Abstract
Background
Endoscopic transpapillary brush cytology and forceps biopsy are widely used for the pathological diagnosis of suspected malignant biliary strictures (MBS). However, the sensitivity of these methods remains insufficient, and it can be difficult to confirm the diagnosis. We aimed to evaluate the diagnostic ability of endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) and the impact of this technique on clinical management in patients with suspected MBS where endoscopic brush cytology and biopsy yielded negative results.
Methods
This study included 225 consecutive patients with suspected MBS, who underwent endoscopic brush cytology and biopsy at our institutions. Negative results were obtained for these pathological tests in 75 patients, and EUS-FNA was performed in 22 of these patients. We retrospectively compared the EUS-FNA results with the final diagnosis and examined the influence of the EUS-FNA diagnosis on treatment selection.
Results
FNA specimens were successfully obtained in all patients, and the pathological results confirmed malignancy in 16 cases and predicted that the other 6 cases were benign. Of the 6 cases that were suspected to be benign, 3 patients were diagnosed with xanthogranulomatous cholecystitis by surgical pathology, and the remaining 3 patients were diagnosed with benign diseases at a follow-up after 12–18 months. Thus, the EUS-FNA-based diagnosis was proven correct for all the patients. In addition, the treatment strategy was altered as a result of the EUS-FNA results in the above 6 patients (27%).
Conclusions
EUS-FNA is a sensitive and safe diagnostic modality for patients with suspected MBS and can be an additional option in cases where endoscopic brush cytology and biopsy have produced negative results.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It is difficult to reliably differentiate between benign and malignant biliary strictures (MBS). Endoscopic transpapillary cytology and/or biopsy are currently used in patients with suspected MBS, but their sensitivity is insufficient, at 30–81% [1]. In difficult cases, alternative sampling techniques are required to provide a definitive diagnosis that will aid in choosing a treatment strategy. In recent years, endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) has become increasingly popular for obtaining samples from a variety of organ sites. Several reports have already evaluated the efficacy of the procedure for biliary lesions [2–10]. However, only a few reports have evaluated the diagnostic ability of this technique in patients after negative endoscopic retrograde cholangiopancreatography (ERCP) cytology results [4, 7]. In addition, these studies included only proximal biliary strictures.
In this study, we evaluated the EUS-FNA yield and its impact on treatment selection in patients with suspected malignant extrahepatic biliary stricture following negative ERCP cytology and biopsy results.
Methods
Patients
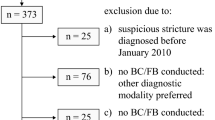
Patient records were retrospectively collected for a cohort of 225 patients with suspected MBS who underwent endoscopic transpapillary cytology and biopsy at the First Department of Internal Medicine, Gifu University Hospital, and the Department of Gastroenterology, Hokkaido University Hospital, between December 2007 and December 2009. In this cohort, 150 patients showed positive cytology or biopsy, whereas 75 were negative (Fig. 1). The latter group received additional evaluation with other imaging techniques, such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET), as well as a more in-depth blood biochemistry analysis, including tests for tumor markers and IgG4.
As a result, obvious masses were detected in 39 patients, and irregular thickening of the bile duct wall was observed in 16 patients on CT and/or MRI. In addition, the mass had invaded other organs and/or major vessels in 21 patients. Furthermore, CT and PET-CT findings indicated possible metastasis and peritoneal dissemination in 6 and 4 patients, respectively. Increased serum levels of carcinoembryonic antigen (CEA) were observed in 32 patients. Ultimately, we diagnosed malignancy in 44 patients, from combinations of these findings and the cholangiograms.
Because diffuse swelling of the whole pancreas and diffuse narrowing of the main pancreatic duct were observed in 4 patients on the previous imaging tests, the serum IgG4 level was measured. The serum IgG4 level was elevated in all 4 of these patients, and they were diagnosed as having IgG4-related sclerosing cholangitis. Subsequent steroid therapy attenuated the biliary stricture in all 4 patients. In 5 other patients, the cholangiograms showed a relatively smooth stricture. No obvious mass and no irregular thickening of the bile duct wall was seen on any of the imaging tests. Serum CEA level was also not increased. Therefore, we considered these cases likely to be benign.
In the remaining 22 patients, the serum CEA levels were not elevated. No obvious masses were seen on the CT or MRI images, except in 8 cases that were suspected to be xanthogranulomatous cholecystitis (XGC). Each of these 8 patients showed a mass in the gallbladder, and in 3 patients, the mass had also invaded the liver and surrounding large vessels. However, the lumen of the gallbladder was relatively well preserved for the tumor size, and deposition of fat in the mass and the presence of dilated Rokitansky-Aschoff sinuses were suspected from the MRI findings. We could not reach a conclusion and conducted EUS-FNA in these 22 patients (Fig. 1). Patient treatments are described at the bottom of Fig. 1. In the cases diagnosed as likely benign, the patients were followed up after 12–18 months at the December 2010 data update and were doing well.
Demographic and clinical characteristics of the 22 patients in whom EUS-FNA was performed are given in Table 1.
EUS-FNA procedures
After informed consent had been obtained, EUS-FNA was performed with an oblique-forward-viewing electronic linear scanning video echoendoscope (GF-UC240P-AL5; Olympus Optical, Tokyo, Japan) connected to a processor with a color Doppler function (SSD-5000; Aloka, Tokyo, Japan). Following EUS evaluation of the lesion, puncture was performed via the gastric or duodenal wall with a 25-, 22-, or 19-gauge needle (EchoTip; Wilson-Cook, Winston-Salem, NC, USA) guided by real-time EUS imaging. The needle was moved back and forth in the lesion about 10 times for a 25- or 22-gauge needle and about 5 times for a 19-gauge needle. The aspirated material was treated as we have previously described [11–15].
Because neither a pathologist nor a cytologist was present on-site at our institutions, the puncture procedure was repeated until whitish material became visible macroscopically. Cytological and histological diagnoses were made on the basis of Papanicolaou and hematoxylin–eosin staining, respectively (Figs. 2, 3). Immunohistochemical stains were also performed on request. The procedure was performed on an outpatient basis unless the patient was already hospitalized for other medical conditions. The outpatients were observed for immediate complications in the recovery room for 2 h, and contact was maintained for 24 h after the procedure to monitor any complications.
A case of obstructive jaundice due to bile duct tumor. a Endoscopic ultrasound (EUS) image shows an undemarcated hypoechoic tumor in the middle bile duct invading the portal vein. EUS-FNA was performed on the tumor. The image on the left is a fundamental image, and the one on the right is an image obtained by using the color Doppler function. b The cytological diagnosis was adenocarcinoma (Papanicolaou stain, ×400). PV portal vein, IVC inferior vena cava
A case of obstructive jaundice due to gallbladder tumor. a An EUS image shows an undemarcated hypoechoic tumor (arrowheads) in the neck of the gallbladder invading and obstructing the common bile duct. b The histological diagnosis was granuloma, and giant cells (arrow) were also seen (H&E stain, ×100). Xanthogranulomatous cholecystitis was highly suspected, and simple cholecystectomy was performed in this patient. The final diagnosis of xanthogranulomatous cholecystitis was confirmed by the pathological result of the surgical specimen. GB gallbladder, CBD common bile duct, IVC inferior vena cava
Final diagnoses of benign disease were made for the following conditions: (1) if surgical pathology proved a benign disease; (2) if autoimmune pancreatitis was suspected from pancreatography and an increased level of IgG4, and the biliary stricture was attenuated by subsequent steroid therapy; or (3) if spontaneous resolution or lack of progression was noted on follow-up imaging studies for at least 12 months without any deterioration of the patient’s general health.
Results
FNA results
EUS-FNA of the bile duct was attempted 22 times in 22 patients. The patients’ ages, male-to-female ratio, length of the bile duct stricture, punctured organ, and puncture route are given in Table 1. Nineteen patients had biliary drainage placed during the initial ERCP due to obstructive jaundice. EUS visualized a mass at the stricture site in 19 patients; the median diameter of the masses at their largest points was 29 mm (range 7–61 mm). In the 3 other patients, only wall thickening of the bile duct was observed, and the thickened wall was punctured. Puncture approach to the lesions was successful in all cases, and pathological samples were successfully obtained in all cases. When the successful procedure was defined as successful puncture and successful collection of sufficient material for pathological diagnosis, the success rate was 100%. The pathological examination showed benign results in 6 cases and malignant results in 16 cases. Of the malignant cases, 13 were adenocarcinoma, 2 were squamous cell carcinoma, and 1 was undifferentiated carcinoma. Of the 6 benign cases, 2 were granulomas (Fig. 3), and 4 revealed no atypical cells (Table 2).
Intervention following EUS-FNA
Of the 16 patients with malignancies, 4 underwent surgical resection, and 10 received chemotherapy. In the remaining 2 patients, we chose to use best supportive care. Of the 6 patients with benign results, 3 underwent surgical management and were diagnosed with XGC (Fig. 3). One patient received endoscopic treatment, resulting in a diagnosis of Mirizzi syndrome. We followed up on the 2 other patients with benign bile duct stricture. These 2 patients had had bile duct stones, and the biliary stricture was found after the removal of the stones. Thus, the stricture might have been caused by the endoscopic procedures of stone removal. They were not given biliary stents and were followed up at 12 and 18 months, without any adverse events (Fig. 4). Final diagnoses are given in Table 3 and at the bottom of Fig. 4.
Impact of EUS-FNA on clinical management
In all 22 patients with EUS-FNA, malignancy had been suspected. However, in 6 of these patients the condition was shown not to be malignant by EUS-FNA. Of these patients, 2 patients with gallbladder tumors had been scheduled to undergo hepatopancreatoduodenectomy, but because of the EUS-FNA results, they instead underwent simple cholecystectomy. Another patient with a gallbladder tumor had already started chemotherapy for the diagnosis of advanced gallbladder cancer, but this treatment was canceled immediately due to the benign result on EUS-FNA, and the patient underwent simple cholecystectomy. These 3 patients were followed up conservatively according to the pathological results of XGC after cholecystectomy.
A case of Mirizzi syndrome was initially thought to be gallbladder cancer and the patient was scheduled to start chemotherapy but received endoscopic treatment alone after the EUS-FNA. Two other patients also avoided cancer therapy after benign results were shown on EUS-FNA, and they are being followed up (Fig. 4). In total, EUS-FNA resulted in a major change of treatment management in 6 of the 22 patients (27%).
Diagnostic ability and safety of EUS-FNA
Comparisons were made between the EUS-FNA diagnosis and the final clinical diagnosis derived from surgical pathology or follow-up data. Of the 22 cases, 16 were correctly diagnosed as malignant by FNA, and 6 were correctly diagnosed as negative for malignancy. Thus, there were no false-positives. Estimated sensitivity and specificity were both 100%. No significant complications—such as massive bleeding, bile peritonitis, shock, or infection—were noted in any patients.
Discussion
Over the past decade, several attempts have been made to examine the pathology of bile duct stricture through an endoscopic approach [16–25]. Such a diagnosis is highly desirable to allow adequate subsequent planning of surgical or nonsurgical treatment [21, 22].
Biliary brush cytology has been a mainstay diagnostic method for suspected extrahepatic biliary tree malignancies because it is technically easy, requires little time, and is generally safe. However, the sensitivity for cancer is modest, ranging from 30 to 57% in most published studies [1, 22, 23, 25]. It has been suggested that this limited sensitivity is mainly a result of inadequate cellular yield [1].
Transpapillary bile duct forceps biopsy is another diagnostic method. Although this technique is more time-consuming and technically difficult, it provides a sample of bile duct tissue deep into the epithelium, theoretically obviating the problem of inadequate sampling that may occur with brush cytology. Indeed, some investigators have reported better sensitivity with this technique and concluded that forceps biopsy is the single best diagnostic method for the evaluation of biliary stricture at ERCP [1, 23, 25]. However, the sensitivity is still insufficient, ranging from 43 to 81% [1, 16, 22–25]. Such low sensitivity may be attributed to tumor-associated fibrosis or ulceration, well-differentiated cancers, submucosal spread, or external compression of the bile duct by the tumor [9]. Furthermore, it may result from the difficulty of reliable lesion sampling; the tissue sampling is performed under fluoroscopic guidance, and the biopsy procedure is performed somewhat blindly. In addition, it is difficult to open the biopsy forceps at the stricture site, and the sampling is often attempted at inappropriate sites below the stricture.
A combination of brush cytology and forceps biopsy probably enhances cancer detection. Several studies have shown that the combination increased the sensitivity to about 55–74% [1, 23, 25–27]. Multiple cytology brushings and biopsies also increase the sensitivity of cancer detection. Therefore, it is generally recommended that 2 consecutive brushings and at least 3 biopsy specimens be taken from the stricture [1]. In the present study, a median of 2 brushings (range 1–3) and 3 biopsy specimens (range 2–7) were obtained from the strictures, and the sensitivity of cancer detection was relatively high (79%). However, false-negative diagnoses were made in 16 (21%) of the 75 cases that tested negative by biliary brush cytology and forceps biopsy. Therefore, an alternative sampling technique is required when these transpapillary sampling techniques do not provide a definitive diagnosis.
Two studies have attempted to use EUS-FNA on biliary strictures following negative ERCP brush cytology results. In their prospective study, Fritscher-Ravens et al. [4] initially evaluated the suitability of EUS-FNA for the preoperative diagnosis of hilar cholangiocarcinoma with negative transpapillary brush cytology results. Adequate material was obtained in 43 of 44 patients by EUS-FNA, and the cytology results revealed hilar cholangiocarcinoma in 26 patients, other malignancies in 5 patients, and benign results in 12 patients. Because 4 of the benign results were false-negatives, the final accuracy, sensitivity, and specificity were 91, 89, and 100%, respectively. Their study showed that EUS-FNA was technically feasible and without significant risks and could change preplanned management in about half of the patients. Later, DeWitt et al. [7] also reported their experience with EUS-FNA of proximal biliary stricture after negative ERCP brush cytology results. Their retrospective cohort study included 24 patients, and the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of EUS-FNA were 77, 100, 100, 29, and 79%, respectively.
In the above-mentioned studies, EUS-FNA was attempted only in patients with hepatic hilar stricture. In contrast, Eloubeidi et al. [9] attempted EUS-FNA in 28 patients; the tumor or stricture was located in the proximal bile duct in 60% of the patients and in the distal bile duct in 40% of the patients. The researchers evaluated the EUS-FNA yield and its impact on patient management for patients with suspected cholangiocarcinoma. Of these patients, 88% had nondiagnostic bile duct brushing at ERCP. In addition, no definitive mass was seen on CT or MRI scans for 14 of the 21 patients (67%) with proven cholangiocarcinoma. The sensitivity, specificity, PPV, NPV, and accuracy of EUS-FNA were 86, 100, 100, 57, and 88%, respectively. Eloubeidi et al. [9] concluded that EUS-FNA had a positive impact on patient management in 84% of cases.
Our study also included both distal and proximal biliary strictures where endoscopic transpapillary brush cytology and forceps biopsy had failed, and EUS-FNA provided confirmatory diagnoses in all 22 patients, which indicated that the sensitivity, specificity, PPV, NPV, and accuracy were all 100%. We cannot explain such extremely high diagnostic results. The median number of passes in the present study was 2 (range 1–3), which was similar to that in the previous reports (median 2–4) [4, 7, 9]. However, our results might be related to our policy on needle selection. When puncture was possible, we generally used a 19-gauge needle for patients requiring histological assessment, because this enabled us to obtain a significantly larger amount of tissue [11–14]. Theoretically, histological assessment on sufficient material can lead to a more correct diagnosis than cytology or histological assessment on insufficient material. Indeed, in the present study, 2 cases were highly suspected to have XGC on the basis of histopathological findings because they were diagnosed with granuloma, and aggregates of foamy macrophages (giant cells) were also seen on the histopathological samples obtained by 19-gauge needles (Fig. 3).
Compared with transpapillary brush cytology and forceps biopsy, EUS-FNA has several advantages in the evaluation of biliary strictures. EUS-FNA can allow tissue sampling directly from a tumor under real-time EUS imaging guidance. This enabled us to obtain pathological samples at more appropriate lesion sites. Moreover, EUS, because of the fine image quality, often visualized a mass in patients with previously negative findings on imaging studies [7].
Interestingly, EUS-FNA enabled the diagnosis of bile duct cancer even in patients without mass formation. In the present study, 3 patients without a mass at the stricture site were correctly diagnosed—with bile duct cancer in 1 case and benign biliary stricture in the other 2. In addition, EUS can evaluate extraluminal lesions—such those occurring in the pancreas, gallbladder, and lymph nodes—which can cause biliary strictures. Moreover, the identification of regional lymphadenopathy and the pathological sampling provided by EUS-FNA can provide additional staging information.
The EUS-FNA technique has already been established, and it is quite safe. The incidence of cancer-cell seeding is also considered to be extremely low, and only a few cases have been reported [28–31]. Even for pancreatic masses—the major indication for EUS-FNA—only 2 cases with tumor seeding have been reported (1 pancreatic cancer [29] and 1 intraductal papillary adenocarcinoma [31]). However, bile leakage during EUS-FNA may raise the risk of cancer-cell seeding in EUS-FNA performed for biliary lesions. Indeed, a previous study reported percutaneous transhepatic biliary drainage catheter tract recurrence in 5.2% of the patients with resected bile duct cancer [32], whereas the frequencies of needle-tract seeding from other malignancies, such as liver and pancreatic cancer, were reported to be only 0.003–0.009% [33]. Therefore, we were careful not to puncture the lesion through the gall bladder and bile duct lumen and to avoid bile leakage if at all possible. For reference, 4 patients with final diagnoses of malignancy were treated operatively in the present study, but cancer seeding was not observed during the surgery.
Our study has several limitations. It was a retrospective study and included a relatively small number of subjects. Therefore, a prospective study with a larger number of subjects will be needed in the future. Furthermore, not all patients underwent surgery to confirm the final pathological results. However, all patients without surgical pathology were followed carefully, and final results were assessed from their clinical courses, including imaging and serological tests.
Our results suggest that EUS-FNA is a sensitive and safe method for the diagnosis of suspected MBS. Patients with negative or nondiagnostic sampling on ERCP are particularly good candidates for EUS-FNA. The diagnostic result can have a significant impact on patient management, as shown in the present study. However, this procedure sometimes has technical difficulties. The transduodenal puncture approach is generally more difficult than the transgastric approach and must be carefully performed to avoid nearby large vessels, such as the portal vein and hepatic artery. Care must also be taken not to puncture the lesion through the gallbladder and bile duct lumen, if at all possible, in order to avoid bile leakage during the procedure.
References
de Bellis M, Sherman S, Fogel EL, Cramer H, Chappo J, McHenry L Jr, et al. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 2). Gastrointest Endosc. 2002;56:720–30.
Rosch T, Hofrichter K, Frimberger E, Meining A, Born P, Weigert N, et al. ERCP or EUS for tissue diagnosis of biliary strictures? A prospective comparative study. Gastrointest Endosc. 2004;60:390–6.
Fritscher-Ravens A, Broering DC, Sriram PV, Topalidis T, Jaeckle S, Thonke F, et al. EUS-guided fine-needle aspiration cytodiagnosis of hilar cholangiocarcinoma: a case series. Gastrointest Endosc. 2000;52:534–40.
Fritscher-Ravens A, Broering DC, Knoefel WT, Rogiers X, Swain P, Thonke F, et al. EUS-guided fine-needle aspiration of suspected hilar cholangiocarcinoma in potentially operable patients with negative brush cytology. Am J Gastroenterol. 2004;99:45–51.
Meara RS, Jhala D, Eloubeidi MA, Eltoum I, Chhieng DC, Crowe DR, et al. Endoscopic ultrasound-guided FNA biopsy of bile duct and gallbladder: analysis of 53 cases. Cytopathology. 2006;17:42–9.
Lee JH, Salem R, Aslanian H, Chacho M, Topazian M. Endoscopic ultrasound and fine-needle aspiration of unexplained bile duct strictures. Am J Gastroenterol. 2004;99:1069–73.
DeWitt J, Misra VL, Leblanc JK, McHenry L, Sherman S. EUS-guided FNA of proximal biliary strictures after negative ERCP brush cytology results. Gastrointest Endosc. 2006;64:325–33.
Byrne MF, Gerke H, Mitchell RM, Stiffler HL, McGrath K, Branch MS, et al. Yield of endoscopic ultrasound-guided fine-needle aspiration of bile duct lesions. Endoscopy. 2004;36:715–9.
Eloubeidi MA, Chen VK, Jhala NC, Eltoum IE, Jhala D, Chhieng DC, et al. Endoscopic ultrasound-guided fine needle aspiration biopsy of suspected cholangiocarcinoma. Clin Gastroenterol Hepatol. 2004;2:209–13.
Hijioka S, Mekky MA, Bhatia V, Sawaki A, Mizuno N, Hara K, et al. Can EUS-guided FNA distinguish between gallbladder cancer and xanthogranulomatous cholecystitis? Gastrointest Endosc. 2010;72:622–7.
Yasuda I, Tsurumi H, Omar S, Iwashita T, Kojima Y, Yamada T, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy for lymphadenopathy of unknown origin. Endoscopy. 2006;38:919–24.
Iwashita T, Yasuda I, Doi S, Kato T, Sano K, Yasuda S, et al. The yield of endoscopic ultrasound-guided fine needle aspiration for histological diagnosis in patients suspected of stage I sarcoidosis. Endoscopy. 2008;40:400–5.
Iwashita T, Yasuda I, Doi S, Nakashima M, Tsurumi H, Hirose Y, et al. Endoscopic ultrasound-guided fine-needle aspiration in patients with lymphadenopathy suspected of recurrent malignancy after curative treatment. J Gastroenterol. 2009;44:190–6.
Iwashita T, Yasuda I, Tsurumi H, Goto N, Nakashima M, Doi S, et al. Endoscopic ultrasound-guided fine needle aspiration biopsy for splenic tumor: a case series. Endoscopy. 2009;41:179–82.
Yasuda I, Kato T, Asano F, Okubo K, Omar S, Kako N, et al. Mediastinal lymph node staging in potentially resectable non-small cell lung cancer: a prospective comparison of CT and EUS/EUS-FNA. Respiration. 2009;78:423–31.
Sugiyama M, Atomi Y, Wada N, Kuroda A, Muto T. Endoscopic transpapillary bile duct biopsy without sphincterotomy for diagnosing biliary strictures: a prospective comparative study with bile and brush cytology. Am J Gastroenterol. 1996;91:465–7.
Vandervoort J, Soetikno RM, Montes H, Lichtenstein DR, Van Dam J, Ruymann FW, et al. Accuracy and complication rate of brush cytology from bile duct versus pancreatic duct. Gastrointest Endosc. 1999;49:322–7.
Leung JW, Sung JY, Chung SC, Chan KM. Endoscopic scraping biopsy of malignant biliary strictures. Gastrointest Endosc. 1989;35:65–6.
Foutch PG, Kerr DM, Harlan JR, Manne RK, Kummet TD, Sanowski RA. Endoscopic retrograde wire-guided brush cytology for diagnosis of patients with malignant obstruction of the bile duct. Am J Gastroenterol. 1990;85:791–5.
Foutch PG. Diagnosis of cancer by cytologic methods performed during ERCP. Gastrointest Endosc. 1994;40:249–52.
Fogel EL, Sherman S. How to improve the accuracy of diagnosis of malignant biliary strictures. Endoscopy. 1999;31:758–60.
Pugliese V, Conio M, Nicolo G, Saccomanno S, Gatteschi B. Endoscopic retrograde forceps biopsy and brush cytology of biliary strictures: a prospective study. Gastrointest Endosc. 1995;42:520–6.
Ponchon T, Gagnon P, Berger F, Labadie M, Liaras A, Chavaillon A, et al. Value of endobiliary brush cytology and biopsies for the diagnosis of malignant bile duct stenosis: results of a prospective study. Gastrointest Endosc. 1995;42:565–72.
Kubota Y, Takaoka M, Tani K, Ogura M, Kin H, Fujimura K, et al. Endoscopic transpapillary biopsy for diagnosis of patients with pancreaticobiliary ductal strictures. Am J Gastroenterol. 1993;88:1700–4.
Jailwala J, Fogel EL, Sherman S, Gottlieb K, Flueckiger J, Bucksot LG, et al. Triple-tissue sampling at ERCP in malignant biliary obstruction. Gastrointest Endosc. 2000;51:383–90.
Schoefl R, Haefner M, Wrba F, Pfeffel F, Stain C, Poetzi R, et al. Forceps biopsy and brush cytology during endoscopic retrograde cholangiopancreatography for the diagnosis of biliary stenoses. Scand J Gastroenterol. 1997;32:363–8.
Kitajima Y, Ohara H, Nakazawa T, Ando T, Hayashi K, Takada H, et al. Usefulness of transpapillary bile duct brushing cytology and forceps biopsy for improved diagnosis in patients with biliary strictures. J Gastroenterol Hepatol. 2007;22:1615–20.
Shah JN, Fraker D, Guerry D, Feldman M, Kochman ML. Melanoma seeding of an EUS-guided fine needle track. Gastrointest Endosc. 2004;59:923–4.
Paquin SC, Gariepy G, Lepanto L, Bourdages R, Raymond G, Sahai AV. A first report of tumor seeding because of EUS-guided FNA of a pancreatic adenocarcinoma. Gastrointest Endosc. 2005;61:610–1.
Doi S, Yasuda I, Iwashita T, Ibuka T, Fukushima H, Araki H, et al. Needle tract implantation on the esophageal wall after EUS-guided FNA of metastatic mediastinal lymphadenopathy. Gastrointest Endosc. 2008;67:988–90.
Hirooka Y, Goto H, Itoh A, Hashimoto S, Niwa K, Ishikawa H, et al. Case of intraductal papillary mucinous tumor in which endosonography-guided fine-needle aspiration biopsy caused dissemination. J Gastroenterol Hepatol. 2003;18:1323–4.
Takahashi Y, Nagino M, Nishio H, Ebata T, Igami T, Nimura Y. Percutaneous transhepatic biliary drainage catheter tract recurrence in cholangiocarcinoma. Br J Surg. 2010;97:1860–6.
Smith EH. Complications of percutaneous abdominal fine-needle biopsy. Review. Radiology. 1991;178:253–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohshima, Y., Yasuda, I., Kawakami, H. et al. EUS-FNA for suspected malignant biliary strictures after negative endoscopic transpapillary brush cytology and forceps biopsy. J Gastroenterol 46, 921–928 (2011). https://doi.org/10.1007/s00535-011-0404-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0404-z