Abstract
Background
Two genome-wide association studies on gastric cancer showed a previously unknown gastric cancer susceptible locus in PLCE1 at 10q23. We hypothesized that the single nucleotide polymorphism (SNP) rs2274223 A/G is associated with the survival rate of gastric cancer.
Methods
We genotyped the above SNP in 940 gastric cancer patients to investigate the association between the polymorphism and gastric cancer survival by the TaqMan method.
Results
We found that patients carrying PLCE1 rs2274223 AA genotype survived for a significantly shorter time than those carrying the AG and GG genotypes (log-rank P = 0.046). This significance was enhanced in the dominant model (AA vs. AG/GG, log-rank P = 0.014). Multivariate Cox regression analyses showed that the AG/GG genotypes were associated with a significantly decreased risk of death from gastric cancer [adjusted hazard ratio (HR) = 0.79, 95% confidence interval (CI) = 0.65–0.95]. Most of stratification analysis did not find an enhanced association between the same genotype and prognosis, except for patients with TNM stage III disease (HR = 0.63, 95% CI = 0.48–0.83).
Conclusion
Our findings showed that the PLCE1 SNP rs2274223 was associated with significantly improved gastric cancer survival in a Chinese population. Further functional studies are needed to validate our results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As a common malignant tumor of the digestive system, gastric cancer remains the second leading cause of cancer-related mortality all over the world [1]. Nearly 40% of gastric cancer cases occur in China, which has been a high-incidence area in past decades. The 5-year overall survival rate of gastric cancer is approximately less than 50% in China [2]. Gastric cancer is induced by a series of factors such as the diet, smoking, and Helicobacter pylori infection [3, 4], although the precise mechanisms regulating the development of gastric cancer are still undetermined. Actually, finding suitable biomarkers for prognosis in gastric cancer may help to increase survival rates after surgical operations.
Single nucleotide polymorphisms (SNPs), which are common variations in the human genome, could be suitable molecular markers for locating and identifying genes related to specific diseases. Previous studies have indicated various SNPs involved in the invasion, development, and prognosis of gastric cancer [5–10]. A two-stage genome-wide association study (GWAS) based on a Japanese population found that the PSCA gene was associated with susceptibility to diffuse-type gastric cancer [11]. Two GWASs, recently conducted by Abnet et al. and Wang et al. confirmed that a notable SNP located in PLCE1 rs2274223 was associated with gastric cancer [12, 13]. These results might provide new insight into the incidence of gastric cardia cancers, although the role of this SNP in the prognosis of gastric cancer is still unknown.
The PLCE1 at chromosome 10q23, encoding phospholipase C epsilon 1 (PLCε1), is a unique member of the phospholipase family. Secondary messengers, including inositol-1,4,5-trisphosphate and diacylglycerol, are formed after the hydrolysis of polyphosphoinositides catalyzed by PLCε1 [14]. Subsequently they take part in the process of cell growth and differentiation [14]. PLCε−/− mice resist the activation of 12-O-tetradecanoylphorbol-13-acetate (TPA) in skin squamous tumors induced by 7,12-dimethylbenzanthracene [15]. Of note, variations in the human PLCE1 gene, related to nephrotic syndrome, may be a potential factor for carcinogenesis [16].
In the present study, we have hypothesized that the PLCE1 rs2274223 polymorphism is associated with the survival of gastric cancer patients in a Chinese population.
Patients, materials, and methods
Study population
The study patients were recruited from Yixin People’s Hospital, Yixin City, China, between January 1999 and December 2006. The detailed population information has been described in our previous study [17]. Briefly, we collected data on 1,022 patients who had their surgical resection at Yixin People’s Hospital; 78 patients (7.6%) were excluded because of the lack of adequate follow-up information and 4 patients (0.4%) were excluded because they did not have adenocarcinoma. Finally, 940 patients were entered into the survival analysis. The maximum follow-up time for all patients was 119.0 months (last follow-up in March 2009) and the median follow-up time was 35.0 months.
From the patients’ medical records, we gathered data on clinicopathological variables such as tumor site, invasion depth, and distant metastasis. The histopathology of tumors was grouped as diffuse or intestinal type according to Lauren’s criteria [18]. The tumor-node-metastasis (TNM) stages were evaluated according to the TNM classification of the American Joint Committee on Cancer (AJCC cancer staging manual, 6th edition) [19]. The whole study design was approved by the Institutional Review Board of Nanjing Medical University.
Genotyping
Genomic DNA was obtained from paraffin sections of patients’ tissues. The ABI 7900HT real-time PCR System (Applied Biosystems, Foster City, CA, USA) was used for the TaqMan SNP genotyping assay. Genotype analysis was carried out by two persons independently in a blind fashion. About 10% of the samples were selected randomly for repeated genotyping for confirmation, and the results were 100% concordant. Genotyping failed in two cases because of DNA quality. Finally, 938 gastric cancer cases were included in the analysis.
Statistical analysis
Survival time was calculated from the date of gastric cancer diagnosis to the date of death or last follow-up. The associations between survival time and demographic characteristics, clinical features, and PLCE1 rs2274223 polymorphism were estimated using the Kaplan–Meier method and log-rank test. Mean survival time was provided when the median survival time (MST) could not be calculated. Univariate or multivariate Cox regression analysis was fitted to estimate the crude hazard ratios (HRs), adjusted HRs, and 95% confidence intervals (CIs). Cox stepwise regression analysis was also performed to determine predictive factors of gastric cancer prognosis, with P < 0.05 for entering and P > 0.10 for removing the respective explanatory variables. The Hardy–Weinberg equilibrium (HWE) of the case genotype distribution was tested by a goodness-of-fit χ 2 test. All the statistical analyses were performed with SAS software (version 9.1.3; SAS Institute, Cary, NC, USA) with two-sided P values, unless indicated otherwise.
Results
Patients’ characteristics and clinical features
Patients’ characteristics and clinical data are summarized in Table 1. The median age was 62 years (range, 28 to 83 years) for the 938 patients retained in the study. There were 722 males (77.0%) and 216 females (23.0%) in the patient panel, and all of them were gastric adenocarcinoma cases. In a period of 119.0 months of follow-up, 437 patients died of gastric cancer. Tumor size, histological type, depth of invasion, lymph node metastasis, distant metastasis, and TNM stage were significantly associated with survival time (all log-rank P < 0.01). Univariate Cox regression analysis showed that the risk of death from gastric cancer was significantly increased as the depth of invasion and TNM stage increased and lymph node metastasis and distant metastasis expanded (log-rank P < 0.001 for depth of invasion, lymph node metastasis, and TNM stage; log-rank P = 0.003 for distant metastasis). Patients with tumor size of >5 cm (MST 49.2 months) had a 43% significantly increased risk of death (HR = 1.43, 95% CI = 1.18–1.73), compared with those with tumor size of ≤5 cm (MST 99.9 months). Patients with diffuse-type gastric cancer (MST 51.1 months) had a significantly higher risk of death (HR = 1.46, 95% CI = 1.20–1.77), compared with those with intestinal-type (MST 57.2 months). The genotype frequencies of PLCE1 rs2274223 in the cases were in agreement with the HWE (P = 0.716).
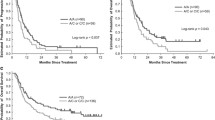
Association of PLCE1 rs2274223 and gastric cancer survival
Kaplan–Meier survival curves and the log-rank test were used to assess the associations of PLCE1 genotypes and gastric cancer patients’ survival in different genetic models (Table 2). In the overall model, the PLCE1 rs2274223 polymorphism was associated with the survival of gastric cancer (log-rank P = 0.046, Fig. 1a). Survival in patients with the AG genotype (MST 96.4 months) was significantly different compared with that of patients with the AA genotype (MST 52.9 months), who had a 22% higher risk of death (HR = 0.78, 95% CI = 0.64–0.95). In the dominant model, a significantly lower risk of death (HR = 0.79, 95% CI = 0.65–0.95) was found (log-rank P = 0.014), as shown in Fig. 1b.
Stratified analyses and stepwise Cox regression model for survival in gastric cancer patients
Among all of the independent variables, some may potentially contribute to overall gastric cancer survival. According to these possible confounders we analyzed the association of the rs2274223 polymorphism and survival of gastric cancer patients. As shown in Table 3, patients carrying AG/GG genotypes had a 21% higher survival rate than those with the AA genotype. The protective effect was statistically significant in subgroups of patients with tumor size >5 cm (HR = 0.75, 95% CI = 0.56–0.99), diffuse-type gastric cancer (HR = 0.77, 95% CI = 0.61–0.98), T3 depth invasion (HR = 0.68, 95% CI = 0.53–0.86), lymph node metastasis (HR = 0.74, 95% CI = 0.59–0.93), no distant metastasis (HR = 0.81, 95% CI = 0.66–0.99), TNM stage III (HR = 0.63, 95% CI = 0.48–0.83), and chemotherapy (HR = 0.78, 95% CI = 0.62–0.98). A stepwise Cox regression model was used to evaluate the correlation between variables including selected demographic characteristics, clinical features, the PLCE1 rs2274223 polymorphism, and gastric cancer survival. Consequently, four variables (lymph node metastasis, distant metastasis, TNM stage, and rs2274223) were included in the regression model with a significance level of <0.05 for entering a variable and >0.10 for removing it (P = 0.010 for lymph node metastasis, P = 0.003 for distant metastasis, P = 0.020 for TNM stage III, and P = 0.011 for rs2274223; Table 4).
Discussion
In the present study, we investigated the effect of the PLCE1 rs2274223 SNP on general gastric cancer survival. Our results indicated that the heterozygote genotype was associated with a significantly higher survival rate of gastric cancer, and the association was also observed when analyzing the dominant model, suggesting that the PLCE1 rs2274223 G allele may be associated with survival of gastric cancer.
PLCε1 is a multiple-function protein with a complex structure [14]. It interacts with small G-protein, recognizing and conducting an interaction with G-protein, catalyzing nucleotide changing of Ras family protein GTP (guanosine triphosphate); PLCε1 also possesses CDC25 and shows series connection of the RA (RalGDS/AF-6) structural domain. Promoting PLC and RasGEF, PLCε1 induces Ca2+ migration and the activation of protein kinase C (PKC), and serves as a guanine nucleotide conversion factor of the Ras superfamily [20–23]. Promoted PLCε1 also catalyzes polyphosphoinositides, hydrolyzing them to inositol-1,4,5-triphosphate (IP3) and diacylglycerol (DAG ) [14].
To date, only two independent GWASs have discovered that a novel locus at PLCE1 was associated with susceptibility to gastric cancer, although there have been no related studies on prognosis, to our knowledge. Previous research on PLCE1 has mainly focused on its impact in diseases of the urinary system, including nephrotic syndrome (NS), focal and segmental glomerulosclerosis (FSGS), and diffuse mesangial sclerosis (DMS) [24–27]. Results of experiments with PLCε−/− mice suggested a crucial role of PLCε in ras oncogene-induced de-novo carcinogenesis, introducing PLCε as a possible molecular target for the development of anticancer drugs [14]. Our results in the present study indicate that the survival of gastric cancer patients differs between populations with different genotypes of PLCE1, suggesting a probable role of PLCE1 in the treatment of cancers.
Tumor size, depth of invasion, lymph node metastasis, distant metastasis, and TNM stage were potential factors related to the survival of gastric cancer patients according to our findings on clinical features. These findings may be considered as indicating the normal cancer process especially in patients mainly with advanced gastric cancer and a late diagnosis. Based on our observations in the present study, cancer sites (cardia gastric cancer and non-cardia gastric cancer) were not associated with patients’ survival. Diffuse-type gastric cancer which is reportedly increasing in prevalence worldwide [28], is also a risk factor for reduced survival compared to the intestinal type, by our observation. In the present study, on analyzing the overall survival of gastric cancer patients, we found that individuals carrying PLCE1 rs2274223 AG/GG genotypes had a higher survival rate than those carrying the AA genotype, which suggested to us that the rs2274223 G allele may be associated with prognosis in gastric cancer patients. The recent GWAS showed that the PLCE1 rs2274223 G allele was associated with risk of gastric cancer. A case–control study, based on a population from the same region as ours (i.e., Jiangsu province), which is a high-risk area of gastric cancer, reproducibly indicated that this SNP rs2274223 was associated with gastric cancer susceptibility in a Chinese population [29]; thus, Jiangsu province, as a high-risk area of gastric cancer, may be considered as a good study region. In contrast to the above study [29], we found that the PLCE1 rs2274223 G allele conferred a favorable survival for gastric cancer. Few functional studies have focused on the association between this SNP and gastric cancer before. Wang et al. [13] showed that more cells in esophageal squamous cell carcinoma and gastric cardia adenocarcinoma tissues contained PLCE1 than cells in normal tissues. Considering that the mechanisms underlying gastric cancer susceptibility are complicated and still largely unknown, it is difficult to assess the effect of this SNP on gastric cancer prognosis. The discrepancy between our study and the above case-control study [29] might be attributable to the biological variations between susceptibility and prognosis in gastric cancer patients. Further functional studies are warranted, and our findings on this polymorphism might also predict the survival of gastric cancer.
As we know, the survival rate of gastric cancer patients remains low. Individual therapy is needed to improve the prognosis of these patients. A useful marker for prevention and for monitoring of treatment is not yet available. Such a marker might open a brand new avenue of research at the molecular level. Our previous study recommended the PSCA gene, which was established in another GWAS [11], as a candidate biomarker for diffuse gastric cancer [17]. The present results also indicated a new potential marker. Our figures on cumulative survival indicated different outcomes between our overall model and the dominant model.
Some limitations of the present study should be mentioned. First, PLCE1 rs2274223 was the only polymorphism examined. SNPs at other loci which may be linked with rs2274223 were neglected. Second, Helicobacter pylori, as a known crucial factor in gastric carcinogenesis, was not considered due to the lack of related follow-up information. Third, we rechecked the database and medical records, and found that the treatment of most patients was a surgical operation. The proportion of patients who received chemotherapy was relatively low, at 32.5%, and all the chemotherapy treatments were administered after surgery. A significantly lower risk of death was observed in patients with chemotherapy after surgery, although the association was marginal. A larger number of patients will be needed to assess the association between the SNP rs2274223 at PLCE1 and gastric cancer survival in future studies. Finally, functional assays are required for further studies.
In conclusion, we found a notable SNP rs2274223 at PLCE1 that may be associated with the prognosis of gastric cancer patients. The survival of patients in the dominant model was significantly better than the survival in the overall model, suggesting that the mutant allele may serve as a suitable marker for the survival of gastric cancer patients, especially in a Chinese population. Further functional evaluations of this polymorphism are warranted to validate our findings.
References
Parkin DM. International variation. Oncogene. 2004;23:6329–40.
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
Crew KD, Neugut AI. Epidemiology of upper gastrointestinal malignancies. Semin Oncol. 2004;31:450–64.
Uemura N, Okamoto S, Yamamoto S, Matsumura N, Yamaguchi S, Yamakido M, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med. 2011;345:784–9.
Chen SQ, Lin XD, Zhu JW, Tang Y, Lin JY. Association of a MYCL1 single nucleotide polymorphism, rs3134613, with susceptibility to diffuse-type gastric cancer and with differentiation of gastric cancer in a southeast Chinese population. DNA Cell Biol. 2010;29:739–43.
Guan X, Zhao H, Niu J, Tan D, Ajani JA, Wei Q, et al. Polymorphisms of TGFB1 and VEGF genes and survival of patients with gastric cancer. J Exp Clin Cancer Res. 2009;28:94.
Hishida A, Matsuo K, Goto Y, Naito M, Wakai K, Tajima K, et al. Combined effect of miR-146a rs2910164 G/C polymorphism and toll-like receptor 4 +3725 G/C polymorphism on the risk of severe gastric atrophy in Japanese. Dig Dis Sci. 2011;56(4):1131–7.
Nguyen TV, Janssen MJ, van Oijen MG, Bergevoet SM, te Morsche RH, van Asten H, et al. Genetic polymorphisms in GSTA1, GSTP1, GSTT1, and GSTM1 and gastric cancer risk in a Vietnamese population. Oncol Res. 2010;18:349–55.
Sun LM, Shang Y, Zeng YM, Deng YY, Cheng JF. HOGG1 polymorphism in atrophic gastritis and gastric cancer after Helicobacter pylori eradication. World J Gastroenterol. 2010;16:4476–82.
Sun Q, Gu H, Zeng Y, Xia Y, Wang Y, Jing Y, et al. Hsa-mir-27a genetic variant contributes to gastric cancer susceptibility through affecting miR-27a and target gene expression. Cancer Sci. 2010;101:2241–7.
Sakamoto H, Yoshimura K, Saeki N, Katai H, Shimoda T, Matsuno Y, et al. Genetic variation in PSCA is associated with susceptibility to diffuse-type gastric cancer. Nat Genet. 2008;40:730–40.
Abnet CC, Freedman ND, Hu N, Wang Z, Yu K, Shu XO, et al. A shared susceptibility locus in PLCE1 at 10q23 for gastric adenocarcinoma and esophageal squamous cell carcinoma. Nat Genet. 2010;42:764–7.
Wang LD, Zhou FY, Li XM, Sun LD, Song X, Jing Y, et al. Genome-wide association study of esophageal squamous cell carcinoma in Chinese subjects identifies susceptibility loci at PLCE1 and C20orf54. Nat Genet. 2010;42:759–63.
Wing MR, Bourdon DM, Harden TK. PLC-epsilon: a shared effector protein in Ras-, Rho-, and G alpha beta gamma-mediated signaling. Mol Interv. 2003;3:273–80.
Bai Y, Edamatsu H, Maeda S, Saito H, Suzuki N, Satoh T, et al. Crucial role of phospholipase C epsilon in chemical carcinogen-induced skin tumor development. Cancer Res. 2004;64:8808–10.
Hinkes B, Wiggins RC, Gbadegesin R, Vlangos CN, Seelow D, Nürnberg G, et al. Positional cloning uncovers mutations in PLCE1 responsible for a nephrotic syndrome variant that may be reversible. Nat Genet. 2006;38:1397–405.
Wang M, Bai J, Tan Y, Wang S, Tian Y, Gong W, et al. Genetic variant in PSCA predicts survival of diffuse-type gastric cancer in a Chinese population. Int J Cancer. 2011;129(5):1207–13.
Lauren P. The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand. 1965;64:31–49.
Green FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC cancer staging manual. 6th ed. New York: Springer Press; 2002. p. 111–118.
Ada-Nguema AS, Xenias H, Hofman JM, Wiggins CH, Sheetz MP, Keely PJ. The small GTPase R-Ras regulates organization of actin and drives membrane protrusions through the activity of PLC epsilon. J Cell Sci. 2006;119:1307–19.
Evellin S, Nolte J, Tysack K, vom Dorp F, Thiel M, Weernink PA, et al. Stimulation of phospholipase C-epsilon by the M3 muscarinic acetylcholine receptor mediated by cyclic AMP and the GTPase Rap2B. J Biol Chem. 2002;277:16805–13.
Kelley GG, Kaproth-Joslin KA, Reks SE, Smrcka AV, Wojcikiewicz RJ. G-protein-coupled receptor agonists activate endogenous phospholipase C epsilon and phospholipase Cbeta3 in a temporally distinct manner. J Biol Chem. 2006;281:2639–48.
Wang H, Oestreich EA, Maekawa N, Bullard TA, Vikstrom KL, Dirksen RT, et al. Phospholipase C epsilon modulates beta-adrenergic receptor-dependent cardiac contraction and inhibits cardiac hypertrophy. Circ Res. 2005;97:1305–13.
Boyer O, Benoit G, Gribouval O, Nevo F, Pawtowski A, Bilge I, et al. Mutational analysis of the PLCE1 gene in steroid resistant nephrotic syndrome. J Med Genet. 2010;47:445–52.
Gbadegesin R, Bartkowiak B, Lavin PJ, Mukerji N, Wu G, Bowling B, et al. Exclusion of homozygous PLCE1 (NPHS3) mutations in 69 families with idiopathic and hereditary FSGS. Pediatr Nephrol. 2009;24:281–5.
Gilbert RD, Turner CL, Gibson J, Bass PS, Haq MR, Cross E, et al. Mutations in phospholipase C epsilon 1 are not sufficient to cause diffuse mesangial sclerosis. Kidney Int. 2009;75:415–9.
Machuca E, Benoit G, Nevo F, Tete MJ, Gribouval O, Pawtowski A, et al. Genotype-phenotype correlations in non-Finnish congenital nephrotic syndrome. J Am Soc Nephrol. 2010;21:1209–17.
Crew KD, Neugut AI. Epidemiology of gastric cancer. World J Gastroenterol. 2006;12:354–62.
Zhang H, Jin G, Li H, Ren C, Ding Y, Zhang Q, et al. Genetic variants at 1q22 and 10q23 reproducibly associated with gastric cancer susceptibility in a Chinese population. Carcinogenesis. 2011;32(6):848–52.
Acknowledgments
This study was partly supported by the National Natural Science Foundation of China (30872084 and 30972444), the National Natural Science Foundation of Jiangsu Province (2010080), the Key Program for Basic Research of Jiangsu Provincial Department of Education (08KJA330001), the Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD), and the Postdoctoral Science Foundation of China (20100481164).
Conflict of interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
D. Luo and Y. Gao contributed equally to this work.
Rights and permissions
About this article
Cite this article
Luo, D., Gao, Y., Wang, S. et al. Genetic variation in PLCE1 is associated with gastric cancer survival in a Chinese population. J Gastroenterol 46, 1260–1266 (2011). https://doi.org/10.1007/s00535-011-0445-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0445-3