Abstract
Purpose
Acute kidney injury (AKI) is a frequent dose-limiting toxicity induced by cisplatin. Mannitol has been used in hydration protocols to mitigate this adverse event but its role remains controversial. The aim of this study is to define the impact of mannitol on AKI in patients receiving cisplatin.
Methods
This retrospective observational study was conducted in cancer patients who received at least one dose of cisplatin between September 2010 and December 2016 at the Centre hospitalier de l’Université de Montréal. The primary outcome of this study was the comparison of all grade cisplatin-associated AKI between hydration protocols with or without mannitol.
Results
A total of 1821 patients were included of which 658 received mannitol whilst 1163 received hydration alone. The risk of all grade cisplatin-associated AKI was significantly lower for the mannitol group (Hazard Ratio (HR) = 0.62; 95% CI [0.42, 0.89]). This result was mainly driven by gynecologic (HR = 0.50), upper gastrointestinal (HR = 0.32), urinary tract malignancies (HR = 0.29) and lymphoma (HR = 0.33). No significant difference was seen for head and neck (HN), lung, germ cells and other cancers. However, HN cancers patients receiving mannitol had fewer grade 2 and 3 AKI. Significantly fewer AKI events were observed in HN, lung, upper gastrointestinal and urinary tract cancer when mannitol was added for cisplatin dose <75 mg/m2.
Conclusion
Although the results were generally driven by a decrease of grade 1 AKI for most cancers, the greatest benefit of mannitol was seen with cisplatin doses lower than 75 mg/m2 and should probably be reinstated in this setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cisplatin is a platinum-based antineoplastic drug commonly used in the treatment of various types of cancer, including head and neck, lung, and cervix. Common adverse events of cisplatin include nausea and vomiting, neurotoxicity, myelosuppression, ototoxicity, and nephrotoxicity. According to recent studies, cisplatin-induced acute kidney injury (AKI) occurs in 15 to 35% of patients despite nephroprotective measures [1, 2]. Dose-related nephrotoxicity remains the major dose-limiting toxicity and usually occurs within the first 10 days following cisplatin infusion and may persist for up to 3 weeks [3].
Cisplatin nephrotoxicity occurs mainly in the proximal tubule cells where its uptake through an organic cation transporter leads to accumulation. Direct tubular epithelial cell toxicity, vasoconstriction in the renal microvasculature, and pro-inflammatory effects also contribute to renal dysfunction [1, 3,4,5,6,7]. Traditionally, the use of intensive intravenous hydration before and after cisplatin infusion has been the mainstay of AKI prevention [4]. Additionally, use of diuretics such as mannitol and furosemide, although controversial, has been hypothesized to further limit cisplatin renal toxicity. Diuretics decrease urinary cisplatin concentration by increasing water excretion and blocking chloride reabsorption, which decreases the rate of cisplatin activation by aquation [2, 6, 8, 9].
Initial studies investigating the role of mannitol associated its use with a decrease in nephrotoxicity [8, 10, 11]. In 2003 and 2010, two studies concluded that mannitol had no impact on the incidence of cisplatin-induced nephrotoxicity when compared with hydration alone [12, 13]. A subsequent international mannitol drug shortage in 2012 called into question its role in cisplatin hydration protocols. Furthermore, in a review evaluating the role of mannitol, the authors concluded that hydration alone was the most reasonable strategy to reduce cisplatin-induced nephrotoxicity owing to the lack of compelling evidence favoring mannitol use [14]. Given the paucity of evidence, many centers worldwide, including our institution, removed mannitol from all cisplatin-containing hydration regimens.
In 2017, a systematic review of 24 studies evaluated strategies to prevent cisplatin-induced nephrotoxicity in 2546 patients with various types of solid tumors. Most of the studies included fewer than 100 patients (range of 17 to 496 patients) and evaluated different hydration regimens in patients receiving cisplatin doses greater than or equal to 50 mg/m2. Hydration volumes varied between 1 and 6 L of fluid and a wide range of definitions were used to assess nephrotoxicity [2]. Based on seven studies (564 patients) directly evaluating the role of mannitol, the authors stated that mannitol may be considered for cisplatin doses higher than 100 mg/m2 and/or patients with preexisting hypertension [2, 5, 8, 10,11,12,13, 15]. The authors also concluded that insufficient evidence supported the use of furosemide for forced diuresis.
Later, another retrospective study of 313 patients suggested that mannitol lowered the incidence of grade 2 or higher acute nephrotoxicity compared with hydration protocols without mannitol in patients with non-gynecologic malignancies and those receiving cisplatin doses greater than or equal to 70 mg/m2 (6% vs. 23%; p = 0.001 and 7% vs. 22%; p = 0.03, respectively) [16]. A retrospective case-control study of 1245 patients showed no influence of mannitol dosage (12 g, 20 g, or 40 g) on cisplatin-induced AKI (1.08, 95% CI 0.94–1.25, p = 0.29). However, results from a subgroup analysis suggested that patients receiving cisplatin 50 mg/m2 with 12 g of mannitol were less likely to develop nephrotoxicity compared with those who received hydration alone (OR 0.28, 95% CI 0.14–0.57, p < 0.001) [17].
Given the conflicting results observed throughout the literature, the role of mannitol in prevention of cisplatin-induced nephrotoxicity remains controversial. The aim of this study is to compare all grade nephrotoxicity between hydration protocols with or without mannitol in all patients receiving cisplatin for the treatment of cancer.
Methods
Patients
This retrospective trial was conducted at the Centre hospitalier de l’Université de Montréal (CHUM) in Canada. Patients were included if they were 18 years of age or older and received at least one intravenous dose of cisplatin with or without other concomitant cancer drugs and one of the three hydration protocols detailed below. Patients were excluded if they did not receive the volume of hydration provided in the usual protocols or if they received a cisplatin infusion in more than 4 h (ex: continuous perfusion over 24 h, etc.). For patients who received two different hydration protocols during the same regimen, only data from the first protocol was collected to prevent confusion bias. Furthermore, cycles for which creatinine values were not available within 6 weeks of the last cisplatin dose administered were considered missing data and therefore censored.
Study design
Electronic medical records were used to identify patients who received at least one dose of cisplatin between September 2010 and December 2016. Approval by the CHUM research and ethics committee was obtained prior to data collection.
Prior to the 2012 mannitol shortage, the standard hydration protocol for cisplatin according to our local practice contained mannitol with 1 L of normal saline (NS) alternating with 1 L dextrose 5% (D5%) and sodium chloride 0.45% (0.45% NaCl) (D5%–0.45% NaCl). Mannitol dosage, volume of hydration, and duration of cisplatin infusion varied according to the cisplatin dose. A total of 3 L of fluids (2 L before and 1 L after cisplatin) and 12.5 g of mannitol were administered with doses of cisplatin lower than 75 mg/m2. With doses greater than or equal to 75 mg/m2, a total of 4 L of fluids (3 L before and 1 L after cisplatin) and 25 g of mannitol were administered. Following the drug shortage and given the lack of evidence supporting its use, mannitol was removed from hydration protocols and NS alternating with D5%–0.45% NaCl became the standard protocol [14]. In 2015, our protocol was updated. Dextrose 5% (D5%) was removed from the hydration protocol and NS alone was given. This decision was taken after consultation with our nephrologists and was based on studies demonstrating a possible benefit of NS over D5% alone on the incidence of nephrotoxicity [18, 19]. Therefore, in the current study, patients were divided into three groups based on the hydration protocol they received, the mannitol, the D5%–0.45% NaCl, and the NS group, respectively.
The primary outcome of this study was the comparison of all grade cisplatin-associated AKI, according to Common Terminology Criteria for Adverse Events (CTCAE) version 4.03. (Table S1 of the Supplementary Material), between hydration protocols with or without mannitol [20]. The analysis was done by cycle by comparing baseline serum creatinine (SCr) to the highest SCr levels between cycles and for up to 6 weeks after cisplatin treatment completion. In some cases, there is a right censoring because the last serum creatinine was not available. The frequency of serum creatinine measures varied according to each chemotherapy protocol but also according to emergency room visits (see Table 1). Secondary outcomes included the comparison of all grade AKI for patients who received doses of cisplatin less than 75 mg/m2 and for patients who received doses greater than or equal to 75 mg/m2. All grade AKI was also compared between the D5% and 0.45% NaCl and the NS group for patients who did not receive mannitol. Other exploratory descriptive outcomes included the distribution of AKI toxicity by malignancy, consequences of toxicity for each malignancy, and frequency of adverse events associated with cisplatin.
Baseline demographic, concomitant nephrotoxic medication (see definition in Table S2 of the Supplementary Material), treatment data, hydration type, mannitol use, baseline, and follow-up magnesemia, kalemia, and natremia were collected. Data related to toxicity included baseline SCr (within a month before cisplatin), creatinine clearance (calculated with Cockroft-Gault equation), and SCr between every cycle. All variables were collected using electronic medical records, laboratory records, and prescriptions.
Statistical analysis
Counting process specification of the Cox’s regression models was used to estimate the hazard ratio (HR) with 95% confidence intervals (CI) for the difference of AKI between hydration groups [21]. This approach allows for adjustments using different risk sets at different time points [21]. Because of the significant interaction between cancer types and hydration groups, the effect of mannitol had to be analyzed separately by cancer types. These results were adjusted for cisplatin doses and use of furosemide. The overall effect of mannitol was estimated with a random effect meta-analysis. Probability of AKI-free events between groups with or without mannitol was calculated using the Kaplan-Meier method and curves were compared using the log-rank test. All statistical analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, NC, USA) with a significance level of 0.05.
Results
Of 1932 patients identified, 1821 were included in this study and 111 patients were excluded since they did not receive one of the three standard hydration protocols. A total of 658 patients (36.1%) received mannitol, 732 patients (40.2%) received D5%–0.45% NaCl and 431 patients (23.7%) received NS alone for a total of 6002 doses of cisplatin. For each cancer types, the groups with and without mannitol were similar in regards to baseline characteristics (Table 1). Most patients had a normal kidney function whilst few patients had a baseline creatinine clearance less than 60 mL/min (4%). Furosemide use was significantly more frequent in the mannitol group compared with patients receiving D5%–0.45% NaCl and NS (97.9%, 43.9%, and 24.1% respectively; p < 0.001) as it was a standard practice at that time. A higher percentage of patients was treated for a gynecologic malignancy in the mannitol group and so the cisplatin doses and hydration volume were lower.
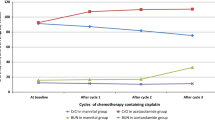
Overall, 1212 AKI events were reported in 562 patients. The primary outcome of the trial, the risk of all grade cisplatin-associated AKI was significantly lower for the mannitol group (hazard ratio (HR) = 0.62; 95% CI [0.42, 0.89]). Certain tumor sites demonstrating an important advantage in favor of the mannitol group like gynecologic (HR = 0.50; P = 0.0377), upper gastrointestinal (GI) (HR = 0.32; p = 0.0086), urinary tract malignancies (HR = 0.29; p = 0.0047), and lymphoma (HR = 0.33; p = 0.0075). However, no difference was seen for head and neck (HR = 1.00; p = 0.99), lung (HR = 0.73; p = 0.096), germ cells (HR = 1.15; p = 0.8355), and other cancers (HR = 1.29; p = 0.5076) (Fig. 1). A Kaplan-Meier analysis of the probability of AKI-free events was performed for each cancer type and is presented in Figure S1. These figures show that most AKI events occurred during the first cycle of treatment and are evenly distributed afterwards.
For most malignancies, no statistical difference was seen between hydration protocols with or without mannitol in patients receiving doses greater than or equal to 75 mg/m2 (Table 2). Conversely, with the exception of gynecologic, lymphomas, and other cancers, patients receiving cisplatin doses lower than 75 mg/m2 were significantly less likely to develop AKI when mannitol was administered (Table 2).
In patients not receiving mannitol, the risk of all grade AKI was significantly lower for patients with gynecologic malignancies in the D5%–0.45% NaCl group when compared with the NS group [HR = 0.38 (95% CI 0.18–0.77); p = 0.0072]. Patients receiving treatment for a head and neck or a lung cancer were less likely to develop all grade AKI with dextrose hydration compared with non-dextrose hydration although the association was not statistically significant. In patients with lymphoma, upper GI, and urinary tract cancers, there was a higher risk of all grade AKI in patients receiving dextrose compared with patients receiving NS (Fig. 2). However, this trend was statistically nonsignificant.
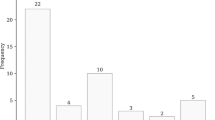
Exploratory analysis showed that grade 1 AKI were the most common, whereas grade 3 AKI were the least common (Table S3 of the Supplementary Material). Head and neck cancer patients receiving mannitol had fewer grade 2 or 3 AKI events (Table S3). No grade 4 AKI were observed in any cancer types. Electrolytic disorders occurring during treatment are detailed in Table S4. No clear pattern emerges from the consequence of toxicity between hydration protocols. However, dose reduction and chemotherapy cycle omission appear less frequent in gynecologic cancer patients who received mannitol-containing hydration protocols although the exact reason was not collected (cytopenia, AKI, etc.) (Table S5).
Discussion
In this retrospective study, the addition of mannitol to a standardized hydration protocol in prevention of cisplatin-induced nephrotoxicity was associated with a risk reduction of all grade AKI in our entire cohort of patients. This result was obtained from a random effect meta-analysis because the interaction of cancer types was significant in the counting process specification of Cox’s regression models. Because of the interaction, the extrapolation of the overall effect of mannitol should be done with caution. The analysis by cancer types became necessary as certain tumor sites demonstrating an important advantage in favor of the mannitol group (gynecologic, upper GI, and urinary tract cancers and lymphomas) in comparison with other malignancies (head and neck, lung, and germ cell tumors) (see Fig. 1).
A clinically compelling result in this trial is the benefit of mannitol in patients treated for gynecologic, urinary tract and upper GI malignancies. These patients generally received doses lower than 75 mg/m2. As shown in Table 2, for most malignancy groups, patients receiving lower doses of cisplatin (< 75 mg/m2) were less likely to experience nephrotoxicity in the mannitol group. According to the local hydration protocol, patients who were given cisplatin doses less than 75 mg/m2 received 3 L of IV fluid whilst patients who were given higher doses received 4 L of fluid. Thus, we hypothesize that the use of mannitol may have counterbalanced the use of lower fluid volume for these patients. This would, however, imply that the nephrotoxic effect of cisplatin is both dose dependent and influenced by the volume of fluid administered. This is opposed to the current literature which suggests a dose-dependent effect only [7, 14]. Previous retrospective studies showed significant benefits on mannitol-containing hydration protocols in patients receiving doses higher than 70 mg/m2 [6, 15]. Another explanation could be that doses of cisplatin ≥ 75 mg/m2 requires a higher dose of mannitol than those used in this study (25 g). However, a previous study showed no influence of mannitol dosage (12 g, 20 g, or 40 g) on cisplatin-induced AKI [17].
Many factors may explain the differences between our results and those published in previous studies. The definition and assessment of nephrotoxicity vary throughout studies and may account for some of the differences observed. Similarly to previous studies, we believe that the definition of AKI according to the CTCAE was the most appropriate way to evaluate cisplatin-induced nephrotoxicity because this grading system allows easy quantification of nephrotoxicity and is widely used in oncology [13, 15, 16]. This definition prevailed at the time of writing the protocol in January 2017 before the updated version 5 of CTCAE became available. As the measurement of creatinine greatly influences the clinical management of the patient, we believe that the choice of our primary objective is adequate. Important clinical consequences on treatment (omission, discontinuation, delay, or dose reduction) in Table S5 were not collected specifically for acute kidney injury and included treatment change for other reasons such as ototoxicity or fatigue. Additionally, the characteristics of the hydration protocols used may have affected the effectiveness of mannitol. The protocols used in this study required administration of greater volumes of fluid (3 L or 4 L) compared with previously published studies, which usually used 1 to 2 L [5, 12, 15, 16]. Therefore, this may explain the lower rate of all grade nephrotoxicity found in our study. Although patients in the mannitol group received furosemide more frequently than patients in the other hydration groups, the results were adjusted accordingly. Thus, the impact on our results is lessened.
Our results suggest that mannitol-containing hydration protocols may reduce nephrotoxicity in patients with head and neck, lung, upper gastrointestinal, and urinary tract cancer treated with cisplatin doses lower than 75 mg/m2 (Table 2). In patients with head and neck cancer, although no differences were seen between hydration protocols regarding the proportion of patients with at least one occurrence of any grade AKI (Fig. 1), those who received mannitol had fewer grades 2 and 3 AKI events (Table S3). However, it is unclear if this observation is driven by the subgroup of patients receiving cisplatin doses lower than 75 mg/m2. Regardless, the benefit of mannitol in patients with head and neck cancer is consistent with other studies [5, 15]. Thus, we believe mannitol use could be reinstated in this population, irrespective of cisplatin dose. In gynecologic cancer patients, mannitol was associated with a significant risk reduction of all grade nephrotoxicity (HR = 0.50, p = 0.0325). These results were mainly driven by a reduction of grade 1 AKI (Table S3) and clinical relevance is questionable. Unexpectedly, hydration protocols containing D5%–0.45% NaCl without mannitol were associated with a significative risk reduction of all grade nephrotoxicity compared with NS in the gynecologic cancer population (HR = 0.37, p = 0.0056). Lobo et al. reported that NS offers better volume repletion than D5% in non-cancer patients [18]. However, D5% was associated with a faster and more pronounced diuresis compared with NS. Consequently, D5%-induced diuresis is potentially beneficial to limit renal accumulation of cisplatin in patients receiving higher dose intensity regimens such as weekly cisplatin 40 mg/m2 in gynecologic malignancies. Since mannitol-containing hydration protocols also incorporated D5%–0.45% NaCl, the significant results favoring mannitol use in gynecologic cancers may be driven by the use of D5%. Therefore, hydration protocols containing D5% without mannitol should be considered in this population. Finally, lymphoma patients were the only subgroup to benefit from mannitol use with cisplatin doses greater than or equal to 75 mg/m2 (see Table 2). Since few patients received cisplatin doses lower than 75 mg/m2, we believe mannitol should be administered in all lymphoma patients receiving cisplatin. Exceptions must be made with patients receiving a continuous infusion of cisplatin for more than 4 h such as DHAP and ESHAP protocols as they were excluded from this study.
This study has several limitations. First, because of its retrospective nature, control of unknown confounding variables was not feasible. Residual differences between the characteristics of our patients in smaller groups (ex. lymphoma) may persist and for which we could not account for. Second, information bias may have affected our results. We chose to assess AKI by measuring SCr between each cisplatin cycle instead of taking the highest SCr throughout treatment. This allowed us to have an increased sensitivity to detect low-grade AKI. Because cisplatin-induced AKI usually occurs in the first ten days of cisplatin administration, we were more likely to detect nephrotoxicity for weekly platinum regimens than for those with longer cycle frequency. The latter may partially explain our results in gynecologic cancers and lymphomas [3]. We were also more likely to detect AKI in patients who received chemotherapy on day 8 every 3 weeks or weekly. To limit this risk of detection bias, we decided to classify patients according to types of malignancy instead of pooling them all together. The blood test frequency follow-up is similar between each subgroup (see Table 1). Additionally, our results show that grade 1 AKI was predominant in all tumor sites (Table S3 of the Supplementary Material). Hence, it is reasonable to believe that our results are mainly driven by a risk reduction in grade 1 AKI rather than any other grade and clinical relevance may be questionable in this context. Also, given that hydration protocol administration is determined by drug shortage and departmental decisions, this study was not subjected to indication bias.
To our knowledge, HYDRA is the largest study exploring the role of mannitol in cisplatin nephrotoxicity prevention with a total of 1821 patients included. This allowed us to classify patients according to cancer types thus limiting the existing heterogeneity. Since we did not exclude patients on the basis of malignancy type, we included patients that we believe were understudied such as upper GI, urinary tract, and lymphomas. Although a smaller number of patients are included in these groups, the results obtained are consistent with the rest of our conclusions. Secondly, our study comprehensively details patient characteristics and hydration protocols used. The results are more easily generalized to a broader population.
Conclusion and relevance
To date, studies examining the role of mannitol in hydration protocols to prevent cisplatin-induced AKI are controversial. Recent studies suggested that mannitol has a protective effect against cisplatin-induced nephrotoxicity for high-dose cisplatin used in head and neck cancer. Data is still lacking for other tumor sites and some hospitals continue to use mannitol while others do not. Our study showed that mannitol-containing hydration protocols significantly reduced the risk of AKI compared with hydration alone in patients with lymphomas, gynecologic, upper GI, and urinary tract malignancies. However, since these results are driven by a reduction in grade 1 toxicity, clinical relevance remains to be seen. Mannitol provided more benefit to patients with doses lower than 75 mg/m2 amongst most malignancies. These results suggest that mannitol should be added in this context. For head and neck cancers, the hydration protocols containing mannitol did not decrease all grade AKI but reduced the number of grade 2 and 3 AKI. Therefore, mannitol should also be used in this setting. Despite the significant results obtained, our findings suggest that the nephroprotective effects of hydration may also depend on the volume of fluid administered. Thus, future studies should also focus on evaluating the ideal volume of hydration.
References
Yao X, Panichpisal K, Kurtzman N, Nugent K (2007) Cisplatin nephrotoxicity: a review. Am J Med Sci 334:115–124
Crona DJ, Faso A, Nishijima TF, McGraw KA, Galsky MD, Milowsky MI (2017) A systematic review of strategies to prevent cisplatin-induced nephrotoxicity. Oncologist 22:609–619
Pabla N, Dong Z (2008) Cisplatin nephrotoxicity: mechanisms and renoprotective strategies. Kidney Int 73:994–1007
Launay-Vacher V, Rey JB, Isnard-Bagnis C, Deray G, Daouphars M (2008) Prevention of cisplatin nephrotoxicity: state of the art and recommendations from the European Society of Clinical Pharmacy Special Interest Group on Cancer Care. Cancer Chemother Pharmacol 61:903–909
Morgan KP, Snavely AC, Wind LS, Buie LW, Grilley-Olson J, Walko CM, Weiss J (2014) Rates of renal toxicity in cancer patients receiving cisplatin with and without mannitol. Ann Pharmacother 48:863–869
Mach CM, Kha C, Nguyen D, Shumway J, Meaders KM, Ludwig M, Williams-Brown MY, Anderson ML (2017) A retrospective evaluation of furosemide and mannitol for prevention of cisplatin-induced nephrotoxicity. J Clin Pharm Ther 42:286–291
Miller RP, Tadagavadi RK, Ramesh G, Reeves WB (2010) Mechanisms of cisplatin nephrotoxicity. Toxins (Basel) 2:2490–2518
Ostrow S, Egorin MJ, Hahn D et al (1981) High-dose cisplatin therapy using mannitol versus furosemide diuresis: comparative pharmacokinetics and toxicity. Cancer Treat Rep 65:73–78
Ward JM, Grabin ME, LeRoy AF, Young DM (1977) Modification of the renal toxicity of cis-dichlorodiammineplatinum(II) with furosemide in male F344 rats. Cancer Treat Rep 61:375–379
Hayes DM, Cvitkovic E, Golbey RB, Scheiner E, Helson L, Krakoff IH (1977) High dose cis-platinum diammine dichloride: amelioration of renal toxicity by mannitol diuresis. Cancer 39:1372–1381
Al-Sarraf M, Fletcher W, Oishi N et al (1982) Cisplatin hydration with and without mannitol diuresis in refractory disseminated malignant melanoma: a southwest oncology group study. Cancer Treat Rep 66:31–35
Santoso JT, Lucci JA 3rd, Coleman RL et al (2003) Saline, mannitol, and furosemide hydration in acute cisplatin nephrotoxicity: a randomized trial. Cancer Chemother Pharmacol 52:13–18
Leu L, Baribeault D (2010) A comparison of the rates of cisplatin (cDDP)--induced nephrotoxicity associated with sodium loading or sodium loading with forced diuresis as a preventative measure. J Oncol Pharm Pract 16:167–171
Morgan KP, Buie LW, Savage SW (2012) The role of mannitol as a nephroprotectant in patients receiving cisplatin therapy. Ann Pharmacother 46:276–281
McKibbin T, Cheng LL, Kim S et al. (2015) Mannitol to prevent cisplatin-induced nephrotoxicity in patients with squamous cell cancer of the head and neck (SCCHN) receiving concurrent therapy. Support Care Cancer
Williams RP, Jr., Ferlas BW, Morales PC, Kurtzweil AJ (2016) Mannitol for the prevention of cisplatin-induced nephrotoxicity: A retrospective comparison of hydration plus mannitol versus hydration alone in inpatient and outpatient regimens at a large academic medical center. J Oncol Pharm Pract
Dhillon P, Amir E, Lo M, Kitchlu A, Chan C, Cochlin S, Yip P, Chen E, Lee R, Ng P (2019) A case-control study analyzing mannitol dosing for prevention of cisplatin-induced acute nephrotoxicity. J Oncol Pharm Pract 25:875–883
Lobo DN, Stanga Z, Simpson JA et al (2001) Dilution and redistribution effects of rapid 2-litre infusions of 0.9% (w/v) saline and 5% (w/v) dextrose on haematological parameters and serum biochemistry in normal subjects: a double-blind crossover study. Clin Sci (Lond) 101:173–179
Dumas M, de Gislain C, d’Athis P, Chadoint-Noudeau V, Escousse A, Guerrin J, Autissier N (1990) Influence of hydration on ultrafilterable platinum kinetics and kidney function in patients treated with cis-diamminedichloroplatinum(II). Cancer Chemother Pharmacol 26:278–282
Common Terminology Criteria for Adverse Events (CTCAE) Version 4.03, U.S. Departement of Health and Human services, National Institutes of Health and National Cancer Institute. In. 2010
Cnaan A, Ryan L (1989) Survival analysis in natural history studies of disease. Stat Med 8:1255–1268
Funding
This work was financially supported by a research grant from the Faculty of Pharmacy at Université de Montréal.
Author information
Authors and Affiliations
Contributions
AMB, MLM, EBD, EL, NL, MFA, and JPA designed the study. AMB, MLM, EBD, and EL collected the data. MG performed the statistical analysis. All the authors analyzed and discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Approval by the CHUM research and ethics committee was obtained prior to data collection.
Conflict of interest
AM Bégin, ML Monfette, E Boudrias-Dalle, E Lavallé, V Samouelian, D Soulières, M. Chagnon, and N Letarte declare that they have no conflict of interest. MA Fournier reports personal fees from Amgen and Pfizer outside the submitted work. JP Adam reports personal fees from Amgen, Novartis, Abbvie, Sandoz, and Celgene outside the submitted work.
Disclaimer
We have full control of all primary data and we agree to allow the journal to review our data if requested.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented as Poster Discussion Session at the 54th American Society of Clinical Oncology Annual Meeting, Chicago, IL, June 1–5, 2018
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Bégin, AM., Monfette, ML., Boudrias-Dalle, É. et al. Effect of mannitol on acute kidney injury induced by cisplatin. Support Care Cancer 29, 2083–2091 (2021). https://doi.org/10.1007/s00520-020-05703-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-020-05703-7