Abstract
Background
Nucleotide analogues have recently been approved for the treatment of patients with hepatitis B virus (HBV) infection. However, it is still controversial whether the decrease of HBV-DNA amount induced by treatment with nucleotide analogues can reduce the risk of hepatocellular carcinoma (HCC) development in HBV patients.
Methods
A total of 293 HBV patients without HCC who were treated with lamivudine (LAM) were enrolled in a multicenter trial. The incidence of HCC was examined after the start of LAM therapy, and the risk factors for liver carcinogenesis were analyzed. The mean follow-up period was 67.6 ± 27.4 months.
Results
On multivariate analysis for HCC development in all patients, age ≥50 years, platelet count <14.0 × 104/mm3, cirrhosis, and median HBV-DNA levels of ≥4.0 log copies/ml during LAM treatment were significant risk factors. The cumulative carcinogenesis rate at 5 years was 3% in patients with chronic hepatitis and 30% in those with cirrhosis. For the chronic hepatitis patients, the log-rank test showed the significant risk factors related to HCC development to be age ≥50 years, platelet count <14.0 × 104/mm3, and hepatitis B e antigen negativity, but median HBV-DNA levels of <4.0 log copies/ml (maintained viral response, MVR) did not significantly suppress the development of HCC. In cirrhosis patients, however, the attainment of MVR during LAM treatment was revealed to reduce the risk of HCC development.
Conclusions
These results suggest that the incidence of HCC in HBV patients with cirrhosis can be reduced in those with an MVR induced by consecutive LAM treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 350 million people worldwide suffer from chronic infection with hepatitis B virus (HBV) [1–3]. Chronic HBV infection eventually leads to the development of cirrhosis and hepatocellular carcinoma (HCC), and raises the risk of hepatic disease-related death [4–6]. In Japan, up to 15% of HCC patients are diagnosed with HBV-related liver disease [7].
HCC is one of the most common malignancies in Japan and its incidence has been increasing over the past 30 years. Recently, various treatments such as transcatheter arterial embolization/chemoembolization, radio-frequency ablation, and hepatic resection have been reported to yield significant improvements in overall patient survival [8–11]. However, HCC relapse has thus far been observed in a majority of treated patients due to its highly malignant potential. In this regard, successful treatment of chronic HBV infection should prevent the patient’s liver from progressing to cirrhosis and reduce the risk of HCC development. In recent years, the treatment of chronic hepatitis has changed greatly with the development of various antiviral therapies with nucleoside/nucleotide analogues such lamivudine (LAM), adefovir (ADV), and entecavir (ETV) [12–15]. LAM has long been used against chronic hepatitis, and many reports have demonstrated that LAM is effective in stabilizing inflammatory activity, suppressing HBV-DNA replication, and improving liver histological findings in chronic hepatitis patients [16, 17] and in HBV-related cirrhosis patients [18]. Furthermore, LAM has been reported to reduce the incidence of HCC in patients with chronic hepatitis B [19]. However, it is still controversial whether or not treatment using nucleotide analogues can reduce the risk of HCC development in HBV-infected patients [20, 21], and the relationship between the effect of HBV suppression and HCC development during LAM treatment has not yet been discussed in detail. Also, the risk factors for HCC development in HBV-infected patients who have been treated with LAM have not been sufficiently evaluated. In this study, we aimed to clarify whether the decrease of HBV-DNA amount induced by LAM therapy could reduce the incidence of HCC in HBV-infected patients.
Patients and methods
Patient selection and study design
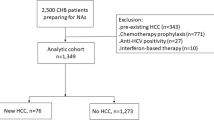
This study was conducted at Osaka University Hospital and other institutions participating in the Osaka Liver Forum in Japan. The subjects were 293 consecutive patients with HBV infection who underwent continuous LAM therapy for more than 24 weeks from September 2000 to September 2006. All patients tested positive for hepatitis B surface antigen (HBs Ag) or had detectable levels of HBV DNA in their sera according to findings from a polymerase chain reaction (PCR)-based method or a transcription-mediated amplification (TMA) method. Exclusion criteria were patients with anti-hepatitis C antibody, anti-human immunodeficiency virus antibody, and other liver diseases (alcoholic liver disease, drug-induced liver disease, and autoimmune hepatitis). Also excluded were patients with a history of HCC and those who developed HCC within the first 24 weeks of the follow-up period after the initiation of LAM therapy (because of the possibility that microscopic HCC had been present before the initiation of treatment).
All patients were treated with 100 mg of LAM daily. Of the 293 patients, 129 underwent ADV (10 mg/day) therapy in addition to receiving ongoing LAM treatment. For 43 patients who started ETV administration in lieu of LAM, the observation period was terminated when they started ETV. LAM resistance was confirmed by virological breakthrough and was defined as an increase in serum HBV-DNA by >1 log10 greater than the nadir [22]. If virological breakthrough developed and alanine aminotransferase (ALT) was elevated over the upper normal limit, the patients received add-on ADV at 10 mg/day.
In this study, all patients were examined for serum HBV-DNA level just before therapy initiation and every 6 months during treatment. The initial viral response (IVR) was defined as HBV-DNA <4.0 log copies/ml in the first 24 weeks of the follow-up period after the initiation of LAM therapy, and the maintained viral response (MVR) was defined as median HBV-DNA levels of less than 4.0 log copies/ml measured every 6 months during therapy.
This study protocol followed the ethical guidelines of the Declaration of Helsinki amended in 2008, and informed consent was obtained from each patient.
HBV testing
HBs Ag, hepatitis B e antigen (HBe Ag) and anti-hepatitis B e antibody (anti-HBe) levels were examined by chemiluminescence immunoassay or enzyme immunoassay. HBV DNA was measured by a PCR-based method (Amplicor HBV monitor; Roche Diagnostics, Tokyo, Japan) or a TMA method (TMA-HPA; Fujirebio, Tokyo, Japan), which have lower detection limits of 2.6 and 3.7 log copies/ml, respectively. The LAM-resistant YMDD mutant virus was examined by a PCR-ELMA method. Serum samples were stored frozen at −80°C.
Diagnosis of HCC and cirrhosis
Ultrasonography was carried out before LAM therapy and every 3–6 months during the follow-up period. New space-occupying lesions detected or suspected at the time of ultrasonography were further examined by computed tomography (CT), magnetic resonance imaging (MRI), or hepatic angiography. HCC was diagnosed by the presence of typical hypervascular characteristics on angiography, in addition to the findings from CT or MRI. If no typical image of HCC was observed, fine-needle aspiration biopsy was carried out with the patient’s consent or the patient was carefully followed until a diagnosis was possible with definite observation by CT, MRI, or hepatic angiography. Cirrhosis was diagnosed by liver biopsy or laparoscopy, and for patients without this information, by clinical data, imaging modalities, and portal hypertension.
Statistical analysis
Quantitative variables were expressed as means ± SD. Quantitative variables at the baseline were compared among two groups, the chronic hepatitis and cirrhosis groups, using the Mann–Whitney U-test. Categorical data, such as gender and status of HBe Ag, were compared using Fisher’s exact test. The cumulative incidence of HCC was evaluated with a Kaplan–Meiercurve and the differences between groups were analyzed by the log-rank test. For multivariate analysis to investigate factors affecting the cumulative incidence of HCC, Cox’s regression analysis was carried out. A value of p < 0.05 (two-tailed) was considered to be statistically significant. All calculations were performed with SPSS version 15.0J (SPSS, Chicago, IL, USA).
Results
Baseline characteristics of patients
The baseline clinical features of the enrolled patients before LAM administration are shown in Table 1. The mean age of the patients was 48.0 ± 10.7 years, 214 (73%) of the entire group were male, and 163 (56%) tested positive for HBe Ag. Of the 293 patients, 205 (70%) were diagnosed as having chronic hepatitis and 88 (30%) as having cirrhosis. The median HBV-DNA level was 7.0 (range 3.0 to 8.5<) log copies/ml. At baseline, the aspartate aminotransferase (AST) level was 131 ± 151 IU/l, the ALT level was 203 ± 252 IU/l, the total bilirubin level was 1.2 ± 1.6 mg/dl, the albumin (Alb) level was 3.8 ± 0.5 g/dl, and the platelet count was 13.7 ± 5.4 × 104/mm3. The mean follow-up period for all patients was 67.6 ± 27.4 months, with a range of 12–110 months from the start of LAM treatment. There were significant differences between patients with chronic hepatitis and those with liver cirrhosis in age, AST, ALT, total bilirubin, Alb, and platelet counts.
Cumulative incidence of development of HCC
Figure 1a shows the Kaplan–Meier curve of the cumulative HCC incidence for all HBV patients treated with LAM or LAM plus ADV. Of the 293 patients with HBV infection, 32 (10.9%) developed HCC and the cumulative carcinogenesis rate was 6% at 3 years, 12% at 5 years, and 15% at 7 years.
Figure 1b shows the Kaplan–Meier curve of the cumulative HCC incidence according to initial diagnosis (chronic hepatitis vs. cirrhosis). Eight (4%) of the 205 enrolled chronic hepatitis patients developed HCC and the cumulative carcinogenesis rate was 2% at 3 years, 3% at 5 years, and 5% at 7 years. On the other hand, 24 (27%) of the 88 enrolled cirrhosis patients developed HCC and the cumulative carcinogenesis rate was 15% at 3 years, 30% at 5 years, and 35% at 7 years.
Risk factors for cumulative incidence of HCC development in all HBV-infected patients
Univariate analysis with the log-rank test was performed for all HBV-infected patients treated with LAM, with the results shown in Table 2. Univariate analysis with the log-rank test showed that the following were significant risk factors for the development of HCC: older age (≥50 years) (p < 0.001), cirrhosis (p < 0.001), high total bilirubin level (>1.2 g/dl) (p = 0.004), low Alb level (<3.8 g/dl) (p = 0.019), low platelet count (<14 × 104/mm3) (p < 0.001), and non-MVR (p = 0.035).
Stepwise multivariate analyses of four of these variables were performed by Cox’s regression analysis for all patients treated with LAM with the results shown in Table 3. The analysis indicated the following factors as independent significant risk factors related to the development of HCC: age ≥50 years [hazard ratio (HR) 3.20, 95% confidence interval [CI] 1.08–9.53, p = 0.036], platelet count <14.0 × 104/mm3 (HR 4.76, 95% CI 0.05–0.96, p = 0.045), cirrhosis (HR 4.64, 95% CI 1.75–12.4, p = 0.002), and non-MVR (HR 2.70, 95% CI 1.09–6.56, p = 0.032).
Cumulative incidence of and risk factors for HCC development in patients with chronic hepatitis and cirrhosis
The results of univariate analysis with the log-rank test for the development of HCC in chronic hepatitis patients treated with LAM are shown in Table 4, and the following were significant risk factors: older age (≥50 years) (p = 0.002), HBe Ag negativity (p = 0.005), and low platelet count (<14 × 104/mm3) (p = 0.004). Suppression of median HBV-DNA levels to <4.0 log copies/ml by LAM treatment was not associated with the development of HCC in the chronic hepatitis patients. Only non-MVR (median HBV-DNA amount ≥4.0 log copies/ml) was shown to be a significant risk factor for the development of HCC in the cirrhosis patients (p = 0.029), while the factors of age, HBe Ag status, and platelet count were not significant in these patients (Table 4).
Cumulative incidence of HCC development according to effectiveness of treatment (MVR vs. non-MVR)
Figure 2a shows the Kaplan–Meier curve of cumulative HCC incidence in all HBV-infected patients treated with LAM according to the effectiveness of treatment (MVR vs. non-MVR). The cumulative carcinogenesis rate for MVR-positive patients was 2% at 3 years, 4% at 5 years, and 6% at 7 years. On the other hand, the cumulative carcinogenesis rate for MVR-negative patients was 5% at 3 years, 13% at 5 years, and 16% at 7 years. MVR during LAM significantly suppressed the cumulative HCC incidence compared with non-MVR in all HBV-infected patients (p = 0.035).
Figure 2b shows the Kaplan–Meier curve of the cumulative HCC incidence in chronic hepatitis patients according to the effectiveness of treatment (MVR vs. non-MVR). The cumulative carcinogenesis rate for MVR-positive patients was 0% at 3 years, 0% at 5 years, and 2% at 7 years. On the other hand, the cumulative carcinogenesis rate for MVR-negative patients was 2% at 3 years, 4% at 5 years, and 6% at 7 years. MVR during LAM did not significantly suppress the cumulative HCC incidence compared with non-MVR in the chronic hepatitis patients (p = 0.144).
Figure 2c shows the Kaplan–Meier curve of the cumulative HCC incidence in cirrhosis patients according to the effectiveness of treatment (MVR vs. non-MVR). The cumulative carcinogenesis rate for MVR-positive patients was 8% at 3 years, 14% at 5 years, and 14% at 7 years. On the other hand, the cumulative carcinogenesis rate for MVR-negative patients was 18% at 3 years, 40% at 5 years, and 44% at 7 years. MVR during LAM significantly suppressed the cumulative HCC incidence compared with non-MVR in the cirrhosis patients (p = 0.029).
Relationship between IVR and MVR
Maintained viral response (MVR) was achieved by 142 (48%) of the 293 patients enrolled in this study. IVR was achieved by 204 (79%) of the 259 patients who were examined for IVR. The relationship between IVR and MVR is shown in Fig. 3; 60% (122/204) of the IVR-positive patients achieved an MVR, while only 16% (9/55) of the IVR-negative patients achieved an MVR (p < 0.001). The LAM-resistant YMDD mutant virus was found in 149 (51%) of all patients during follow-up, and in 52% (107/204) of the IVR-positive patients, a finding which was nearly equal to that for the IVR-negative patients (51%, 28/55). Among the IVR-positive patients, the MVR rate was lower in patients with the YMDD mutation, compared with that in those without the YMDD mutation (44%, 47/107 vs. 77%, 75/97, p = 0.016), while the MVR rates were low in the IVR-negative patients, irrespective of their YMDD mutation status (with and without the mutation, 15 vs. 18%, respectively). ADV was added to LAM treatment for 73 (68%) of the 107 IVR-positive patients with the YMDD mutation and 20 (36%) of the 55 IVR-negative patients with the YMDD mutation. However, MVR was only achieved at the low rates of 33% (24/73) for the former patients and 20% (4/20) for the latter.
Discussion
Lamivudine treatment has been shown to improve the liver histological findings in patients with HBV-infected liver disease by reducing the HBV load and stabilizing inflammatory activity [16–18]. One report has shown that LAM effectively reduced the incidence of HCC in patients with chronic hepatitis B, but the study only compared LAM-treated patients with non-treated patients in a matched case-controlled study [19]. However, there have been few detailed reports about the relationship between virological response and HCC development in HBV-infected patients during LAM treatment. In the present study, we retrospectively examined the incidence of HCC to clarify the indicators of LAM therapy, including median HBV-DNA levels, for reducing the risk of HCC in HBV-infected patients.
Many investigators have reported that serum HBV DNA levels higher than 4.0–4.5 log copies/ml before HBV treatment serve as a strong risk predictor of HCC [23–25]. Di Marco et al. [26] have reported that the incidence of HCC was higher in patients with serum HBV levels of more than 5.0 log copies/ml, at least once, during LAM therapy than in those in whom serum HBV levels were maintained at 5.0 log copies/ml or less. However, the add-on ADV therapy had not been adopted when the study of Di Marco et al. was reported. When the use of ADV is possible, an evaluation method is needed to measure the antiviral effects of nucleoside/nucleotide analogues against HBV-related liver disease. In the present study, we set the cut-off value for HBV-DNA at 4.0 log copies/ml. The basis of this cut-off value is that a serum HBV DNA level higher than 4.0 log copies/ml before HBV treatment was reported to serve as a strong risk predictor of HCC [23]. MVR, defined as a median HBV-DNA level of less than 4.0 log copies/ml measured every 6 months during therapy, was adopted as an indicator of viral replication, and non-MVR (median HBV-DNA >4.0 log copies/ml) during LAM therapy was shown to be significantly associated with the development of HCC in HBV-infected patients. We also found that a median HBV-DNA level of >4.0 log copies/ml during LAM therapy was a risk factor for HCC development. On the other hand, IVR, defined as HBV-DNA of <4.0 log copies/ml in the first 6 months of the follow-up period after the initiation of therapy, was not associated with the development of HCC in HBV patients in this study. As shown in Fig. 3, 84% of the IVR-negative patients could not achieve an MVR, suggesting that it is crucial to achieve an IVR in order to achieve an MVR. The reason why IVR was not a significant factor for MVR seemed to be the appearance of the YMDD mutation, which reduced the antiviral effect of LAM for HBV in IVR-positive patients. The LAM-resistant YMDD mutant virus was found in 52% of the IVR-positive patients. Although ADV was added to LAM treatment for 73 patients, only 33% of these patients could achieve an MVR. We speculate that the antiviral effect of ADV is not very strong [27] and it takes time to reduce the YMDD mutant virus, which may explain the low MVR rate (33%) in patients with the add-on ADV therapy. The immediate administration of ADV when the LAM-resistant YMDD mutant virus appears can be important [28]. A switch to ETV, which induces resistant virus less frequently, could also raise MVR rates among IVR-positive patients without the YMDD mutant virus.
As the duration of the add-on ADV therapy was included in this study, we compared the cumulative incidence of HCC in patients receiving LAM monotherapy with that in patients who also received the add-on ADV therapy. Sixteen (10%) of the 164 patients who received the LAM monotherapy developed HCC and the cumulative carcinogenesis rate was 6% at 3 years, 10% at 5 years, and 15% at 7 years. On the other hand, 16 (12%) of the 129 patients who received LAM plus ADV developed HCC and the cumulative carcinogenesis rate was 6% at 3 years, 12% at 5 years, and 14% at 7 years. No significant difference was found between these two groups (p = 0.986). In addition, we examined the cumulative incidence of HCC development according to the effectiveness of treatment (MVR vs. non-MVR) in patients for whom the observation period was terminated when ADV was added, and the same results were obtained (data not shown).
Older age (≥50 years), cirrhosis, and low platelet count (<14 × 104/mm3) were shown to be significantly associated with the development of HCC in patients with HBV infection. These results were consistent with those of previous reports [29–31], suggesting that patients of older age with advanced fibrosis should be followed up carefully for longer periods in order to detect early stages of HCC even if LAM therapy does effectively suppress HBV. Of note, in the present study we estimated the cumulative HCC incidence according to the initial diagnosis of chronic hepatitis or cirrhosis. In the chronic hepatitis patients, older age (≥50 years), HBe Ag negativity, and low platelet count (<14 × 104/mm3) were significant risk factors for the development of HCC, but this was not the case in the cirrhosis patients. Because liver biopsies had not been performed, the liver fibrosis stage could not be evaluated with respect to the risk factors for HCC in this study. Instead, the factors of age, HBe Ag status, and platelet count may reflect the degree of liver fibrosis in chronic hepatitis patients. In fact, cirrhotic patients, in comparison with chronic hepatitis patients, were of older age (chronic hepatitis vs. cirrhosis: 46.3 ± 10.7 vs. 51.9 ± 9.8 years, p < 0.001), had higher rates of HBe Ag negativity (chronic hepatitis vs. cirrhosis: 39 vs. 51%, p = 0.065), and had lower platelet counts (chronic hepatitis vs. cirrhosis: 15.6 ± 4.9 vs. 9.3 ± 3.8 × 104/mm3, p < 0.001). This seems to explain why none of these factors were significant risk factors for HCC in cirrhotic patients. On the other hand, in the chronic hepatitis patients, MVR was not a significant factor for HCC development, while MVR was a significant factor for HCC development in the cirrhotic patients. We speculate that HBV suppression induced by LAM therapy could reduce the incidence of HCC in patients infected with HBV, especially those with cirrhosis, who displayed higher malignant potential. Investigation over a longer period is needed to clarify the effect of HBV suppression on the development of HCC in chronic hepatitis patients.
In conclusion, the present study shows that the attainment of an MVR induced by LAM therapy has a significant beneficial effect on the clinical course of HBV-infected patients by decreasing the incidence of HCC. The newer nucleotide analogues, such as ETV and tenofovir, should be able to further reduce the incidence of HCC, given their greater potency.
Abbreviations
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- LAM:
-
Lamivudine
- ADV:
-
Adefovir
- ETV:
-
Entecavir
- Hbs Ag:
-
Hepatitis B surface antigen
- PCR:
-
Polymerase chain reaction
- TMA:
-
Transcription-mediated amplification
- IVR:
-
Initial viral response
- MVR:
-
Maintained viral response
- HBe Ag:
-
Hepatitis B e antigen
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- ALT:
-
Alanine aminotransferase
References
Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007;45:507–39.
Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107.
Lee WM. Hepatitis B virus infection. N Engl J Med. 1997;337:1733–45.
Beasley RP. Hepatitis B virus: the major etiology of hepatocellular carcinoma. Cancer. 1988;61:1942–56.
Lok SF. Chronic hepatitis B. N Engl J Med. 2002;346:1682–3.
Tang B, Kruger WD, Chen G, Shen F, Lin WY, Mboup S, et al. Hepatitis B viremia is associated with increased risk of hepatocellular carcinoma in chronic careers. J Med Virol. 2004;72:35–40.
Kim SR, Kudo M, Hino O, Han KH, Chung YH, Lee HS. Epidemiology of hepatocellular carcinoma in Japan and Korea. A review. Oncology. 2008;75:13–6.
Marcellin P, Chang TT, Lim SG, Tong MJ, Sievert W, Shiffman ML, et al. Adefovir dipivoxil for the treatment of hepatitis B e antigen-positive chronic hepatitis B. N Engl J Med. 2003;348:808–16.
Taura K, Ikai I, Hatano E, Fujii H, Uyama N, Shimahara Y. Implication of frequent local ablation therapy for intrahepatic recurrence in prolonged survival of patients with hepatocellular carcinoma undergoing hepatic resection: an analysis of 610 patients over 16 years old. Ann Surg. 2006;244:265–73.
Shimada K, Sano T, Sakamoto Y, Kosuge T. A long-term follow-up and management study of hepatocellular carcinoma patients surviving for 10 years or longer after curative hepatectomy. Cancer. 2005;104:1939–47.
Takayasu K, Arii S, Ikai I, Omata M, Okita K, Ichida T, et al. Prospective cohort study of transarterial chemoembolization for unresectable hepatocellular carcinoma in 8510 patients. Gastroenterology. 2006;131:461–9.
Dienstag JL, Perrillo RP, Schiff ER, Bartholomew M, Vicary C, Rubin M. A preliminary trial of lamivudine for chronic hepatitis B infection. N Engl J Med. 1995;333:1657–61.
Nevens F, Main J, Honkoop P, Tyrrell DL, Barber J, Sullivan MT, et al. Lamivudine therapy for chronic hepatitis B: a six-month randomized dose-ranging study. Gastroenterology. 1997;113:1258–63.
Rapti I, Dimou E, Mitsouka P, Hadziyannis SJ. Adding-on versus switching-to adefovir therapy in lamivudine-resistant HBVAg-negative chronic hepatitis B. Hepatology. 2007;45:307–13.
Chang TT, Lai CL, Kew Yoon S, Lee SS, Coelho HS, Carriho FJ, et al. Entecavir treatment for 5 years in patients with hepatitis Be antigen-positive chronic hepatitis B. Hepatology. 2010;51:422–30.
Kiyosawa K, Tanaka E, Sodeyama T. Hepatitis C virus and hepatocellular carcinoma. Curr Stud Hematol Blood Transfus. 1998;62:161–80.
Ohkoshi S, Norio O, Ichida T. The long-term clinical outcome of 1-year treatment of chronic hepatitis B with lamivudine-5 years observation. Hepatol Res. 2003;27:13–7.
Chu CM, Liaw YF. Hepatitis B virus-related cirrhosis: natural history and treatment. Semin Liver Dis. 2006;26:142–52.
Matsumoto A, Tanaka E, Rokuhara A, Kiyosawa K, Kumada H, Omata M, et al. Efficacy of lamivudine for preventing hepatocellular carcinoma in chronic hepatitis B: a multicenter retrospective study of 2795 patients. Hepatol Res. 2005;32:173–84.
Shamliyan TA, MacDonald R, Shaukat A, Taylor BC, Yuan JM, Johnson JR, et al. Antiviral therapy for adults with chronic hepatitis B: a systematic review for a National Institutes of Health Consensus Development Conference. Ann Intern Med. 2009;150(2):111–24.
Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, et al. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004;351(15):1521–31.
Perrillo R, Hann HW, Mutimer D, Willems B, Leung N, Lee WM, et al. Adefovir dipivoxil added to ongoing lamivudine in chronic hepatitis B with YMDD mutant hepatitis B virus. Gastroenterology. 2004;126:81–90.
Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73.
Chan HL, Hui AY, Wong ML, Tse AM, Hung LC, Wong VW, et al. Genotype C hepatitis B virus infection is associated with increased risk of hepatocellular carcinoma. Gut. 2004;53:1494–8.
Chan HL, Tse CH, Koh FM, Wong VW, Wong GL, Chan SL, et al. High viral load and hepatitis B virus subgenotype Ce are associated with increased risk of hepatocellular carcinoma. J Clin Oncol. 2008;26:177–82.
Di Marco V, Marzano A, Lampertico P, Andreone P, Santantonio T, Almasio PL, et al. Clinical outcome of HBeAg-negative chronic hepatitis B in relation to virological response to lamivudine. Hepatology. 2004;40:883–91.
Marcellin P, Chang TT, Lim SG, Tong MJ, Sievert W, Shiffman ML, et al. Adefovir dipivoxil for the treatment of hepatitis B e antigen-positive chronic hepatitis B. N Engl J Med. 2003;348:808–16.
Kurashige N, Hiramatsu N, Ohkawa K, Yakushijin T, Kiso S, Kanto T, et al. Factors contributing to antiviral effect of adefovir dipivoxil therapy added to ongoing lamivudine treatment in patients with lamivudine-resistant chronic hepatitis B. J Gastroenterol. 2009;44(6):601–7.
Chen CJ, Yu MW, Liaw YF. Epidemiological characteristics and risk factors of hepatocellular carcinoma. J Gastroenterol Hepatol. 1997;12:5294–308.
Yun LF. Natural history of chronic hepatitis B virus infection and long-term outcome under treatment. Liver Int. 2009;29:100–7.
Sung JJ, Tsoi KK, Wong VW, Li KC, Chan LL. Meta-analysis: treatment of hepatitis B infection reduces risk of hepatocellular carcinoma. Aliment Pharmacol Ther. 2008;28:1067–77.
Acknowledgments
This work was supported by Grants-in-Aid for Research on Hepatitis and BSE from the Ministry of Health Labour and Welfare of Japan and for Scientific Research from the Ministry of Education, Science, and Culture of Japan.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kurokawa, M., Hiramatsu, N., Oze, T. et al. Long-term effect of lamivudine treatment on the incidence of hepatocellular carcinoma in patients with hepatitis B virus infection. J Gastroenterol 47, 577–585 (2012). https://doi.org/10.1007/s00535-011-0522-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0522-7