Abstract
Background
A traditional Japanese medicine, rikkunshito, has been reported to relieve dyspepsia symptoms. We investigated the effect of rikkunshito on RE-induced abdominal dyspepsia, and performed experiments to elucidate the mechanism of that effect.
Methods
RE model rats were prepared using 8-week-old male Wistar rats, and rikkunshito was administered in drinking water. Voluntary movement was used as an index of RE-induced abdominal dyspepsia, which was monitored by an infrared sensor. On the tenth day after surgery, the total area of esophageal erosion was measured, and samples of nonerosive mucosa were collected. Using those samples, intercellular spaces of epithelial mucosa were examined by transmission electron microscopy, and the NP-40-soluble and -insoluble levels of the tight junction proteins claudin-1, -3 and -4 and their mRNAs were determined.
Results
Rikkunshito did not reduce the average total area of erosive lesions in the esophageal mucosa of RE model rats. On day 10, voluntary movement was significantly decreased in the RE model rats and rikkunshito significantly increased it. Nonerosive esophageal mucosa from RE rats showed dilation of intercellular spaces in epithelium, and significantly decreased claudin-3 mRNA and protein levels. Rikkunshito significantly suppressed intercellular space dilation and significantly increased the level of NP-40-insoluble claudin-3, but it did not affect the mRNA level, suggesting that it promoted tight junction formation by facilitating the translocation of proteins.
Conclusion
Rikkunshito increased voluntary movement in RE model rats. This may have been because rikkunshito ameliorated the symptoms of RE by improving the barrier function of esophageal mucosa.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroesophageal reflux disease (GERD) is a condition that develops when the reflux of stomach contents causes troublesome symptoms and/or complications [1]. It can have a considerable negative impact on the patient’s quality of life [2, 3]. The mechanism of GERD symptom manifestation is complicated. Although mucosal damage in GERD increases in proportion to the extent of reflux of gastric acid, the severity of GERD symptoms is not related to the extent of esophageal mucosa damage [4]. GERD symptoms are thought to be caused by the complex interaction of a variety of factors, including reflux of gastric contents, esophageal motility dysfunction, impaired esophageal epithelial resistance, and hypersensitivity [5]. This suggests that the symptoms of GERD may not be relieved by treatment with inhibitors of gastric acid secretion only, and it has been reported that proton pump inhibitors are less effective in nonerosive reflux disease (NERD) than in reflux esophagitis (RE) [6, 7].
In recent years, the herbal medicine rikkunshito has been used to treat symptoms of GERD, and reports that it is efficacious have been appearing [8, 9]. However, its mechanism of action is not well understood. Therefore, in this study, we used a rat model of RE to investigate the effect of rikkunshito on GERD and the mechanism of action of that effect. In these experiments, the effect of rikkunshito on symptoms was evaluated by using the amount of voluntary movement by the rats as an index of symptoms, and the mechanism of symptom reduction was investigated by focusing on the intercellular spaces in epithelium of esophageal mucosa, and on tight junctions of the esophageal epithelium.
Materials and methods
Experimental animals
Male Wistar rats aged 6–7 weeks were purchased from Clea Japan Inc. (Tokyo, Japan). After the rats had been acclimatized for 1–2 weeks, they were used in the experiments at 8 weeks of age. During the experiments, the rats were subjected to an artificial light–dark cycle with light from 7:00 a.m. to 7:00 p.m., were provided with food and water ad libitum, and were housed at 24 ± 2°C and 55 ± 10% relative humidity. All of the experiments were performed in accordance with the guidelines of the animal welfare committee of Tsumura & Co. (Tokyo, Japan), and were performed between the hours of 9 a.m. and 6 p.m.
Drugs
Rikkunshito, which was obtained from Tsumura and Co., is a powder prepared by extracting a mixture of Glycyrrhizae radix, Zingiberis rhizoma, Atractylodis lanceae rhizoma, Zizyphi fructus, Aurantii nobilis pericarpium, Ginseng radix, Pinelliae tuber, and Hoelen in hot water and then spray drying the resulting extract. Suspensions (0.3 and 0.6% w v−1) of rikkunshito in purified water were administered as drinking water daily for 10 days, beginning on the day after surgery.
Preparation of the rat chronic acid reflux esophagitis model
The chronic acid RE model was prepared based on the method of Omura et al. [10]. Rats were fasted for 24 h and then anesthetized with ether, the abdomen of each rat was opened with a midline epigastric incision; the stomach and duodenum were exteriorized, and the transitional region between the forestomach and the glandular stomach (the limiting ridge) was ligated with 1–0 silk thread (Natsume Seisakusho Co., Tokyo, Japan). Next, the duodenum was wrapped near the pylorus with a 2-mm-wide piece of an 18-Fr Nélaton catheter (Terumo Corporation, Tokyo, Japan), and the catheter was immobilized by suturing it to the serosa of the pylorus with 5-0 nylon thread (Natsume); see Fig. 1. After confirming that hemorrhage was absent, the abdomen was closed by suturing the abdominal wall with 2-0 silk thread (Natsume) and the skin with an automatic suturing device. The sham operations were identical except that the transitional region between the forestomach and the glandular stomach was not ligated, and a piece of catheter was not placed around the duodenum. Instead, the exteriorized stomach and duodenum were left outside the body for approximately 1 min and then returned to the abdominal cavity. After surgery, the rats were fasted for another 24 h.
Preparation of the rat model of reflux esophagitis. Duodenal stenosis was created by wrapping the duodenum near the pylorus with a piece of 18-Fr Nélaton catheter (width: 2 mm). To prevent catheter dislodgement, the edge of the catheter was sutured to the serosa of the pylorus using a 5-0 nylon thread. The transitional region between the forestomach and the glandular portion (the limiting ridge) was ligated with 1-0 silk thread
Measurement of voluntary movement
The rats were housed at 2 animals per cage and acclimatized for 1 week before measuring voluntary movement. Beginning on the day after surgery, the amount of voluntary movement in each cage was measured for 12 h per day (from 7 p.m. to 7 a.m. the next day) with an infrared sensor (NS-AS01; Neuroscience Inc., Tokyo, Japan). The infrared sensor (placed on the top of the cage) counted the movements of the rats, the movement from initiation to completion was regarded as one count, and the sensor was adjusted to ignore grooming or standing up [11].
Measurement of gross esophageal lesions and investigation of intercellular spaces in esophageal epithelium
On the tenth day after preparation of the RE model (day 10), each rat was laparotomized under ether anesthesia, the abdominal vena cava was severed, and the animal was exsanguinated. Then the esophagus was removed, opened with a longitudinal incision, and immobilized on a rubber plate with insect pins. The entire esophagus was photographed with a digital camera (E5700; Nikon Corporation, Tokyo, Japan), the image was imported into image analysis software (WinROOF; Mitani Corporation, Tokyo, Japan), sites of esophageal mucosal erosion were identified, and the total area of those sites was measured.
Esophageal mucosal tissue from randomly selected nonerosive sites located at least 2 mm from erosive sites was collected for examination by transmission electron microscopy from rats euthanized on day 10. In this animal model, erosions were mainly seen in the middle of the esophagus. The tissue was cut into squares of approximately 5 mm, which were fixed in 2.5% glutaraldehyde and postfixed in 1% osmium tetroxide. Those specimens were treated with ethanol and n-butyl glycidyl ether (QY-1), and then embedded in Epon 812 Resin (TAAB Laboratories Equipment Ltd., Aldermaston, UK). The intercellular spaces in esophageal epithelium in 5 randomly selected visual fields per specimen were examined with a transmission electron microscope (JEM-1010; JEOL Ltd., Tokyo, Japan) at a magnification of 20,000.
RNA isolation and reverse transcription
On day 10, the esophagus was removed as described above. Mucosal tissue was obtained from sites that were superior to the gastroesophageal junction and within 3 cm of it, and that appeared nonulcerated on the basis of macroscopic examination. At such sites, 0.5 mL of ice-cold physiological saline was injected in the submucosa with a 27 G needle, and the mucosa was detached from the muscular layer in 3- to 4-mm squares.
Total RNA was isolated from the esophageal mucosa samples with a Qiagen RNeasy Mini Kit (Qiagen, Valencia, CA, USA) according to the product protocol, and the concentration of each total RNA sample was determined with a NanoDrop 1000 system (Thermo Scientific). Reverse transcription reactions were carried out with TaqMan reagents (Applied Biosystems) in a thermal cycler (Applied Biosystems) at 25°C for 5 min, 48°C for 30 min, and 95°C for 5 min.
Quantification of claudin mRNA using real-time PCR
Real-time polymerase chain reactions (PCRs) were performed using TaqMan 2× PCR Master Mix (Applied Biosystems) and a 7900HT Fast Real-Time PCR System (Applied Biosystems). The primers provided with TaqMan Gene Expression Assays (claudin-1, Rn00581740m1; claudin-3, Rn00581751s1; claudin-4, Rn01196224s1; β-actin: Rn00667869m1) (Applied Biosystems) were used as the claudin and β-actin primers. All of the real-time PCRs were run under the following thermal cycling conditions: hold at 50°C for 2 min and then 95°C for 10 min, followed by 40 cycles of 95°C for 15 s and 60°C for 1 min. The amount of each claudin mRNA was normalized to the amount of β-actin.
Assessment of protein levels by western blot analysis
On day 10, samples (3- to 4-mm squares) of detached esophageal mucosa were obtained as described above for RNA isolation and reverse transcription. Those samples were divided into NP-40-soluble and -insoluble fractions by the method of Sakakibara et al. [12]. Each sample was immersed in 200 μL of ice-cold NP-40 lysis buffer [25 mM HEPES/NaOH pH 7.4, 150 mM NaCl, 4 mM ethylenediaminetetraacetic acid (EDTA), 25 mM NaF, 1% NP-40, 1 mM Na3VO4, protease inhibitor cocktail (Sigma–Aldrich Corporation, St. Louis, MO, USA)] and then homogenized. The homogenized sample was mixed gently on a rotary shaker for 30 min at 4°C, and then centrifuged at 10,000g for 30 min at 4°C. The resulting supernatant was collected as the NP-40-soluble fraction. The sediment was homogenized again in 40 μL of sodium dodecyl sulfate (SDS) lysis buffer (25 mM HEPES/NaOH pH 7.5, 4 mM EDTA, 25 mM NaF, 1% SDS, 1 mM Na3VO4), and then mixed with 160 μL of NP-40 lysis buffer. Next, each sample was mixed gently on a rotary shaker for 30 min at 4°C, and was then centrifuged at 10,000g for 30 min at 4°C. The resulting supernatant was collected as the NP-40-insoluble fraction. Protein concentrations were measured with a protein assay kit (Bio-Rad Laboratories Inc., Hercules, CA, USA) using bovine serum albumin as the standard.
The NP-40-soluble and -insoluble fractions from each sample were loaded on a 12.5% polyacrylamide gel (Atto Corporation, Tokyo, Japan) at 0.6 μg of protein per well and electrophoresed at 0.3 mA cm−2 for 60 min in SDS-polyacrylamide gel electrophoresis buffer (25 mM Tris-base, 19 mM glycine, 0.1% SDS). After electrophoresis, the proteins were transferred to polyvinylidene difluoride membranes (GE Healthcare UK Ltd., Little Chalfont, UK) by a current of 1.75 mA cm−2 for 45 min using the semidry method. Next, blocking was performed by placing each membrane in TBS-T buffer (0.1% Tween 20) containing 5% skim milk for 60 min at room temperature. After blocking, the membranes were washed once with TBS-T buffer, and then were exposed to rabbit anti-claudin-1 antibody (50 ng mL−1; Zymed Laboratories, San Francisco, CA, USA), rabbit anti-claudin-3 antibody (500 ng mL−1; Zymed Laboratories), or rabbit anti-claudin-4 antibody (50 ng mL−1; Zymed Laboratories) overnight in a refrigerator. The membranes were then washed with TBS-T buffer 3 times for 10 min each, after which they were exposed for 60 min at room temperature to horseradish peroxidase-labeled goat anti-rabbit IgG antibody (GE Healthcare UK Ltd.) diluted 5000-fold. Each antibody was diluted to the specified concentration with TBS-T buffer (0.1% Tween 20) containing 1% skim milk. The membranes were again washed with TBS-T buffer 3 times for 10 min each and then were treated with western blotting detection reagent (ECL Plus; GE Healthcare UK Ltd.) at room temperature for 5 min. The fluorescence intensity of each band was scanned with a variable-mode imager (Typhoon 9410; GE Healthcare UK Ltd.) and quantified with image processing software (ImageQuant TL; GE Healthcare UK Ltd.). Claudin-1, -3, and -4 were detected as a 22 kD band. The quantity of each protein in each fraction was calculated relative to the average intensity of the soluble fraction band for that protein in the sham-operated animals, which was assigned a value of 1.
Statistical analysis
Measured values are shown as mean ± standard error (SE). For each parameter, the difference between the sham group and the vehicle control group was tested for significance by Student’s t test, and if the t test showed a significant difference, the difference between the vehicle control group and each treatment group was tested for significance by Dunnett’s multiple comparison test. The significance level was 5% on both sides.
Results
Effect of rikkunshito on the total area of erosive lesions in esophageal mucosa
On day 10, mucosal erosion was not observed in the esophagus of sham-operated rats, but was obvious in the esophagus of RE model rats treated with vehicle (Fig. 2a). Rikkunshito (0.3 and 0.6% w v−1) did not suppress the average total area of erosive lesions in the esophageal mucosa of RE model rats (Fig. 2b).
Effect of rikkunshito on the average total area of erosive lesions in the esophageal mucosa of each RE model rat. a Mucosal erosion is not seen in the esophagus of a sham-operated rat (a), but it is obvious in the esophagus of an RE model rat on day 10 (b), while treatment with rikkunshito (0.6% w v−1) did not suppress mucosal erosion in the esophagus of an RE model rat (c). Bar 10 mm. b Rikkunshito did not reduce the average total area of erosive lesions in the esophageal mucosa of RE model rats. Results are expressed as the mean ± SE of 18–21 animals
Effect of rikkunshito on voluntary movement of RE model rats
Table 1 shows the amount of voluntary movement on day 10 in sham-operated rats and RE model rats. Treatment of sham-operated rats with rikkunshito (0.6% w v−1) did not result in significantly greater voluntary movement than that observed in sham-operated rats treated with vehicle.
RE model rats treated with vehicle showed significantly less voluntary movement than did sham-operated rats (P < 0.01), and treatment of RE model rats with rikkunshito (0.3% and 0.6% w v−1) resulted in significantly more voluntary movement (P < 0.05) than was observed in RE model rats treated with vehicle.
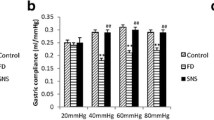
Effect of rikkunshito on intercellular spaces in epithelium from nonerosive areas of esophageal mucosa
On day 10, intercellular spaces in epithelium from esophageal mucosa of sham-operated rats and RE model rats that was free of macroscopically detectable erosive lesions were examined by electron microscopy. The spaces in epithelium from RE model rats treated with vehicle were significantly dilated from the stratum spinosum to the stratum basale compared to the spaces in epithelium from sham-operated rats (P < 0.05). Rikkunshito (0.6% w v−1) significantly suppressed this dilation (P < 0.05) (Fig. 3a, b).
Changes in intercellular spaces in esophageal mucosa of RE model rats, and the effect of rikkunshito on those spaces. a On day 10 after surgery, intercellular spaces of epithelium are dilated in the stratum spinosum or basal area of esophageal mucosa of a RE model rat (Vehicle) compared to those of a sham-operated rat (Sham). Rikkunshito (0.6% w v−1) markedly suppressed such dilation (20,000×). Bar 400 nm. b Intercellular space diameter (ISD) was significantly increased in RE model rats (Vehicle) compared with sham-operated rats (Sham) on day 10, and rikkunshito (0.6% w v−1) significantly suppressed the dilation. Arrows shows intercellular spaces of epithelium. Results are expressed as the mean ± SE of 5 animals. # P < 0.05 versus sham. *P < 0.05 versus vehicle
Effect of rikkunshito on levels of tight junction protein mRNAs in epithelial cells from nonerosive areas of esophageal mucosa
On day 10, esophageal mucosa that was free of macroscopically detectable erosive lesions was collected from sham-operated rats and RE model rats, and levels of tight junction protein mRNAs in the mucosal tissue were measured. The claudin-3 mRNA level was 25% lower in RE model rats treated with vehicle than in sham-operated rats (P < 0.01). Rikkunshito (0.3 and 0.6% w v−1) did not affect the claudin-3 mRNA level (Fig. 4b).
Effect of rikkunshito on levels of claudin-1, -3 and -4 mRNAs in epithelium from the esophageal mucosa of RE model rats. On day 10, the claudin-1 (a) and claudin-4 (c) mRNA levels in epithelium from the esophageal mucosa of RE model rats (Vehicle) were not decreased compared with the levels from sham-operated rats (Sham). b Only the claudin-3 mRNA level was significantly lower in RE model rats (Vehicle) than in sham-operated rats (Sham) on day 10. In the RE model rats, rikkunshito at 0.3 and 0.6% w v−1 did not increase the claudin-3 mRNA level. Results are expressed as the mean ± SE of 8–9 animals. ## P < 0.01 versus sham
Effect of rikkunshito on the levels of tight junction proteins in epithelial cells from nonerosive areas of esophageal mucosa
On day 10, esophageal mucosa that was free of macroscopically detectable erosive lesions was collected from sham-operated rats and RE model rats, and the protein in that tissue was divided into detergent (1% NP-40)-soluble and -insoluble fractions.
Levels of NP-40-soluble claudin-1, -3 and -4 protein were decreased by 25, 30 and 22%, respectively, in RE model rats treated with vehicle compared to sham-operated rats (P < 0.01). Rikkunshito (0.6% w v−1) significantly decreased levels of NP-40-soluble claudin-1, -3 and -4 protein (Fig. 5a–c).
Effect of rikkunshito on levels of claudin-1, -3 and -4 proteins in epithelium from the esophageal mucosa of RE model rats. a The claudin-1 level in the NP-40-soluble fraction was significantly lower in RE model rats (Vehicle) than in sham-operated rats (Sham) on day 10. In RE model rats, rikkushito at 0.6% w v−1 significantly reduced the NP-40-soluble claudin-1 level. b The claudin-3 level in both the NP-40-soluble and -insoluble fractions was significantly lower in RE model rats (Vehicle) than in sham-operated rats (Sham) on day 10. In RE model rats, rikkushito at 0.6% w v−1 significantly reduced the NP-40-soluble claudin-3 level and increased the NP-40-insoluble claudin-3 level. c The claudin-4 level in the NP-40-soluble fraction was significantly lower in RE model rats (Vehicle) than in sham-operated rats (Sham) on day 10. In RE model rats, rikkushito at both 0.3 and 0.6% w v−1 significantly reduced the NP-40-soluble claudin-4 level. Results are expressed as the mean ± SE of 8–9 animals. ## P < 0.01 versus sham. *P < 0.05 and **P < 0.01 versus vehicle
The level of NP-40-insoluble claudin-3 protein was decreased by 36% in RE model rats treated with vehicle compared to sham-operated rats (P < 0.01). Rikkunshito (0.6% w v−1) significantly increased the level of NP-40-insoluble claudin-3 protein (Fig. 5b). Namely, regarding claudin-3, the proportions of the NP-40-insoluble and -soluble fractions were changed, though the total protein level in rikkunshito-treated rats was unchanged compared to that in rats treated with vehicle (data not shown). Levels of NP-40-insoluble claudin-1 and -4 protein did not show a statistically significant difference between RE model rats treated with vehicle and sham-operated rats, but rikkunshito (0.6% w v−1) showed a tendency to increase levels of NP-40-insoluble claudin-1 and -4 proteins (Fig. 4a, c).
Discussion
Rikkunshito is a traditional Japanese medicine that is widely used to treat a variety of gastrointestinal conditions, including indigestion, anorexia, distention, nausea, and vomiting [13–15]. In animal studies, rikkunshito has been shown to promote adaptive gastric relaxation [16], facilitate gastric emptying [17], suppress cisplatin-induced anorexia [18], and favorably affect the selective serotonin reuptake inhibitor-induced gastrointestinal motility reduction model [19]. Recently, rikkunshito has been reported to ameliorate symptoms of patients with GERD and patients with NERD [8, 9, 20], but the mechanism of this effect is not well understood. Therefore, in this study, we investigated the effect of rikkunshito on experimental RE in rats and the mechanism of that effect.
In a previous study, we showed that decreases in voluntary movement may be able to serve as an index of gastrointestinal symptoms in RE model rats [11]. Therefore, in the present study, we first evaluated GERD symptoms in the RE rats by measuring their voluntary movement with an infrared monitoring system. Then, to reconfirm the improvement of symptoms and investigate the mechanism responsible for any such improvement, we investigated the effect of rikkunshito on intercellular spaces and tight junctions in epithelium of esophageal mucosa. Dilation of intercellular spaces in esophageal epithelium is seen in GERD and NERD patients with heartburn [21, 22] and is considered to be a marker of GERD symptoms. Tight junctions are structures that seal neighboring cells together; they have a barrier role and/or regulate permeability to ions. Evidence, including experiments using animals deficient in tight junction proteins and experiments using downregulation caused by acid and oxidative stress, has shown that tight junctions play an important role in supporting the barrier function of the esophagus [23–25].
Increased expression of neurotransmitters in the spinal chord, dorsal root ganglia, and nodose ganglia has been reported in studies using in vivo models of acute and chronic pain [26, 27] and is recognized as an index of pain. Increased expression of substance P was also observed in the rat model of RE, and omeprazole suppressed such increased expression [28]. In the present study, rikkunshito significantly increased voluntary movement in RE model rats. Because omeprazole inhibited decreases in voluntary movement in RE model rats in a previous study [11], and rikkunshito did not affect the voluntary movement of sham-operated rats in the present study, we attributed the increased voluntary movement of the RE model rats treated with rikkunshito in the present study to amelioration of visceral symptoms, including pain, by rikkunshito. In the present study, rikkunshito also suppressed the dilation of intercellular spaces in epithelial cells from nonerosive sites in esophageal mucosa, a finding which suggests that rikkunshito might ameliorate symptoms of GERD. The total area of erosive lesions in esophageal mucosa can serve as an index of damage to the esophagus [29]. In our previous study, the proton pump inhibitor omeprazole reduced this area in RE model rats [11], but in the present study, rikkunshito did not reduce it at all. Furthermore, we have obtained preliminary results indicating that rikkunshito does not inhibit the secretion of gastric acid (data not shown). These results indicate that this drug had no or little effect on acid secretion and/or reflux in this study. This suggests that the effect of rikkunshito on the voluntary movement of RE model rats may have a mechanism that is different from that of proton pump inhibitors.
It has been hypothesized that noxious stimuli, including acid, penetrate deep into esophageal mucosa and cause symptoms by stimulating nociceptive receptors such as TRPV1 [30]. Namely, abnormal barrier function in the mucosal epithelium may cause GERD symptoms [30]. Tight junctions are structures that play a major role in maintaining the barrier function of epithelial cells. The tight junction proteins that actually form the junctions, as well as related proteins, are crucial to the barrier function of epithelial cells, including squamous epithelial cells [23–25]. Decreased levels of the tight junction protein claudin-3 in the esophageal mucosa of RE model rats have been reported [11, 31]. Therefore, in the present study, we examined the effect of rikkunshito on claudins. It has been reported that functional tight junction proteins are insoluble in nonionic detergent [12, 32], and it is generally thought that the claudins in the detergent-insoluble fraction are functionally important. Therefore, in the present study, we divided proteins from esophageal mucosa into nonionic detergent (NP-40)-soluble and -insoluble fractions, and measured the levels of claudin-1, -3 and -4 in each fraction. The level of NP-40-insoluble claudins was decreased in RE model rats compared with sham-operated rats, and rikkunshito inhibited this decrease. In particular, the insoluble claudin-3 protein level was significantly decreased in RE model rats, and rikkunshito significantly inhibited that decrease. We also measured the level of claudin-3 mRNA in esophageal mucosa, and found that it was significantly decreased in RE model rats; rikkunshito, however, had no effect on this decrease. As shown in Fig. 5, both the soluble and the insoluble claudin-3 protein levels were significantly decreased in RE model rats. Addition of rikkunshito (0.6% w v−1) decreased the level of NP-40-soluble claudin-3 but significantly increased the level of NP-40-insoluble claudin-3. Furthermore, as shown in Fig. 4, the level of claudin-3 mRNA in the esophageal mucosa of RE model rats was not affected by this drug. These findings suggest the possibility that rikkunshito may affect the localization of claudins in inflamed tissue. In other words, rikkunshito may improve the barrier function of esophageal mucosa by facilitating the translocation of the tight junction proteins from the soluble to the insoluble fraction, which is thought to be more functional.
Based on the results of the present study, we hypothesize that rikkunshito acts as follows. Exposure of esophageal mucosa to gastric contents causes changes in the levels of tight junction proteins in the mucosa, and those changes impair the barrier function of the mucosa, which leads to reflux-associated symptoms [30]. By promoting the formation of tight junctions mediated by the localization of claudins, rikkunshito improves the barrier function of the esophageal mucosa and prevents the diffusion of gastric acid into the tissues.
Because intercellular spaces in esophageal epithelium are regarded as an index of junctional damage, which relates to GERD symptoms [30], the fact that rikkunshito narrows such spaces supports the view that rikkunshito ameliorates RE symptoms in rats. By decreasing the diffusion of gastric acid through damaged epithelium, rikkunshito may inhibit the activation of transient receptor potential vanilloid receptor 1 (TRPV-1) and other chemosensitive nociceptors [30]. However, the effect of this drug on voluntary movement may possibly be explained by other mechanisms than strengthened barrier function. In fact, our previous study demonstrated that the proton pump inhibitor omeprazole increased the voluntary movement, which may be largely due to a reduced amount of acid reflux [11]. In addition, other pharmacological properties of rikkunshito have been reported, including reducing distal esophageal acid exposure by improving esophageal acid clearance [33, 34], accelerated gastric emptying [34, 35] or promoting adaptive relaxation [34, 36]. These effects of this drug may also help to ameliorate RE symptoms.
Thus, while clinical evidence is still insufficient, rikkunshito shows promise for the alleviation of symptoms of GERD patients. To demonstrate this effect conclusively, well-designed clinical research is needed. Furthermore, rikkunshito is a crude drug that contains 8 herbal ingredients. It is not known which of these herbs—and the compounds in them—are involved in local changes in claudins, or the mechanisms of any such involvement. Such questions should be investigated in future studies.
References
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900–20.
Dimenäs E. Methodological aspects of evaluation of quality of life in upper gastrointestinal diseases. Scand J Gastroenterol Suppl. 1993;119:18–21.
Dimenäs E, Carlsson G, Glise H, Israelsson B, Wiklund I. Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl. 1996;221:8–13.
Venables TL, Newland RD, Patel AC, Hole J, Wilcock C, Turbitt ML. Omeprazole 10 milligrams once daily, omeprazole 20 milligrams once daily, or ranitidine 150 milligrams twice daily, evaluated as initial therapy for the relief of symptoms of gastro-oesophageal reflux disease in general practice. Scand J Gastroenterol. 1997;32:965–73.
Fujiwara Y, Arakawa T. Epidemiology and clinical characteristics of GERD in the Japanese population. J Gastroenterol. 2009;44:518–34.
Dean BB, Gano AD Jr, Knight K, Ofmann JJ, Fass R. Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol. 2004;2:656–64.
Miwa H, Sasaki M, Furuta T, Koike T, Habu Y, Ito M, et al. Efficacy of rabeprazole on heartburn symptom resolution in patients with non-erosive and erosive gastro-oesophageal reflux disease: a multicenter study from Japan. Aliment Pharmacol Ther. 2007;26:69–77.
Koide A, Yamaguchi T, Koyama H, Koyama H, Tsuyuguchi T, Kitahara H, et al. Effect and role of TJ-43: Rikkun-shi-to from the aspects of endoscopic findings and QOL improvement in GERD patients. Gastroenterology. 2005;128:A-530.
Kawahara H, Kubota A, Hasegawa T, Okuyama H, Ueno T, Ida S, et al. Effects of rikkunshito on the clinical symptoms and esophageal acid exposure in children with symptomatic gastroesophageal reflux. Pediatr Surg Int. 2007;23:1001–5.
Omura N, Kashiwagi H, Chen G, Suzuki Y, Yano F, Aoki T. Establishment of surgically induced chronic acid reflux esophagitis in rats. Scand J Gastroenterol. 1999;34:948–53.
Miwa H, Oshima T, Sakurai J, Tomita T, Matsumoto T, Iizuka S, et al. Experimental oesophagitis in the rat is associated with decreased voluntary movement. Neurogastroenterol Motil. 2009;21:296–303.
Sakakibara A, Furuse M, Saitou M, Ando-Akatsuka Y, Tsukita S. Possible involvement of phosphorylation of occludin in tight junction formation. J Cell Biol. 1997;137:1393–401.
Tatsuta M, Iishi H. Effect of treatment with liu-jun-zi-tang (TJ-43) on gastric emptying and gastrointestinal symptoms in dyspeptic patients. Aliment Pharmacol Ther. 1993;7:459–62.
Tomono H, Ito Y, Watanabe T. Successful antiemetic treatment of TSUMURA Rikkunshi-to extract granules for ethical use in addition to other antiemetic agents in neoadjuvant chemotherapy for an advanced breast cancer patient. Jpn J Cancer Chemother. 2006;33:1129–31.
Oka T, Tamagawa Y, Hayashida S, Kaneda Y, Kodama N, Tsuji S. Rikkunshi-to attenuates adverse gastrointestinal symptoms induced by fluvoxamine. Biopsychosoc Med. 2007;15:21–6.
Hayakawa T, Arakawa T, Kase Y, Akiyama S, Ishige A, Takeda S, et al. Liu-Jun-Zi-Tang, a kampo medicine, promotes adaptive relaxation in isolated guinea pig stomachs. Drugs Exp Clin Res. 1999;25:211–8.
Kido T, Nakai Y, Kase Y, Sakakibara I, Nomura M, Takeda S, et al. Effects of rikkunshi-to, a traditional Japanese medicine, on the delay of gastric emptying induced by N(G)-nitro-l-arginine. J Pharmacol Sci. 2005;98:161–7.
Takeda H, Sadakane C, Hattori T, Katsurada T, Ohkawara T, Nagai K, et al. Rikkunshito, an herbal medicine, suppresses cisplatin-induced anorexia in rats via 5-HT2 receptor antagonism. Gastroenterology. 2008;134:2004–13.
Fujitsuka N, Asakawa A, Hayashi M, Sameshima M, Amitani H, Kojima S, et al. Selective serotonin reuptake inhibitors modify physiological gastrointestinal motor activities via 5-HT2c receptor and acyl ghrelin. Biol Psychiatr. 2009;65:748–59.
Hiyama T, Yoshihara M, Tanaka S, Haruma K, Chayama K. Strategy for treatment of nonerosive reflux disease in Asia. World J Gastroenterol. 2008;28:3123–8.
Tobey NA, Carson JL, Alkiek RA, Orlando RC. Dilated intercellular spaces: a morphological feature of acid reflux-damaged human esophageal epithelium. Gastroenterology. 1996;111:1200–5.
Caviglia R, Ribolsi M, Maggiano N, Gabbrielli AM, Emerenziani S, Guarino MP, et al. Dilated intercellular spaces of esophageal epithelium in nonerosive reflux disease patients with physiological esophageal acid exposure. Am J Gastroenterol. 2005;100:543–8.
Furuse M, Hata M, Furuse K, Yoshida Y, Haratake A, Sugitani Y, et al. Claudin-based tight junctions are crucial for the mammalian epithermal barrier: a lesson from claudin-1-deficient mice. J Cell Biol. 2002;156:1099–111.
Okuyama M, Fujiwara Y, Tanigawa T, Watanabe K, Shiba M, Tominaga K, et al. Roles of ZO-1 and epidermal growth factor in esophageal epithelial defense against acid. Digestion. 2007;75:135–41.
Hashimoto K, Oshima T, Tomita T, Kim Y, Matsumoto T, Joh T, et al. Oxidative stress induces gastric epithelial permeability through claudin-3. Biochem Biophys Res Commun. 2008;376:154–7.
Lu CL, Pasricha PJ, Hsieh JC. Changes of the neuropeptides content and gene expression in spinal cord and dorsal root ganglion after noxious colorectal distention. Regul Pept. 2005;131:66–73.
Donaldson LF, Harmar AJ, McQueen DS, Seckl JR. Increased expression of preprotachykinin, calcitonin gene-related peptide, but not vasoactive intestinal peptide messenger RNA in dorsal root ganglia during the development of adjuvant monoarthritis in the rat. Brain Res Mol Brain Res. 1992;16:143–9.
Banerjee B, Meadda BK, Lazarova Z, Bansal N, Shaker R, Sengupta JN. Effect of reflux-induced inflammation on transient receptor potential vanilloid one (TRPV1) expression in primary sensory neurons innervating the oesophagus of rats. Neurogastroenterol Motil. 2007;19:681–91.
Omura N, Kashiwagi H, Chen G, Yano F, Suzuki Y, Aoki T. Effects of ecabet sodium on experimentally induced reflux esophagitis. J Gastroenterol. 2000;35(7):504–9.
Barlow WJ, Orlando RC. The pathogenesis of heartburn in nonerosive reflux disease: a unifying hypothesis. Gastroenterology. 2005;128:771–8.
Asaoka D, Miwa H, Hirai S, Ohkawa A, Kurosawa A, Kawabe M. Altered localization and expression of tight-junction proteins in a rat model with chronic acid reflux esophagitis. J Gastroenterol. 2005;40:781–90.
Stevenson BR, Goodenough DA. Zonulae occludentes in junctional complex—enriched fractions from mouse liver: preliminary morphological and biochemical characterization. J Cell Biol. 1984;98:1209–21.
Kawahara H, Kubota A, Hasegawa T, et al. Effects of rikkunshito on the clinical symptoms and esophageal acid exposure in children with symptomatic gastroesophageal reflux. Pediatr Surg Int. 2007;23(10):1001–5.
Suzuki H, Inadomi JM, Hibi T. Japanese herbal medicine in functional gastrointestinal disorders. Neurogastroenterol Motil. 2009;21(7):688–96.
Kawahara H, Mitani Y, Nomura M, et al. Impact of rikkunshito, an herbal medicine, on delayed gastric emptying in profoundly handicapped patients. Pediatr Surg Int. 2009;25(11):987–90.
Hayakawa T, Arakawa T, Kase Y, et al. Liu-Jun-Zi-Tang, a kampo medicine, promotes adaptive relation in isolated guinea pig stomachs. Drug Exp Clin Res. 1999;25:211–8.
Acknowledgments
We deeply thank Ms. M. Togawa and N. Kamiya for their technical assistance and Y. Okano for her dedicated secretarial assistance.
Conflict of interest statement
H. Miwa is a consultant to AstraZeneca (Japan) Co. Ltd., Takeda Pharmaceutical Co. Ltd., Eisai Co. Ltd., Tsumura & Co., and Dainippon Sumitomo Pharmaceutical Co. Ltd. T. Matsumoto is a consultant to Tanabe-Mitsubishi Pharmaceutical Co. Ltd., Otsuka Pharmaceuticals Co. Ltd., and Ajinomoto Pharma Co. Ltd. J. Koseki, T. Hattori, K. Kubota and S. Iizuka are employees of Tsumura & Co.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miwa, H., Koseki, J., Oshima, T. et al. Rikkunshito, a traditional Japanese medicine, may relieve abdominal symptoms in rats with experimental esophagitis by improving the barrier function of epithelial cells in esophageal mucosa. J Gastroenterol 45, 478–487 (2010). https://doi.org/10.1007/s00535-009-0180-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-009-0180-1