Abstract
Background
Although chronic intestinal pseudo-obstruction (CIPO) is a rare and extremely severe functional digestive disorder, its clinical course and severity show various patterns. We assessed small bowel peristalsis in CIPO patients using cine-MRI (video-motion MRI) and their clinical characteristics to evaluate the clinical importance of performing cine-MRI in patients with this intractable disease.
Methods
The medical records of 131 patients referred to our institution with a suspected diagnosis of CIPO between 2010 and 2015 were retrospectively evaluated. Thirty-three patients (22 female/11 male; age range 16–79 years) who met the criteria for CIPO and underwent cine-MRI were enrolled. Mean luminal diameter (MLD), contraction ratio (CR), and contraction cycle (CC) were determined and compared with these parameters in healthy volunteers. Clinical outcomes in patients with CIPO were also evaluated.
Results
The median follow-up time was 25.2 months (range, 1–65 months). Of the 33 patients with CIPO, 23 (70 %) showed apparently disturbed small intestinal peristalsis, whereas 10 (30 %) did not. The percentage of patients requiring intravenous alimentation was significantly higher (p = 0.03), and the mean serum albumin level was significantly lower (p = 0.04), in patients with than without impaired small intestinal peristalsis. Although both cine-MRI and CT findings in the latter ten cases were within the normal range, MLD and CR differed significantly from healthy volunteers.
Conclusions
Cine-MRI is useful in predicting severe clinical features in patients with CIPO, and in detecting slightly impaired small contractility that cannot be detected on CT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic intestinal pseudo-obstruction (CIPO) is an intractable and serious digestive disorder characterized by severe impairment of gut propulsive motility. The clinical features of CIPO resemble those of mechanical obstruction, including bloating, abdominal pain, and vomiting in the absence of any organic disorders. Although the small intestine is the most severely affected part of the digestive tract, the entire gut from the esophagus to the rectum can be affected [1–6].
CIPO is a rare disease in clinical practice, and its etiology, pathophysiology, and prevalence remain poorly understood. Our previous investigation of the epidemiology of CIPO in Japan using a nationwide questionnaire survey found that the total number of patients being treated for this disease throughout Japan during the given year to be 1148 [7]. The annual rates of CIPO among male and female individuals have been reported to be 0.21/100,000 and 0.24/100,000, respectively [7].
We also found that the average time from onset of symptoms to a correct diagnosis of CIPO was over 7 years [7]. Although most patients with CIPO experience recurrent episodes of obstruction and have potentially life-threatening complications, they are often misdiagnosed. Many may undergo inappropriate surgical operations because CIPO lacks specific laboratory findings and specific biological markers, and because its symptoms overlap with those of several other forms of gut motor dysfunction. Although there is no consensus regarding the diagnosis of CIPO, most studies [2, 5, 8–11] have suggested the following criteria: (1) recurrent and/or chronic episodes suggesting mechanical intestinal obstruction; (2) lack of a fixed lumen-occluding lesion, as determined by endoscopy and/or radiology; and (3) radiological evidence of dilated bowel loops with air-fluid levels. Our group, The Research Group for CIPO in Japan, proposed the following plain diagnostic criteria for CIPO in Japan [12]: (1) typical clinical manifestations, such as abdominal bloating and/or abdominal pain for more than 6 months; (2) radiological evidence of distended bowel loops with air-fluid levels; and (3) absence of any organic obstruction of the gut lumen. These criteria were found to be valid, having a sensitivity of 86.3 % in a Japanese population [12].
The onset of CIPO is generally insidious, with a slow progression of symptoms over the years. Patients may have occasional symptom-free periods followed by periods of severe symptoms. As the most important roles of the small intestine are digestion and absorption, most patients with CIPO experience malnutrition [1, 13]. These patients are often unable to maintain normal body weight because of inadequate oral intake and/or impaired absorptive capacity, with the latter being the main cause of small intestinal failure and one of the most severe clinical features of CIPO [1, 13].
Few studies to date have described long-term outcomes in patients with CIPO. Their 10-year survival rate has been reported to be 60–80 % [5, 8, 14]; however, the 5-year survival rate among patients requiring home parental nutrition (HPN) was found to be 52–75 % [15]. Thus, despite CIPO being a benign functional disorder, its prognosis is rather poor.
Clinical courses can vary widely among patients with CIPO. Some patients have a severe clinical presentation and/or require frequent hospitalization, resulting in a severely impaired quality of life, whereas others exhibit more moderate clinical manifestations. These findings suggested that multiple pathophysiologies may be involved in disease onset and progression, indicating a need for new methods of determining disease severity.
Although motility disturbances may affect all parts of the gastrointestinal tract in CIPO patients [1–6], impairments in small intestinal motility are considered the main causes of severe clinical outcomes [16]. Thus, assessment of small bowel motility may be important for understanding differences in clinical features among patients with CIPO.
At present, computed tomography (CT) and plain radiography, which are available at most institutions, are the modalities most frequently used to detect distended bowel loops with air-fluid levels and to rule out mechanical obstruction. However, these modalities are less useful for evaluating bowel peristalsis. Although intestinal manometry and scintigraphy have proven useful in detecting motor abnormalities in Western countries, these techniques are invasive and can only be performed at a limited number of institutions [17–19].
Advances in technology have enabled the use of magnetic resonance imaging (MRI) to assess various gastrointestinal disorders. Recently, cine-MRI has emerged as a noninvasive radiation-free method for assessing and monitoring gastrointestinal motility function [20–22]. We reported that intestinal luminal diameter was significantly higher and the contraction ratio significantly lower in CIPO patients than in patients with irritable bowel syndrome (IBS) and healthy subjects [21]. To our knowledge, that study was the first to use cine-MRI to evaluate small bowel motility in patients with CIPO.
To date, however, no study has used cine-MRI to assess small intestinal peristalsis in patients already had diagnosed with CIPO. This study therefore retrospectively evaluated small bowel motility using cine-MRI in CIPO patients, and examined the relationships between clinical outcomes and small intestinal peristalsis. The aim of this study was to evaluate the clinical importance of cine-MRI in patients with CIPO.
Methods
Study design and setting
The clinical records of 131 consecutive patients referred to the Department of Gastroenterology at Yokohama City University Hospital for a suspected diagnosis of CIPO between January 2010 and October 2015 were retrospectively reviewed. Patients were included if they (1) were definitely diagnosed of CIPO according to the criteria proposed by the Japanese Ministry of Health, Labour, and Welfare; (2) underwent cine-MRI evaluation of small bowel peristalsis prior to any medical intervention for CIPO; and (3) underwent cine-MRI according to the standardized protocol described below.
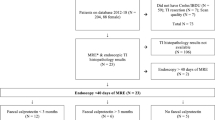
Of the 131 patients (88 female, 43 male, mean age, 44.4 ± 16.6 years; range, 14–81 years) evaluated during the study period, 68 patients met the criteria for CIPO. However, 35 of these patients were excluded because they did not meet the inclusion criteria (Fig. 1). The remaining 33 patients (21 female, 12 male, mean age 46.6 ± 18.1 years; range, 16–80 years) were included in the study, and their cine-MRI results and clinical courses were analyzed retrospectively. Their cine-MRI results were also compared with those of 11 healthy volunteers who had been analyzed in our previous study [21]. The associations between small intestinal peristalsis and patient clinical course, including sex, age, and underlying disease, were evaluated. Body mass index (BMI) and serum albumin level at the first visit to our institution and eating habits were determined, as well as whether patients required enteral or parenteral nutrition during the follow-up period. Patient need for persistent decompression therapy and patient outcomes were also evaluated.
MRI protocol
Cine-MRI was performed using a 1.5-T system (Achieva; Philips Healthcare, Best, The Netherlands), a four-element phased-array surface coil (SENSE body coil) and a balanced turbo field-echo sequence with image acquisition in the coronal plane, a repetition time/echo time of 4.1/2.0 ms, a flip angle of 80°, a field of view of 38 × 38 cm, a slice thickness of 10 mm, a matrix of 256, a temporal resolution of 0.5 s, a scan time of 16 s, and breath-hold image acquisition. Before the actual cine-MRI examination, coronal images of the entire abdomen were obtained to identify an appropriate imaging plane, and three optimal images were selected to cover the maximum length of the small bowel loops during each examination. Sequential scanning was performed every 0.5 s, with 30 images obtained within a scan time of 16 s for each coronal plane. Cine-MRI was performed in the morning on patients in fasting condition. Just prior to the examination, patients ingested 1000 ml of water orally to fill the small bowel loops and to enable easier determination of the bowel walls and more accurate measurements of the luminal diameter. Patients unable to ingest 1000 ml of water because of severe abdominal symptoms were encouraged to ingest no water or as much as possible to prevent any worsening of their symptoms.
Data sampling
Small bowel peristalsis was assessed as described [21], with small bowel motility function determined using software (Philips DICOM Viewer R3.0 SP3, Philips Healthcare). Three bowel segments (the proximal jejunum, middle intestine, and distal ileum) were selected for the caliber measurements. A line perpendicular to the long axis of the selected loops was drawn, with the same task repeated for all sequential images at exactly the same location (Fig. 2). The luminal diameters of the bowel loops were measured on all the images, and the temporal changes in caliber were plotted on a graph. The amplitude, contraction cycle, and contraction ratio were calculated using the following equations based on the completed graph (Fig. 3):
Graph of a cine-MRI images showing the methods used to calculate amplitude, contraction cycle, and contraction ratio. Amplitude = Caliber of maximum extension − Caliber of maximum contraction; contraction cycle = time between the maximum contractions; contraction ratio = amplitude/caliber of maximum extension
The mean luminal diameter (MLD), CR, and CC of the 11 healthy volunteers were reported to be 11.1 mm (95 % confidence interval [CI], 9.6–12.6 mm), 73.0 % (95 % CI, 63.7–82.3 %), and 7.8 s (95 % CI, 6.8–8.8 s) [21]. However, accepted normal ranges for these parameters have not yet been determined. Only one other study [22] has used cine-MRI to examine small bowel peristalsis in healthy volunteers; that study reported that MLD was 10.4 ± 4.5 mm, but did not evaluate CR. Therefore, only our previous study examined all these parameters using cine-MRI. Although currently available quantitative data on small intestinal peristalsis are insufficient to determine a normal range, the criteria for favorable small intestinal peristalsis were defined based on our previous data [21]. That is, individuals with an MLD < 15 mm or a CR ≥ 60 % were defined as having well-preserved peristalsis, whereas individuals with an MLD ≥ 15 mm and a CR < 60 % were defined as having decreased peristalsis.
Statistical analysis
Data were expressed as median and range or as mean ± standard deviation. All the parametric results were compared using Student’s t test, with p < 0.05 considered statistically significant. All statistical analyses were performed using commercially available software (SPSS Inc., Chicago, IL, USA).
Results
A total of 33 patients (21 female, 12 male) fulfilled the inclusion criteria. The median follow-up time was 25.2 months (range, 1–65 months). Of these 33 subjects, 23 (70 %) exhibited impairments in small intestinal peristalsis and 10 (30 %) did not.
The demographic data and the location of the dilated bowel loops on CT images of individual subjects are shown in Table 1. All patients with impaired small intestinal peristalsis, but none without impaired small intestinal peristalsis, had distended small bowel loops on CT.
The mean ± SD MLDs in patients with and without impaired small intestinal peristalsis and in healthy volunteers were 41.8 ± 14.2 mm, 13.6 ± 1.9 mm, and 11.0 ± 1.5 mm, respectively. The mean ± SD CRs in these three groups were 17.5 ± 11.8 %, 66.4 ± 10.4 %, and 75.1 ± 5.8 %, respectively, and the mean ± SD CCs were 8.4 ± 1.6 s, 6.8 ± 1.4 s, and 7.9 ± 1.0 s, respectively.
The MLD, CR, and CC for each subject are shown in Fig. 4. All parameters differed significantly between CIPO patients with and without impaired small intestinal peristalsis (p < 0.05). MLD and CR also differed significantly in CIPO patients with impaired peristalsis and healthy volunteers (p < 0.05). Although cine-MRI findings in the latter ten cases were within the normal range, significant differences in MLD and CR were observed between this group and the group of healthy volunteers (p < 0.05).
We have included a representative video recording (see Supplementary videos A–C online) and a typical image for each group of subjects (Figs. 4, 5). Patients with impaired peristalsis showed marked distention and severely disturbed contractions of the small intestine, whereas patients without impaired peristalsis and healthy volunteers showed non-dilated and well-preserved contractions of the small intestine.
Typical cine-MRI images for CIPO patients with and without impaired small intestinal peristalsis and healthy controls. Marked distention and severely disturbed contraction of the small intestine were observed in CIPO patients with impaired peristalsis, whereas no dilation and a well-preserved small intestine were observed in patients without impaired peristalsis and healthy controls
Table 2 shows the clinical features of the groups of CIPO patients with and without impaired small intestinal peristalsis. Detailed clinical records were not available for two and one patients, respectively; thus, the clinical features of 21 and nine patients, respectively, were reviewed. The frequency of intravenous hyperalimentation (IVH) was significantly higher (p = 0.03), and the mean serum albumin level was significantly lower (p = 0.04), in patients with than without impaired small intestinal peristalsis.
Five (23.8 %) patients with impaired small intestinal peristalsis died during the follow-up period. The causes of death of two patients were related to CIPO (aspiration pneumonia in one and septic translocation of the gastrointestinal tract in the other). Other causes of death were suicide and exacerbation of an underlying disease in one patient each; the fifth died of unknown causes.
Discussion
This retrospective study evaluated the ability and clinical significance of cine-MRI to assess small intestinal peristalsis in patients diagnosed with CIPO. To our knowledge, this was the first study to evaluate the relationship between clinical features and cine-MRI findings in patients with CIPO.
Two disease patterns were observed in CIPO patients who met the inclusion criteria, with one group showing severely impaired small intestinal peristalsis and the other showing an absence of severe impairment. All cine-MRI parameters differed significantly between these groups. Patients with severe impairment were significantly more likely to require IVH and had a significantly lower serum albumin level, suggesting a high likelihood of malnutrition. In contrast, fewer patients without severe impairment had severe clinical symptoms. Impaired small intestinal peristalsis may be associated with poorer clinical outcomes and/or reduced survival, and these findings are compatible with those of previous manometric studies [23, 24]. These results suggest that cine-MRI is a useful method of evaluating the severity of CIPO.
The ability to maintain sufficient oral intake was shown to be independently prognostic for survival in patients with CIPO [8]. Improvements in nutritional status may reduce patient mortality rates, especially in CIPO patients with disturbed small intestinal peristalsis. Assessments of small intestinal contractility may be useful in identifying patients at higher risk of malnutrition and in adopting appropriate therapeutic strategies.
Although CT showed no dilation of small bowel loops and cine-MRI showed that MLD and CR were within normal ranges in CIPO patients, these patients showed slight dilation and lower contractility of the small bowel loops, compared with healthy controls, when evaluated by cine-MRI.
Our previous study found that CC did not differ significantly among CIPO patients, IBS patients, and healthy volunteers [21]. However, this study found that CC was significantly slower in CIPO patients with than without impaired small intestinal peristalsis. Pathological abnormalities underlying CIPO can be classified into three major entities; neuropathies, mesenchymopathies, and myopathies. Mesenchymopathies are alterations in the interstitial cells of Cajal (ICC), which generate slow waves of phasic changes in intraluminal pressure and induce pacemaker activity of intestinal motility [25]. Therefore, disturbances in ICC may be associated with reduced contractility of bowel loops. Because myenteric nerves and ICC in the smooth muscle of the small intestine are much lower in patients with CIPO, CC may also become slower under such severely altered pathological conditions. However, as we did not assess the pathophysiology of CIPO, this hypothesis cannot be confirmed. Additional studies, including evaluation of pathophysiology, are needed in larger numbers of patients. Long-term evaluation of these patients may reveal whether this slight change leads to severely impaired small intestinal peristalsis.
This study had several limitations. First, there are no accepted criteria for normal ranges of cine-MRI parameters. Significant differences were observed among groups of patients within normal cine-MRI ranges. Accumulation of additional cine-MRI data and establishment of a gold standard for cine-MRI analysis are required. Second, the follow-up period varied among the study patients and may have been too short for precise assessment of clinical severity. However, all five patients who died had disturbed small intestinal peristalsis, strongly indicating that the clinical course was more severe in this group than in patients without impaired peristalsis. Third, all patients were evaluated by cine-MRI only once, at their first visit to our institution. Thus, the long-term outcome of small intestinal peristalsis is unclear. Long-term evaluation by cine-MRI and monitoring of CIPO patients are also required. Fourth, the retrospective design of this study and the extreme rarity of CIPO make it difficult to reduce the bias and generalize our conclusions. Prospective evaluations are required to establish the usefulness of cine-MRI in patients with CIPO. Fifth, because CIPO is a rare clinical entity, we could not accumulate sufficient patients to determine an appropriate sample size based on statistical analysis. Therefore, this study included all patients diagnosed with this condition over 5 years. Sixth, the exclusion of 22 patients because they did not undergo cine-MRI may have introduced the bias. Finally, cine-MRI was not directly compared with other modalities used to diagnose gastrointestinal motility disorders. At present, plain radiography, small-bowel follow-through, and CT are the main modalities used to diagnose CIPO. However, all of these modalities result in still images and cannot evaluate the actual motion of the small intestine. In Western countries, manometry also has had a supportive role in diagnosing CIPO. Although manometry is useful in evaluating peristalsis, it can only evaluate limited points of the small intestine. In contrast, cine-MRI can evaluate the peristaltic movements of the entire small bowel directly at any playback speed (e.g., fast-forward and slow-motion), allowing affected loops to be detected easily. Furthermore, cine-MRI is noninvasive and radiation-free. Because of these advantages, cine-MRI may in the future become a key modality in the diagnosis of CIPO.
In conclusion, cine-MRI is a promising diagnostic modality for evaluating differences in small bowel contractility among patients who meet the criteria for CIPO. Cine-MRI may be useful in predicting a severe clinical course, as well as being superior to CT in detecting early stages of impaired small intestinal contractility.
References
Cogliandro RF, De Giorgio R, Barbara G, et al. Chronic intestinal pseudo-obstruction. Best Pract Res Clin Gastroenterol. 2007;21:657–69.
Stanghellini V, Cogliandro RF, De Giorgio R, et al. Natural history of intestinal failure induced by chronic idiopathic intestinal pseudo-obstruction. Transplant Proc. 2010;42:15–8.
Stanghellini V, Cogliandro RF, De Giorgio R, et al. Chronic intestinal pseudo-obstruction: manifestations, natural history and management. Neurogastroenterol Motil. 2007;19:440–52.
Antonucci A, Fronzoni L, Cogliandro L, et al. Chronic intestinal pseudo-obstruction. World J Gastroenterol. 2008;14:2953–61.
Mann SD, Debinski HS, Kamm MA. Clinical characteristics of chronic idiopathic intestinal pseudo-obstruction in adults. Gut. 1997;41:675–81.
Sutton DH, Harrell SP, Wo JM. Diagnosis and management of adult patients with chronic intestinal pseudoobstruction. Nutr Clin Pract. 2006;21:16–22.
Iida H, Ohkubo H, Inamori M, et al. Epidemiology and clinical experience of chronic intestinal pseudo-obstruction in Japan: a nationwide epidemiologic survey. J Epidemiol. 2013;23:288–94.
Amiot A, Joly F, Alves A, et al. Long-term outcome of chronic pseudo-obstruction adult patients requiring home parenteral nutrition. Am J Gastroenterol. 2009;104:1262–70.
Stanghellini V, Cogliandro RF, De Giorgio R, et al. Natural history of chronic idiopathic intestinal pseudo-obstruction in adults: a single center study. Clin Gastroenterol Hepatol. 2005;3:449–58.
De Giorgio R, Sarnelli S, Corinaldesi R, et al. Advances in our understanding of the pathology of chronic intestinal pseudo-obstruction. Gut. 2004;53:1549–52.
Lindberg G, Tornblom H, Iwarzon M, et al. Full-thickness biopsy findings in chronic intestinal pseudo-obstruction and enteric dysmotility. Gut. 2009;58:1084–90.
Ohkubo H, Iida H, Takahashi H, et al. An epidemiologic survey of chronic intestinal pseudo-obstruction and evaluation of the newly proposed diagnostic criteria. Digestion. 2012;86:12–9.
Lauro A, De Giorgio R, Pinna AD. Advancement in the clinical management of intestinal pseudo-obstruction. Expert Rev Gastroenterol Hepatol. 2015;9:197–208.
Miazga A, Osinski M, Cichy W, et al. Current views on the etiopathogenesis, clinical manifestation, diagnostics, treatment and correlation with other nosological entities of SIBO. Adv Med Sci. 2015;60:118–24.
Scolapio JS, Fleming CR, Kelly DG, et al. Survival of home parental nutrition-treated patients: 20 years of experience at the Mayo Clinic. Mayo Clin Proc. 1999;74:217–22.
Amiot A, Joly F, Cazals-Hatem D, et al. Prognostic yield of esophageal manometry in chronic intestinal pseudo-obstruction: a retrospective cohort of 116 adult patients. Neurogastroenterol Motil. 2012;24:1008–e542.
Stanghellini V, Cogliandro R, Cogliandro L, et al. Clinical use of manometry for the diagnosis of intestinal motor abnormalities. Dig Liver Dis. 2000;32:532–41.
Bassotti G, Bologna S, Ottaviani L, et al. Intestinal manometry: who needs it? Gastroenterol Hepatol Bed Bench. 2015;8:246–52.
Rao SS, Camilleri M, Hasler WL, et al. Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil. 2011;23:8–23.
Takahara T, Kwee TC, Sadahiro S, et al. Low b-value diffusion-weighted imaging for diagnosing strangulated small bowel obstruction: a feasibility study. J Magn Reson Imaging. 2011;34:1117–24.
Ohkubo H, Kessoku T, Fuyuki A, et al. Assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction using cine-MRI. Am J Gastroenterol. 2013;108:1130–9.
Wakamiya M, Furukawa A, Kanasaki S, et al. Assessment of small bowel motility function with cine-MRI using balanced steady-state free precession sequence. J Magn Reson Imaging. 2011;33:1235–40.
Masaki T, Sugihara K, Nakajima A, et al. Nationwide survey on adult type chronic intestinal pseudo-obstruction in surgical institutions in Japan. Surg Today. 2012;42:264–71.
Lindberg G, Iwarzon M, Tornblom H. Clinical features and long-term survival in chronic intestinal pseudo-obstruction and enteric dysmotility. Scand J Gastroenterol. 2009;44:692–9.
Amiot A, Cazals-Hatem D, Joly F, et al. The role of immunohistochemistry in idiopathic chronic intestinal pseudoobstruction (CIPO): a case-control study. Am J Surg Pathol. 2009;33:749–58.
Acknowledgments
We thank Hiroshi Takahashi for his technical assistance and Kyoko Koike for her clerical assistance. This study was supported in part by grants for the Rare/Intractable Disease Project from the Japan Agency for Medical Research and Development (15545459).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fuyuki, A., Ohkubo, H., Higurashi, T. et al. Clinical importance of cine-MRI assessment of small bowel motility in patients with chronic intestinal pseudo-obstruction: a retrospective study of 33 patients. J Gastroenterol 52, 577–584 (2017). https://doi.org/10.1007/s00535-016-1251-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-016-1251-8