Abstract
Background
The diagnostic efficacy of endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) cytology may vary greatly depending on the treatment of the samples obtained and the level of proficiency of the cytopathologist or cytoscreener.
Methods
We prospectively evaluated the diagnostic efficacy of the cell block (CB) method and that of smear cytology using tissue samples obtained in the same needle pass at EUS-FNA in 33 patients with pancreatic tumors, abdominal tumors or swollen lymph nodes. An average of 3.1 passes were applied during the procedure without affirmation by rapid cytology. About half of the material obtained by each single pass was subjected to smear cytology, while the other half was evaluated by the CB method. Four to 12 glass slides were prepared for both Papanicolaou stain and Giemsa stain. The CB sections were prepared using the sodium alginate method and subjected to HE, PAS-AB and immunohistochemical stains. Two pathologists independently made cytological and histological diagnoses. The final diagnosis was based on integration of cytohistological findings, diagnostic imaging, and clinical course.
Results
The diagnostic accuracy of the CB method and that of smear cytology were 93.9 and 60.6%, respectively (p = 0.003), and their respective sensitivities were 92.0 and 60.0% (p = 0.02). It was easier to make a definite diagnosis of not only malignancies but also benign conditions by the CB method than by the smear method.
Conclusion
The CB method with immunostaining showed a higher diagnostic yield than smear cytology in patients who had undergone EUS-FNA without rapid on-site cytology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) cytology is widely used for histological confirmation of abdominal tumors, especially in patients with pancreatic tumors and/or possible nodal metastases [1–12]. However, its diagnostic efficacy may vary greatly depending on the level of proficiency of the cytopathologists or cytoscreeners when only the smear method is used. On the other hand, the cell block (CB) method allows cytological and/or histological evaluation with hematoxylin and eosin (HE) staining, which is familiar to pathologists, and with immunostaining for serial sections if necessary. However, the CB method utilizes a much smaller number of cells for examination than smear cytology and usually necessitates complicated preparation. Recently, a CB method using sodium alginate (SA) has been reported to be simple and inexpensive [13–15]. We prospectively evaluated the diagnostic efficacy of the CB method using SA in comparison with smear cytology of tissue samples obtained by EUS-FNA from patients with pancreatic tumors, abdominal tumors or swollen lymph nodes.
Patients and methods
This was a single-center prospective study performed at Sendai City Medical Center. The inclusion criteria were as follows: patients who needed cytological confirmation for (1) suspected pancreatic malignant tumors diagnosed as nonresectable by diagnostic imaging modalities, or those diagnosed as being benign or indeterminate by cytopathology under endoscopic retrograde cholangiopancreatography (ERCP), (2) swollen intra-abdominal lymph nodes, or (3) intra-abdominal tumors. Exclusion criteria included (1) age less than 18 years and (2) pancreatic tumors diagnosed cytologically or histologically before EUS-FNA.
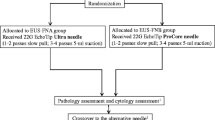
Between June 2005 and December 2008, pancreatic juice cytology and/or biopsy from the pancreatic duct, bile duct, or duodenum revealed malignancies in 43 of 216 patients with suspected malignant pancreatic tumors (Fig. 1). In the remaining 173, EUS-FNA was performed for those who gave informed consent, i.e., 9 patients with benign or indeterminate diagnoses, and for another 10 patients, to obtain cytological evidence for chemotherapy or pancreaticoduodenectomy. In this period, EUS-FNA was also performed in 12 patients with intra-abdominal lymphadenopathy and in 2 patients with an intra-abdominal tumor.
In total, EUS-FNA was performed in 33 patients (pancreatic tumor, 19: head, 8, body and tail, 11; abdominal lymphadenopathy, 12: peripancreatic-head, 3, peripancreatic-body or para-aorta, 9; abdominal tumor, 2: retrogastric, 1 and peripancreatic-tail, 1) using a GF-UC240P-AL5 endoscope (Olympus Ltd., Tokyo, Japan) and Echo-Tip 22G needles (Cook Endoscopy, Winston-Salem, NC, USA). At least two passes were made during the procedure, transduodenally in 3 patients with a pancreatic-head tumor and transgastrically in the remaining 30 patients, with the samples being immediately processed by a medical technician in the endoscopy suite without performing rapid cytology such as Diff-Quik stain.
Using the air in the syringe and the stylet of the needle, the material was gradually pushed out from the needle in more than four blocks, alternately onto glass slides for smear cytology and into a centrifuge tube with 10% formalin for CB evaluation. About half of the material obtained by each single pass of EUS-FNA was allocated for smear cytology, while the other half was allocated for the CB method, with the order of assignment to smear cytology or the CB method being changed with each puncture. Smears were made immediately at the bedside by a medical technician, and at least four (range 4–12) glass slides each were prepared for Papanicolaou stain and Giemsa stain. EUS-FNA was repeated until a whitish thin paste on glass slides or floating fragments in a centrifuge tube were confirmed by the medical technician and a endoscopist.
Cell block sections were made using the sodium alginate CB method [13–15], as illustrated in Fig. 2. Hematoxylin and eosin (HE) staining, periodic acid Schiff and Alcian-blue (PAS–AB) staining, and immunohistochemical stainings for Ki67, p53, chromogranin A, etc., were applied to the CB sections. The monoclonal or polyclonal antibodies used were MIB-1 (Immunotech, Marseilles, France) against Ki67, DO-7 (DAKO, Glostrup, Denmark) and Pab 1801 (Novocastra, Newcastle, UK) against p53 protein, DAK-A3 (Dako, Glostrup, Denmark) against chromogranin A, Ma695 (Novocastra, Newcastle, UK) against MUC1, Ccp58 (Novocastra, Newcastle, UK) against MUC2, 1G8 (Zymed Laboratories, Carlsbad, CA, USA) against MUC4, CLH2 (Novocastra, Newcastle, UK) against MUC5AC, CLH5 (Novocastra, Newcastle, UK) against MUC6, PD7/26/16, 2B11 (Nichirei, Tokyo, Japan) against LCA, N1580 (DAKO, Tokyo, Japan) against CD3, L26 (DAKO, Tokyo, Japan) against CD20cy, and MAB1313 (Chemicon International Inc., Temecula, CA, USA) against IgG4. Immunostaining was carried out by the streptavidin–biotin peroxidase (SAB) complex method, which was performed after treating the specimens in an autoclave in 10 mmol/L citrate buffer (pH 6.0) at 120°C for 10 min for Ki67 and p53. Two pathologists independently made cytological and histological diagnoses, with the diagnosis of greater malignancy being adopted.
The diagnostic criteria of the CB method were similar to those of biopsy. First, the cytopathological diagnoses obtained by the CB method were made with only HE staining and PAS–AB staining. In cases in which it was difficult to establish the diagnosis, immunostaining was also performed. The presence of positive cells for p53 stain or MUC1 stain along with high Ki67 LI was considered to be indicative of malignancy. The diagnostic criteria of smear cytology were based on the guidelines of the Papanicolaou Society of Cytopathology for fine-needle aspiration procedure and reporting [16], and Classes IV and V were regarded as malignant. Immunohistochemical stains were not employed in smear cytology.
In cytopathological diagnosis malignant lymphoma, endocrine tumors and gastrointestinal stromal tumors (GIST) were categorized as malignancies.
The diagnostic efficacies of smear cytology and the CB method with or without immunostaining were compared. The final diagnosis was based on the integration of cytohistological findings, diagnostic imaging, and clinical course for more than 6 months.
Statistical analysis
The necessary sample size was estimated to be 32 patients to detect a difference in accuracy at a 5% level of significance with a power of 80%, hypothesizing the expected accuracies of smear cytology and the CB method to be 60 and 90%, respectively.
Statistical analysis was performed by the χ 2 test or Fisher’s exact test where appropriate. Differences were considered significant at the p < 0.05 level.
Results
In 33 patients, an average of 3.1 passes (range: 2–5) were made during the EUS-FNA procedure.
The final diagnosis was malignancy in 25 patients and benignity in 8 patients (Table 1). The accuracies of cytological diagnosis by histological type using the CB method with and without immunostaining and by smear cytology were 94, 76, and 58%, respectively. A diagnosis of adenocarcinoma was established in 95% (19/20) and in 85% (17/20) of the patients by the CB method with and without immunohistochemical stains, respectively, and in 65% (13/20) by smear cytology. In 7 patients with adenocarcinoma, 5 with pancreatic cancer and 2 with nodal metastatic cancer, smear cytology failed to establish the correct diagnosis. The CB method using only HE staining and PAS–AB staining also did not give the correct diagnosis in 3 patients with pancreatic adenocarcinoma. Immunochemical stains in the CB method were positive for p53 in 4/7, for MUC1 in 5/7, and Ki67LI ≥10% in 7/7. In only one patient with pancreatic-body cancer, cytological diagnosis by the CB method with immunostaining was negative for malignant cells (negative for p53 and MUC1), although Ki67LI was higher than 10%.
In a patient with an endocrine tumor, immunohistochemical staining in the CB method was positive for chromogranin A. In a patient with a clinically malignant retrogastric tumor 50 mm in diameter, the cell block specimen showed a small number of bundles of spindle cells focally positive for c-kit. However, it was difficult to determine whether or not the lesion was a malignant GIST. In this patient, smear cytology and the CB method without immunostaining also failed to confirm malignancy. Histological examination of the surgically resected tumor revealed it to be a gastric GIST.
A discrepancy between the cytological diagnosis obtained with the CB method with immunostaining and that obtained by smear cytology was observed in 8 patients with a final diagnosis of malignancy: 4 with pancreatic cancer, 1 with pancreatic endocrine tumor, 2 with nodal metastasis and 1 with GIST, all of whom were correctly diagnosed by the CB method with immunostaining. Especially in 5 patients, i.e., 2 with pancreatic cancer, 1 with pancreatic endocrine tumor, 1 with malignant lymphoma, and 1 with GIST, immunohistochemical staining contributed to the establishment of the diagnosis by the CB method. It was easier to make a definite diagnosis of malignancy by the CB method with the addition of immunohistochemical staining than by the smear method (Figs. 3, 4). Furthermore, a diagnosis of sarcoidosis was made due to the presence of Ziehl–Neelsen negative staining of granulomas proven by the CB method.
a Microscopic findings of the CB method. Well-differentiated tubular adenocarcinoma (H&E ×50). b AB–PAS ×50. c Ki67LI >40%, ×50. d Diffusely positive for p53 stain, ×50. e Diffusely positive for MUC1 stain, ×50. Same case as that shown in Fig. 3
The diagnostic efficacies of smear cytology and the CB method with and without immunostaining are shown in Tables 2 and 3. The sensitivity (72%) and the accuracy (79%) of the CB method using only HE staining and PAS–AB staining were higher than those of the smear method (60 and 61%), although not significantly. On the other hand, the sensitivity (92%) and the accuracy (94%) of the CB method with immunostaining were significantly higher than those of the smear method (p < 0.02 and p < 0.003, respectively). Although the positive predictive value (PPV) of smear cytology and that of the CB method with immunostaining were both high, the negative predictive value (NPV) of smear cytology was lower (36%) than that of the CB method with immunostaining (89%) (p < 0.03).
No serious complications were observed in the present study.
Discussion
EUS-FNA is increasingly performed for cytological and/or histological evaluations of pancreatic masses and abdominal lymphadenopathy, and is thought to be a safe and cost-efficient method for adequately selecting surgical candidates [1–12]; there have been relatively few reports of complications such as bleeding and tumor seeding after EUS-FNA [17–19].
Smear cytology, which has long been performed as a standard technique for cytology, entails several problems. Cells of the sections used for Papanicolaou staining tend to peel off due to ethanol fixation. Because cells are swollen and degenerated by Giemsa stain and Diff-Quick stain, it is usually difficult to evaluate individual cells in cumulative clusters. Schwartz et al. [6] reported that the false-positive rate of EUS-FNA was 1.6% in 188 patients with malignant cytology results who had undergone surgery. Therefore, the expertise of a cytopathologist is mandatory in order to make accurate cytological diagnoses using sections obtained by EUS-FNA.
The diagnostic accuracy of EUS-FNA is reported to be high if an experienced cytopathologist or cytoscreener is present in the endoscopy unit during the procedure and confirms the adequacy of the material using a rapid smear cytology technique such as Diff-Quick stain immediately after tissue acquisition [2, 8]. However, in most institutions, the on-site presence of such a specialist for every EUS-FNA is difficult in practice due to financial constraints. Layfield et al. [5] reported that remuneration for intraprocedural consultations by cytopathologists for FNA is insufficient by current Medicare compensation schedules based on the CPT code 88172 for on-site evaluation in the United States.
It is sometimes possible to obtain an adequate tissue sample for histological examination by EUS-FNAB (EUS-guided fine-needle aspiration biopsy) without confirmation by on-site rapid cytology [20]. Also, serial sections using immunochemical staining for tissue obtained by EUS-FNAB are very useful for the determination of a histological diagnosis [21]. However, due to the stiffness of the needle, there are limitations on the puncture route and difficulties in obtaining sufficient material with currently available needles in some cases, especially for lesions in the pancreatic head and uncinate process [22]. In the present study, EUS-FNA was performed without difficulty in almost all of the patients with lesions at various sites using a 22G needle. The results obtained by the CB method were more satisfactory than those obtained with conventional smear cytology. EUS-FNA with the CB method was effective in achieving adequate material acquisition and in establishing a histological diagnosis regardless of the location of lesions or approach routes.
Wallace et al. [4] reported that Cytospin-CB methods did not add any additional diagnostic information compared with direct smear cytology. They flushed the needle with sterile saline solution and gathered the residual contents contained therein after no further material could be retrieved for smear cytology, and subjected the flushed material to Cytospin-CB methods. In the present study, we used nearly the same amount and quality of material for both the CB method and for smear cytology. This is probably the main reason that the efficacy of the CB method was much better than that in the previous reports [1, 4]. Moreover, the serial sections with immunohistochemical staining were very useful for establishing a definitive cytohistological diagnosis in the majority of patients [7, 9]. Chhieng et al. [7] applied immunohistochemical stains for MUC1 and MUC2 to the CB obtained by EUS-FNA in 39 patients with pancreatic tumor and reported that MUC1 staining was noted in 96% of pancreatic ductal carcinomas.
On the other hand, in a retrospective study of EUS-FNA for pancreatic neoplasms, Ardengh et al. [23] reported that the accuracy of the CB method (86.5%) was better than that of smear cytology (68%), although their NPVs were not satisfactory (55.1 and 36%, respectively). They did not allocate the samples obtained in the same needle pass to the two methods and did not apply immunohistochemical staining to ductal cancer. In the present study, we prospectively compared the diagnostic efficiency of the CB method, using immunohistochemical stains if necessary, with smear cytology in the same patients and found the NPV of the CB method (89%) to be higher than that of smear cytology (36%).
Although the CB method is useful, processing of the material is somewhat complicated. Of the various CB methods, the CB method using SA is probably one of the simplest and most inexpensive methods for paraffin sectioning of minute specimens, as this method can be carried out at room temperature without additional special instruments [13–15].
On the other hand, although immunochemistry on direct smears has potential utility, it entails several problems as follows [24]: (1) Serial sections are not available for use with antibody panels. (2) Cell loss may occur during staining. (3) Three-dimensional cell groups may “trap” antibodies, leading to nonspecific staining. (4) A mechanical smearing process may lead to disruption of cells and leakage of antigen. (5) There is a potential for high background staining due to blood and necrotic materials. These problems with false-positive and false-negative reactions have limited the widespread application of this technique. Therefore, we did not perform immunochemical staining on direct smears and performed only Papanicolaou staining and Giemsa staining for smear cytology.
However, smear cytology is superior to the CB method in several points. The number of cells examined by smear cytology is usually much larger than that examined by the CB method. Generally, the majority of cells obtained by EUS-FNA are available for a number of preparations for microscopic evaluation by smear cytology, while only one section can be examined by the CB method. Secondly, smear cytology requires a much shorter time for preparation and staining than the CB method.
Probably the best method for EUS-FNA is a combination of smear cytology with on-site rapid evaluation and the CB method with immunostaining. However, every facility has limitations on staff and equipment. The findings of our study on the sensitivity (92%) and accuracy (94%) of the CB method with immunostaining showed that the method is promising for clinical use and has the potential to reduce the cost of establishing a diagnosis by EUS-FNA.
The present study had limitations. Firstly, the final diagnosis was not confirmed by histological examination of the resected specimens in most patients. Secondly, the number of patients included in this study was not sufficient to evaluate the diagnostic efficacy of the CB method for each organ such as the pancreas or the lymph nodes separately. Thirdly, the diagnostic efficacy of the CB method was not compared between those with and those without on-site confirmation of adequate material by a cytopathologist or cytoscreener. Further studies such as a randomized controlled trial with an adequate number of patients with and without rapid on-site cytology by an experienced cytopathologist or cytoscreener are warranted to evaluate the need for confirmation by on-site smear cytology in addition to the CB method.
In conclusion, the CB method with immunostaining showed a higher diagnostic yield than smear cytology in patients who had undergone EUS-FNA without on-site rapid cytology. This suggests that the CB method with immunostaining for tissue samples obtained by EUS-FNA is a promising alternative to smear cytology.
References
Chang KJ, Nguyen P, Erickson RA, Durbin TE, Katz KD. The clinical utility of endoscopic ultrasound-guided fine-needle aspiration in the diagnosis and staging of pancreatic carcinoma. Gastrointest Endosc. 1997;45:387–93.
Erickson RA, Sayage-Rabie L, Beissner RS. Factors predicting the number of EUS-guided fine-needle passes for diagnosis of pancreatic malignancies. Gastrointest Endosc. 2000;51:184–90.
Yamao K, Ohashi K, Nakamua T, Suzuki T, Watanabe Y. Endoscopic ultrasound-guided fine-needle aspiration. Digestive Endosc. 2000;12:S53–6.
Wallace MB, Kennedy T, Durkalski V, Eloubeidi MA, Etamad R, Matsuda K, et al. Randomized controlled trial of EUS-guided fine needle aspiration techniques for the detection of malignant lymphadenopathy. Gastrointest Endosc. 2001;54:441–7.
Layfield LJ, Bentz JS, Gopez EV. Immediate on-site interpretation of fine-needle aspiration smears. A cost and compensation analysis. Cancer (Cancer Cytopathol). 2001;93:319–22.
Schwartz DA, Unni KK, Levy MJ, Clain JE, Wiersema MJ. The rate of false-positive results with EUS-guided fine-needle aspiration. Gastrointest Endosc. 2002;56:868–72.
Chhieng DC, Benson E, Eltoum I, Eloubeidi MA, Jhala N, Jhala D, et al. MUC1 and MUC2 espression in pancreatic ductal carcinoma obtained by fine-needle aspiration. Cancer (Cancer Cytopathol). 2003;99:365–71.
Klapman JK, Logrono R, Dye CE, Waxman I. Clinical impact of on-site cytopathology interpretation on endoscopic ultrasound-guided fine needle aspiration. Am J Gastroenterol. 2003;98:1289–94.
Ardengh JC, Paulo GA, Ferrari AP. EUS-guided FNA in the diagnosis of pancreatic neuroendocrine tumors before surgery. Gastrointest Endosc. 2004;60:378–84.
Volmar KE, Vollmer RT, Jowell PS, Nelson RC, Xie HB. Pancreatic FNA in 1000 cases: a comparison of imaging modalities. Gastrointest Endosc. 2005;61:854–61.
Agarwal B, Krishna NB, Labundy JL, Safdar R, Akduman EI. EUS and/or EUS-guided FNA in patients with CT and/or magnetic resonance imaging findings of enlarged pancreatic head or dilated pancreatic duct with or without a dilated common bile duct. Gastrointest Endosc. 2008;68:237–42.
Michael H, Ho S, Pollack B, Gupta M, Gress F. Diagnosis of intra-abdominal and mediastinal sarcoidosis with EUS-guided FNA. Gastrointest Endosc. 2008;67:28–34.
Basch PF. An alginate matrix double-embedding method for paraffin sectioning of minute specimens. Stain Technol. 1986;61:235–8.
Guo J, Jourdian GW, Maccallum DK. Culture and growth characteristics of chondrocytes encapsulated in alginate beads. Connect Tissue Res. 1989;19:277–97.
Sano J, Yoshimoto N, Mizoguchi Y, Saito M. Utility of sodium alginate cell block method. J Jpn Soc Clin Cytol. 2005;44:291–7. In Japanese with English abstract.
Suen KC, Abdul-Karim FW, Kaminsky DB, Layfield LJ, Miller TR, Spires SE, et al. Guidelines of the Papanicolaou Society of Cytopathology for fine needle aspiration procedure and reporting: the Papanicolau Society of Cytology Task Force on Standards of Practice. Diagn Cytopathol. 1997;17:239–47.
Wiersema MJ, Vilmann P, Giovannini M, Chang KJ, Wiersema LM. ASGE guideline: complications of EUS. Gastrointest Endosc. 2005;61:8–12.
Paquin SC, Gariepy G, Lepanto L, Bourdages R, Raymond G, Sahai AV. A first report of tumor seeding because of EUS-guided FNA of a pancreatic adenocarcinoma. Gastrointest Endosc. 2005;61:610–1.
Doi S, Yasuda I, Iwashita T, Ibuka T, Fukushima H, Akaki H, et al. Needle tract implantation on the esophageal wall after EUS-guided FNA of metastatic mediastinal lymphadenopathy. Gastrointest Endosc. 2008;67:988–90.
Storch I, Jorda M, Thurer R, Raez L, Rocha-Lima C, Vernon S, et al. Advantage of EUS trucut biopsy combined with fine-needle aspiration without immediate on-site cytopathologic examination. Gastrointest Endosc. 2006;64:505–11.
Yasuda I, Tsurumi H, Omar S, Iwashita T, Kojima Y, Yamada T, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy for lymphadenopathy of unknown origin. Endoscopy. 2006;38:919–24.
Shah SM, Ribeiro A, Levi J, Jorda M, Rocha-Lima C, Sleeman D, et al. EUS-guided fine needle aspiration with and without trucut biopsy of pancreatic masses. J Pancreas. 2008;9:422–30.
Ardengh JC, Lopes CV, Lima LFP, Venco F, Santo GC, Begnami MD, et al. Cell block technique and cytological smears for the differential diagnosis of pancreatic neoplasms after endosonography-guided fine-needle aspiration. Acta Gastroenterol Latinoam. 2008;38:246–51.
Ronald AD, Hoda RS. Immunochemistry and molecular biology in cytological diagnosis. In: Koss LG, Melamed MR, editors. Koss’s diagnostic cytology and its histopathologic bases. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 1635–80.
Acknowledgments
We are grateful to Ms. Takako Kato, Mr. Mitsuru Sasaki, Mr. Shinya Kudo, Ms. Junko Watanabe, and Ms. Miyuki Abe for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noda, Y., Fujita, N., Kobayashi, G. et al. Diagnostic efficacy of the cell block method in comparison with smear cytology of tissue samples obtained by endoscopic ultrasound-guided fine-needle aspiration. J Gastroenterol 45, 868–875 (2010). https://doi.org/10.1007/s00535-010-0217-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-010-0217-5