Abstract
Background
Palliative care (PC) education for fellows in hematology/oncology (H/O) training programs is widely accepted, but no studies to date have assessed PC education practices and values among program leadership.
Methods
Program Directors and Associate Program Directors of active H/O fellowship programs in the U.S.A. were surveyed.
Results
Of 149 programs contacted, 84 completed the survey (56% response rate), of which 100% offered some form of PC education. The most frequently utilized methods of PC education were didactic lectures/conferences (93%), required PC rotations (68%), and simulation/role-playing (42%). Required PC rotations were ranked highest, and formal didactic seminars/conferences were ranked fifth in terms of perceived effectiveness. The majority felt either somewhat (60%) or extremely satisfied (30%) with the PC education at their program. Among specific PC domains, communication ranked highest, addressing spiritual distress ranked lowest, and care for the imminently dying ranked second lowest in importance and competency. Solid tumor oncologists reported more personal comfort with pain management (p = 0.042), non-pain symptom management (p = 0.014), ethical/legal issues (p = 0.029), reported their fellows were less competent in pain assessment/management (p = 0.006), and communication (p = 0.011), and were more satisfied with their program’s PC education (p = 0.035) as compared with hematologists.
Conclusions
Significant disparities exist between those modalities rated most effective for PC education and those currently in use. Clinical orientation of program leadership can affect both personal comfort with PC skills and estimations of PC curriculum effectiveness and fellows’ competency. H/O fellowship programs would benefit from greater standardization and prioritization of active PC education modalities and content.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Palliative care (PC) education for fellows in hematology/oncology training programs is broadly accepted and included in consensus guidelines by the American Society of Clinical Oncology (ASCO), the European Society for Medical Oncology (ESMO), the American Society of Hematology (ASH), and the American Association of Hospice and Palliative Medicine (AAHPM) [1,2,3,4]. The Accreditation Council for Graduate Medical Education (ACGME) explicitly identifies PC as a “core competency” for hematology/oncology fellows, stating: “Fellows must demonstrate competence in […] the management of pain, anxiety, and depression in patients with cancer and hematologic disorders; [and] palliative care, including hospice [5].”
Despite this, studies indicate significant gaps in PC education for hematology/oncology fellows. Buss and colleagues (2011) conducted a national study of second year hematology/oncology fellows in the U.S.A. and found that while there was agreement about the importance of education about pain management and psychosocial needs, less than one-third of trainees received any formal education on these domains. In addition to this, the quality of PC education was rated lower than fellowship education in general [6]. A subsequent national survey of hematology/oncology fellows by Thomas and colleagues (2015) found increased rates of PC education during fellowship; however, over 25% still reported no teaching in assessing prognosis, timing of hospice referrals, or conducting family meetings [7]. These studies demonstrate continued need for improved PC education in hematology/oncology fellowships, but ambiguity remains regarding how efforts should be focused.
Program leadership, including Program Directors (PD) and Assistant/Associate Program Directors (APD), is a critical stakeholder in setting the educational agenda, with unique insight into current curricular design and developmental barriers. To date, we are aware of no prior studies evaluating PD/APD values and perceptions of PC education in hematology/oncology fellowships. This needs assessment survey characterizes practices, beliefs, and challenges of current PC education in U.S.A. hematology/oncology fellowships described by program leadership.
Materials/methods
The University of California, Los Angeles Institutional Review Board committee exempted this study from further review. Participation was voluntary, and there were no financial incentives offered for completion or participation in this study.
Survey development
The authors developed a 24-question survey with Likert-style and multiple-choice questions, as well as qualitative free text answer choices (Supplementary Appendix 1). Demographic information about fellowship class size, number of faculty, and teaching hospital types was included to assess the diversity of respondents. We specifically sought estimates of the number of PC-trained hematologist/oncologists at each institution, given the potential impact this new area of subspecialization could have on PC education within hematology/oncology [8].
Specific teaching methods included in the survey were drawn from previous surveys of PC education in other medical specialties [8, 9]. Questions 11 through 14 elicited perceptions on 9 core PC domains, as gathered from ASCO, AAHPM, ESMO, and ACGME guidelines and used in previous PC education surveys [1,2,3,4,5, 8]. Question 12 (“How well do you think each of following palliative care topics fits into the scope of practice for hematology/oncology?”) was added to disambiguate PC domains perceived as important to learn (Q11) from those that serve practicing hematologist/oncologists on a routine basis. While related, we felt this reframing could define those areas that respondents believe fall more within the purview of specialist PC clinicians.
Survey distribution
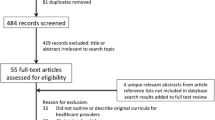
This web-based survey was distributed to PD of U.S. hematology and medical oncology fellowship programs with trainees using automated emails containing unique survey links via Qualtrics software. If no response was obtained after the first 2 months, a personalized follow-up email was sent to the prospective respondent. After three attempts at follow-up, contact for study recruitment was shifted to an APD at the same institution. Follow up contact for APD nonresponders was attempted roughly 1 month apart and up to three times. The recruitment period for participation was December 2019 to June 2020.
Participants
All accredited U.S. adult hematology and medical oncology fellowship programs with fellows enrolled at the time of survey distribution were included. Programs without trainees at the time of survey distribution were excluded. Contact information for PD and program coordinators was obtained using the publicly available ACGME program search directory. Contact information for APD was gathered through departmental website listings, published articles, or referral from program coordinators. Demographic information was primarily self-reported. Information not provided through self-reporting was gathered from departmental websites and publications.
Data analysis
Answers to values-based questions (questions 10–15) were correlated with primary clinical role as a hematologist (H) or solid tumor oncologist (STO) using the Mann–Whitney U test. Qualitative data obtained from free text, write-in answers were included in the results if thematically linked content appeared more than twice, with representative quotes chosen at the authors’ discretion. Qualtrics software (version October 2019; copyright © 2019 Qualtrics) was utilized for survey distribution, data collection, and descriptive analyses. Completion of the survey was not contingent on all survey questions being answered, however participants must have reached the end of the survey and hit submit to be included in the final data analysis.
Results
Baseline characteristics
In total, 149 fellowship programs were contacted, including 146 combined hematology/oncology programs and 3 medical oncology programs. Of these, 84 (56.3%) consented and completed the survey and 3 (2%) did not consent. Respondents were predominantly PD (62%) whose primary clinical specialty was solid tumor oncology (60.7%) (Table 1). Most programs reported having either 0 (27%) or 1–2 (41%) hematology/oncology faculty members with formal PC training. Programs reported fellows rotate at university-based hospitals (83.3%), community hospitals (33.7%), military hospitals (15.1%), and public hospitals (11.6%). All but 1 respondent reported having PC services at their institution (98.8%). Most (67.9%) reported an affiliated PC fellowship program. All participants reported their fellowship program included some form of PC education.
Delivery methods and content
Varied modalities of PC education were represented among respondents. Didactic seminars/conferences (92%) and required PC rotations (68%) were reported by the majority of programs. Education was primarily provided by PC faculty (93%), hematology/oncology faculty with (41%) and without (42%) formal PC training, and nurse practitioners with formal PC training (37%). When asked about proprietary and non-proprietary materials used for PC education, no one source predominated. The most common content reported by programs was materials developed at their home institution (36%) (Table 2).
Among programs that reported using PC didactic seminars/conferences, 77% reported 1–4 h of total didactic time annually (Table 3). Settings of required PC rotations were inpatient only (39%), outpatient only (11%), or both (50%), and were 1–2 weeks (34%) or 3–4 weeks (58%) long.
Simulation/role playing/standardized patients were reported by 42% of programs as part their PC curriculum, with 1–4 h annually in 67% of programs. Programs using live practice with formal feedback for communication skills training reported no minimum (38%) or 1–2 (38%) required sessions throughout the course of fellowship training.
Values and perceptions
The majority of those surveyed felt either somewhat (60%) or extremely satisfied (30%) with their program’s PC education (Table 4). Responses were scored as somewhat (+ 1) or extremely (+ 2) satisfied, or somewhat (− 1) or extremely (− 2) dissatisfied. Stratification by primary clinical role revealed that solid tumor oncologists were significantly more satisfied with their institution’s PC education than hematologists (1.26 vs 0.82, p = 0.035).
Participants were asked how likely they were to add PC education curriculum hours to the next academic year, ranging from “not at all likely” (0) to “absolutely” (4). Programs responded not at all likely (33%), somewhat likely (38%), very likely (18%), and absolutely (12%). Solid tumor oncologists did not significantly differ from hematologists in their likelihood to add PC education hours to the curriculum (0.94 vs 1.29, p = 0.197). Perceived barriers were time for teaching (63%), availability of faculty (54%), faculty expertise (32%), educational resources (21%), and fellow support (19%) (Table 4).
Participants ranked the effectiveness of educational delivery methods, ranging from “not effective” (1) to “critical” (4). Delivery methods ranked highest were required PC rotations (average 3.22), followed by live practice with formal feedback (3.09), elective rotations (2.84), simulation/role playing (2.67), and formal didactic seminars/conferences (2.62) (Fig. 1).
Participants ranked each of 9 core PC domains, ranging from “not at all important” (1) to “critical” (5). Core PC domains included pain assessment, nonpain symptom assessment, advance care planning, care for imminently dying, prognostication, addressing spiritual distress, ethical/legal issues, hospice/palliative care resources, and communication. Participants assessed each domain in terms of (1) relative importance; (2) how well it fits into the scope of practice for a practicing hematologist/oncologist; (3) how well trained they felt their fellows were within each domain (fellows’ competency); and (4) how comfortable they themselves felt in each of the domains (personal competency). The domain ranked highest was communication (average 4.68), and lowest was addressing spiritual distress (3.87) across all 4 categories (Fig. 2).
Perceptions of palliative care education by domain (n = 82). Comparative results of a 5-point Likert scale of the following questions: 1. “How important do you believe it is for hematology/oncology fellows to receive education on the following palliative care topics?” (1 = not at all important, 5 = critical); 2. “How well do you think each of following palliative care topics fits into the scope of practice for hematology/oncology?” (1 = not at all well, 5 = extremely well); 3. “How well trained do you think your hematology/oncology fellows are in the following palliative care topics” (1 = not at all well, 5 = extremely well); 4. As a hematologist/oncologist yourself, how comfortable are you with providing the following palliative care for your patients? (1 = extremely uncomfortable; 5 = extremely comfortable)
As compared with hematologists, solid tumor oncologists ranked significantly higher personal competency with pain assessment/management (4.65 vs 4.36, p = 0.042), nonpain symptom management (4.71 vs 4.36, p = 0.014), and ethical and legal issues (4.47 vs 4.07, p = 0.029), with differences in communication approaching significance (4.90 vs 4.64, p = 0.064). Solid tumor oncologists also felt that fellows at their institution were significantly less competent in pain assessment/management (1.86 vs 2.39, p = 0.006) and communication (1.60 vs 2.03, p = 0.011), with differences in nonpain symptom management approaching significance (1.93 vs 2.29, p = 0.075).
Qualitative descriptions
Five survey questions (questions 9–10, 16–18) provided space for optional, free-text entries. We selected specific responses for qualitative analysis of recurrent themes.
The first recurrent theme was the value of experiential learning. One PD, summarizing PC education at their institution (Q17), wrote “Learning by doing. Much of what oncologists do is palliative care.” Another PD wrote, “Most valuable is real life experience with oncology patients as they transition through stages of cancer. Other “materials“ are less effective.”
The second recurrent theme was the difficulty of delivering effective feedback. One PD wrote, “Direct observation with feedback is very effective […] however, fellows often have these conversations without direct observation so it is difficult to standardize a way to provide routine effective feedback.” Another wrote, “A more robust educational experience with interactive feedback is needed but we lack the time and resources to devote to improving the palliative care education.”
The third recurrent theme was the importance of PC education early in fellowship training. One PD wrote, “We do the rotation towards the end of the 1st year so they can reflect on what they’ve seen and adjust their practice going forward--I want them to incorporate it early in the first year before their practice style/pattern is set. Sometimes the 2nd and 3rd year fellows know everything already…”.
The last recurrent theme was dynamics between PC clinicians and hematology/oncology fellows. Participants reported fellows’ experiences with PC were shaped by a combination of formal education hours, role modeling by PC faculty, comanagement of mutual patients, and the deeper cultural and interprofessional dynamics within the institution. One respondent stated, “A very good relationship between the palliative care and the H/o [hematology/oncology] team is critical. When the fellows don’t feel supported by palliative care or feel their involvement is detrimental, it hinders their desire to involve them in early co-management, and thus they have less opportunity to learn and see the benefits of palliative care.” The reliance on PC team support was also identified multiple times as a potential barrier to fellows’ PC education. One PD stated, “I think, overall, our fellows are able to avoid learning palliative care because our institution has such a large palliative care practice. We simply defer to them.” Similarly, “Consult [to] palliative care by fellows instead of managing patient themselves leads to lack of experience.”
Discussion
Our survey characterizes the current PC education practices and values in U.S. hematology/oncology fellowship programs from the perspective of program leadership. Inclusion of at least some form of PC education across all programs surveyed adheres with ACGME requirements as well as ASH and ASCO guidelines for fellowship education in hematology/oncology and demonstrates investment in fellows’ PC training.
We found high rates of program leadership satisfaction with their current hematology/oncology fellowship PC education. Similar to prior studies of program leadership from other medical specialties, satisfaction seems to be congruent with rates of reported formal integrated PC education. Our findings of high satisfaction are similar to those among leadership of neuro-oncology fellowships (83%), who similarly reported high rates of formal PC education (88%) [9]. By contrast, program leadership of pulmonary/critical care reported lower satisfaction rates (20–50%) and lower integration of PC education, with only 20% reporting use of PC clinical rotations, and less than 10% used simulation/role-playing [10]. Similarly, program leadership in surgical oncology reported satisfaction rates of 40% and low integration of PC education, with only 15% of programs using lectures/small group discussions, and 15% utilizing required or elective PC clinical rotations [11]. The higher uptake of PC educational modalities in our group of respondents may account for the increased satisfaction reported here. Overall, 67% of respondents in our survey were at least somewhat likely to add PC education hours to next year’s curriculum, suggesting continued motivation to improve and expand formal PC education.
Evaluations of specific PC domains showed a trend towards valuing teaching communication and less value to teaching about care for the imminently dying or spiritual distress. This parallels teaching domains emphasized by the ASCO/AAHPM multidisciplinary consensus panel on high quality PC in oncology, wherein communication skills were endorsed as important with high consistency (79%), and spiritual and cultural assessment were considered important with low consistency (35%) [4]. By contrast, this same panel also rated End-Of-Life (EOL) care as the most important domain (81%). The low value assigned to teaching EOL care in our survey may reflect respondents’ self-reported discomfort with their skills in this domain relative to others. Previous surveys of hematology/oncology fellows have found the perception of better teaching in EOL care domains was associated with lower rates of emotional exhaustion and depersonalization (traditional proxies for burnout), and that fellows who felt a responsibility to help patients at the EOL had higher sense of personal accomplishment [12]. This further supports the importance of identifying gaps in PC educational domains for hematology/oncology fellows.
When stratified by clinical specialty (solid tumor oncologist vs hematologist), PD and APD who are solid tumor oncologists reported significantly more comfort with certain PC domains than their hematologist counterparts. Differences in PC delivery for patients with solid tumors versus hematologic malignancies have been well documented, and show that patients with hematologic malignancies have high rates of chemotherapy use, hospitalization and ICU stay within 30 days of death, less effective symptom control, and less integration with hospice and PC services [13,14,15,16]. Thus, solid tumor oncologists may have more familiarity with PC delivery and therefore increased comfort with PC. PC domains that solid tumor oncologists felt particularly comfortable with were inversely related to their evaluation of the fellows’ competency in these domains, suggesting that educators who feel better trained in a given clinical domain may harbor higher standards for their trainees. Solid tumor oncologists also endorsed higher satisfaction with current PC education at their institution, which may reflect their own perceived comfort. Our findings support the general conclusion that the clinical orientation of fellowship program leaders in hematology/oncology may affect their views of PC education. However, no significant differences were seen in preferences for certain education modalities or PC domains, or in motivation to add PC curricular hours, suggesting these differences may have functionally little effect on PC education delivery.
Consistent with prior data suggesting diversity in the approach to PC education across GME programs, we found different formats for PC education [17]. This was anticipated, as the ACGME charges programs with training fellows to “demonstrate competence” in PC without specific guidance about methods. The majority reported the use of didactic seminars and conferences, which represent the most common and structurally convenient format of medical education delivery overall [18]. However, cognitive science and learning theory consistently emphasize the use of active over passive forms of learning for improved retention and learner satisfaction [19]. Recognition of this seemed to be reflected in PD and APD attitudes towards different PC education methods, as the more active modalities (PC clinical rotations, live practice with formal feedback, simulation/role play) were given higher average ratings than their more passive counterparts (didactic conferences/seminars, self-directed reading materials, online modules). Notably, respondents gave the highest ratings to required PC clinical rotations, a view that coheres with ASCO’s 2020 vision for PC education, which explicitly advocates for the inclusion of mandatory 1-month clinical rotations in palliative cancer care during oncology fellowship [3]. Despite this, nearly one-third of programs surveyed did not report use of required PC rotations. This dissonance between attitudes and practice represents an area for potential improvement, whereby institutions could prioritize transitions from passive to active PC education modalities, such as simulation or clinical rotations. Such active teaching modalities also serve to elevate the learner’s evaluable skills, from understanding and retention to observable behaviors—an ascension up the Kirkpatrick Triangle [20]. However, this must be balanced against the additional time and resources required to facilitate these sessions, which were readily recognized as current barriers to PC education.
There are multiple limitations of our study. First is the response bias inherent to survey methods. Program leadership that responded may be particularly passionate about or comfortable with PC education at their institution. Reliance on accurate participant reporting of measures of current PC education practices may result in recall bias. The response rate reported here is comparable to prior published surveys of oncology subspecialty fellowship directors, which ranged from 55 to 65% [21,22,23]. Survey respondents collectively represented 56% of active hematology/oncology fellowships in the U.S.A., with a variety of program sizes, geographical regions, and hospitals included, suggesting external validity. Combining PD and APD survey responses may represent two different populations with distinct roles within the fellowship program and curricular development. These roles may correlate with differing educational values and potential to implement change.
Conclusion
Program leadership in U.S. hematology/oncology fellowship programs report a high satisfaction and implementation rate of PC education, despite varied educational delivery methods and content. The clinical orientation of program leadership can affect both personal comfort with PC skills and estimations of PC curriculum and fellows’ competency. National guidelines from ACGME emphasizing EOL care and specific PC educational modalities such as PC clinical rotations and simulation may result in greater standardization of curricular content, and assure prioritization of more active PC education modalities. Additional studies are needed to assess the long-term impact of PC education on fellows’ PC skill development.
Data availability
Deidentified data for this study are available online via Open Science Framework at the following link: https://osf.io/eq5u2/?view_only=d1e6dd41f0dc4c98ac48f5936959650f
References
Dittrich C, Kosty M, Jezdic S et al (2016) ESMO/ASCO recommendations for a global curriculum in medical oncology edition 2016. ESMO Open 1(5):1–96.https://doi.org/10.1136/esmoopen-2016-000097
American Society of Hematology (2014) HEMATOLOGY-ONCOLOGY CURRICULAR MILESTONES: a collaboration of the American Society of Hematology & American Society of Clinical Oncology 4/18/14 EDITION. https://www.hematology.org/Educators/Training-Directors/2720.aspx. Accessed 07 July 2020
Ferris FD, Bruera E, Cherny N, Cummings C, Currow D, Dudgeon D, JanJan N, Strasser F, von Gunten CF, von Roenn JH (2009) Palliative cancer care a decade later: accomplishments, the need, next steps—from the American Society of Clinical Oncology. J Clin Oncol 27:3052–3058
Bickel KE, McNiff K, Buss MK et al (2016) Defining high-quality palliative care in oncology practice: an American Society of Clinical Oncology/American Academy of hospice and palliative medicine guidance statement. J Oncol Pract 12(9):828–838
Accreditation Council of Graduate Medical Education (2019) ACGME program requirements for graduate medical education in hematology and medical oncology.https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/155_HematologyAndMedicalOncology_2019.pdf?ver=2019-06-13-093131-547. Accessed 07 July 2020
Buss MK, Lessen DS, Sullivan AM, von Roenn J, Arnold RM, Block SD (2011) Hematology/ oncology fellows’ training in palliative care. Cancer 117:4304–4311
Thomas RA, Curley B, Wen S, Zhang J, Abraham J, Moss AH (2015) Palliative care training during fellowship: a national survey of U.S. hematology and oncology fellows. J Palliat Med 18(9):747–751
Hui D, Finlay E, Buss MK, Prommer EE, Bruera E (2015) Palliative oncologists: specialists in the science and art of patient care. J Clin Oncol 33(20):2314–2317. https://doi.org/10.1200/JCO.2014.60.3274
Mehta AK, May N, Verga S et al (2018) Palliative care education in U.S. adult neuro-oncology fellowship programs. J Neuro-Oncol 140:377. https://doi.org/10.1007/s11060-018-2963-9
Richman PS, Saft HL, Messina CR (2016) Palliative and end-of-life educational practices in US pulmonary and critical care training programs. J Crit Care 31(1):172–177
Larrieux G, Wachi BI, Miura JT et al (2015) Palliative care training in surgical oncology and hepatobiliary fellowships: a national survey of program directors. Ann Surg Oncol 22:S1181–S1186
Mougalian SS, Lessen DS, Levine RL, Panagopoulos G, von Roenn J, Arnold R, Block S, Buss M (2013) Palliative care training and associations with burnout in oncology fellows. J Support Oncol 11:95–102
Beaussant Y, Daguindau E, Chauchet A, Rochigneux P, Tournigand C, Aubry R, Morin L (2018) Hospital end-of-life care in haematological malignancies. BMJ Support Palliat Care 8(3):314–324
Hui D, Didwaniya N, Vidal M, Shin SH, Chisholm G, Roquemore J, Bruera E (2014) Quality of end-of-life care in patients with hematologic malignancies: a retrospective cohort study. Cancer 120(10):1572–1578
LeBlanc TW, Smith JM, Currow DC (2015) Symptom burden of haematological malignancies as death approaches in a community palliative care service: a retrospective cohort study of a consecutive case series. Lancet Haematol 2(8):e334–e338
Odejide OO, Cronin AM, Earle CC, LaCasce AS, Abel GA (2016) Hospice use among patients with lymphoma: impact of disease aggressiveness and curability. J Natl Cancer Inst 108(1):djv280
Weissman DE, Block SD (2002) ACGME requirements for end- of-life training in selected residency and fellowship programs: a status report. Acad Med 77:299–304
Hurst WJ (2004) The over lecturing and under teaching of clinical medicine. (reprinted) arch. Intern Med 164:1605–1608
Fink LD (2003) Creating significant learning experiences. Jossey-Bass, San Francisco
Kern DE, Thomas PA, Hughes MT (1998) Curriculum development for medical education: a six-step approach. Johns Hopkins University Press, Baltimore
Roth M, Wang D, Kim M, Moody K (2009) An assessment of the current state of palliative care education in pediatric hematology/oncology fellowship training. Pediatr Blood Cancer 53:647–651
Spiker M, Paulsen K, Mehta AK (2020) Primary palliative care education in US residencies and fellowships: a systematic review of program leadership perspectives. J Palliat Med 23(10):1392–1399. https://doi.org/10.1089/jpm.2020.0331
Lefkowits C, Sukumvanich P, Claxton R, Courtney-Brooks M, Kelley JL, McNeil MA, Goodman A (2014) Needs assessment of palliative care education in gynecologic oncology fellowship: we’re not teaching what we think is most important. Gynecol Oncol 135(2):255–260. https://doi.org/10.1016/j.ygyno.2014.08.016
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The University of California, Los Angeles Institutional Review Board committee reviewed this study and declared it exempt from further review.
Consent to participate
Informed consent was obtained from all individual participants in this study.
Consent for publication
Participants consented to publication of submitted responses in aggregate. No individual identifying information of participants is included in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Al-Mondhiry, J.H., Burkenroad, A.D., Zhang, E. et al. Needs assessment of current palliative care education in U.S. hematology/oncology fellowship programs. Support Care Cancer 29, 4285–4293 (2021). https://doi.org/10.1007/s00520-020-05919-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05919-7