40, SF-36, and VAS. In patients receiving other anti-pruritic drugs such as bile acid sequestrants, anti-histamines, and moisturizing agents, the dosages of these were fixed throughout the study period and any additional treatments were prohibited. Detailed clinical information was collected at baseline and at the end of the treatment period. These data included the date of diagnosis, liver histological stage at diagnosis (if liver biopsy was performed), liver biochemistry, and clinical events such as jaundice, ascites, edema, hepatic encephalopathy, esophageal or gastric varices, and hepatocellular carcinoma. Additionally, we collected sera from the patients at baseline and the end of treatment to measure serum autotaxin levels.
Statistical analyses
All statistical analyses were performed using SPSS® Statistics version 22 (IBM Japan, Tokyo, Japan). Continuous variables are presented as the mean ± the standard deviation if normally distributed, or median (interquartile range) otherwise. We excluded the prothrombin time and international normalization ratio from the analysis because the missing data rates for these two variables were exceptionally high (33 and 39%, respectively). The Pearson correlation efficient was used to assess the correlation between VAS, PBC-40, and SF-36, and between continuous variables and VAS/PBC-40 itch scores. Comparisons between values at baseline and at week 12 were performed using a paired Student’s t test for continuous and normally distributed variables, and the Mann–Whitney U test for variables without normal distribution. A result was considered to be statistically significant when the P value was < 0.05.
Results
Study participants
A total of 44 patients with PBC agreed to participate in this interventional study, and their clinical characteristics are shown in Table 1. The serum alkaline phosphatase level was > 1.5 × ULN in 7 patients, and serum bilirubin was > 1.5 mg/dL in only 1 patient (1.7 mg/dL). Although all participants were currently attending outpatient clinics, one or more clinical events (jaundice, ascites, edema, hepatic encephalopathy, esophageal or gastric varices, or hepatocellular carcinoma) had occurred previously in 9 (20.9%) of the patients. Treatment with UDCA and bezafibrate was recorded in 43 (97.7%) and 6 (13.6%) of the patients, respectively.
Changes in PBC-40 scores
First, we examined whether pruritus, measured by the itch domain of PBC-40, was improved by treatment with nalfurafine. The mean scores for this PBC-40 domain (Q8–Q10) at baseline and at week 12 were 8.56 and 7.63, respectively, indicating that this intervention caused a marginally significant reduction (P = 0.041) (Fig. 1a). Analysis of the individual scores only identified a significant reduction for Q10 (P = 0.013), but not for Question 8, (P = 0.482) or Question 9 (P = 0.087) (Fig. 1b). The scores in the other PBC-40 domains were not significantly altered by this intervention (Fig. 2).
a The average itch domain scores of PBC-40 (Q8–Q10) at baseline and at week 12 (12 W) of nalfurafine treatment are shown in the participating Japanese PBC patients (n = 44). The error bars represent standard deviations. b The average scores for each PBC-40 itch domain question (Q8, Q9, Q10) are shown at baseline and at week 12 of nalfurafine treatment. The error bars represent standard deviations
Changes in VAS, autotaxin levels, and SF-36
Next, we assessed pruritus using VAS. The mean VAS at baseline and at week 12 was 42.9 and 29.3, respectively, representing a more pronounced reduction (P = 0.001) (Fig. 3a) than that detected by PBC-40. In contrast, serum autotaxin levels at baseline and at week 12 were 1.10 and 1.17 mg/L, respectively, representing a significant increase after treatment intervention with nalfurafine (P < 0.001) (Fig. 3b). The scores in each domain of the SF-36 were not significantly altered by intervention with nalfurafine (Fig. 4).
The average score for each SF-36 domain at baseline (BL) and at week 12 (12 W) of nalfurafine treatment are shown. PF physical functioning, RP role-physical, BP bodily pain, GH general health perception, VT vitality, SF social functioning, RE role-emotional, MH mental health. The error bars represent standard deviations
Association of VAS/PBC-40 with SF-36
Significant associations were repeatedly observed between PBC-40 and SF-36 in the original study [19] and in our previous validation of the Japanese version of PBC-40 [18]. The present study confirmed that there were significant correlations between every combination of PBC-40 and SF-36 domains (Table 2). However, it is notable that the PBC-40 itch domain showed a relatively weak correlation with SF-36, and the Pearson correlation coefficients were > − 0.5 in each domain (Table 2). Additionally, VAS also showed a weak correlation with each domain of SF-36. Collectively, these findings indicate that although SF-36 provides a generic HRQOL assessment tool, it is less sensitive to impairments in HRQOL caused by pruritus.
Analysis of the associations between the changes in VAS and PBC-40 itch scores and other variables
Finally, we aimed to elucidate whether any clinical or laboratory variables were related to the changes in VAS or PBC-40 itch scores. We analyzed age at diagnosis, follow-up period, age at participation, serum levels of aspartate transaminase, alanine transaminase, and alkaline phosphatase (× ULN), and serum levels of bilirubin and albumin as continuous variables, and sex, the presence of clinical events, and use of bezafibrate as categorical variables. UDCA was used in 43 of the 44 enrolled patients and therefore use of UDCA was not evaluated. As shown in Table 3a, there were no significant correlations between the change in VAS or PBC-40 itch scores and continuous variables. The P value was only < 0.05 for the association between age at participation and the PBC-40 itch score (P = 0.030); the association between age at participation and VAS was not significant (P = 0.123). Serum levels of liver enzymes, bilirubin and albumin were not significantly associated with the changes in VAS or the PBC-40 itch score. In addition, sex, the presence of clinical events, and use of bezafibrate were not associated with the change in VAS or PBC-40 itch score (Table 3b). Taken together, this analysis indicated that the efficacy of nalfurafine was not dependent on these clinical parameters.
Discussion
The current multicenter, post-marketing, single-arm, prospective study had four main aims. First, it investigated the efficacy of nalfurafine for pruritus in patients with PBC and moderate to severe pruritus. Second, it explored whether any clinical variables were associated with the efficacy of nalfurafine. Third, it determined whether the serum autotaxin level, reported to serve as a biomarker of pruritus [16], associated with the severity of pruritus in patients with PBC. Finally, and most importantly, it examined whether an improvement of pruritus was linked to better PRO; this is regarded as a vital outcome in PBC because overall survival in patients with this condition is excellent and comparable to that of the general population.
In the current study, the scores for the PBC-40 itch domain and VAS declined significantly following nalfurafine treatment, confirming the efficacy of nalfurafine for cholestatic pruritus that was previously demonstrated in a phase 3 trial in Japan [14]. As pruritus is a subjective symptom, the placebo effect should not be underestimated. Indeed, the phase 3 trial of nalfurafine found that VAS declined by 19.46 points at week 4 even in the placebo group [14]. A placebo arm was not included in the design of the current study and it is therefore possible that this effect contributed to the observed improvement of pruritus. However, since nalfurafine has been officially approved for refractory pruritus in patients with chronic liver diseases, including PBC, it was not ethically valid to assign participants to a placebo arm.
The decline in score was more pronounced for VAS than for the PBC-40 itch score. This is probably because the itch domain of PBC-40 includes three items (questions), and these yielded different responses. Both Question 8 “Itching disturbed my sleep the time” and Question 9 “I scratched so much I made my skin raw” relate to very severe pruritus, while Question 10 “I felt embarrassed because of the itching” could apply to milder pruritus. As a result, the mean score and the decline following nalfurafine treatment were greatest for Q10, and lower in Q8 and Q9. On the other hand, VAS can measure generic and mild pruritus. Therefore, the score and extent of decline were comparable for VAS and Q10, but not for Q8 and Q9.
The phase 3 trial of nalfurafine for patients with PBC did not provide detailed clinical information and it is therefore unclear which patients will benefit from nalfurafine and which will not. To address this, we searched for any associations between clinical variables and the change in VAS/PBC-40 itch domain, but failed to find any relationships between these. In our previous observational study, which was performed to screen patients for this study, we found that the severity of pruritus (measured by PBC-40 itch scores in Japanese PBC patients) was independently associated with a longer follow-up period and lower serum albumin levels [17]; however, neither the follow-up period nor the serum albumin level was associated with the treatment-associated change in PBC-40/VAS. This indicated that nalfurafine is likely to be effective in all patients with PBC, regardless of their clinical characteristics including age, sex, and disease progression. We should note, however, that the sample size was not large enough to draw conclusive results.
Autotaxin is a 125-kD type II ectonucleotide pyrophosphatase/phosphodiesterase that catalyzes the conversion of lysophosphatidylcholine into lysophosphatidic acid [23], which is a potential mediator of cholestasis-induced pruritus [24]. The serum autotaxin level was previously reported to associate with cholestatic pruritus [25]. Therefore, we expected serum autotaxin levels to decrease along with the improvement in pruritus with nalfurafine treatment, but this was not the case. The reason for this discrepancy is unclear but we believe that the role of autotaxin in cholestatic pruritus should be further evaluated in Japanese patients with PBC. All previous reports demonstrating the association of autotaxin with pruritus came from European countries, and pruritus may be influenced by social and cultural backgrounds.
Although the severity of pruritus was improved by nalfurafine, the scores in other PBC-40 domains were not affected, suggesting that overall PRO was not improved by nalfurafine treatment. Furthermore, the baseline SF-36 scores were < 50, which is defined as the mean of the general population. Therefore, PRO measured by the SF-36 was impaired at baseline, especially in the physical functioning and role-physical domains. The SF-36 scores were not altered by nalfurafine treatment. These findings could partly reflect the fact that other domains of PBC-40 and the SF-36 were originally designed to be less sensitive to pruritus. The “symptoms” domain of PBC-40 mainly measures pain, abdominal discomfort, and dryness, rather than pruritus. Similarly, the SF-36 asks about symptoms of body pain and fatigue but not about pruritus. Nevertheless, it is obvious that nalfurafine did not affect emotional, social, or cognitive PBC-40 domains or the general health perception, vitality, social functioning, role-emotional, and mental health domains of SF-36, resulting in no marked improvement of PRO. In this regard, we conclude that nalfurafine has some efficacy for the treatment of pruritus in patients with PBC, but that this effect was not sufficient. We should note, however, that treatment with nalfurafine was limited to 3 months in the current study and the PRO measured by other domains of PBC-40 and SF-36 may be improved if the treatment will be continued much longer. Nevertheless, more effective anti-pruritic drugs capable of resolving cholestasis, which is involved in the etiology of pruritus in PBC, are strongly warranted to improve PRO in patients with PBC and pruritus.
Abbreviations
- PBC:
-
Primary biliary cholangitis
- HRQOL:
-
Health-related quality of life
- UDCA:
-
Ursodeoxycholic acid
- VAS:
-
Visual analog scale
- PRO:
-
Patient-reported outcomes
- SF-36:
-
Short form 36
References
Kaplan MM, Gershwin ME. Primary biliary cirrhosis. New Engl J Med. 2005;353(12):1261–73.
Lindor KD, Gershwin ME, Poupon R, et al. Primary biliary cirrhosis. Hepatology. 2009;50(1):291–308.
Talwalkar JA, Souto E, Jorgensen RA, et al. Natural history of pruritus in primary biliary cirrhosis. Clin Gastroenterol Hepatol. 2003;1(4):297–302.
Dyson JK, Wilkinson N, Jopson L, et al. The inter-relationship of symptom severity and quality of life in 2055 patients with primary biliary cholangitis. Aliment Pharmacol Ther. 2016;44(10):1039–50.
Mells GF, Pells G, Newton JL, et al. Impact of primary biliary cirrhosis on perceived quality of life: the UK-PBC national study. Hepatology. 2013;58(1):273–83.
Newton JL, Bhala N, Burt J, et al. Characterisation of the associations and impact of symptoms in primary biliary cirrhosis using a disease specific quality of life measure. J Hepatol. 2006;44(4):776–83.
Beuers U, Kremer AE, Bolier R, et al. Pruritus in cholestasis: facts and fiction. Hepatology. 2014;60(1):399–407.
Rudic JS, Poropat G, Krstic MN, et al. Ursodeoxycholic acid for primary biliary cirrhosis. Cochrane Database Syst Rev. 2012;12:CD000551.
EASL. EASL Clinical practice guidelines: management of cholestatic liver diseases. J Hepatol. 2009;51(2):237–67.
Working Subgroup for Clinical Practice Guidelines for Primary Biliary Cirrhosis. Guidelines for the management of primary biliary cirrhosis: the intractable hepatobiliary disease Study Group supported by the Ministry of Health, Labour and Welfare of Japan. Hepatol Res. 2014;44(Suppl S1):71–90.
Bergasa NV. Pruritus in primary biliary cirrhosis: pathogenesis and therapy. Clin Liver Dis. 2008;12(2):385–406.
Bergasa NV, Jones A, Kleiner DE, et al. Pilot study of low dose oral methotrexate treatment for primary biliary cirrhosis. Am J Gastroenterol. 1996;91(2):295–9.
Kumagai H, Ebata T, Takamori K, et al. Effect of a novel kappa-receptor agonist, nalfurafine hydrochloride, on severe itch in 337 haemodialysis patients: a Phase III, randomized, double-blind, placebo-controlled study. Nephrol Dial Transplant. 2010;25(4):1251–7.
Kumada H, Miyakawa H, Muramatsu T, et al. Efficacy of nalfurafine hydrochloride in patients with chronic liver disease with refractory pruritus: a randomized, double-blind trial. Hepatol Res. 2017;47(10):972–82.
Akuta N, Kumada H, Fujiyama S, et al. Predictors of pruritus in patients with chronic liver disease and usefulness of nalfurafine hydrochloride. Hepatol Res. 2018;48(1):45–50.
Kremer AE, van Dijk R, Leckie P, et al. Serum autotaxin is increased in pruritus of cholestasis, but not of other origin, and responds to therapeutic interventions. Hepatology. 2012;56(4):1391–400.
Yagi M, Tanaka A, Abe M, et al. Symptoms and health-related quality of life in Japanese patients with primary biliary cholangitis. Submitted.
Tanaka A, Miura K, Yagi M, et al. The assessment of subjective symptoms and patient-reported outcomes in patients with primary biliary cholangitis using PBC-40. Kanzo [in Japanese]. 2016;57:457–67.
Jacoby A, Rannard A, Buck D, et al. Development, validation, and evaluation of the PBC-40, a disease specific health related quality of life measure for primary biliary cirrhosis. Gut. 2005;54(11):1622–9.
Ware JEJ. The SF-36 health survey. In: Spilker B, editor. Quality of life and pharmacoeconomics in clinical trials. 2nd ed. Philadelphia: Lippincott-Raven; 1996.
Fukuhara S, Bito S, Green J, et al. Translation, adaptation, and validation of the SF-36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51(11):1037–44.
Fukuhara S, Ware JE Jr, Kosinski M, et al. Psychometric and clinical tests of validity of the Japanese SF-36 Health Survey. J Clin Epidemiol. 1998;51(11):1045–53.
Sun Y, Zhang W, Evans JF, et al. Autotaxin, pruritus and primary biliary cholangitis (PBC). Autoimmun Rev. 2016;15(8):795–800.
Kremer AE, Martens JJ, Kulik W, et al. Lysophosphatidic acid is a potential mediator of cholestatic pruritus. Gastroenterology. 2010;139(3):1008–18.
Kremer AE, Martens JJ, Kulik W, et al. Autotaxin but not bile salts correlate with itch intensity in cholestasis. J Hepatol. 2010;52(Supplement 1):S1.
Acknowledgements
We are sincerely grateful to all of the patients who participated in this study. Also, we sincerely appreciate the secretarial assistance of Ms. Kayono Unno and Ms. Kanako Iwai.
Funding
This study was financially supported by the Japan Agency for Medical Research and Development (AMED; #17ek01091490003).
Author information
Authors and Affiliations
Consortia
Contributions
A.T. and M.Y. designed the study. T.N., A.T., M.A., A.H., Y.M., H.O., H.Y., and H.T. invited participants and collected clinical data. A.T., Y.N., and H.T. analyzed and interpreted the data. A.T. and M.Y. drafted the paper; all authors critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
AT received consultant fees from EA Pharma and GlaxoSmithKline. YM received lecture fees from Mitsubishi Tanabe Pharma, MSD K.K., AbbVie GK, Gilead Science, Janssen Pharmaceutical K.K. and commercial research findings from MSD K.K., AbbVie GK, Gilead Science, and Nobelpharma, Eisai Co.
Rights and permissions
About this article
Cite this article
Yagi, M., Tanaka, A., Namisaki, T. et al. Is patient-reported outcome improved by nalfurafine hydrochloride in patients with primary biliary cholangitis and refractory pruritus? A post-marketing, single-arm, prospective study. J Gastroenterol 53, 1151–1158 (2018). https://doi.org/10.1007/s00535-018-1465-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-018-1465-z