Abstract
Background
Intestinal Behçet’s disease (BD) is very rare, and epidemiologic data regarding BD are scarce. Moreover, there have been no population-based studies focusing on intestinal BD. We conducted a nationwide population-based study to examine the incidence and clinical course of Korean patients with intestinal BD.
Methods
We collected data on 365 patients diagnosed with intestinal BD from 2011 to 2014 using the Health Insurance Review and Assessment Services claims database. We analyzed the incidence and clinical outcomes, including cumulative rates of bowel resection, hospitalization, and medication use.
Results
During the study period, the average annual incidence for intestinal BD was 0.18 per 105 population, and the proportion of cases with intestinal involvement was 3.9%. At 1 and 4 years after diagnosis, the cumulative rates of surgery were 5.0 and 10.9%, respectively, whereas those of hospitalization were 27.8 and 32.4%, respectively. The 1- and 4-year cumulative rates of requirements for medications were 39.8 and 49.1% for moderate- to high-dose corticosteroids, 33.6 and 42.1% for immunomodulators, and 3.5 and 6.8% for biologics, respectively. The cumulative probability of corticosteroid and immunomodulator use was higher in male than in female patients and in younger (<40 years) than in older (≥40 years) patients. However, there were no significant differences in the cumulative probabilities of surgery, hospitalization, and biologics use according to sex and age group.
Conclusions
The incidence of intestinal BD in Korea is quite low and has been stable in recent years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Behçet’s disease (BD) is a rare, chronic, inflammatory, multisystem disorder characterized by recurrent oral and genital ulcers, ocular lesions, skin manifestations, and arthritis as well as vascular, neurological, and intestinal involvement [1, 2]. The prevalence of BD is very low globally, but relatively high in the Mediterranean area and East Asia at approximately 1–10 cases per 10,000 people, whereas a rate of only 1–2 cases per 1,000,000 people is observed in the United Kingdom and North America [3].
Intestinal BD is diagnosed when there is a typically shaped ulcer in the gastrointestinal (GI) tract and clinical findings meet the diagnostic criteria for BD [4]. The GI involvement in BD differs in various countries, ranging from 0 to 20% [2]. Interestingly, intestinal involvement occurs more commonly in East Asia, including Korea and Japan, than in the Mediterranean area [2, 5, 6]. However, all available data on the frequency of intestinal BD are derived from referral centers and/or small-sized case series. At present, accurate data on the incidence of intestinal BD do not exist.
Data concerning the clinical course of intestinal BD in a population-based setting also do not exist. Intestinal BD has a fulminant clinical course in some cases [7]. Intestinal BD often requires surgical treatment due to the high frequency of complications, such as intestinal perforations and massive intestinal bleeding, coupled with unresponsiveness to pharmaceutical treatments [8, 9]. Moreover, intestinal BD frequently recurs, even after surgical treatment, and occasionally requires repeated surgery [8, 10]. However, all of the available data on the clinical course of intestinal BD are derived from hospital-based studies [7,8,9,10,11,12,13]. Therefore, those results may have a referral-center bias due to the inclusion of more severe cases.
Intestinal BD is a very rare disease, so epidemiologic studies of this disease are scarce. In contrast to ulcerative colitis (UC) and Crohn’s disease (CD), no population-based study of intestinal BD is reported. As a number of population-based studies conducted in Western countries provide useful information on the epidemiologic features of UC and CD [14], a population-based study of intestinal BD in East Asia is needed, given its high prevalence in this region. Such a population study will help us to better understand the burden of disease and further characterize the clinical features and natural course of intestinal BD.
As the Korean government operates a mandatory nationwide insurance system (National Health Insurance, NHI), all health care utilization information is registered in a comprehensive database operated by the Health Insurance and Review Agency (HIRA). The HIRA database allows us to study national epidemiology and clinical outcomes of intestinal BD using reliable information. In this study, we conducted a nationwide population-based study using the HIRA database to investigate the incidence and clinical outcomes of intestinal BD in Korea, including cumulative rates of bowel resection, hospitalization, medication use, and cause of death.
Materials and methods
Data source
This study used data from the NHI, which provides mandatory universal health insurance that covers all health services, including admission, ambulatory care, and pharmaceutical services. Medical institutions submit health care utilization information in electronic form for reimbursement purposes, and this information is integrated into the HIRA claims database, which covers the entire population of Korea (>50 million).
The database contains information on all patients, including demographic characteristics, admission and ambulatory care history, principal diagnosis and comorbidities according to the 10th revision of the International Classification of Disease (ICD-10), prescriptions, and diagnostic and surgical procedures. The source population for this study comprised all beneficiaries during 2010–2014, and their data were reviewed retrospectively.
Patient identification and clinical information
The main endpoints of this study were the incidence of intestinal BD and the cumulative probabilities of surgery, hospitalization, and medication use, including corticosteroids, immunomodulators, and biologics.
The diagnosis of BD was based on the International Study Group diagnostic criteria for BD (recurrent oral ulceration plus two of recurrent genital ulceration, eye lesions, skin lesions, or positive pathergy test) [1]. To increase the diagnostic accuracy of intestinal BD, intestinal BD was defined as a case including all three of the following: the appropriate diagnostic code (ICD-10 code M35.2), performance of colonoscopy, and prescription of 5-aminosalicylic acids at a gastroenterology clinic for >1 month. In other words, among patients registered for BD in the HIRA database from January 2010 to December 2014, patients who underwent a colonoscopy and were prescribed 5-aminosalicylic acids at a gastroenterology clinic for >1 month were included in the study. Because 5-aminosalicylic acids are only used in the treatment of intestinal involvement in BD, not in the treatment of any other involvement, a prescription of 5-aminosalicylic acids can be regarded as confirmation of a diagnosis of intestinal BD. Therefore, prescription of 5-aminosalicylic acids was included in the definition of intestinal BD, and the date of diagnosis with intestinal BD was regarded as the start date of the prescription of 5-aminosalicylic acids.
Corticosteroid use included both oral and intravenous corticosteroids. Moderate- to high-dose corticosteroid use was defined as ≥30 mg prednisolone, ≥50 mg methylprednisolone, or ≥200 mg hydrocortisone. To more accurately assess corticosteroid use at the time of disease flare-up, the cumulative probability of corticosteroid use was analyzed in terms of moderate- to high-dose corticosteroid use. Surgical cases were defined as patients who had undergone bowel resection (surgery involving the resection of the small bowel, colon, or rectum). Hospitalization was defined as admission to the Division of Gastroenterology for the purpose of surgery or administration of intestinal BD-specific medicine (moderate- to high-dose corticosteroids, immunomodulators, or biologics) in order to include only intestinal BD-related admissions as far as possible. Cause of death was regarded as the principal diagnosis at the time of death and classified according to the ICD-10.
Statistical analysis
We used health care utilization information from the HIRA claims database to analyze the incidence of BD and intestinal BD. An incident case for BD was defined as a patient registered for BD for 2 years in a row, excluding patients with a history of health care utilization for BD before 2010 in the HIRA database. An incident case of intestinal BD was defined as a patient newly diagnosed with intestinal BD in the corresponding year. Because the inclusion of previous prevalent cases may confound incidence, we used a washout period of 1 year. Thus, we assessed the incidence of BD between 2011 and 2013 and the incidence of intestinal BD between 2011 and 2014. The incidence was defined as the number of incident cases in the corresponding year per 105 population using the resident registration population on July 1 of each year. Age- and sex-specific incidence was calculated by dividing the number of cases in age- and sex-stratified groups by the corresponding age- and sex-specific population, and was expressed as cases per 105 population.
The cumulative probabilities of surgery, hospitalization, and medication use including corticosteroids, immunomodulators, or biologics after diagnosis were calculated using the Kaplan–Meier method, and the differences by age group (<40 vs. ≥40 years) and sex were determined using the log-rank test. All analyses were performed using SAS Enterprise Guide (SAS Institute, Inc., Cary, NC, USA). P values of less than 0.05 were considered statistically significant.
Ethical considerations
All identifiable personal information in medical records are de-identified to comply with the Health Insurance Portability and Accountability Act privacy rule. Also, as the information in the HIRA database was encrypted, the database does not contain personal identifiers. This study protocol was approved by The Institutional Review Board of Severance Hospital, Yonsei University.
Results
Incidence
The incidence of BD and that of intestinal BD are shown in Table 1. There were 7148 new cases of BD from 2011 to 2013, and there were 365 new cases of intestinal BD from 2011 to 2014. The incidence of BD in 2011, 2012, and 2013 was 5.63, 4.63, and 4.04 per 105 population, respectively, with an average annual incidence of 4.77 per 105 population. The incidence of intestinal BD from 2011 to 2014 was 0.16–0.21 per 105 population, with an average annual incidence of 0.18 per 105 population. That is, 3.9% of the BD patients had intestinal BD (n = 282/7148, 2011–2013).
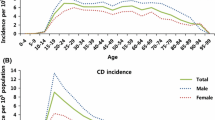
Among patients with intestinal BD, the mean age of diagnosis was 44.1 ± 14.4 years and the male-to-female ratio was 0.87. The incidence of intestinal BD by sex and age group is shown in Fig. 1. The incidence of intestinal BD was highest for ages 45–54 (0.31 per 105 population) and steadily decreased thereafter.
Clinical outcomes
Among all incident cases (n = 365), 26 (7.1%) underwent bowel resection and 108 (29.6%) were hospitalized during the follow-up period (for 4 years, 2011–2014). At 1, 2, 3, and 4 years after diagnosis, the cumulative rates of surgery were 5.0, 8.1, 9.3, and 10.9%, respectively, while the cumulative rates of hospitalization were 27.8, 31.1, 32.4, and 32.4%, respectively.
Among all incident cases, 130 (35.6%) received immunomodulators (azathioprine or 6-mercaptopurine) and 17 (4.7%) received biologics (infliximab or adalimumab). Because only 3 patients received treatment with methotrexate, we did not include methotrexate in immunomodulator use. A total of 194 patients (53.2%) received corticosteroid therapy of any dose, and 156 patients (42.7%) received moderate- to high-dose corticosteroid therapy. Of 17 patients who received biologics, 9 were treated with infliximab and 8 were treated with adalimumab.
The cumulative rates of requirement for medications at 1, 2, 3, and 4 years after diagnosis were 39.8, 43.5, 47.0, and 49.1% for moderate- to high-dose corticosteroids; 33.6, 37.7, 40.1, and 42.1% for immunomodulators, and 3.5, 5.4, 6.8, and 6.8% for biologics, respectively.
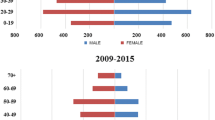
The cumulative probabilities of surgery and hospitalization after diagnosis by sex and age group are shown in Fig. 2, and those of moderate- to high-dose corticosteroid use and immunomodulator use are shown in Fig. 3. There were no significant differences in the cumulative probabilities of surgery and hospitalization according to sex (P = 0.526 and P = 0.560, respectively) or age group (P = 0.946 and 0.281, respectively) (Fig. 2). On the other hand, the cumulative probabilities of moderate- to high-dose corticosteroid use and immunomodulator use were higher in male patients compared with female patients (P < 0.001 and P = 0.033, respectively) and in younger patients compared with older patients (P = 0.001 and P < 0.001, respectively) (Fig. 3). There were no significant differences in the cumulative probabilities of biologics use according to sex (P = 0.056) or age group (P = 0.136) (data not shown).
Because younger patients may be at risk of more severe disease, we further compared the clinical outcomes between patients aged <30 vs. ≥30 years. As a result, similar to the results for patients aged <40 vs. ≥40 years, there were no significant differences in the cumulative probabilities of surgery and hospitalization between patients aged <30 vs. ≥30 years (P = 0.732 and P = 0.405, respectively), while the cumulative probabilities of corticosteroid use and immunomodulator use were higher in patients aged < 30 years compared with patients aged ≥30 years (P = 0.009 and P < 0.016, respectively).
During the study period, 51 patients (11%) were identified as having been prescribed 5-aminosalicylic acids for 1 month or less. Because it is possible that non-intestinal BD patients might have been misdiagnosed as having intestinal BD and temporarily misprescribed 5-aminosalicylic acids, we considered the prescription of 5-aminosalicylic acids for >1 month when defining intestinal BD.
In-hospital mortality
We identified 11 patients who died. The principal diagnosis at the time of death was regarded as the cause of death. Of the 11 patients who died, 4 died of cancer (C00-C97), 1 died of hemophagocytic lymphohistiocytosis (D76.1), 2 died of a circulatory system disease (I00-I99), 2 died of a respiratory system disease (J00–J99), and 2 died of BD itself (M35.2). Of the 4 patients who died of cancer, 2 died of leukemia [1 died of precursor T cell lymphoma leukemia (C91.01) and 1 died of acute myeloblastic leukemia (C92.08)], 1 died of myelodysplastic and myeloproliferative disease (C94.6), and 1 died of ovarian cancer.
Discussion
In this Korean population-based study, 365 patients with intestinal BD were newly identified from 2011 to 2014, with an average annual incidence of 0.18 per 105 population, and 7148 patients with BD were newly identified from 2011 to 2013, with an average annual incidence of 4.77 per 105 population. Among BD patients, 3.9% had intestinal BD; this proportion is lower than that reported in previous studies. The previously reported frequency of GI involvement in BD has varied widely, ranging from 0 to 50% [2, 15, 16]. This may because the diagnostic criteria for intestinal BD have varied from study to study. Some studies have considered the mere presence of GI symptoms as a diagnosis of intestinal BD, which may have resulted in the overestimation of the true frequency [15, 16]. Because we considered both endoscopy and medications when defining intestinal BD, our results regarding the frequency of intestinal BD may be more accurate and reliable than previous studies.
Meanwhile, the incidence of intestinal BD was much lower than that of UC or CD. Recently, a Korean population-based study demonstrated that the mean annual incidence for UC was 4.6 per 105 population and that for CD was 3.2 per 105 population during the 2006–2012 period [17]. In the present study, the incidence of BD in 2011, 2012, and 2013 was 5.63, 4.63, and 4.04 per 105 population, respectively. Although our study period was too short to assess temporal changes in the incidence of disease, in contrast to the increasing incidence of inflammatory bowel disease (IBD) in Korea, the incidence of BD appears to show a slightly declining trend. However, our data on BD incidence might have been overestimated owing to the lack of a clear definition of BD. A more accurate definition of BD and longer follow-up studies are necessary to draw a concrete conclusion about the true trend of BD incidence.
The mean age of diagnosis for intestinal BD was 44.1 years. The peak age for intestinal BD (45–54 years) was higher than that for BD (30–40 years) [18, 19] or CD (20–30 years) [20, 21]. Intestinal involvement seems to have its onset later (by approximately 5–15 years) during the course of BD. Previous studies also support this [22, 23]. Similar to the female preponderance of BD in Japan and Korea [18, 19], there were more female patients with intestinal BD than male patients (male-to-female ratio 0.87). This is contrary to the male predominance for IBD in Asia [20, 24].
In the present study, the 1- and 4-year cumulative rates of surgery were 5.0 and 10.9%, respectively, and those of hospitalization were 27.8 and 32.4%, respectively. These rates were lower than those in previous studies showing that the 1- and 5-year cumulative rates of surgery were 20% and 32–33%, respectively, and those of hospitalization were 44–45% and 59–61%, respectively [25, 26]. However, previous studies were non-population-based studies in a hospital setting. Therefore, previous studies might have been biased toward patients with severe disease and a poorer prognosis than the cases in the current study. This may be one reason for the lower surgery and hospitalization rates in our study compared with previous studies. In addition, the cumulative rates of surgery among patients with intestinal BD in our study were lower than those of population-based studies of patients with CD. A meta-analysis of seven population-based studies demonstrated that 1- and 5-year rates of surgery were 12.6 and 24.2%, respectively, in patients with CD [27]. However, our study period was only 4 years, which is too short to fully understand the natural course and long-term prognosis of intestinal BD. Future extended long-term studies are needed to elucidate the clinical outcomes of intestinal BD.
On the other hand, in contrast to the surgery and hospitalization rates, the cumulative rates of immunomodulator use were higher than those of previous studies investigating intestinal BD. In our study, the 1- and 4-year cumulative probabilities of immunomodulator use were 33.6 and 42.1%, respectively, whereas previous studies reported 1- and 5-year cumulative rates of immunomodulator use of 10–11% and 25–27%, respectively [25, 26]. Regarding biologics, only 1.4% of patients were treated with infliximab in a previous study [25], whereas in our study, 4.7% were treated with infliximab or adalimumab. Furthermore, considering the previous studies were non-population-based studies in a hospital setting, which could include patients with more severe disease, the patients in our study may have received more aggressive pharmaceutical treatment than in previous studies. The higher rates of immunomodulator and biologics use compared with the results in previous studies may be because of the use of recent data in our study (2011–2014 in our study vs. 1986–2010 in previous studies). In other words, there may be a temporal bias. Improvements in pharmaceutical treatments such as immunomodulators and biological agents in addition to increased knowledge and awareness of medical treatment of intestinal BD among physicians may have led to more aggressive pharmaceutical treatment in our more recent study. Many studies have indicated that mucosal healing can change the natural course of the disease by decreasing the need for surgery and reducing hospitalization rates for both UC and CD [28,29,30]. Therefore, mucosal healing has emerged as a therapeutic goal in IBD treatment; accordingly, accelerated step-up therapy has been regarded as the best approach for the majority of IBD patients to achieve early mucosal healing [29]. Although little is known about the effects of mucosal healing on the clinical course of intestinal BD, accumulating evidence regarding IBD may have led to the early use of immunomodulators and biologics, even for intestinal BD. These early aggressive pharmaceutical treatments including immunomodulators may also be a reason for the lower rates of surgery in our study compared with previous studies.
Meanwhile, the cumulative rates of immunomodulator use among patients with intestinal BD in our study were comparable to those among patients with CD in previous population-based studies, with 25–35% at 1 year and 36–46% at 5 years [31,32,33]. However, the cumulative rates of biologics use in patients with intestinal BD were lower than those in patients with CD. Our study demonstrated that 1- and 4-year rates of biologics use in patients with intestinal BD were only 3.5 and 6.8%, respectively, whereas a previous population-based study showed 1- and 5-year rates of biologics use of 9 and 19%, respectively, for CD patients [33]. The reason for the lower rate of biologics use in patients with intestinal BD is that the Korean government did not offer insurance benefits for biologics use for patients with intestinal BD during the study period. The insurance benefit for adalimumab use was offered in 2015, but an insurance benefit for infliximab use is not yet offered in Korea.
Regarding corticosteroid use, its cumulative rates at 1 and 4 years were 39.8 and 49.1%, respectively, and they were slightly higher than those of intestinal BD hospital-based studies, with 24–25% at 1 year and 42–43% at 5 years [25, 26], and were comparable to those of CD population-based studies, with 35% at 1 year and 46–52% at 5 years [33, 34]. Given that we investigated the rates of moderate- to high-dose corticosteroid use, the rates of corticosteroid use in patients with intestinal BD may be slightly higher than those in patients with CD. In particular, our study showed that many patients received corticosteroid therapy immediately after their diagnosis of intestinal BD. Physicians may tend to prescribe more and earlier corticosteroids to patients with intestinal BD compared with patients with CD because medical therapy options for intestinal BD are limited.
We found that the cumulative probabilities of corticosteroid and immunomodulator use were higher in male than in female patients and in younger (<40 years) than in older (≥40 years) patients. However, there were no significant differences in the cumulative probabilities of surgery, hospitalization, and biologics use according to sex or age group. The lower rate of immunomodulator use in female patients may be due to factors such as pregnancy and childbirth. Even though it is difficult to reach a definitive conclusion based only on the difference in corticosteroid and immunomodulator use, our results suggest that male sex and younger age of onset may be associated with more severe disease and a worse prognosis. These results are consistent with those of BD and CD studies. In the literature concerning BD, several studies have shown that male sex and younger age of onset are associated with more severe disease [35,36,37]. In addition, some researchers have reported that mortality in patients with BD was specifically increased among young male patients [38, 39]. A young age at onset is also known to be a poor prognostic factor in patients with CD [40]. Similar to patients with BD and CD, younger age at onset seems to be a poor prognostic factor in intestinal BD patients. Previous studies also support this. Several studies have demonstrated that younger age at diagnosis is associated with a more severe clinical course and a poorer prognosis in patients with intestinal BD [11, 12, 26, 41, 42].
In our study, a prescription of 5-aminosalicylic acids was regarded as confirmation of a diagnosis of intestinal BD. As 5-aminosalicylic acids theoretically have intestine-specific activity, they can only be used in the treatment of intestinal involvement among patients with BD. Although clinical evidence proving the effectiveness of 5-aminosalicylic acids for the treatment of intestinal BD is scant, 5-aminosalicylic acids are the main empiric maintenance therapeutic option for intestinal BD in Korea [11]. A consensus agreement by experts in Japan also concluded that 5-aminosalicylic acids are indicated for all cases of intestinal BD [43]. Our recent study supports this. The study analyzed data from 143 patients maintaining remission under only 5-aminosalicylic acids without corticosteroids or immunosuppressive agents [11]. As a result, only 46 (32%) experienced a clinical relapse (the median follow-up period after the start of 5-aminosalicylic acids therapy was 80 months), and the cumulative relapse rates at 1, 3, and 5 years after remission were 8.1, 22.6, and 31.2%, respectively [11]. This study shows that 5-aminosalicylic acids are effective at maintaining remission in patients with mild to moderate intestinal BD.
We sought to identify the effect of medication on surgery rate, although the relevant data were not shown in the “Results” section. To investigate the association between medication use and the risk of surgery, we carried out a nested case–control analysis. We used this approach in order to avoid length bias and match the exposure durations of cases and controls. As a result, both corticosteroid use [odds ratio (OR) 4.48, 95% confidence interval (CI) 1.22–16.47] and immunomodulator use (OR 3.78, 95% CI 1.17–12.25) was significantly associated with a high risk of surgery. It is likely that severe patients are both more likely to take corticosteroids and/or immunomodulators and to undergo surgery. We think that the study period was too short (maximum of 4 years) to fully evaluate the effect of medications on clinical outcomes, including surgery.
This is the first nationwide population-based study on the epidemiology and clinical course of intestinal BD in the world; nonetheless, it had several limitations. First, because we used administrative data, we could not obtain clinical activity, endoscopic findings, or laboratory findings, so we did not evaluate detailed clinical status or disease severity. Second, we did not verify the diagnostic accuracy of BD and intestinal BD. As we used insurance claims data, it is possible that some intestinal BD patients might have been missed or non-intestinal BD patients might have been misdiagnosed as having intestinal BD. To overcome this limitation, we considered performance of a colonoscopy and the prescription of 5-aminosalicylic acids at a gastroenterology clinic for >1 month as well as the diagnostic code when defining intestinal BD. If there is a typically shaped ulcer on colonoscopy, clinicians will diagnose intestinal BD, and they will then prescribe 5-aminosalicylic acids only in patients who are definitely diagnosed with intestinal BD. Moreover, 5-aminosalicylic acids are not used in the treatment of other organ involvement—only for intestinal involvement in BD. Therefore, we think that the definition of intestinal BD diagnosis in our study is reliable. However, the definition of BD needs to be further investigated. Third, the study period was too short to fully assess the natural course and temporal changes in the incidence of intestinal BD. Finally, because we could only obtain data on in-hospital mortality, the mortality rate may have been underestimated, and it was not compared with that in the general population. Whether mortality in patients with intestinal BD is different from that in the general population is still an unsolved issue. Also, considering the principal diagnosis at the time of death as the cause of death may have reduced the accuracy of the cause of death.
Despite these limitations, our population-based data provide a better understanding of the natural course of patients recently diagnosed with intestinal BD. The incidence of intestinal BD in Korea is quite low and has been stable in recent years. The 1- and 4-year cumulative rates of intestinal resection were 5.0 and 11%, respectively, whereas those of immunomodulator use were 34 and 42%, respectively. The early clinical course of patients who were recently diagnosed with intestinal BD was milder than our expectations, which may be because of early aggressive pharmaceutical treatment including immunomodulators.
References
Dalvi SR, Yildirim R, Yazici Y. Behcet’s syndrome. Drugs. 2012;72:2223–41.
Cheon JH, Kim WH. An update on the diagnosis, treatment, and prognosis of intestinal Behçet’s disease. Curr Opin Rheumatol. 2015;27:24–31.
Suzuki Kurokawa M, Suzuki N. Behcet’s disease. Clin Exp Med. 2004;4:10–20.
Cheon JH, Kim ES, Shin SJ, et al. Development and validation of novel diagnostic criteria for intestinal Behçet’s disease in Korean patients with ileocolonic ulcers. Am J Gastroenterol. 2009;104:2492–9.
Chang HK, Kim JW. The clinical features of Behcet’s disease in Yongdong districts: analysis of a cohort followed from 1997 to 2001. J Korean Med Sci. 2002;17:784–9.
Yazici Y, Yurdakul S, Yazici H. Behçet’s syndrome. Curr Rheumatol Rep. 2010;12:429–35.
Jung YS, Cheon JH, Park SJ, et al. Clinical course of intestinal Behcet’s disease during the first five years. Dig Dis Sci. 2013;58:496–503.
Jung YS, Yoon JY, Lee JH, et al. Prognostic factors and long-term clinical outcomes for surgical patients with intestinal Behcet’s disease. Inflamm Bowel Dis. 2011;17:1594–602.
Ketch LL, Buerk CA, Liechty D. Surgical implications of Behcet’s disease. Arch Surg. 1980;115:759–60.
Iida M, Kobayashi H, Matsumoto T, et al. Postoperative recurrence in patients with intestinal Behcet’s disease. Dis Colon Rectum. 1994;37:16–21.
Jung YS, Hong SP, Kim TI, et al. Long-term clinical outcomes and factors predictive of relapse after 5-aminosalicylate or sulfasalazine therapy in patients with intestinal Behcet disease. J Clin Gastroenterol. 2012;46:e38–45.
Jung YS, Cheon JH, Hong SP, et al. Clinical outcomes and prognostic factors for thiopurine maintenance therapy in patients with intestinal Behcet’s disease. Inflamm Bowel Dis. 2012;18:750–7.
Jung YS, Hong SP, Kim TI, et al. Early versus late surgery in patients with intestinal Behçet disease. Dis Colon Rectum. 2012;55:65–71.
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54 (quiz e30).
Shimizu T, Ehrlich GE, Inaba G, et al. Behcet disease (Behcet syndrome). Semin Arthritis Rheum. 1979;8:223–60.
Jankowski J, Crombie I, Jankowski R. Behcet’s syndrome in Scotland. Postgrad Med J. 1992;68:566–70.
Kim HJ, Hann HJ, Hong SN, et al. Incidence and natural course of inflammatory bowel disease in Korea, 2006–2012: a nationwide population-based study. Inflamm Bowel Dis. 2015;21:623–30.
Alpsoy E. Behçet’s disease: a comprehensive review with a focus on epidemiology, etiology and clinical features, and management of mucocutaneous lesions. J Dermatol. 2016;43:620–32.
Cho SB, Bang D. New insights in the clinical understanding of Behçet’s disease. Yonsei Med J. 2012;53:35–42.
Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016;14:111–9.
Loftus EV, Sandborn WJ. Epidemiology of inflammatory bowel disease. Gastroenterol Clin North Am. 2002;31:1–20.
Ugurlu N, Bozkurt S, Bacanli A, et al. The natural course and factors affecting severity of Behçet’s disease: a single-center cohort of 368 patients. Rheumatol Int. 2015;35:2103–7.
Ideguchi H, Suda A, Takeno M, et al. Behçet disease: evolution of clinical manifestations. Medicine. 2011;90:125–32.
Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asia-Pacific Crohn’s and Colitis Epidemiology Study. Gastroenterology. 2013;145(158–165):e152.
Jung YS, Cheon JH, Park SJ, et al. Long-term clinical outcomes of Crohn’s disease and intestinal Behcet’s disease. Inflamm Bowel Dis. 2013;19:99–105.
Jung YS, Yoon JY, Hong SP, et al. Influence of age at diagnosis and sex on clinical course and long-term prognosis of intestinal Behcet’s disease. Inflamm Bowel Dis. 2012;18:1064–71.
Frolkis AD, Dykeman J, Negrón ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013;145:996–1006.
Schnitzler F, Fidder H, Ferrante M, et al. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn’s disease. Inflamm Bowel Dis. 2009;15:1295–301.
Burger D, Travis S. Conventional medical management of inflammatory bowel disease. Gastroenterology. 2011;140(1827–1837):e1822.
Colombel JF, Rutgeerts P, Reinisch W, et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology. 2011;141:1194–201.
Lakatos PL, Golovics PA, David G, et al. Has there been a change in the natural history of Crohn’s disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977–2009. Am J Gastroenterol. 2012;107:579–88.
Ramadas AV, Gunesh S, Thomas GA, et al. Natural history of Crohn’s disease in a population-based cohort from Cardiff (1986–2003): a study of changes in medical treatment and surgical resection rates. Gut. 2010;59:1200–6.
Rungoe C, Langholz E, Andersson M, et al. Changes in medical treatment and surgery rates in inflammatory bowel disease: a nationwide cohort study 1979–2011. Gut. 2014;63:1607–16.
Chhaya V, Saxena S, Cecil E, et al. Steroid dependency and trends in prescribing for inflammatory bowel disease—a 20-year national population-based study. Aliment Pharmacol Ther. 2016;44:482–94.
Yazici H, Tüzün Y, Pazarli H, et al. Influence of age of onset and patient’s sex on the prevalence and severity of manifestations of Behçet’s syndrome. Ann Rheum Dis. 1984;43:783–9.
Alpsoy E, Donmez L, Onder M, et al. Clinical features and natural course of Behçet’s disease in 661 cases: a multicentre study. Br J Dermatol. 2007;157:901–6.
Bardak Y. Effects of age and sex on Behçet’s disease. J Rheumatol. 1999;26:1008–9.
Kural Seyahi E, Fresko I, Seyahi N, et al. The long-term mortality and morbidity of Behçet syndrome: a 2-decade outcome survey of 387 patients followed at a dedicated center. Medicine. 2003;82:60–76.
Yazici H, Basaran G, Hamuryudan V, et al. The ten-year mortality in Behcet’s syndrome. Br J Rheumatol. 1996;35:139–41.
Miheller P, Kiss LS, Juhasz M, et al. Recommendations for identifying Crohn’s disease patients with poor prognosis. Expert Rev Clin Immunol. 2013;9:65–75 (quiz 76).
Moon CM, Cheon JH, Shin JK, et al. Prediction of free bowel perforation in patients with intestinal Behçet’s disease using clinical and colonoscopic findings. Dig Dis Sci. 2010;55:2904–11.
Park JJ, Kim WH, Cheon JH. Outcome predictors for intestinal Behçet’s disease. Yonsei Med J. 2013;54:1084–90.
Kobayashi K, Ueno F, Bito S, et al. Development of consensus statements for the diagnosis and management of intestinal Behcet’s disease using a modified Delphi approach. J Gastroenterol. 2007;42:737–45.
Acknowledgements
This research was supported by two grants (A120176 and HI13C1345) from the Korean Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), which is funded by the Ministry of Health and Welfare, Republic of Korea; two grants (NRF-2013R1A2A2A01067123 and NRF-2014R1A1A1008096) from the Basic Science Research Program through the National Research Foundation of Korea, which is funded by the Ministry of Science, ICT and Future Planning; and a faculty research grant (2012-31-0477) from the Department of Internal Medicine, Yonsei University, College of Medicine.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
M. Han and Y. S. Jung contributed equally to this study.
Rights and permissions
About this article
Cite this article
Han, M., Jung, Y.S., Kim, W.H. et al. Incidence and clinical outcomes of intestinal Behçet’s disease in Korea, 2011–2014: a nationwide population-based study. J Gastroenterol 52, 920–928 (2017). https://doi.org/10.1007/s00535-016-1300-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1300-3