Abstract
Objectives
To examine the survival of patients with spontaneous ruptured hepatocellular carcinoma treated with transarterial embolization (TAE).
Methods and materials
Patients diagnosed with spontaneous ruptured hepatocellular carcinoma treated with TAE were retrospectively studied. Hospital records were reviewed and data were collected and analyzed from the years 2000–2006. A total of 62 patients who had been diagnosed with spontaneous ruptured hepatocellular carcinoma were managed in our hospital during this period.
Results
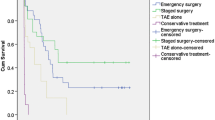
All 62 patients (who had been diagnosed with ruptured hepatocellular carcinoma and were managed in our hospital) patients were treated with TAE, with a success rate of 91% (57/62). Early mortality (within 30 days after rupture) was 38%. Factors that were associated with early mortality were old age, low hemoglobin at presentation, elevated bilirubin at presentation, prolonged prothrombin time at presentation (INR > 1.3), low albumin level at presentation, and unsuccessful embolization. A low albumin level was the only independent risk factor for early mortality. The overall median survival time was 39 days. Surgical resections were possible in seven patients. Their cumulative survival was significantly longer (P = 0.002) than that of patients managed with non-operative treatment after embolization.
Conclusion
Transarterial embolization (TAE) can achieve good hemostasis, though low albumin level, which reflects poor liver reserve, may predict early mortality. Portal vein thrombosis should not be regarded as an absolute contraindication for TAE. Staged surgical resection after embolization is safe and produces a good survival outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most common primary hepatic tumor and one of the most common cancers worldwide. The incidence of spontaneous rupture of HCC reported in the literature varies from 5 to 26% [1–4]. The benefits of transarterial embolization (TAE) therapy in the treatment of patients with ruptured HCC has been demonstrated in earlier studies; this therapy allows us to control bleeding and the selection of suitable patients for later liver resection [5].
Materials and methods
This is a retrospective review of patients with spontaneous rupture of HCC treated with TAE during the period of 2000–2006 in our hospital. The aim of this study is to examine the survival of patients with spontaneous ruptured HCC who were treated with TAE. The definition of “spontaneous” is without a history of recent procedure or trauma. Diagnosis was established or suspected using contrast computed tomography of the abdomen and/or on clinical grounds (such as positive paracentesis in patients with a known history of HCC). All patients admitted to our hospital with a diagnosis of spontaneous ruptured HCC that was either confirmed or suspected underwent TAE performed by an interventional radiologist. The only contraindication in this study is poor liver reserve defined by a Child class C score of 12 or above (according to Child-Pugh classification of chronic liver disease); conservative management was adopted for these patients. Patients who were diagnosed during a laparotomy were also excluded (only one patient was diagnosed with ruptured HCC during a laparotomy for peritonitis during this period). During this period, 62 patients diagnosed with of spontaneous ruptured HCC who were treated with TAE were included in this study. Eighteen percent (11/62) of the patients had a history of HCC.
A successful embolization was defined as an angiographically completed procedure without any sign of bleeding and with a clinical stabilization of hemodynamic conditions and hemoglobin levels without further transfusion involving more than two units of blood within 48 hours. Rebleeding was defined as a sign of bleeding (an unstable hemodynamic condition with a persistent, unexplained drop in hemoglobin levels) that occurred within 48 hours after the initial successful embolization.
Transarterial embolization was carried out in a well-equipped interventional radiological suite by a team of experienced interventional radiologists. A right femoral approach was usual taken, using a 5 Fr catheter through a 5 Fr arterial sheath.
The hepatic arteries were catheterized, usually from the celiac axis or the superior mesenteric artery. A coaxial microcatheter was used if needed. Gelfoam was injected into the right or left hepatic artery, sometimes both, depending on the likely site of rupture. Gelfoam was preferred in our study because the arteries would still be amenable to recanulation for future chemoembolization. The Gelfoam pad was cut into 1 mm cubes, then plunged between two 10 cc syringes and made into Gelfoam slurry. Gelfoam was then injected through the catheter till there is stasis of blood flow in the target artery.
Clinical and laboratory data were collected from hospital records or the computer system and analyzed. Clinical outcomes including 7-day, 30-day, and in-hospital mortality, and overall survival were reviewed. Factors associated with 30-day mortality were also examined.
Statistical analysis was performed by Chi-square test to compare discrete variables. The Student’s t test was used to compare continuous variables. Multivariate analysis was performed with a logistic regression model, and survival analysis was estimated by the Kaplan–Meier survival method. Statistical analysis was performed with the help of SPSS software version 10.0 for Windows (SPSS, Inc., Chicago, IL). A P-value of less than 0.05 was considered to be statistically significant.
Results
Of these 62 patients, there were 9 females and 53 males, with a mean and median age of 63 years and 64 years, respectively (age range 32–91 years). Abdominal pain was the common presentation. Shock (defined as systolic blood pressure <100 mmHg and pulse rate >110 b.p.m.) was present in 27% (17/62) of patients. All patients were treated with TAE, with a success rate of 91% (57/62). In this study, 7-day and 30-day mortality were 26 and 38%, respectively. In-hospital mortality was 45%. Clinical and tumor characteristics and laboratory data were compared between patients with or without early mortality (<30 days), as described in Table 1. Three patients died within 24 hours after successful embolization, with the likely cause of death being cardiac-related and with no clinical evidence of rebleeding. Two patients developed rebleeding and both died within seven days. Five patients had unsuccessful embolizations, two due to a failure to catheterize the bleeding artery because of spasm and anatomical variation, and three who had clinically ongoing bleeding defined by hemodynamic instability, a persistent need for transfusion and a significant drop in hemoglobin levels within the first 48 hours after the procedure with no other source of bleeding found. The overall median survival was 39 days.
In our study, factors that were associated with early (30 days) mortality included old age, low hemoglobin level at presentation, elevated bilirubin level at presentation, prolonged prothrombin time (International Normalized Ratio > 1.3) at presentation, low albumin level at presentation and unsuccessful embolization. The presence of portal vein thrombosis was not associated with early mortality. In multivariate analysis by binary logistic regression model likelihood ratio (LR) method, albumin level was the only independent predictive factor for early (30 days) mortality (P = 0.001; odds ratio 0.864, 95% CI 0.795–0.940) (Table 2).
After embolization, seven patients (11%) had a staged hepatectomy performed after initial embolization. Eight patients received further transarterial chemoembolization (TACE) as palliation. The rest were managed conservatively. No local ablative therapy, such as radiofrequency ablation or alcohol injection, was performed.
Discussion
Spontaneous ruptured HCC is an uncommon but lethal complication with an occurrence of approximately 15% in Asia [6]. The efficacy of TAE has been demonstrated in previous studies since the mid 1980s [5, 7, 8], and it has become a popular treatment option. After diagnosis with an ultrasound or CT scan, TAE can be performed within a few hours. The success rate for hemostasis ranges from 0 to 36.4% [9–11]. In this study, the success rate was 91% and the rebleeding rate was 3%. The relatively high success rate may be explained by the following reasons: Almost every patient has a contrast CT before embolization, so the lesion that bled was identified. Selective or superselective catheterization of the relevant hepatic artery is then accurately performed with information obtained from CT. Apart from increasing the efficacy of the embolization itself, this may also help to reduce the chance of liver failure after embolization. Embolization was performed with gelfoam slurry until complete stasis was achieved, and most importantly, an angiogram was then performed to confirm the successful result. Last but not the least, all procedures were performed by a team of dedicated interventional radiologists.
Previous reports demonstrated that emergency hepatic resection for ruptured HCC could achieve hemostasis and long-term survival [12–14] and suggested that one-stage surgical operation was a treatment modality for selected patients whose lesions were located peripherally, who were stable hemodynamically, and who had reasonable liver function (Child-Pugh A or B). However, one-stage emergency liver resection resulted in an in-hospital mortality of 16.5 to 100% [15]. This poor outcome is due to the tumor stage and the liver functional reserve being unclear. Furthermore, hemorrhagic shock renders the liver function weaker than usual. The presence of coagulopathy in a patient with compromised liver function further increases the risk. When compared with one-stage emergency liver resection, staged liver resection has a much lower in-hospital mortality rate (0–9%) and a better survival rate: 1-year survival rate, 54.2–100%; 3-year survival rate, 21.2–48%; and 5-year survival rate, 15–21.2%) [15]. Other alternatives have been described in small studies or case reports, including alcohol injection [16], the use of radiofrequency ablation [17], or the use of new chemicals such as OK-432 [18], with some success.
Thirty-day mortality after TAE ranges from 0 to 38% [11–13, 19–21] which is comparable to our study. In previous studies, Liu et al. [4] noted that early mortality was largely determined by the prerupture disease state (known diagnosis of HCC before rupture), the liver function at the time of rupture (total serum bilirubin level), and the severity of hemorrhage from the rupture (shock and hemoglobin level on admission), whereas Tan et al. [21] asserted that the presence of cirrhosis, Childclass C status, shock on admission, a higher blood transfusion requirement, raised alpha fetoprotein, raised alkaline phosphatase, raised aspartate transaminase, and raised indocyanine green at 15 min were all associated with increased risk of 30-day mortality. In this study, a low hemoglobin level, elevated bilirubin, prolonged prothrombin time (INR > 1.3), low albumin level, and unsuccessful embolization were associated with 30-day mortality apart from old age. Low albumin level was the only independent risk factor for 30-day mortality. Ten patients had radiological evidence of right portal vein thrombosis, 5 patients had left portal vein thrombosis, and 4 had main portal vein thrombosis; none of these was associated with early mortality. For those who had a successful TAE (57/62), liver failure was the cause of death in 10 patients (18%) (Four of them died within one month, and only four of them had portal vein thrombosis.) TAE can be performed without complications in patients with portal vein thrombosis [10]. For significance of portal vein thrombosis in patients with ruptured HCC who underwent TAE were not well defined in previous studies. In hemodynamically unstable patients with ruptured HCC who are already in such a critical condition, TAE may be the only viable option, despite the presence of portal vein thrombosis. Our study indicates that, although the number of patients in each group was small, and it is difficult to draw any precise conclusion, the presence of portal vein thrombosis should not be regarded as an absolute contraindication for TAE.
Surgical resection was possible in only seven patients (11%), which was lower than in contemporary studies (21–56%) [15]. This was due either to poor liver function or to multiple tumors on presentation. Nevertheless, our results showed that staged liver resection after embolization was safe and resulted in better survival. We agree with the current idea that TAE should be the choice of hemostasis at presentation of ruptured HCC and should be followed by staged hepatectomy in selected patients.
In conclusion, our study shows that TAE can achieve good hemostasis. Low albumin levels reflect poor liver reserve and may predict early mortality. Portal vein thrombosis should not be regarded as an absolute contraindication for TAE.
References
Ong GB, Chu EPH, Yu FYK, Lee TC. Spontaneous rupture of hepatocellular carcinoma. Br J Surg. 1965;52:123–9.
Yamagata M, Maeda T, Ikeda Y, Shirabe K, Nishizaki T, Koyanagi N. Surgical results of spontaneously ruptured hepatocellular carcinoma. Hepatogastroenterology. 1995;42:461–4.
Chearanai O, Plengvanit U, Asavanich C, Damrongsak D, Sindhvananda K, Boonyapisit S. Spontaneous rupture of primary hepatoma: report of 63 cases with particular reference to the pathogenesis and rationale treatment by hepatic artery ligation. Cancer. 1983;51:1532–6.
Liu CL, Fan ST, Lo CM, Tso WK, Poon RTP, Lam CM, et al. Management of spontaneous rupture of hepatocellular carcinoma: single-center experience. J Clin Oncol. 2001;19:3725–32.
Sato Y, Fujiwara K, Furui S, Ogata I, Oka Y, Hayashi S, et al. Benefit of transcatheter arterial embolization for ruptured hepatocellular carcinoma complicating liver cirrhosis. Gastroenterology. 1985;89:157–9.
Ong GB, Taw JL. Spontaneous rupture of hepatocellular carcinoma. BMJ. 1972;4:146–9.
Hirai K, Kawazoe Y, Yamashita K, Kumagai M, Nagata K, Kawaguchi S, et al. Transcatheter arterial embolization for spontaneous rupture of hepatocellular carcinoma. Am J Gastroenterol. 1986;81(4):275–9.
Shiina S, Ibukuro K. Transcatheter arterial embolization for the treatment of ruptured hepatocellular carcinoma. AJR Am J Roentgenol. 1989;153:658–9.
Ohtomo K, Furui S, Kokubo T, Yamauchi T, Yashiro N, Itai Y, et al. Transcatheter arterial embolization for spontaneous rupture of hepatocellular carcinoma: emergency chemoembolization or embolization. Radiology. 1991;180:647–51.
Corr P, Chan M, Lau WY, Metreweli C. The role of hepatic arterial embolization in the management of ruptured hepatocellular carcinoma. Clin Radiol. 1993;48:163–5.
Ngan H, Tso WK, Lai CL, Fan ST. The role of hepatic arterial embolization in the treatment of spontaneous rupture of hepatocellular carcinoma. Clin Radiol. 1998;53:338–41.
Yeh C-N, Lee W-C, Jeng L-B, Chen M-F, Yu M-C. Spontaneous tumor rupture and prognosis in patients with hepatocellular carcinoma. Br J Surg. 2002;89:1125–9.
Chiappa A, Zbar A, Audisio RA, Paties C, Bertani E, Staudacher C. Emergency liver resection for ruptured hepatocellular carcinoma complicating cirrhosis. Hepatogastroenterology. 1999;46:1145–50.
Hai L, Yong-Hong P, Yong F, Ren-Feng L. One-stage liver resection for spontaneous rupture of hepatocellular carcinoma. World J Surg. 2005;29:1316–8.
Lai EC, Lau WY. Spontaneous rupture of hepatocellular carcinoma a systematic review. Arch Surg. 2006;141:191–8.
Sunderland GT, Chisholm EM, Lau WY, Chung SC, Li AKC. Alcohol injection: a treatment for ruptured hepatocellular carcinoma. Surg Oncol. 1992;1:61–3.
Fuchizaki U, Miyamori H, Kitagawa S, Kaneko S. Radiofrequency ablation for life-threatening ruptured hepatocellular carcinoma. J Hepatol. 2004;40:354–5.
Shiratori M, Nagashima I, Takada T, Morofuji S, Motomiya H, Matsuda K, et al. Successful treatment of ruptured hepatocellular carcinoma with intraperitoneal injection of OK-432. J Hepatobiliary Pancreat Surg. 2004;11:426–9.
Shimada R, Imamura H, Makuuchi M, Soeda J, Kobayashi A, Noike T, et al. Staged hepatectomy after emergency transcatheter arterial embolization for ruptured hepatocellular carcinoma. Surgery. 1998;124:526–35.
Liu CL, Fan ST, Lo CM, Tso WK, Poon RT, Lam CM, et al. Management of spontaneous rupture of hepatocellular carcinoma: single-center experience management. J Clin Oncol. 2001;19:3725–32.
Tan FL, Tan YM, Chung AY, Cheow PC, Chow PK, Ooi LL. Factors affecting early mortality in spontaneous rupture of hepatocellular carcinoma. ANZ J Surg. 2006;76:448–52.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Li, WH., Cheuk, E.CY., Kowk, P.CH. et al. Survival after transarterial embolization for spontaneous ruptured hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 16, 508–512 (2009). https://doi.org/10.1007/s00534-009-0094-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-009-0094-6