Abstract
Both optimism and frustration exist regarding therapy for patients with chronic hepatitis B virus infection. Due to the recent advent of several drugs with potent antiviral capacities and comparatively low rates of adverse effects, considerable optimism has developed regarding the treatment of these patients. Chronic hepatitis B is now a treatable disease, and suppression of hepatitis B virus replication, normalization of alanine aminotransferase levels, seronegativity/seroconversion of hepatitis B e antigen and hepatitis B surface antigen, and decreased hepatic inflammation and liver fibrosis have been documented in chronic hepatitis B virus-infected patients treated with antiviral therapy. In contrast, many frustrations regarding antiviral therapy for chronic hepatitis B have arisen, because the disease, although treatable, is not curable. The present regimens of antiviral therapy modulate some intermediate parameters or so-called surrogate markers in chronic hepatitis B virus-infected patients, but usually fail to improve all intermediate parameters or ultimate clinical outcomes. In addition, major concerns remain about the applicability and use of antiviral drugs in developing and resource-constrained countries in which healthcare delivery systems do not support the proper use of antiviral therapy. New and more effective therapeutic regimens for chronic hepatitis B patients are needed that take into account potential surrogate markers of treatment outcomes and allow for effective collaboration between resource-constrained and advanced countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV), a member of the family Hepadnaviridae, is a non-cytopathic DNA virus. Worldwide, nearly 2 billion people have been infected at some point in their lives, and approximately 350–400 million people are chronically infected, a condition that implies ongoing HBV replication in infected hosts. Epidemiologic data indicate that HBV accounts for 0.5–1.2 million deaths annually, and approximately 15–25% of chronic hepatitis B patients will eventually die of HBV-related liver disease [1].
Ideally, all patients with chronic hepatitis B should be treated because they represent a permanent and living reservoir of the virus and can transmit the virus to healthy non-infected subjects. Even with the use of a potent prophylactic vaccine against HBV for the past three decades and the application of different public health measures to contain the spread of HBV, chronic hepatitis B patients are responsible for approximately 50 million new HBV infections each year [2]. In addition, chronic hepatitis B patients often develop complications that may compromise their quality of life and cause early disability and death [3]. However, antiviral therapy is not recommended for all chronic HBV-infected subjects, primarily because these drugs are not effective in patients without ongoing host immunity, a fact manifested by evidence of liver inflammation [4]. In addition, all patients with complications of chronic HBV infection should receive antiviral therapy, which aims to delay more severe complications such as hepatic decompensation, cirrhosis of the liver, hepatocellular carcinoma (HCC), and liver-related death. Much optimism has surrounded the use of antiviral therapy because the powerful drugs that have been developed during the past decade can effectively block HBV replication in a considerable number of patients with chronic hepatitis B. Furthermore, antiviral drugs lead to the normalization of alanine aminotransferase (ALT) levels, decrease liver inflammation and hepatic fibrosis, and induce seronegativity and/or seroconversion of hepatitis B e antigen (HBeAg) and hepatitis B surface antigen (HBsAg) in many chronic hepatitis B patients [5–10]. Randomized controlled trials (RCTs) with antiviral drugs in patients with chronic hepatitis B have shown considerable improvements in some intermediate parameters that have long been regarded as surrogate markers of the clinical outcome of HBV infection in these patients. However, improvement in all intermediate parameters of treatment outcome in chronic hepatitis B has not been achieved via the use of antiviral drugs. In addition, there is a lack of consensus regarding improvement of the clinical outcome in chronic hepatitis B patients using antiviral drugs. Some studies have reported some beneficial effects, whereas others have not shown significant improvement of clinical outcomes with antiviral drugs [11–17]. Furthermore, concerns have been raised about the different surrogate markers of outcome of antiviral therapy for chronic hepatitis B that have been used to assess the therapeutic efficacy of the antiviral drugs.
In addition to concerns about the efficacy of antiviral drugs, there are considerable reservations about the practical use of current antiviral regimens in developing and resource-constrained countries. Most clinical trials and RCTs with antiviral drugs in chronic hepatitis B have been conducted in developed, wealthy, and advanced countries. The inherent strength of developed and advanced countries lies in the fact of their advanced healthcare systems, and their socio-economic infrastructure allows for satisfactory drug compliance, proper assessment of patients for treatment, periodic assessment of viral and other markers that herald adverse effects, and adequate tackling of adverse effects [18, 19]. It is unclear whether chronic hepatitis B patients in developing countries can be treated with antiviral drugs according to recommendations based on the data from RCTs conducted in advanced countries [18–20].
Considering these facts, it appears that there are two major challenges for the therapy of chronic hepatitis B. One is a matter of science and is related to the development of potent and evidence-based therapeutic regimens against HBV. The second is a complex issue that is related to the social, economic, and healthcare delivery systems of developing countries that cannot be altered quickly [18–20]. We assume that these issues can be addressed in a scientific manner by creating real collaboration between developed and developing countries. On the one hand, scientific developments along with basic and clinical trials in advanced countries would elucidate designs for innovative and alternative therapeutic approaches for chronic hepatitis B. However, considerable numbers of chronic hepatitis B patients in advanced countries have already been treated with antiviral drugs. In addition, more powerful antiviral drugs would be used for treatment for chronic hepatitis B in advanced and wealthy countries. This might mean that there will be few cases of treatment-naïve chronic hepatitis B patients in developed countries in whom to conduct clinical trials with new drugs or therapeutic approaches. In contrast, millions of treatment-naïve chronic hepatitis B patients are present in developing countries. The real efficacy of the innovative and alternative therapies developed in advanced countries can only be properly assessed in treatment-naïve chronic hepatitis B patients in developing countries after the proper assessment of safety and efficacy in advanced countries. In addition, the future of therapy for chronic HBV infection may depend on the identification of surrogate markers of treatment outcome for antiviral drugs and a proper understanding of the pathogenesis of chronic HBV infection.
Need for globally applicable therapeutic recommendations for future treatment of chronic hepatitis B
Patients with chronic hepatitis B are treated according to therapeutic recommendations provided by different international and national liver organizations. The American Association for the Study of the Liver (AASLD) [21], the European Association for the Study of Liver Diseases (EASL) [22], and the Asia–Pacific Association for the Study of the Liver (APASL) [23] represent three major liver-related professional organizations that provide therapeutic guidelines for treating chronic hepatitis B patients in international arenas. In addition, different national liver organizations also produce their own recommendations for treating chronic hepatitis B patients, based on local scientific and social realities. The liver organizations update their recommendations from time to time on the basis of scientific developments and transmit these to physicians, policy makers, and patients. The scenario for therapeutic recommendations in most developing and resource-constrained countries is different from that in advanced countries. Most developing countries that harbor millions of HBV carriers lack viable professional liver organizations. They rarely develop therapeutic recommendations based on local realities and constraints. In fact, recommendations prepared by the AASLD, EASL, and APASL are partially followed by physicians in developing countries [20]. In fact, almost all types of drugs are available in these countries and are used in chronic hepatitis B patients as soon as professional associations, like the AASLD, EASL or APASL, recommend them. If this trend continues, it will be difficult to develop logical and rational treatment approaches that take local factors into account in developing countries. Therapeutic recommendations provided by the AASLD, EASL, and APASL have provided detailed criteria about viral load, and the biochemical and histological aspects required to select patients for antiviral therapy. However, there is a paucity of information about criteria for starting therapy in developing countries. Considering the present realities, it seems that therapeutic recommendations should include a note of caution indicating that for patients who would not be able to continue therapy due to economic and social factors, antiviral drugs for chronic hepatitis B should be prescribed cautiously. Physicians in developing countries should carefully counsel their patients about their economic status before prescribing antiviral drugs against HBV infection.
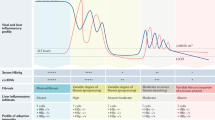
Ongoing regimens of antiviral therapy against chronic hepatitis B
Standard interferon (IFN) and its pegylated form (Peg IFN) have been used in chronic hepatitis B patients for the past three decades. At present, hepatitis B treatments also include nucleos(t)ide analogs (NAs) categorized as l-nucleosides (lamivudine, emtricitabine, telbivudine, and clevudine), acyclic phosphatases (adevovir and tenofovir), and cyclopentanes (entecavir). These drugs are used as monotherapy or in combination. IFN is usually given for a finite duration. On the other hand, a long-term suppressive course is used for NAs, with drugs being given for years. Different regimens of antiviral therapy with different combinations of drugs have been used in chronic hepatitis B patients. The rationale for these different approaches is to maximize therapeutic benefits while minimizing side effects. The effect of antiviral drugs in chronic hepatitis B patients is determined by the on-treatment effect or a sustained response. Different RCTs have shown that antiviral treatment leads to the improvement of one or more intermediate parameters, also regarded as surrogate markers or prognostic markers, in variable numbers of chronic hepatitis B patients; these parameters include decreased levels of HBV DNA, normalization of ALT, seronegativity of HBeAg, development of anti-HBe, clearance of HBsAg, expression of anti-HBs, decreased liver inflammation, and containment of liver fibrosis [5–10]. However, a conclusive positive impact of antiviral drugs on all intermediate parameters has not been shown. In addition, there is a lack of consensus about the modulation of clinical outcomes by antiviral therapy in chronic hepatitis B [11–17]. The Minnesota Evidence-based Practice Center (EPC) for a National Institutes of Health (NIH) Consensus Conference related to the management of chronic hepatitis B analyzed different RCTs of antiviral therapy in chronic hepatitis B [24]. Their data show that antiviral drugs did not reduce death, liver failure, or HCC in any credible study that they included in the analyses [25, 26]. They also reported that no single treatment improved all intermediate outcomes. Furthermore, they indicated that there was insufficient evidence to determine whether biochemical, viral, or histological measures are valid surrogates of treatment effects on mortality, liver failure, or HCC.
The apparent discrepancies regarding outcomes of antiviral therapy in chronic hepatitis B patients in individual RCTs may have been influenced by the nature of the study, the number and type of patients, the drugs used, and the method of assessment. On the other hand, the apparent discrepancies among the outcomes and conclusions of different meta-analyses may be attributable to: (1) the number of studies included, (2) the number of studies excluded, (3) the study size, (4) the quality of the studies, (5) criteria for inclusion, (6) criteria for exclusion, and (7) variability of follow-up duration. We are not going to provide a detailed description of these meta-analyses and will not comment on the quality of individual studies. However, the importance of RCTs and meta-analyses is immense in a global context because these studies provide a rationale for designing therapeutic approaches in different countries. The rest of this review focuses on two main issues that seem to be vital for the development of future therapy for HBV infection: (1) the use of surrogate markers for determining the efficacy of antiviral treatment for chronic hepatitis B and (2) the significance of HBV reduction due to antiviral therapy versus that occurring during the natural course of HBV infection, a factor that would validate the use of an alternative therapeutic regimen, such as immune therapy, in chronic hepatitis B.
Use of surrogate markers for determining efficacy of antiviral treatment for chronic hepatitis B
Antiviral drugs, especially NAs, cause a reduction of HBV DNA. In addition, ALT normalization, HBeAg seronegativity, anti-HBe seroconversion, HBsAg seronegativity, anti-HBs seroconversion, and improvement of liver inflammation and fibrosis have been reported in some, but not all, chronic hepatitis B patients after treatment with antiviral drugs. In spite of improvements in virological, biochemical, immunological, and histological parameters with antiviral therapy, few studies show that antiviral drugs significantly block or delay hepatic decompensation, the occurrence of liver cirrhosis and HCC, and liver-related death. It is controversial whether the HBV DNA load, HBeAg, HBsAg, anti-HBe, anti-HBs, and liver histology can be regarded as true surrogate markers of an efficient therapeutic outcome of antiviral therapy in chronic hepatitis B patients [24–26]. A surrogate marker should be strong enough to predict a final outcome. However, because chronic hepatitis B progresses slowly, it will take considerable time to determine viable surrogate markers of therapeutic efficacy. Studies must be conducted for decades, and serial observations should be done regarding the kinetics of different virological, biochemical, histological, and immunological markers. As a result, one or more surrogate markers may be determined, or, in contrast, studies may determine that no surrogate marker is available. There is a paucity of studies that assess the final outcome of antiviral therapy in chronic hepatitis B patients. One study showed that the occurrence of HCC and liver cancer was decreased in antiviral-treated chronic hepatitis B patients. However, the study was not designed to provide the kinetics of all surrogate markers of treatment outcome [14]. It seems that HBV DNA levels and HBeAg seroconversion may not be true surrogate markers of the clinical outcome of antiviral therapy for chronic hepatitis B [24, 26]. However, assessment should be made regarding the surrogacy of levels of HBsAg or covalently closed circular DNA (cccDNA) in RCTs, because few reports have examined the kinetics of these markers. The value of a surrogate marker of efficacy has considerable influence on antiviral therapy in a global context, and especially in developing countries. Assessment of questionable surrogate markers may shatter the ultimate purpose of good medical practice for treating chronic hepatitis B in developing countries. In these countries, improvement of any surrogate marker of treatment outcome may be defined as a better therapeutic outcome. The idea of using elusive surrogate markers is counterproductive, and, in the long run, compromises confidence in the health systems of developing countries. If surrogate markers are improperly defined, this can negatively regulate different preventive measures against HBV infection.
Significance of HBV reduction due to antiviral therapy
The development of evidence-based therapeutic approaches against HBV infection is dependent on the proper understanding of different cellular and molecular events that control HBV replication and liver damage. To develop insights into these factors, we examined differences in HBV control that occurs naturally versus that caused by antiviral drugs. Almost all epidemiologic data have shown that a high HBV load in patients with chronic hepatitis B has been consistently associated with a poorer clinical outcome. This is particularly relevant when patients with chronic HBV infection with very low or undetectable levels of HBV DNA are compared with patients with 105 or 106 copies/ml of HBV DNA [27, 28]. However, considerable numbers of HBV-infected patients do not develop complications and exhibit natural control of HBV DNA replication without any therapy [1, 3]. Progressive downregulation and negativity of HBV during natural infection is usually followed by the resolution of hepatitis, disappearance of HBV-related antigens, and expression of protective antibody like anti-HBs. The picture is quite different in patients with chronic hepatitis B treated with antiviral drugs. Although most patients with chronic hepatitis B receiving antiviral drugs show HBV DNA reduction, this is not usually followed by the disappearance of all HBV-related antigens, appearance of anti-HBs, or resolution of the disease. Although the mechanisms underlying these differences have not been properly elucidated, during the natural course of resolved HBV infection, downregulation of HBV DNA may be accomplished by the restoration of inherent host immunity. Thus, HBV DNA reduction is usually accompanied by the loss of HBeAg and HBsAg and the expression of anti-HBe and ant-HBs in the sera. On the other hand, in patients in whom antiviral therapy is used, downregulation of HBV DNA is a result of the interplay between drugs and the HBV replication system. This may be followed by the restoration of host immunity in some patients [29–31], but questions remain about the nature, magnitude, and sustainability of host immunity following antiviral drug treatment in chronic hepatitis B patients.
Future aspects of therapy for HBV via modulation of host immunity
HBV therapy faces two major challenges in future. First, more potent or alternative therapeutic approaches should be developed to combat HBV infection. Second, therapeutic regimens should be applicable to people in developing and resource-constrained countries. This latter challenge requires some type of meeting between science and social factors.
Treatment of HBV infection would be drastically altered if an antiviral drug capable of eradicating all forms of HBV; replicating HBV DNA, cccDNA, and extrahepatic HBV DNA, emerged. However, it is unknown whether such a drug will ever be available.
In this context, future attention should focus on developing alternative therapeutic approaches for HBV infection. Insights into prospective therapies have been gained from studies of HBV replication and liver damage after natural infection and after antiviral therapy. HBV is not a cytotoxic virus, and liver damage and HBV-related complications are mediated by the host immune responses. The immune responses of chronic hepatitis B patients may be broadly categorized into two types: one is protective immunity that controls the virus and liver damage and the other is of pathogenic nature, which induces liver damage and may have not a role in virus control. It has been shown that HBV-specific immune responses are usually protective in chronic hepatitis B patients, whereas non-HBV-specific immune responses cause liver damage [32–35]. Although these facts provide a rationale for immune therapy as an alternative therapeutic approach to chronic hepatitis B, the limited efficacy of polyclonal immune modulators in chronic hepatitis B patients is understandable because non-HBV-specific immune therapy may not have proper therapeutic efficacy. However, it is possible that HBV-specific immune responses may be induced later by polyclonal immune modulators, and this hypothesis needs to be assessed in chronic hepatitis B patients [35]. Immune therapy targeting natural killer cells, natural killer T cells, cells of innate immunity, and other immunocytes could provide important insights about the role of immune modulation in patients with chronic hepatitis B. In addition, cell-based immune therapy with bone marrow cells, dendritic cells, stem cells, and mesenchymal cells has shown some promise in chronic hepatitis B, but there is limited information about these studies. HBV-specific immune therapy that uses antigenic epitopes of HBV, HBV-related antigens, and HBV DNA may be effective. An HBsAg-based vaccine has been widely used as an antigen-specific therapy in chronic hepatitis B patients around the world. However, the efficacy of this vaccine is not clear [36]. An HBsAg-based vaccine has also been used in combination with antiviral agents. Unfortunately, significantly better efficacy of a combination of antiviral therapy and HBsAg-based immune therapy versus monotherapy with antiviral drugs could not be substantiated in an RCT [37].
In the meantime, it has become evident that hepatitis B core antigen (HBcAg)-specific cytotoxic T lymphocytes (CTL) are associated with the control of HBV replication and minimizing liver damage in chronic hepatitis B [33, 34]. However, there is a paucity of information about HBcAg-based therapeutic vaccine in chronic hepatitis B, although investigators have highlighted its use [37]. Recently, preliminary data about the therapeutic efficacy of a combination of HBsAg and HBcAg-based vaccine in chronic hepatitis B patients, administered by mucosal (nasal) and parenteral routes has been shown to lead to the sustained control of HBV and ALT levels 1 year after the discontinuation of therapy [38]; however, the authors of this study enrolled only 18 patients with chronic hepatitis B, and a larger study and prolonged follow up is warranted before any claims can be made. Other strategies of immune therapy using different immune modulators should also be tried in chronic hepatitis B patients.
The next challenge is to implement a regimen of anti-HBV therapy in developing countries. Antiviral agents such as NAs are now widely used in developing countries, but proper use of these agents cannot be expected due to the inherent social and economic limitations of these countries. As chronic hepatitis B progresses slowly, its negative impact on a healthcare delivery system will take time, and realization of the adverse effects of misusing current therapies may not be noted until it is too late to reverse them. In this context, attention should focus on innovative and alternative therapeutic regimens against chronic hepatitis B. As antigen-based vaccines are safe and inexpensive, clinical trials with these vaccines may be accomplished in developing countries with the active collaboration of developed countries. There are millions of treatment-naïve chronic hepatitis B patients in developing countries. At the same time, physicians in developed countries are highly experienced at conducting clinical trials. If a credible collaboration can be developed among physicians and hepatologists in developed and developing countries, it may be possible to develop a better regimen of HBV-specific immune therapy to treat chronic hepatitis B.
Conclusion
Future aspects of therapy for chronic hepatitis B virus infection may show considerable heterogeneity in different parts of the world if the present trends continue. More potent NA drugs may be available in the near future, but these drugs cannot be expected to improve clinical outcomes drastically. In advanced countries, an atmosphere of stagnation regarding treatment for chronic hepatitis B may develop if we remain fully dependent on and solely committed to NAs. At the same time, developing countries may become be filled with non-responders and partial responders to NAs, with only a small group of patients benefiting from therapy. Patients with mutant HBV would constitute a major burden to the healthcare delivery systems of resource-constrained countries in the future. Similarly, indiscriminant use of NAs in chronic hepatitis B patients co-infected with other viruses, such as human immune-deficiency virus (HIV), would create a more complex situation for controlling both HBV and HIV. Free drugs are available for HIV infection, but not for chronic hepatitis B, although many HIV/HBV coinfected patients die due to HBV-related liver diseases as opposed to the deaths being due to HIV. In addition, different doses of NAs are prescribed for HIV and chronic hepatitis B, and these drugs are not appropriately used in developing countries. Alternative and innovative therapies constitute some hope for a breakthrough in the treatment of chronic hepatitis B patients. But several steps are needed to get any real benefit from these therapeutic regimens. Vaccines containing antigens, epitopes, and DNA or immune therapy targeting different cells offer hope as alternative therapeutic strategies for chronic hepatitis B. The safety and efficacy of alternative therapies in chronic hepatitis B patients, determined by RCTs, could provide insights into whether these therapies would be able to stand the test of time. Finally, strong collaboration between developed and developing countries would be required to obtain benefits from new and innovative therapies.
References
Liaw YF, Chu CM. Lancet. Lancet. 2009;373:582–92.
Perrillo R. Hepatitis B virus replication × time equals trouble. Gastroenterology. 2006;130:989–91.
Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007;45:507–39.
Zoulim F, Perrillo R. Hepatitis B: reflections on the current approach to antiviral therapy. J Hepatol. 2008;48(Suppl 1):S2–19.
Janssen HL, Gerken G, Carreño V, Marcellin P, Naoumov NV, Craxi A, et al. Interferon alfa for chronic hepatitis B infection: increased efficacy of prolonged treatment. The European concerted action on viral hepatitis (EUROHEP). Hepatology. 1999;30:238–43.
Marcellin P, Lau GK, Bonino F, Farci P, Hadziyannis S, Jin R, et al. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2004;351:1206–17.
Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, Chang TT, Kitis G, Rizzetto M, et al. Adefovir dipivoxil for the treatment of hepatitis B e antigen-negative chronic hepatitis B. N Engl J Med. 2003;348:800–7.
Lai CL, Shouval D, Lok AS, Chang TT, Cheinquer H, Goodman Z, et al. Entecavir versus lamivudine for patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2006;354:1011–20.
Lai CL, Leung N, Teo EK, Tong M, Wong F, Hann HW, et al. A 1-year trial of telbivudine, lamivudine, and the combination in patients with hepatitis B e antigen-positive chronic hepatitis B. Gastroenterology. 2005;129:528–36.
Kweon YO, Goodman ZD, Dienstag JL, Schiff ER, Brown NA, Burchardt E, et al. Decreasing fibrogenesis: an immunohistochemical study of paired liver biopsies following lamivudine therapy for chronic hepatitis B. J Hepatol. 2001;35:749–55.
Liaw YF. Natural history of chronic hepatitis B virus infection and long-term outcome under treatment. Liver Int. 2009;29(Suppl 1):100–7.
Camma C, Giunta M, Andreone P, Craxi A. Interferon and prevention of hepatocellular carcinoma in viral cirrhosis: an evidence-based approach. J Hepatol. 2001;34:593–602.
Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, et al. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004;351:1521–31.
Lin SM, Sheen IS, Chien RN, Chu CM, Liaw YF. Long-term beneficial effect of interferon therapy in patients with chronic hepatitis B virus infection. Hepatology. 1999;29:971–5.
Gish RG, Lok AS, Chang TT, de Man RA, Gadano A, Sollano J, et al. Entecavir therapy for up to 96 weeks in patients with HBeAg-positive chronic hepatitis B. Gastroenterology. 2007;133:1437–44.
Zarski JP, Causse X, Cohard M, Cougnard J, Trepo C. A randomized, controlled trial of interferon alfa-2b alone and with simultaneous prednisone for the treatment of chronic hepatitis B. French Multicenter Group. J Hepatol. 1994;20:735–41.
Lampertico P, Del Ninno E, Manzin A, Donato MF, Rumi MG, Lunghi G, et al. A randomized, controlled trial of a 24-month course of interferon alfa 2b in patients with chronic hepatitis B who had hepatitis B virus DNA without hepatitis B e antigen in serum. Hepatology. 1997;26:1621–5.
Chien RN. On-treatment monitoring of chronic hepatitis B virus infection: an Asian-Pacific perspective. J Gastroenterol Hepatol. 2010;25:852–7.
Liaw YF. Antiviral therapy of chronic hepatitis B: opportunities and challenges in Asia. J Hepatol. 2009;51:403–7.
Akbar SM, Hiasa Y, Mishiro S, Onji M. Treatment of hepatitis B virus-infected patients: utility of therapeutic recommendations in developing countries. Expert Opin Pharmacother. 2009;10:1605–14.
Lok AS, McMahon BJ. AASLD guidelines chronic hepatitis B: update 2009. Hepatology. 2009;50:1–36.
European Association for the Study of the Liver. EASL clinical practice guidelines: management of chronic hepatitis B. J Hepatol. 2009;50:227–42.
Liaw YF, Leung N, Guan R, Lau GK, Merican I, McCaughan G, et al. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2008 update. Hepatol Int. 2008;22:262–83.
Wilt TJ, Shamliyan T, Shaukat A, Taylor BC, MacDonald R, Yuan JM, et al. Management of chronic hepatitis B. Evid Rep Technol Assess (Full Rep). 2008;174:1–671.
Taylor BC, Yuan JM, Shamliyan TA, Shaukat A, Kane RL, Wilt TJ. Clinical outcomes in adults with chronic hepatitis B in association with patient and viral characteristics: a systematic review of evidence. Hepatology. 2009;49(Suppl 5):S85–95.
Shamliyan TA, MacDonald R, Shaukat A, Taylor BC, Yuan JM, Johnson JR, et al. Antiviral therapy for adults with chronic hepatitis B: a systematic review for a National Institutes of Health Consensus Development Conference. Ann Intern Med. 2009;150:111–24.
Chu CM. Natural history of chronic hepatitis B virus infection in adults with emphasis on the occurrence of cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol. 2000;15(Suppl):E25–30.
Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73.
Lu GF, Tang FA, Zheng PY, Yang PC, Qi YM. Entecavir up-regulates dendritic cell function in patients with chronic hepatitis B. World J Gastroenterol. 2008;14:1617–21.
Boni C, Penna A, Ogg GS, Bertoletti A, Pilli M, Cavallo C, et al. Lamivudine treatment can overcome cytotoxic T-cell hyporesponsiveness in chronic hepatitis B: new perspectives for immune therapy. Hepatology. 2001;33:963–71.
Akbar SM, Horiike N, Chen S, Michitaka K, Abe M, Hiasa Y, et al. Mechanism of restoration of immune responses of patients with chronic hepatitis B during lamivudine therapy: increased antigen processing and presentation by dendritic cells. J Viral Hepat. 2011;18:200–5.
Rehermann B. Chronic infections with hepatotropic viruses: mechanisms of impairment of cellular immune responses. Semin Liver Dis. 2007;27:152–60.
Bertoletti A, Maini MK. Protection or damage: a dual role for the virus-specific cytotoxic T lymphocyte response in hepatitis B and C infection? Curr Opin Microbiol. 2000;3:387–92.
Maini MK, Boni C, Lee CK, Larrubia JR, Reignat S, Ogg GS, et al. The role of virus-specific CD8(+) cells in liver damage and viral control during persistent hepatitis B virus infection. J Exp Med. 2000;191:1269–80.
Sprengers D, Janssen HL. Immunomodulatory therapy for chronic hepatitis B virus infection. Fundam Clin Pharmacol. 2005;19:17–26.
Pol S, Michel ML. Therapeutic vaccination in chronic hepatitis B virus carriers. Expert Rev Vaccines. 2006;5:707–16.
Vandepapelière P, Lau GK, Leroux-Roels G, Horsmans Y, Gane E, Tawandee T, et al. Therapeutic vaccination of chronic hepatitis B patients with virus suppression by antiviral therapy: a randomized, controlled study of co-administration of HBsAg/AS02 candidate vaccine and lamivudine. Vaccine. 2007;25:8585–97.
Akbar SM, Al-Mahtab M, Rahman S, Aguilar JC, Onji M, Mishiro S. Therapeutic potential of a novel therapeutic vaccine containing both hepatitis B surface antigen (HBsAg) and hepatitis B core antigen (HBcAg) administered through mucosal and parenteral route in patients with chronic hepatitis B. Hepatology. 2010;52(Suppl):438A–9A.
Conflict of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akbar, S.M.F., Al-Mahtab, M. & Hiasa, Y. Future aspects of therapy for hepatitis B virus infection: value of surrogate markers, innovative therapy, and global collaboration. J Gastroenterol 46, 717–723 (2011). https://doi.org/10.1007/s00535-011-0401-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-011-0401-2