Abstract
Background
Although the prevalence of inflammatory bowel disease (IBD) is reported to have reached a plateau in Western countries, it is increasing in Asia. The etiology of IBD is still under investigation. We performed an epidemiological study to clarify the characteristics of IBD in Japan, focusing on patients’ family history.
Methods
We obtained clinical data on ulcerative colitis (UC) (46,114 cases) and Crohn’s disease (CD) (11,305 cases) in 2007 from an electronic database maintained under the Japanese Ministry of Health, Labour and Welfare’s nationwide registry system, and analyzed the differences in disease characteristics between patients with IBD who had a family history of the disease and those who did not.
Results
A total of 2.7% of the patients with UC and 2.6% of those with CD had a family history. The present age and age at disease onset were lower among the patients with UC who had a family history than among those without (present age: p < 0.001; age at disease onset: p < 0.001; Mann–Whitney U-test), but no similar trend was observed in the patients with CD. Disease severity was worse among both the UC and CD patients with a family history. The clinical course of patients with UC was not affected by family history. Levels of independence in daily life were associated with family history among CD patients, whereas age was associated with levels of independence in daily life among UC patients.
Conclusion
Disease characteristics of IBD vary in some aspects according to the presence or absence of a family history.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inflammatory bowel disease (IBD) includes 2 chronic diseases that cause inflammation of the intestines: ulcerative colitis (UC) and Crohn’s disease (CD). A complex interplay of environmental, genetic, and immunologic factors are involved in the development of IBD [1]. The incidence of IBD is higher in developed countries than in developing countries and among white populations than among non-white populations [2]. However, it is reported that the incidence of IBD has reached a plateau in the northern part of the world [3]. Meanwhile, its prevalence is steadily increasing in Asian countries in spite of improvements in IBD treatment [4]. Environmental change, modernization, and Westernization of lifestyle could be partly responsible for the rising incidence [4], but increasing awareness of IBD among physicians and the availability of better diagnostic tools must also be playing a part in the increasing number of reported cases in Asia [4]. Furthermore, improved socioeconomic conditions have led to a decline in the incidence of infectious colitis, and particularly tuberculosis, in many parts of Asia, which has allowed physicians to diagnose IBD with more confidence [4]. However, the precise reasons for the increasing incidence of IBD have not been fully elucidated.
Since 1972, the Japanese Ministry of Health, Labour and Welfare (MHLW) has been conducting a nationwide investigation to clarify the etiologies of and establish better treatments for patients with any of 45 intractable diseases who satisfy certain criteria [3]. UC and CD have been included in the list since 1975 and 1976, respectively. Patients in whom UC or CD is diagnosed on the basis of the specified diagnostic criteria are required to register annually with their local prefectural government, and each patient’s attending doctor is required to supply detailed information about the patient’s condition in the registration form. The submitted forms are evaluated by specialists on each prefecture’s Committee on Measures for Intractable Diseases, and those patients who pass this screening become eligible for financial aid for their treatment. A pilot study performed in 2004 found that 67.2% of patients claiming aid for UC treatment, and 76.7% of those claiming aid for CD were subsidized via this system (this result was reported in the annual report of the IBD Research Committee [in Japanese]). Since 2001, the prefectural governments have been making efforts to convert the data from the paper registration forms into electronic form. In 2009, Asakura et al. [5] used the electronic data to investigate the prevalence, age and sex distribution, and degree of IBD in Japan.
These electronic forms contain a wide range of data on patients with UC and CD: sex, age, age at onset, location of residence, family history (FH), clinical examination data, symptoms, and signs. The forms also provide data on a large number of patients (more than 40,000 patients with UC and more than 10,000 with CD), making them suitable for descriptive epidemiological analysis. FH is known to be a risk factor for IBD [3], and previous studies have indicated an association between FH and UC severity [6, 7], but no association between FH and CD severity [8, 9]. This large electronic database allowed us to carry out a more detailed investigation of IBD data to clarify the proportion of patients with an FH and the differences in disease characteristics between those with and without an FH of IBD.
Methods
Data source and questionnaire
We used the electronic data on IBD patients for the year 2007 furnished by the Japanese MHLW. Detailed information about the data available from the MHLW has been reported by Asakura et al. [5]. In short, the paper registration forms submitted by IBD patients are collected and converted into electronic form by their local prefectural governments each year. The conversion rates vary with the prefecture, but they range from around 40–60% every year. After the electronic data are anonymized, the MHLW makes them available for medical research. In 2007, 96,994 UC patients and 27,384 CD patients submitted registrations, of which 46,114 (47.5%) and 11,305 (41.3%), respectively, were converted into electronic form. We used only the electronic data for analysis.
Using these data, we examined the distribution of present age, age at disease onset, clinical course, severity of illness, and level of independence in daily life, paying particular attention to patients’ FH of IBD. Invalid data were excluded from the analysis. Attending doctors are required to supply details of FH of IBD in the registration forms. The registration forms include questions about FH of UC and CD for both UC and CD patients. We focused on UC patients’ FH of UC, and on CD patients’ FH of CD.
Clinical course is classified in the registration form according to the appearance of symptoms: one attack only; relapse-remitting; chronic continuous; acute fulminating; or unknown type. Patients are categorized as having the chronic continuous type if their symptoms continue for more than 6 months after the first attack. Acute fulminating type is applied to those whose symptoms are acute and severe with complications such as toxic megacolon, perforation, and septicemia. Classification as acute fulminating type indicates an extremely poor prognosis. Independence in daily life is classified into 5 categories: normal; some inconvenience; in need of partial support; in need of total support; and unknown. Classification is made on the basis of patients’ self-assessments and their doctors’ subjective opinions.
Statistical analysis
Continuous variables and categorical variables were analyzed with Fisher’s exact test or the χ2 test, as appropriate. All statistical analyses were performed with SPSS statistical software, version 18.0J (SPSS, Chicago, IL, USA); p < 0.05 was considered statistically significant.
Ethical considerations
Before filling out a registration form, the patients are asked by their attending doctors whether they consent to their clinical information being used for medical research. If the patients decline, the information is not recorded in the electronic data list. All data provided by the MHLW are anonymous, and researchers cannot access personal information such as the name or address of any patients.
Results
No record of sex was included in the data on 1 of the 46,114 patients registered as having UC and 1 of the 11,305 with CD; these 2 patients were excluded from the study. Table 1 shows that 2.7% of the UC patients and 2.6% of the CD patients had FH; 2.4% of the male UC patients had FH, as compared with 3.2% of the female UC patients. The male (n = 542) to female (n = 611) ratio of these patients was 0.89, while the M: F ratio of the UC patients without FH was 1.19 (male 22,330; female 18,708) (p < 0.001). On the other hand, among the 11,304 patients with CD, the data show no difference in the M: F ratio between patients with or without FH.
For 42,190 UC patients and 11,014 CD patients there was information about both their present age and FH. The peak age of the group without FH [FH (−) group] was 35–39 years among UC patients; in the group of patients with FH [FH (+) group], the peak age was lower than that of the FH (−) group: 30–34 years (Fig. 1). The present age was significantly lower among the patients with UC who had an FH than among those without an FH (p < 0.001; Mann–Whitney U-test). A secondary weak peak was observed at 55–59 years in both groups. Among the CD patients, the peak age in both the FH (+) and FH (−) groups was 30–34 years. No secondary peak in present age was observed in the FH (−) group, but there was a weak peak at 50–59 years in the FH (+) group.
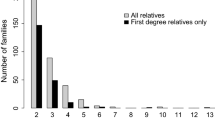
Figure 2 shows the distribution of age at disease onset. Information about both age at onset and FH was provided by 37,282 of the patients with UC and by 9,673 of those with CD. Among the UC patients, the peak onset age was 25–29 years in the FH (−) group. In the FH (+) group, the peak onset age was lower and the range was broader: 15–25 years. Age at disease onset was lower among the UC patients with FH than among those without FH (p < 0.001; Mann–Whitney U-test). The median age of CD onset in the FH (−) group was 24 years, and that of the FH (+) group was 25 years. The peak onset age was the same in both groups: 20–24 years.
Disease severity was graded according to Truelove and Witts’ criteria for UC [10], and according to the International Organization for the Study of Inflammatory Bowel Disease (IOIBD) score for CD [11]. After excluding data on patients who had not responded to the questions about disease severity and/or FH, those who responded that they did not know (“unknown”), and those who provided invalid information (e.g., an IOIBD score of over 10), we compared disease severity in patients with and without FH. Of the UC patients, 40,297 provided valid information about both disease severity and FH, and 9,091 CD patients provided information about both IOIBD scores and FH. In 33.3% of the UC patients without FH and 38.1% of those with FH, disease severity was moderate or severe (Fig. 3). Among the CD patients without FH, the largest group (24.9%) had an IOIBD score of 0; the largest group among the patients with FH (23.2%) had a score of 1. The differences in disease severity between the FH (+) and FH (−) groups showed statistical significance, using the χ2 test (χ2 = 12.6, p = 0.014 for UC, χ2 = 23.3, p = 0.010 for CD). Therefore, it can be concluded that patients with FH generally have greater disease severity than patients without FH.
Only the registration form for UC patients included a section concerning clinical course, which was classified as: one attack only; relapse-remitting; chronic continuous; acute fulminating; or unknown type. We excluded those who did not answer the question about clinical course (946 patients, 21 of whom reported FH, and 925 of whom reported no FH) and those whose answer was “unknown”, (859 patients, 28 of whom reported FH, and 831 of whom reported no FH). About 20% of the remaining patients were in the one-attack-only group, nearly 50% were in the relapse-remitting group, and nearly 25% were in the chronic continuous group. There was no significant difference in distribution between the FH (+) and FH (−) groups.
We analyzed the patient’s level of independence in daily life in association with FH, age, and severity of disease. Valid data on independence in daily life, age, and FH were available for 39,375 patients with UC and 10,313 with CD. First, we compared the levels of independence in daily life between the FH (+) and FH (−) groups (Fig. 4). Among the UC patients, there was no difference in the distribution of independence levels between the 2 groups: about 80% of the patients in both groups were able to lead normal daily lives. Among the CD patients, 61.7% of the patients with FH were able to lead normal lives; the corresponding figure for the patients without FH was 67.8% (χ2 = 9.04, p = 0.029). Contrary to our expectations, we found no statistically significant FH-related differences in independence levels among the UC patients. However, among the patients with CD, independence levels differed between the FH (+) and FH (−) groups. Next, we analyzed the patients’ levels of independence in daily life according to age. Figure 5 shows that about 80% of the UC patients in their teens through 50s led normal lives, but those in their 60s and over gradually encountered difficulties in daily life (p < 0.001). On the other hand, about 60% of the CD patients were able to lead consistently normal lives regardless of age, whereas about 25% of them experienced some inconvenience. As shown in Fig. 6, in both the UC and CD patients, difficulties in daily life increased in line with disease severity (p < 0.001 in both UC and CD). About 80% of the patients with mild UC were able to lead normal lives, whereas only about 40% of those with severe UC were able to do so. Similarly, about 80% of the CD patients with IOIBD scores of 0 lived normal lives, compared with about 30% of those with IOIBD scores of 10. Thus, the independence levels were lower among the CD patients than among the UC patients, especially among the young and middle-aged CD patients with FH.
Discussion
Several studies have investigated FH in relation to IBD. In China, for example, 1.48% of UC patients were found to have an FH [12], and a Korean study showed that 2.01% of UC patients and 1.51% of CD patients had first-degree FH [13]. It is difficult to compare our data directly with those of other epidemiological studies, because different collection methods were used. However, in Western countries, FH has been reported in 5–18% of IBD patients [8, 14–21], which is a much higher rate than that found in Asian studies, including ours. This may reflect the fact that genetic factors are related to IBD development. Of course the existence of FH does not mean directly that the patient has a certain gene or genetic characteristics, because people in the same family have similar lifestyles; namely, family members of IBD patients are exposed to environmental factors similar to those of the IBD patients. However, there are several studies that found genetic mutations specific for IBD and they are probably inherited by family members. We should consider that genetic factors are partly associated with the development of IBD. For example, according to some previous studies, gene mutations differed between different ethnic groups. The HLA-DRB1 alleles associated with UC differ between Asian and Western populations [22–27], and whereas the NOD-2 mutation is not associated with CD in Japanese [28], Chinese [29], or Koreans [30], an association has been identified in Western populations [31, 32]. Thus, the etiology of IBD appears to differ partially between Asian and Western populations. Also, it has been reported that the familial aggregation of IBD is greater among relatives of CD patients than among relatives of UC patients in Western populations [14–21]. In contrast, our study indicates that similar numbers of Japanese UC and CD patients have FHs. Further studies are needed to clarify this discrepancy between Western and Japanese populations.
In the present study, we investigated the differences in IBD characteristics between patients with and without FHs. A previous Japanese study found that 1.9% of UC patients and 1.5% of CD patients had FHs [33]; these rates are slightly lower than those found in the present study. One possible reason for this difference in rates is that improved diagnostic skills in the 15 years since the previous study was carried out have led to a higher rate of diagnosis. Also, family members of patients diagnosed with IBD might be inclined to view the appearance of gastrointestinal symptoms in themselves as a matter requiring quick medical consultation. Another possible reason for the discrepancy in the FH rates found between the previous and present studies may be the relationship between genetic factors and environmental factors, both of which are significant in the development of IBD. It is possible that IBD symptoms appear only when people with certain genetic make-ups are exposed to environmental factors that might cause IBD, such as Westernized dietary habits and better sanitation, both of which have been becoming more prevalent in Japanese society.
Our data correspond with those of Kitahora et al. [6], who reported that disease onset occurs earlier in UC patients with an FH than in those without an FH. Our data also agree with those presented in another report that showed no relation between FH and onset age in Japanese children with CD [7].
Few of the preceding studies mentioned differences in disease severity between adult patients with and without FH, although two indicated that FH had no impact on disease severity [8, 9]. However, we found that IBD patients with an FH tended to experience more severe symptoms than those without an FH. That we were able to detect this tendency may be because we examined data on a larger number of patients.
We found that the UC patients’ levels of independence in daily life were influenced by age but not by FH, whereas those of the CD patients were affected by FH. Moreover, young and middle-aged CD patients experienced more difficulty in daily life than similarly aged UC patients. This difference suggests that disease severity is greater in CD patients with FH, particularly in young patients.
Interestingly, we found that 30–40% of both UC and CD patients in the highest disease severity categories were able to live normal lives. The reason for this counter-intuitive finding is unclear, but one possible reason is that there may have been a time lag between the time when disease severity was judged and the time when individual patients’ independence in daily life was reported: in some cases, information on patients’ daily lives may have been reported after their disease had been treated.
Our study has 2 limitations. The first is that we had no information on the patients’ smoking habits. Smoking is thought to be a risk factor for CD and a determining factor in IBD severity [34, 35], although how it may be associated with FH is not known. The second limitation concerns the generalizability of our results. The information collected by prefectural governments is submitted only by those IBD patients applying for subsidization of their treatment costs and thereby agreeing to the use of their data for medical research. Patients who are in deprived circumstances and who are provided with public financial assistance do not need to be subsidized because the government covers all their medical expenses. In contrast, people who are wealthy enough and would not like to offer their personal information to the government may not apply for the subsidization. If wealthy patients were not included in the analysis, it is possible that the peak of the present age was estimated to be younger than the true value, because older people tend to have higher incomes. Also, if deprived patients were excluded from the analysis, the peak of the present age might also be estimated to be younger than the true value, because the percentage of people who receive public financial assistance is higher in the elderly population. In addition, these populations might include patients who live either in extremely clean or in unsanitary environments or have different lifestyle characteristics such as smoking habits and dietary habits. Thus, we should analyze the data carefully if the same population is again used to do a study to clarify IBD etiology, as there may be some bias regarding the socioeconomic status and condition of the patients whose data were analyzed. However, even if high- or low- income patients or those with mild disease conditions were missed by our study because they had no need of subsidization, the data at our disposal covered nearly 60% of IBD patients in Japan and probably constituted the most representative data on such patients available at the present time. Although the overall conversion rate from paper to electronic registration forms is rather low, we do not think this led to any bias, because data conversion to electronic forms depends only on the workforce allocated by local governments to perform the task and not on any factors relating to individual patients. The proportion of UC and CD patients with FHs was the same when we analyzed FH using data from local governments whose rates of conversion to electronic forms were 80% or more. Therefore, we think that the subjects on whom we obtained data are sufficiently representative.
In conclusion, we found that the presence of FH was associated with IBD severity, the onset age of UC, and the levels of independence in daily life of CD patients. On the other hand, in UC patients, we found no connection between FH and levels of independence in daily life or between FH and clinical course. The existence of FH may play an important role in the onset and severity not only of UC but also of CD. Furthermore, because the presence or absence of FH has a bearing on patients’ activities of daily living, paying attention to FH should allow physicians to better predict an individual patient’s disease course and prognosis.
References
Pinsk V, Lemberg DA, Grewal K, Barker CC, Schreiber RA, Jacobson K. Inflammatory bowel disease in the South Asian pediatric population of British Columbia. Am J Gastroenterol. 2007;102:1077–83.
Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004;126:1504–17.
Baumgart DC, Carding SR. Inflammatory bowel disease: cause and immunobiology. Lancet. 2007;369:1627–40.
Goh K, Xiao SD. Inflammatory bowel disease: a survey of the epidemiology in Asia. J Dig Dis. 2009;10:1–6.
Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn’s disease in Japan. J Gastroenterol. 2009;44:659–65.
Kitahora T, Utsunomiya T, Yokota A. Epidemiological study of ulcerative colitis in Japan: Incidence and familial occurrence. The Epidemiology Group of the Research Committee of Inflammatory Bowel Disease in Japan. J Gastroenterol. 1995;30(Suppl 8):5–8.
Ishige T, Tomomasa T, Takebayashi T, Asakura K, Watanabe M, Suzuki T, et al. Inflammatory bowel disease in children: epidemiological analysis of the nationwide IBD registry in Japan. J Gastroenterol. 2010;45:911–7.
Ben-Horin S, Avidan B, Yanai H, Lang A, Chowers Y, Bar-Meir S. Familial clustering of Crohn’s disease in Israel: prevalence and association with disease severity. Inflamm Bowel Dis. 2009;15:171–5.
Carbonnel F, Macaigne G, Beaugerie L, Gendre JP, Cosnes J. Crohn’s disease severity in familial and sporadic cases. Gut. 1999;44:91–5.
Truelove SC, Witts LJ. Cortisone in ulcerative colitis. Final report on a therapeutic trial. Br Med J. 1955;2:1041–8.
de Dombal F, Softley A. IOIBD report no 1: Observer variation in calculating indices of severity and activity in Crohn’s disease. International Organisation for the Study of Inflammatory Bowel Disease. Gut. 1987;28(4):474–81.
Jiang XL, Cui HF. An analysis of 10218 ulcerative colitis cases in China. World J Gastroenterol. 2002;8:158–61.
Park JB, Yang SK, Byeon JS, Park ER, Moon G, Myung SJ, et al. Familial occurrence of inflammatory bowel disease in Korea. Inflamm Bowel Dis. 2006;12:1146–51.
Monsén U, Broström O, Nordenvall B, Sörstad J, Hellers G. Prevalence of inflammatory bowel disease among relatives of patients with ulcerative colitis. Scand J Gastroenterol. 1987;22:214–8.
Monsén U, Bernell O, Johansson C, Hellers G. Prevalence of inflammatory bowel disease among relatives of patients with Crohn’s disease. Scand J Gastroenterol. 1991;26:302–6.
Yang H, McElree C, Roth MP, Shanahan F, Targan SR, Rotter JI. Familial empirical risks for inflammatory bowel disease: differences between Jews and non-Jews. Gut. 1993;34:517–24.
Roth MP, Petersen GM, McElree C, Vadheim CM, Panish JF, Rotter JI. Familial empiric risk estimates of inflammatory bowel disease in Ashkenazi Jews. Gastroenterology. 1989;96:1016–20.
Farmer RG, Michener WM, Mortimer EA. Studies of family history among patients with inflammatory bowel disease. Clin Gastroenterol. 1980;9:271–7.
Kirsner JB, Spencer JA. Family occurrences of ulcerative colitis, regional enteritis, and ileocolitis. Ann Intern Med. 1963;59:133–44.
Lewkonia RM, McConnell RB. Progress report: familial inflammatory bowel disease: heredity or environment? Gut. 1976;17:235–41.
Tysk C, Lindberg E, Järnerot G, Flodérus-Myrhed B. Ulcerative colitis and Crohn’s disease in an unselected population of monozygotic and dizygotic twins: a study of heritability and the influence of smoking. Gut. 1988;29:990–6.
Futami S, Aoyama N, Honsako Y, Tamura T, Morimoto S, Nakashima T, et al. HLA-DRB1*1502 allele, subtype of DR15, is associated with susceptibility to ulcerative colitis and its progression. Dig Dis Sci. 1995;40:814–8.
Yoshitake S, Kimura A, Okada M, Yao T, Sasazuki T. HLA class II alleles in Japanese patients with inflammatory bowel disease. Tissue Antigens. 1999;53:350–8.
Myung SJ, Yang SK, Jung HY, Chang HS, Park B, Hong WS, et al. HLA-DRB1*1502 confers susceptibility to ulcerative colitis, but is negatively associated with its intractability: a Korean study. Int J Colorectal Dis. 2002;17:233–7.
De La Concha EG, Fernandez-Arquero M, Santa-Cruz S, Lopez-Nava G, Figueredo MA, Diaz-Rubio M, et al. Positive and negative associations of distinct HLA-DR2 subtypes with ulcerative colitis (UC). Clin Exp Immunol. 1997;108:392–5.
Satsangi J, Welsh KI, Bunce M, Julier C, Farrant JM, Bell JI, et al. Contribution of genes of the major histocompatibility complex to susceptibility and disease phenotype in inflammatory bowel disease. Lancet. 1996;347:1212–7.
Cottone M, Bunce M, Taylor CJ, Ting A, Jewell DP. Ulcerative colitis and HLA phenotype. Gut. 1985;26:952–4.
Inoue N, Tamura K, Kinouchi Y, Fukuda Y, Takahashi S, Ogura Y, et al. Lack of common NOD2 variants in Japanese patients with Crohn’s disease. Gastroenterology. 2002;123:86–91.
Leong RW, Armuzzi A, Ahmad T, Wong ML, Tse P, Jewell DP, et al. NOD2/CARD15 gene polymorphisms and Crohn’s disease in the Chinese population. Aliment Pharmacol Ther. 2003;17:1465–70.
Croucher PJ, Mascheretti S, Hampe J, Huse K, Frenzel H, Stoll M, et al. Haplotype structure and association to Crohn’s disease of CARD15 mutations in two ethnically divergent populations. Eur J Hum Genet. 2003;11:6–16.
Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411:603–6.
Hugot JP, Chamaillard M, Zouali H, Lesage S, Cézard JP, Belaiche J, et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411:599–603.
Annual report of the Research Committee of “intractable inflammatory bowel disease”, 1992. The Ministry of Health and Welfare of Japan, Tokyo; 1993 (in Japanese).
Aldhous MC, Drummond HE, Anderson N, Baneshi MR, Smith LA, Arnott ID, et al. Smoking habit and load influence age at diagnosis and disease extent in ulcerative colitis. Am J Gastroenterol. 2007;102:589–97.
Smith BR, Arnott ID, Drummond HE, Nimmo ER, Satsangi J. Disease location, anti-Saccharomyces cerevisiae antibody, and NOD2/CARD15 genotype influence the progression of disease behavior in Crohn’s disease. Inflamm Bowel Dis. 2004;10:521–8.
Acknowledgments
The members of this Japanese IBD Research Group were organized by the Ministry of Health, Labour and Welfare of Japan. This work was supported in part by Health and Labour Sciences Research Grants for Research on Intractable Diseases from the Ministry of Health, Labour and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuwahara, E., Asakura, K., Nishiwaki, Y. et al. Effects of family history on inflammatory bowel disease characteristics in Japanese patients. J Gastroenterol 47, 961–968 (2012). https://doi.org/10.1007/s00535-012-0558-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-012-0558-3