Abstract
Purpose
In patients chronically infected with hepatitis B virus, interferon has been used for the purpose of viral suppression by loss of hepatitis B e antigen (HBeAg) with or without seroconversion to antibody to HBeAg (anti-HBe). However, discussion about the effect of interferon on the development of hepatocellular carcinoma (HCC) has been controversial.
Methods
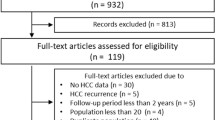
We conducted a meta-analysis of published studies. Eight studies were retrieved (1,303 patients), including two randomized controlled trials (RCTs) and six non-RCTs (553 patients received interferon treatment).
Results
The pooled estimate of the preventive effect of treatment was significantly in favor of interferon (risk difference −5.0%; 95% CI −9.4 to −0.5, P = 0.028). By subgroup analyses, the preventive effect of interferon treatment was shown in the Asian population (risk difference −8.5%; 95%CI −13.6 to −3.6, P = 0.0012), the population with the incidental rate of HCC ≥10% if untreted with interferon (risk difference −9.4%; 95%CI −14.2 to −4.6, P = 0.0001), and the population with the proportion of HBeAg-positive patients to the study population ≥70% (RD −6.0%; 95%CI −11.8 to −0.2, P = 0.043). However, the preventive effect of interferon was not shown in the European population, the population with a lower incidental rate of HCC if untreated with interferon, and the population with the lower proportion of HBeAg-positive patients to the study population. An evaluation using the Begg method indicated no evidence of publication bias.
Conclusions
Interferon treatment is considered to restrain HCC development in patients with chronic hepatitis B virus infection, especially in HBeAg-positive Asians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, more than 350 million people are chronic carriers of the hepatitis B virus (HBV) [1]. The distribution of HBV varies throughout the world. Areas with high prevalence include Southeast Asia, China, and Africa, where approximately 10% of the population are chronic carriers [2]. North America, Western Europe, and Australia have low levels of endemicity. Chronic HBV infection is a leading cause of hepatocellular carcinoma (HCC). A recent study has revealed that half of HCC cases are associated with HBV infection and that worldwide 328,000 people die of HBV-related HCC every year [3]. Patients positive for hepatitis B surface antigen (HBsAg) have been reported to have higher hazard ratios for liver cancer mortality (22.4; 95% CI, 15.2–32.9), and liver cancer mortality ranged from 72.8 per 100,000 persons per year for patients with HBV DNA levels less than 300 copies/ml to 815.6 per 100,000 persons per year for those with HBV DNA levels of 1 million copies/ml or greater [4].
Antiviral treatment with the oral nucleoside analogue lamivudine (LMV) is reported to be effective in reducing HCC risk in Asian patients with advanced chronic hepatitis B [5]. The tolerability and safety of LMV are excellent; however, viral resistance, which is usually followed by loss of the clinical response, the rise of aminotransferase levels, and the worsening of hepatic histology, is related to mutations in the YMDD motif that occurred in 70–80% of patients treated continuously for 4–5 years [6]. Furthermore, concerning long-term LMV treatment, teratogenicity has not been adequately evaluated in humans. In contrast, discussion of the effect of interferon (IFN) on the development of HCC has been controversial. Two randomized controlled trials (RCTs) from Taiwan reported a decrease in the development of HCC among hepatitis B patients who received IFN treatment compared to untreated controls [7, 8]. On the other hand, in 2001, a meta-analysis by Camma and colleagues [9], which included patients with co-infection of HBV and the hepatitis C virus (HCV), reported that IFN did not affect the rate of HCC in HBV-related cirrhosis. IFN prevents the development of HCC in patients with HCV-related cirrhosis [10].
Seroconversion from the hepatitis B e antigen (HBeAg) to antibody to HBeAg (anti-HBe) marks the transition from chronic hepatitis B to the inactive HBsAg carrier state with low or undetectable serum HBV-DNA and normal aminotransferases, and confers a favorable long-term outcome with very low risk of HCC. In 2007, Lin and colleagues [11] reported that IFN-treatment improved the HBeAg seroconversion rate and reduced the development of HCC. Furthermore, after 2001, several studies of the effect of IFN on the development of HCC in patients with chronic HBV infection were reported [11–14]. Thus, we considered the effect of IFN on the development of HCC in patients with chronic HBV infection to be worth investigating by another meta-analysis.
Methods
Literature search
We searched PubMed for the medical literature published by using the following key words: hepatitis B, interferon, and hepatocellular carcinoma. We limited our search to original, English-language articles published between 1 January 1998 and 31 December 2007; earlier studies were excluded because these studies included patients with a positive test for antibody to HCV (anti-HCV). Studies were included if they met all of the following criteria: they consisted of a clinical trial comparing IFN-treated and untreated patients; they excluded patients who had tested positive for anti-HCV or the human immunodeficiency virus; they assessed HCC as an outcome of the treatment’s effect; they had one or more cases with the development of HCC in IFN-untreated patients. However, studies in which HCV-positive patients could be accurately excluded from the study population were included.
Data collection
Two investigators (Y.M., H·K.) trained in hepatology independently reviewed the included studies by using a standardized protocol and data collection form. Discrepancies among reviewers were solved with discussion. We collected data on patient characteristics, study characteristics, IFN treatment, and outcomes. Our primary goal was to investigate the effect of IFN treatment on the development of HCC in patients with chronic HBV infection.
Statistical analysis
Crude rates of HCC were assessed as the only measure of IFN’s potential effect. The evaluation of preventive effectiveness was performed with an intention-to-treat method. In order to combine results from individual studies, we used the crude rate of HCC regardless of when HCC was observed. The risk difference (RD) was calculated for each trial.
In order to obtain an overall measure of the treatment efficacy, we calculated RD and 95% CI for HCC development, according to the DerSimonian and Laird method [15]. Heterogeneity was evaluated by a chi-square test. We considered statistical significance at a P value less than 0.05. When statistically significant heterogeneity of treatment effects was observed, the studies were partitioned (for example, RCTs vs. non-RCTs) to decrease the heterogeneity of studies in a particular partition and increase the differences among the partitions. Subgroup analyses were also performed to evaluate the difference in RD between trials of Europeans and those of Asians, between trials with the rate of HCC in untreated patients below 10% and those above 10%, and between the trials with the rate of HBeAg-positive patients below 70% and those above 70%. We examined publication bias by using the Begg method with funnel plot analysis [16].
Results
Literature searches of PubMed by using the three keywords yielded 347 studies. Of the 347 studies, 336 did not fulfill the inclusion criteria (42 in languages other than English, 5 case reports, 171 review articles, 14 concerning chronic hepatitis C, 88 not concerning the effect of IFN on HCC development, 3 that included HCV-positive patients in which HCV-positive patients could not be accurately excluded from the study population, 6 concerning the second prevention of HBV-related HCC, 4 without untreated patients, and 3 without the development of HCC in IFN-untreated patients). Eleven studies fulfilled the inclusion criteria. However, these 11 studies included 3 studies reported by Lin and colleagues [7, 8, 11] and 2 studies reported by Ikeda and colleagues [17, 18]. One study each [8, 17] was selected from these researchers. Thus, eight studies in total were selected, and included 1,303 patients, 553 of whom received IFN treatment. The main features of the studies evaluated by meta-analysis are shown in Table 1. One study [19] included seven HCV-positive patients, and these seven patients, who did not develop HCC, were excluded from the study population. Among the reviewed studies, 19 and 28 were RCTs, and 6 [12–14, 17, 20, 21] were non-RCTs (NRCTs). All eight studies have been reported as full papers. Three studies [13, 19, 21] were performed in Europe, three [14, 17, 20] in Japan, and one each in Thailand [12] and Taiwan [8]. The sample size of each study varied greatly, ranging from 52 [20] to 404 patients [13]. Variable IFN schedules were used, both for total dose and for length of treatment. IFN was administered in various fixed, variable, and adjusted doses.
The effect of IFN on the development of HCC is shown in Fig. 1. IFN seemingly decreased the incidental rate of HCC in six studies, and a statistically significant decrease was observed in two. The pooled estimate of the preventive effect of treatment was significantly in favor of IFN (RD −5.0%; 95% CI −9.4 to −0.5, P = 0.028) without a significant heterogeneity (χ2 = 10.91, P = 0.14).
A first subgroup analysis was carried out in relation to the ethnic origin of the patients (Europeans vs. Asians). From Asian reports, the pooled estimate of the preventive effect of IFN treatment was significant (RD −8.5%; 95% CI −13.6 to −3.6, P = 0.0012) without a significant heterogeneity (χ2 = 4.47, P = 0.35). On the other hand, from European reports, no preventive effect was shown (RD −0.5%; 95% CI −4.9 to 4.0, P = 0.84) without a significant heterogeneity (χ2 = 0.42, P = 0.81).
A second subgroup analysis was performed in relation to the incidental rate of HCC in untreated patients. In the reports with the incidental rate of HCC ≥10% in untreated patients, the pooled estimate of the preventive effect of IFN treatment was significant (RD −9.4%; 95% CI −14.2 to −4.6, P = 0.0001) without a significant heterogeneity (χ2 = 2.00, P = 0.74). On the other hand, in the reports with the incidental rate of HCC <10% in untreated patients, no preventive effect was shown (RD −0.2%; 95% CI −4.3 to 4.7, P = 0.92) without a significant heterogeneity (χ2 = 0.61, P = 0.74).
A last subgroup analysis was performed in relation to the proportion of HBeAg-positive patients to the study population. In the reports with the proportion of HBeAg-positive patients to the study population ≥70%, the pooled estimate of the preventive effect of IFN treatment was significant (RD −6.0%; 95% CI −11.8 to −0.2, P = 0.043) without a significant heterogeneity (χ2 = 3.43, P = 0.33). On the other hand, in the reports with the proportion of HBeAg-positive patients to the study population <70%, no preventive effect was shown (RD −5.4; 95% CI −15.4 to 4.6, P = 0.29) with a significant heterogeneity (χ2 = 6.74, P = 0.034).
An evaluation using the Begg method suggested no evidence of publication bias visually or statistically (z = 0.99, P = 0.32).
Discussion
In patients with chronic hepatitis B, IFN has been used for the purpose of viral suppression by the loss of HBeAg with or without seroconversion to anti-HBe and a decrease of the serum HBV DNA levels. In patients with HBeAg seroconversion, the intrahepatic HBV-DNA level also decreases largely [22]. In fact, meta-analyses of RCT have shown the benefit of IFN treatment [23–25]. Wong and colleagues [23] reported that, by a meta-analysis, the HBeAg and HBsAg loss rates were 33 versus 12% and 7.8 versus 1.8%, respectively, in patients treated with IFN versus a placebo group. HBeAg seroconversion leads to the improvement of long-term prognosis. For patients with compensated liver cirrhosis, the 5-year survival rates have been reported to be 72% for HBeAg-positive cirrhosis and 97% for HBeAg-negative cirrhosis [26]. Furthermore, the 10-year survival rate is 98% in HBeAg-positive patients treated with IFN compared to 85% in those untreated [8]. The relative risk for HCC has been reported to be 9.6 (95% CI, 6.0–15.2) for men positive for HBsAg alone and 60.2 (95% CI, 35.5–102.1) for men positive for both HBsAg and HBeAg [27]. Hepatic fibrosis improves in patients with HBeAg seroconversion [28]. In this study, the effectiveness of IFN treatment on HCC development was shown in populations mainly including HBeAg-positive patients, but not in populations mainly including HBeAg-negative patients. Thus, IFN treatment is speculated to mainly restrain HCC development through HBeAg seroconversion.
Recently, peginterferon has replaced the use of standard interferon in the treatment of chronic hepatitis B. Peginterferon is superior in efficacy to standard interferon in chronic hepatitis B based on the clearance of HBeAg; however, there are no differences in the frequency and severity of adverse events between the two groups [29, 30]. After 1-year therapy, clearance of HBeAg occurred in 30–36% of patients treated with peginterferon compared to 4–12% of placebo recipients, and the serum HBV DNA levels became undetectable by PCR-based assays in 25% of treated patients [31–35]. Furthermore, peginterferon is effective in approximately one-third of patients who failed to respond to previous standard IFN treatment [36]. Even in patients with advanced fibrosis, peginterferon has been reported to be effective and safe [37]. The introduction of peginterferon is expected to decrease the rate of HCC development even further.
In this study, the incidental rate of HCC in untreated patients was associated with the effectiveness of IFN treatment on HCC development, and four of five studies with the incidental rate of HCC in untreated patients above 10% were performed in Asians. The incidental rate of HCC is higher in Asia than in the United States and Europe [2]. On the other hand, recently, HBV genotypes have been reported to be associated with HCC development. Eight genotypes of A–H have been distinguished. Asian patients are mainly infected with genotypes B and C, while European patients are mainly infected with genotypes A and D [38]. In Asian patients, genotype C is a risk factor for HCC development [39]. Furthermore, the HBV genotype is associated with the response to IFN treatment. Genotype B is associated with a better response to IFN treatment compared with genotype C, whereas patients with genotype D have a lower response rate to IFN treatment compared with genotype A [40–43]. In HBeAg-positive patients, HBsAg clearance by peginterferon treatment is associated with genotype. Patients with genotype A tend to achieve HBsAg clearance most [43]. This study indicates that Asian patients may get a more favorable effect from IFN treatment on HCC development than European patients. The difference in the effect of IFN treatment on HCC development may be associated with HBV genotype.
Does IFN treatment prevent HCC development in HBeAg-negative patients? In this study, standard interferon did not prevent HCC development in HBeAg-negative patients. On the other hand, after 1-year treatment with peginterferon, normalization of serum alanine aminotransferase levels and the lack of detectable HBV DNA occurred in 38 and 63%, respectively, of HBeAg-negative patients [44]. The strong relation between serum HBV DNA levels and HCC development has been reported [45, 46]. Active hepatitis after HBeAg seroconversion is a risk factor for HCC development [47]. Thus, peginterferon treatment may suppress HCC development in HBeAg-negative patients. In order to assess this effect of peginterferon treatment, a study with a longer follow-up period and in a larger study population may be required.
In conclusion, IFN treatment prevented HCC development in patients with chronic hepatitis B infection, especially in Asian patients, patients with the rate of HCC in untreated patients above 10%, and HBeAg-positive patients. However, in this study, associations between a preventive effect of IFN on HCC development and HBV genotypes or serum HBV DNA levels could not be assessed. Furthermore, this meta-analysis included only two RCTs. Further studies are necessary to confirm a preventive effect of IFN on HCC development.
References
World Health Organization. Hepatitis B 2000. http://www.who.int/mediacentre/factsheets/fs204/en/ Accessed 24 Nov 2007.
Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107.
Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529–38.
Iloeje UH, Yang HI, Jen CL, Su J, Wang LY, You SL, et al. Risk and predictors of mortality associated with chronic hepatitis B infection. Clin Gastroenterol Hepatol. 2007;5:921–31.
Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, et al. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004;351:1521–31.
Locarnini S. Molecular virology and the development of resistant mutants: implications for therapy. Semin Liver Dis. 2005;25(Suppl 1):9–19.
Lin SM, Tai DI, Chien RN, Sheen IS, Chu CM, Liaw YF. Comparison of long-term effects of lymphoblastoid interferon alpha and recombinant interferon alpha-2a therapy in patients with chronic hepatitis B. J Viral Hepat. 2004;11:349–57.
Lin SM, Sheen IS, Chien RN, Chu CM, Liaw YF. Long-term beneficial effect of interferon therapy in patients with chronic hepatitis B virus infection. Hepatology. 1999;29:971–5.
Cammà C, Giunta M, Andreone P, Craxì A. Interferon and prevention of hepatocellular carcinoma in viral cirrhosis: an evidence-based approach. J Hepatol. 2001;34:593–602.
Shiratori Y, Ito Y, Yokosuka O, Imazeki F, Nakata R, Tanaka N, et al. Antiviral therapy for cirrhotic hepatitis C: association with reduced hepatocellular carcinoma development and improved survival. Ann Intern Med. 2005;142:105–14.
Lin SM, Yu ML, Lee CM, Chien RN, Sheen IS, Chu CM, et al. Interferon therapy in HBeAg positive chronic hepatitis reduces progression to cirrhosis and hepatocellular carcinoma. J Hepatol. 2007;46:45–52.
Tangkijvanich P, Thong-ngam D, Mahachai V, Kladchareon N, Suwangool P, Kullavanijaya P. Long-term effect of interferon therapy on incidence of cirrhosis and hepatocellular carcinoma in Thai patients with chronic hepatitis B. Southeast Asian J Trop Med Public Health. 2001;32:452–8.
Papatheodoridis GV, Manesis E, Hadziyannis SJ. The long-term outcome of interferon-alpha treated and untreated patients with HBeAg-negative chronic hepatitis B. J Hepatol. 2001;34:306–13.
Mahmood S, Niiyama G, Kamei A, Izumi A, Nakata K, Ikeda H, et al. Influence of viral load and genotype in the progression of hepatitis B-associated liver cirrhosis to hepatocellular carcinoma. Liver Int. 2005;25:220–5.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Ikeda K, Saitoh S, Suzuki Y, Kobayashi M, Tsubota A, Fukuda M, et al. Interferon decreases hepatocellular carcinogenesis in patients with cirrhosis caused by the hepatitis B virus: a pilot study. Cancer. 1998;82:827–35.
Ikeda K, Arase Y, Kobayashi M, Someya T, Hosaka T, Saitoh S, et al. Hepatitis B virus-related hepatocellular carcinogenesis and its prevention. Intervirology. 2005;48:29–38.
Mazzella G, Saracco G, Festi D, Rosina F, Marchetto S, Jaboli F, et al. Long-term results with interferon therapy in chronic type B hepatitis: a prospective randomized trial. Am J Gastroenterol. 1999;94:2246–50.
Fujisawa T, Komatsu H, Inui A, Sogo T, Miyagawa Y, Fujitsuka S, et al. Long-term outcome of chronic hepatitis B in adolescents or young adults in follow-up from childhood. J Pediatr Gastroenterol Nutr. 2000;30:201–6.
International Interferon-alpha Hepatocellular Carcinoma Study Group. Effect of interferon-alpha on progression of cirrhosis to hepatocellular carcinoma: a retrospective cohort study. Lancet. 1998;351:1535–9.
Lu HY, Zhuang LW, Yu YY, Ivan H, Si CW, Zeng Z, et al. Intrahepatic HBV DNA as a predictor of antivirus treatment efficacy in HBeAg-positive chronic hepatitis B patients. World J Gastroenterol. 2007;13:2878–82.
Wong DK, Cheung AM, O’Rourke K, Naylor CD, Detsky AS, Heathcote J. Effect of alpha-interferon treatment in patients with hepatitis B e antigen-positive chronic hepatitis B. A meta-analysis. Ann Intern Med. 1993;119:312–23.
Tinè F, Liberati A, Craxì A, Almasio P, Pagliaro L. Interferon treatment in patients with chronic hepatitis B: a meta-analysis of the published literature. J Hepatol. 1993;18:154–62.
Craxì A, Di Bona D, Cammà C. Interferon-alpha for HBeAg-positive chronic hepatitis B. J Hepatol. 2003;39(Suppl 1):S99–105.
de Jongh FE, Janssen HL, de Man RA, Hop WC, Schalm SW, van Blankenstein M. Survival and prognostic indicators in hepatitis B surface antigen-positive cirrhosis of the liver. Gastroenterology. 1992;103:1630–5.
Yang HI, Lu SN, Liaw YF, You SL, Sun CA, Wang LY, et al. Hepatitis B e antigen and the risk of hepatocellular carcinoma. N Engl J Med. 2002;347:168–74.
Hui CK, Leung N, Shek TW, Yao H, Lee WK, Lai JY, et al. Sustained disease remission after spontaneous HBeAg seroconversion is associated with reduction in fibrosis progression in chronic hepatitis B Chinese patients. Hepatology. 2007;46:690–8.
Cooksley WG, Piratvisuth T, Lee SD, Mahachai V, Chao YC, Tanwandee T, et al. Peginterferon alpha-2a (40 kDa): an advance in the treatment of hepatitis B e antigen-positive chronic hepatitis B. J Viral Hepat. 2003;10:298–305.
Zhao H, Kurbanov F, Wan MB, Yin YK, Niu JQ, Hou JL, et al. Genotype B and younger patient age associated with better response to low-dose therapy: a trial with pegylated/nonpegylated interferon-alpha-2b for hepatitis B e antigen-positive patients with chronic hepatitis B in China. Clin Infect Dis. 2007;44:541–8.
Lau GK, Piratvisuth T, Luo KX, Marcellin P, Thongsawat S, Cooksley G, et al. Peginterferon Alfa-2a, lamivudine, and the combination for HBeAg-positive chronic hepatitis B. N Engl J Med. 2005;352:2682–95.
Lim SG, Ng TM, Kung N, Krastev Z, Volfova M, Husa P, et al. A double-blind placebo-controlled study of emtricitabine in chronic hepatitis B. Arch Intern Med. 2006;166:49–56.
Marcellin P, Chang TT, Lim SG, Tong MJ, Sievert W, Shiffman ML, et al. Adefovir dipivoxil for the treatment of hepatitis B e antigen-positive chronic hepatitis B. N Engl J Med. 2003;348:808–16.
Dienstag JL, Schiff ER, Wright TL, Perrillo RP, Hann HW, Goodman Z, et al. Lamivudine as initial treatment for chronic hepatitis B in the United States. N Engl J Med. 1999;341:1256–63.
Lai CL, Chien RN, Leung NW, Chang TT, Guan R, Tai DI, et al. A one-year trial of lamivudine for chronic hepatitis B. Asia Hepatitis Lamivudine Study Group. N Engl J Med. 1998;339:61–8.
Flink HJ, Hansen BE, Heathcote EJ, Feinman SV, Simsek H, Karayalcin S, et al. Successful treatment with peginterferon alfa-2b of HBeAg-positive HBV non-responders to standard interferon or lamivudine. Am J Gastroenterol. 2006;101:2523–9.
Buster EH, Hansen BE, Buti M, Delwaide J, Niederau C, Michielsen PP, et al. Peginterferon alpha-2b is safe and effective in HBeAg-positive chronic hepatitis B patients with advanced fibrosis. Hepatology. 2007;46:388–94.
Schaefer S. Hepatitis B virus: significance of genotypes. J Viral Hepat. 2005;12:111–24.
Chan HL, Hui AY, Wong ML, Tse AM, Hung LC, Wong VW, et al. Genotype C hepatitis B virus infection is associated with an increased risk of hepatocellular carcinoma. Gut. 2004;53:1494–8.
Wai CT, Chu CJ, Hussain M, Lok AS. HBV genotype B is associated with better response to interferon therapy in HBeAg(+) chronic hepatitis than genotype C. Hepatology. 2002;36:1425–30.
Hou J, Schilling R, Janssen HL, Hansen BE, Heijtink R, Sablon E, et al. Genetic characteristics of hepatitis B virus genotypes as a factor for interferon-induced HBeAg clearance. J Med Virol. 2007;79:1055–63.
Bonino F, Marcellin P, Lau GK, Hadziyannis S, Jin R, Piratvisuth T, et al. Predicting response to peginterferon alpha-2a, lamivudine and the two combined for HBeAg-negative chronic hepatitis B. Gut. 2007;56:699–705.
Flink HJ, van Zonneveld M, Hansen BE, de Man RA, Schalm SW, Janssen HL, et al. Treatment with peg-interferon alpha-2b for HBeAg-positive chronic hepatitis B: HBsAg loss is associated with HBV genotype. Am J Gastroenterol. 2006;101:297–303.
Marcellin P, Lau GK, Bonino F, Farci P, Hadziyannis S, Jin R, et al. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2004;351:1206–17.
Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73.
Yu MW, Yeh SH, Chen PJ, Liaw YF, Lin CL, Liu CJ, et al. Hepatitis B virus genotype and DNA level and hepatocellular carcinoma: a prospective study in men. J Natl Cancer Inst. 2005;97:265–72.
Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, et al. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002;35:1522–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyake, Y., Kobashi, H. & Yamamoto, K. Meta-analysis: the effect of interferon on development of hepatocellular carcinoma in patients with chronic hepatitis B virus infection. J Gastroenterol 44, 470–475 (2009). https://doi.org/10.1007/s00535-009-0024-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00535-009-0024-z