Abstract
Background
Because the biopsy specimen of extrahepatic bile duct carcinoma (EHBDC) is small and shows reactive changes, the histological distinction between malignant and benign tissue can be difficult. Recent studies reported that S100P and insulin-like growth factor II mRNA-binding protein 3 (IMP3) were not only diagnostic molecules but also prognostic biomarkers in several organs. The objective of this study is to clarify the diagnostic and prognostic value of immunohistochemical expression of S100P and IMP3 in transpapillary biliary forceps biopsy (TBFB) samples.
Methods
The TBFB samples were collected from 80 patients (EHBDC, 68 patients; benign, 12 patients), retrospectively.
Results
When using cytoplasmic-positive staining for IMP3 as a marker of malignancy, the sensitivity and specificity reached 79.4 and 91.7 %, respectively. The sensitivity, specificity and accuracy achieved 89.7, 91.7 and 90.0 %, respectively, when using positive staining for IMP3 and/or positive histology as a maker of malignancy. While univariate (P = 0.033) and multivariate (P = 0.039) analysis revealed that S100P-positive EHBDC patients showed significantly shorter survival.
Conclusions
The results of this study suggest that immunohistochemical staining for IMP3 is useful in the diagnosis of EHBDC and that of S100P is useful as a prognostic marker for EHBDC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because surgical therapy of extrahepatic bile duct carcinoma (EHBDC) is invasive (i.e., extended hepatectomy and/or pancreatoduodenectomy) [1–4], preoperative confirmation of the malignant diagnosis is important. Although the usefulness of transpapillary biliary forceps biopsy (TBFB) in the diagnosis of biliary strictures has been reported [5–7], the sensitivity of detection of malignancy ranges from 43 to 81 % [8, 9]. This variability indicates that there are false negatives in more than 20 % of biopsied patients. The false negatives occur because biliary tissue samples, gained via forceps biopsy, are small, show crush artifacts and can show reactive changes, particularly following biliary stent placement. Therefore, immunohistochemical markers that differentiate between benign and malignant tissue would be beneficial.
S100P protein is a small isoform of the S100 protein family that is present in human placenta [10]. Insulin-like growth factor II mRNA-binding protein 3 (IMP3) is an oncofetal protein. IMP3 is a member of the IMP family, which comprises IMP1, IMP2, and IMP3 [11]. Overexpression of S100P or IMP3 has been detected in several tumors, including those of the bile duct [12–15]. It has been reported that immunohistochemical staining for S100P and IMP3 differentiates between benign and malignant processes in different organs [12–21]. Furthermore, in surgically resected samples, S100P expression correlates with patient prognosis in intrahepatic cholangiocarcinoma [12] and IMP3 expression correlates with patient prognosis in bile duct carcinoma [15]. If the prediction of prognosis is possible using preoperative biopsy samples without the requirement for surgically resected samples, it will greatly impact the clinical setting.
Thus, we studied retrospectively the diagnostic and prognostic value of S100P and IMP3 expression in tissues obtained by TBFB of patients with suspected EHBDC.
Methods
Tissue samples
Forceps biopsy samples were collected from 80 patients who underwent diagnostic endoscopic retrograde cholangiography and TBFB for biliary stricture or irregularities of the bile duct wall and were ultimately diagnosed with EHBDC or benign biliary stricture during the period of April 2005–March 2010 at Nagoya University Hospital [5, 22]. The ages of the patients ranged from 29 to 88 years (median, 67 years). Fifty-five patients were male, and 25 were female. The final diagnosis was based on the surgical specimen or was made after more than 12 months of follow-up. Sixty-eight patients were ultimately diagnosed with EHBDC (33 patients with perihilar bile duct carcinoma and 35 patients with distal bile duct carcinoma), and 12 patients were ultimately diagnosed with benign biliary stricture [primary sclerosing cholangitis (PSC), 5 patients; IgG4 related cholangitis, 2 patients; and inflammatory change, 5 patients). A pancreatoduodenectomy, a hemihepatectomy, or a more extended resection was performed in 55/68 bile duct carcinoma patients, and the remaining 13 patients underwent either laparotomy alone or palliative surgery due to peritoneal dissemination, liver metastasis and/or periaortic lymph node metastasis, which were detected during the laparotomy.
The clinical and pathological findings of EHBDC were classified based on the American Joint Committee on Cancer (AJCC) cancer staging manual [23]. Based on the previous study [24], the gross tumor type was assessed as papillary, nodular or diffusely infiltrating. This study was approved by the Institutional Review Board at Nagoya University Hospital.
Immunohistochemical staining and evaluation
Immunohistochemical staining for IMP3 and S100P was performed using 4-μm-thick formalin-fixed, paraffin-embedded tissue sections, as previously described [14, 19, 20]. In brief, the tissue sections were deparaffinized and then incubated in 0.3 % H2O2/methanol for 20 min at room temperature to block endogenous peroxidase activity. Antigen retrieval for IMP3 was performed by heating samples in a microwave oven for 10 min in 0.01 mol/L citrate buffer, pH 9.0, and was performed for S100P by incubating samples with proteinase K for 10 min at room temperature. The tissue sections were then incubated with a mouse monoclonal antibody specific for IMP3 (Clone 69.1; Dako; dilution 1:100) and S100P (Clone 16; BD Biosciences Pharmingen; dilution 1:100) for 1 h at room temperature and then incubated with biotinylated secondary antibodies, followed by incubation with ABC complex (Vectastain Elite ABC kit: Vector laboratories Inc., Burlingame, CA, USA). Staining was visualized using diaminobenzidine, and sections were counterstained with hematoxylin.
All hematoxylin and eosin slides were independently reviewed by two observers (T.T. and Y.S.) to verify the diagnoses of forceps biopsy tissue samples, which were based on criteria described by the World Health Organization [25]. Samples showing significant discrepancy in interpretations were resolved by a rereview by two observers. In general, an immunostain was considered positive if 1 % or more of the cells of interest exhibited immunoreactivity. Positive stains were graded as weak, intermediate or strong for staining intensity; focal if 1–50 % of the cells stained; and diffuse if more than 50 % of the cells were positively stained. Cytoplasmic staining was considered positive for IMP3. Nuclear or nuclear/cytoplasmic staining was considered positive for S100P, but if only cytoplasmic staining was detected, the sample was considered negative.
Statistical analysis
Statistical analyses were performed using IBM SPSS, version 19 (Chicago, IL, USA). Statistical analyses of group differences were performed using the Chi-squared test, the Fisher exact test or the Mann–Whitney U test. The Kaplan–Meier method was used for univariate survival analysis, and a comparison was made based on the log-rank test. Multivariate analyses were calculated based on the Cox’s proportional hazards model. P < 0.05 was considered to be statistically significant.
Results
S100P and IMP3 expression in samples of transpapillary biliary forceps biopsies
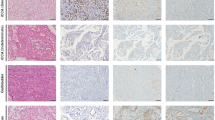
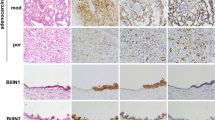
Nuclear or nuclear/cytoplasmic immunostaining for S100P was detected in 52 (76.5 %) of 68 biopsy samples of patients who were ultimately diagnosed with malignant tumors (Fig. 1), and in 6 (50 %) of 12 samples of patients diagnosed with benign tumors (Table 1). When using positive immunochemical staining for S100P as indicative of EHBDC, the sensitivity and specificity were 76.5 and 50.0 %, respectively (Table 3).
S100P and IMP3 expression in transpapillary biliary forceps biopsy samples. a Focal and intermediate nuclear/cytoplasmic staining for S100P observed in extrahepatic bile duct carcinoma (EHBDC) (original magnification 200×). b Diffuse and strong nuclear/cytoplasmic staining for S100P observed in EHBDC (original magnification 100×). c Focal and intermediate nuclear/cytoplasmic staining for S100P observed in benign biliary stricture (IgG4 related cholangitis, original magnification 400×). d Focal and weak cytoplasmic staining for IMP3 observed in EHBDC (original magnification 200×). e Diffuse and weak cytoplasmic staining for IMP3 observed in EHBDC (original magnification 200×). f Focal and strong cytoplasmic staining for IMP3 observed in EHBDC (original magnification 200×). g Diffuse and strong cytoplasmic staining for IMP3 observed in EHBDC (original magnification 200×)
Cytoplasmic immunostaining for IMP3 was detected in 54 (79.4 %) of 68 biopsy samples of patients who were ultimately diagnosed with malignancies (Fig. 1), and it was detected in only 1 (8.3 %) of 12 samples of patients diagnosed with benign strictures (Table 2). This benign patient was ultimately diagnosed with PSC, and IMP3 expression in the biopsy from this patient was only focal and weak. When using positive immunochemical staining for IMP3 as indicative of EHBDC, the sensitivity and specificity reached 79.4 and 91.7 %, respectively. Moreover, the sensitivity, specificity and accuracy reached 89.7, 91.7 and 90.0 %, respectively, when positive histology and/or positive immunochemical staining for IMP3 was used to indicate EHBDC (Table 3).
S100P and IMP3 expression and clinicopathologic correlations in EHBDC
Of the 68 patients who were ultimately diagnosed with malignant strictures, S100P expression was significantly lower in patients with papillary growth type (P = 0.024). There was no statistically significant association between S100P or IMP3 expression and any of the other clinical characteristics (Table 4).
Of the 55 EHBDC patients who underwent surgical resection, although IMP3 expression was significantly lower in females (P = 0.024), there was no statistically significant association between S100P or IMP3 expression and any other clinical or pathological characteristic.
S100P and IMP3 expression and outcomes in EHBDC patients who underwent surgical resection
The survival of the 55 patients who underwent surgical resection was evaluated over a mean period of 865 days. In univariate and multivariate analyses, the EHBDC patients from the S100P-positive expression group showed significantly shorter survival times than those in the S100P-negative expression group. There was no significant association between IMP3 expression and survival. Of the other clinicopathologic factors, the EHBDC patients who underwent R1 operations showed significantly shorter survival times than patients who underwent R0 operations. And T3- and 4-pathological-grade patients showed significantly shorter survival times than patients carrying T1- and 2-grade patients. There was no significant association between any other clinical or pathological characteristic and patient survival (Table 5).
Discussion
Recent studies have reported the diagnostic value of immunohistochemical staining for S100P and IMP3 using tissue samples obtained from endoscopic transpapillary bile duct biopsy. Levy et al. [14] reported that a combination of immunohistochemical staining for S100P, von Hipple–Lindau gene product and IMP3 were useful in the diagnosis of cholangiocarcinoma. Furthermore, Hamada et al. [13] reported that a combination of S100P immunohistochemical staining and conventional histology improved diagnostic sensitivity. In this study, S100P staining provided high sensitivity (76.5 %), but the specificity was low (50.0 %) due to many false-positive samples. Focal S100P-positive staining has been detected in normal intrahepatic bile duct [19]. In this study, focal expression of S100P was detected in 5/12 (41.7 %) of the extrahepatic bile duct samples that were ultimately diagnosed as benign and 17/68 (25.0 %) of the samples ultimately diagnosed as malignant. Because false positive results should be avoided as much as possible in the clinical setting, S100P immunohistochemical staining is not useful for the diagnosis of EHBDC. In contrast, IMP3 immunohistochemical staining showed high sensitivity and specificity (79.4 and 91.7 %, respectively). However, there were 7 (14.3 %) IMP3-negative samples in 49 histologically positive samples. These results suggested that the combination of IMP3 immunohistochemistry with conventional histology was straightforward and that it was the most useful test for the diagnosis of EHBDC when using TBFB samples. This result could contribute to the preoperative examination of bile duct strictures.
The reason underlying the significant association between IMP3 expression and gender in EHBDC patients was unclear.
There was a significant association between S100P expression and the outcome of EHBDC patients who underwent surgical resection in this study. In addition to T factor and residual-tumor factor, the multivariate analysis revealed that S100P expression was a significant independent prognostic factor. It was reported that peripheral intrahepatic cholangiocarcinoma with positive S100P showed poorer prognosis after surgery than those with negative S100P [12]. Because there was no significant difference between S100P expression and clinicopathologic features in patients who underwent surgical resection in this study, the reason why S100P-positive EHBDC patients showed poorer prognosis remained unclear. The molecular studies which investigate the correlation between S100P expression and outcome of EHBDC patients are required. But of the 68 patients who were ultimately diagnosed with malignant strictures, S100P expression was significant lower in patients with papillary growth type in this study. Papillary growth type EHBDC has been reported to show unique features, such as a tendency to result in percutaneous transhepatic biliary drainage catheter tract recurrence [26], and to spread superficially [24] when compared with other types of EHBDC. Typical papillary type EHBDC was thought not to be invasive. These features of papillary type EHBDC may contribute to the significant association between S100P expression and patient outcome.
In conclusion, the results of this study suggest that IMP3 immunohistochemical staining is useful for the diagnosis of EHBDC, and S100P immunohistochemical staining is useful as a prognostic marker for EHBDC even in a small endoscopic transpapillary biopsy sample.
This study is limited by its design because it is a single-center based retrospective study. Further confirmation of the usefulness of S100P and IMP3 immunohistochemical staining is required.
References
Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 2012;256:297–305.
Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer surgical outcome and long-term follow-up. Ann Surg. 2006;243:364–72.
Nagino M, Nimura Y, Nishio H, Ebata T, Igami T, Matsushita M, et al. Hepatectomy with simultaneous resection of the portal vein and hepatic artery for advanced perihilar cholangiocarcinoma. Ann Surg. 2010;252:115–23.
Natsume S, Ebata T, Yokoyama Y, Igami T, Sugawara G, Shimoyama Y, et al. Clinical significance of left trisectionectomy for perihilar cholangiocarcinoma: an appraisal and complication with left hepatectomy. Ann Surg. 2012;255:754–62.
Kawashima H, Itoh A, Ohno E, Goto H, Hirooka Y. Transpapillary biliary forceps biopsy to distinguish benign biliary stricture from malignancy: how many tissue samples should be obtained? Dig Endosc. 2012;24:s22–7.
Sugiyama M, Atomi T, Wada N, Kuroda A, Muto T. Endoscopic transpapillary bile duct biopsy without sphincterotomy for diagnosis biliary strictures: a prospective comparative study with bile brush cytology. Am J Gastroenterol. 1996;91:465–7.
Tamada K, Tomiyama T, Wada S, Ohashi A, Satoh Y, Ido K, et al. Endoscopic transpapillary bile duct biopsy with the combination of intraductal ultrasonography in the diagnosis of biliary strictures. Gut. 2002;50:326–31.
De Bellis M, Sherman S, Fogel EL, Cramer H, Chappo J, McHenry L Jr, et al. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 1). Gastrointest Endosc. 2002;56:552–61.
De Bellis M, Sherman S, Fogel EL, Cramer H, Chappo J, McHenry L Jr, et al. Tissue sampling at ERCP in suspected malignant biliary strictures (Part 2). Gastrointest Endosc. 2002;56:720–30.
Becker T, Gerke V, Kube E, Weber K. S100P, a novel Ca(2+)-binding protein from human placenta. cDNA cloning, recombinant protein expression and Ca2+ binding properties. Eur J Biochem. 1992;207:541–7.
Nielsen J, Christiansen J, Lykke-Andersen J, Johnsen AH, Wewer UM, Nielsen FC. A family of insulin-like growth factor II mRNA-binding proteins represses translation in late development. Mol Cell Biol. 1999;19:1262–70.
Aishima S, Fujita N, Mano Y, Kubo Y, Tanaka Y, Taketomi A. Different roles of S100P overexpression in intrahepatic cholangiocarcinoma: carcinogenesis of perihilar type and aggressive behavior of peripheral type. Am J Surg Pathol. 2011;35:590–8.
Hamada S, Satoh K, Hirota M, Kanno A, Ishida K, Umino J, et al. Calcium-binding protein S100P is a novel diagnostic marker of cholangiocarcinoma. Cancer Sci. 2011;102:150–6.
Levy M, Lin F, Xu H, Dhall D, Spaulding BO, Wang HL. S100P, von Hipple-Lindau gene product, and IMP3 serve as a useful immunohistochemical panel in the diagnosis of adenocarcinoma on endoscopic bile duct biopsy. Hum Pathol. 2010;41:1210–9.
Reiner MO, Frizsche FR, Clavien PA, Pestalozzi BC, Probst-Hensch N, Jochum W. IMP3 expression in lesions of the biliary tract: a marker for high-grade dysplasia and an independent prognostic factor in bile duct carcinomas. Hum Pathol. 2009;40:1377–87.
Dowen SE, Crnogorac-Jurcevic T, Gangeswaran R, Hansen M, Eloranta JJ, Bhakta V, et al. Expression of S100P and its novel binding partner S100PBPR in early pancreatic cancer. Am J Pathol. 2005;166:81–92.
Hashimoto K, Yamamoto H, Shiratsuchi H, Nakashima T, Tamiya S, Higaki Y, et al. S100P expression in ductal type of carcinoma ex pleomorphic adenoma. Am J Surg Pathol. 2011;35:346–55.
Li C, Rock KL, Woda BA, Jiang Z, Fraire AE, Dresser K. Expression of a novel biomarker for adenocarcinoma in situ of the uterine cervix: an immunohistochemical study in comparison with p16(INK4a) expression. Mod Pathol. 2007;20:242–7.
Lin F, Shi J, Liu H, Hull ME, Dupree W, Prichard JW, et al. Diagnostic utility of S100P and von Hippel-Lindau gene product (pVHL) in pancreatic adenocarcinoma-with implication of their roles in early tumorigenesis. Am J Surg Pathol. 2008;32:78–91.
Pryor JG, Bourne PA, Yang Q, Spaulding BO, Scott GA, Xu H. IMP-3 is a novel progression marker in malignant melanoma. Mod Pathol. 2008;21:431–7.
Yantiss RK, Woda BA, Fanger GR, Kalos M, Whalen GF, Tada H, et al. KOC (K homology domain containing protein overexpressed in cancer): a novel molecular marker that distinguishes between benign and malignant lesions of the pancreas. Am J Surg Pathol. 2005;29:188–95.
Kawashima H, Itoh A, Ohno E, Itoh Y, Ebata T, Nagino M, et al. Preoperative endoscopic nasobiliary drainage in 164 consecutive patients with suspected perihilar cholangiocarcinoma—a retrospective study of efficacy and risk factors related to complications. Ann Surg (in press).
Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A 3rd. AJCC cancer staging manual. 7th ed. Berlin: Springer; 2010.
Sakamoto E, Nimura Y, Hayakawa N, Kamiya J, Kondo S, Nagino M, et al. The pattern of infiltration at the proximal border of hilar bile duct carcinoma. A histologic analysis of 62 resected cases. Ann Surg. 1998;227:405–11.
Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. Lyon: IARC; 2010.
Takahashi Y, Nagino M, Nishio H, Ebata T, Igami T, Nimura Y. Percutaneous transhepatic biliary drainage catheter tract recurrence in cholangiocarcinoma. Br J Surg. 2010;97:1860–6.
Acknowledgments
This work was supported by Grant-in Aid for Young Scientists (B) 22790525 from the Ministry of Education, Culture, Sports, Science and Technology of Japan. Additionally, the authors wish to thank Yuya Itoh, MD, Yosuke Nakamura, MD, Takeshi Hiramatsu, MD, Hiroyuki Sugimoto, MD, Hajime Sumi, MD and Daijuro Hayashi, MD for their contributions.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kawashima, H., Itoh, A., Ohno, E. et al. Diagnostic and prognostic value of immunohistochemical expression of S100P and IMP3 in transpapillary biliary forceps biopsy samples of extrahepatic bile duct carcinoma. J Hepatobiliary Pancreat Sci 20, 441–447 (2013). https://doi.org/10.1007/s00534-012-0581-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-012-0581-z