Abstract
Purpose
Despite more women undergoing treatment for breast cancer and increased survival rates, many women suffer from anxiety and physical symptoms (e.g., pain, fatigue) surrounding diagnosis and surgery. Research investigating the efficacy of psychosocial interventions for breast cancer patients during this period is limited. This randomized controlled pilot study examined the effect of a brief lovingkindness meditation intervention on these key outcomes.
Methods
Participants were 60 women who underwent core needle breast biopsy, received an abnormal biopsy result, and underwent breast surgery (White = 73.6%; African American = 22.6%; Asian American = 3.8%; Age M = 56). Participants were randomly assigned to one of three treatment conditions at breast biopsy: (1) lovingkindness meditation, (2) music, and (3) usual care. Assessments of anxiety, pain, fatigue, physiologic reactivity, and self-compassion occurred prior to patients’ biopsy, following biopsy, 1 week after receipt of biopsy results, and 1 week following breast surgery.
Results
Multilevel modeling analyses demonstrated that lovingkindness meditation significantly improved pain (p = 0.02), self-compassion (p = 0.004), and heart rate (p = 0.02) over time compared to control conditions. There was a trend for anxiety (p = 0.05). Music significantly improved pain (p = 0.04) compared to usual care.
Conclusions
These findings provide preliminary evidence for the feasibility and efficacy of a lovingkindness meditation intervention for breast cancer patients during the diagnostic and surgical period. Improving psychological and physical well-being during this time frame has the potential to improve longer-term health outcomes during adjuvant treatment and survivorship. Interventions that cultivate positive adjustment during the diagnostic and surgical period of breast cancer are an important area of future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Breast cancer is the most common cancer among women in the United States (U.S.) with over 255,000 women diagnosed in 2017 [1]. Many suffer from emotional distress and physical symptoms associated with breast cancer treatment [2,3,4,5], particularly during the diagnostic and surgical time frame [5,6,7]. Distress experienced during this period has been associated with negative psychological (e.g., anxiety) and physical (e.g., pain, fatigue) outcomes following breast cancer surgery [8,9,10].
Few studies have investigated psychosocial interventions to help breast cancer patients cope with elevated distress and bothersome symptoms during the diagnostic and surgical period. Most studies have focused solely on the surgical timeframe [11], neglecting the diagnostic period (e.g., time of biopsy, receipt of pathology results) despite its elevated levels of distress. Past studies have also targeted negative symptoms associated with surgery [12], with little or no attention on enhancing positive adjustment. Brief mind-body interventions such as meditation may offer a unique treatment approach for the diagnostic and surgical period given their ability to reduce negative emotional and physical symptoms [13, 14], while also improving well-being [15].
Lovingkindness meditation (LKM) may hold particular promise for breast cancer patients during the diagnostic and surgical period. LKM is a practice dedicated to developing positive emotions and releasing negative emotions [16]. Recent studies demonstrate preliminary efficacy of LKM protocols among healthy and clinical populations [17, 18]. Brief LKM interventions (i.e., 7–20 min) have been shown to reduce anxiety and pain [19, 20], and enhance autonomic functioning and positive psychological outcomes (e.g., self-compassion) [21, 22].
A brief LKM protocol introduced to patients early in the diagnostic period (i.e., breast biopsy) has the potential to improve important psychological and physical symptoms throughout the diagnostic and surgical period of breast cancer. We recently conducted a randomized controlled pilot study of a brief LKM protocol introduced during image-guided core needle breast biopsy (CNBB). Results found that LKM reduced anxiety, pain, and fatigue in patients during CNBB [23]. In the current study, the primary aim was to examine the feasibility and preliminary efficacy of the brief LKM protocol on anxiety, pain, and fatigue among women with abnormal biopsy results who subsequently underwent surgery. A secondary aim was to examine the effects of LKM on physiologic reactivity (i.e., blood pressure [BP], heart rate [HR]) and self-compassion.
Methods
Participants
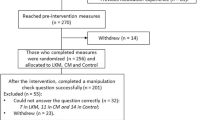
Participants were recruited from a breast biopsy clinic at a southeastern U.S. academic medical center between September 2012 and December 2013 as part of the larger, initial study examining women undergoing CNBB [23]. Eligibility criteria included (1) women ≥ 21 years old; (2) undergoing CNBB; (3) mammography/ultrasound BIRADS final assessment category 4a-c (suspicious) to 6 (cancer diagnosis); (4) able to speak and read English; and (5) provide consent. The present study examines the subsample of women who received an abnormal biopsy result and underwent surgery (Fig. 1).
In this HIPPA-compliant study, 138 of 203 invited participants provided informed consent. Sixty patients from our initial study [23] met inclusion criteria of receiving an abnormal/cancerous biopsy result and being referred for surgery. Four participants did not undergo surgery and were excluded, resulting in a final 56-patient sample.
Procedures
All eligible patients presenting to the biopsy clinic were given a brochure describing the study. If interested, they provided informed consent and a baseline assessment (validated questionnaires assessing anxiety, pain, fatigue, self-compassion; BP and HR measurements).
Participants were then randomized to one of the three study conditions with equal allocation (stratified by ultrasound vs. stereotactic-guided biopsy) using the program Block Stratified Randomization Version 5.0: (1) LKM, (2) music, and (3) usual care (UC). Music was selected as a comparison intervention condition because it was an equally feasible intervention to deliver during the diagnostic/surgical period and had been shown to reduce distress associated with biopsy and surgical procedures [24, 25]. Study staff communicated randomization results to participants and introduced interventions.
Following biopsy (see Soo et al.; [23]), patients completed a second assessment (questionnaires as above; demographic/medical questionnaire; BP and HR measurements) and were given written information regarding breast and women’s health. Participants in the LKM and music conditions were provided with audio recordings of their respective intervention for home practice.
Approximately 3 days to 1 week following biopsy, participants received biopsy results. Participants receiving abnormal or cancerous results indicating the need for surgery completed a third assessment by phone prior to surgery (i.e., 1 week after receiving the diagnosis). A fourth assessment occurred 1 week after surgery, following the same procedures. Home practice was assessed during phone assessments for patients randomized to LKM and music interventions. BP and HR were obtained via electronic medical records at participants’ pre- and post-surgical appointments.
Intervention conditions
Lovingkindness meditation
Participants were given a description of LKM and rationale for its use during biopsy [23]. During the biopsy procedure, participants used headphones/earbuds to listen to an MP3 playing the guided meditation audio file, specifically developed for use during biopsy.
The LKM focused on developing positive emotions towards oneself and others and releasing negative emotions. It began with a focus on the breath to encourage relaxation and then transitioned to contemplating a person one felt warm feelings towards (e.g., child, loved one). These feelings were then extended to a wider circle of individuals (e.g., oneself, other women receiving breast biopsies). The meditation included silent repetition of phrases (e.g., May I be safe; May she be peaceful) to direct feelings of love, compassion, and gratitude to different groups.
Following biopsy, participants were given a CD of LKM practices (e.g., 20-min guided meditation, 5-min guided meditation, informal meditation instruction). Participants were asked to practice for up to 20 min daily and told the meditation could help them relax and cope with challenges post-biopsy (e.g., discomfort, stress, difficult thoughts/emotions), referencing relevant LKM research (e.g., ability to reduce pain, distress; improve well-being) [17,18,19, 21]. Suggestions for practice were provided (e.g., find a quiet, comfortable place to practice; eliminate distractions).
After completing the post-result and post-surgery assessment, a 15-min scripted booster conversation occurred with study staff. LKM CD use was assessed, obstacles related to practice were discussed (e.g., forgetting to practice, complaints of discomfort), and suggestions for overcoming obstacles were provided (e.g., using daily reminders, listening to shorter tracks).
Music
Participants were provided with a brief rationale of the benefits of music during biopsy and picked a musical genre (i.e., classical music, jazz, world music, nature sounds). During biopsy, participants used headphones/earbuds to listen to the music audio file.
Following biopsy, participants took home a music CD of their selected genre. Participants were encouraged to listen to the music for up to 20 min at least once per day. A rationale for use was reviewed with participants (e.g., listening to music could help them relax and cope with discomfort/distress post-biopsy), referencing research that music can decrease pain and distress [26]. Suggestions for finding a quiet, comfortable place to listen to music were provided. A booster phone call occurred, as described above for LKM.
Usual care
Participants received supportive dialogue from the biopsy team during biopsy, the usual care in clinic. Supportive dialogue included questions and distractive dialogue (e.g., “how are you feeling?”, “where do you live?”).
Measures
Anxiety was assessed using the State Anxiety Scale of the State-Trait Anxiety Inventory (STAI) [27]. Items were summed, creating a total score (α = 0.94).
Body pain was assessed using the 4-item Brief Pain Inventory (BPI) pain intensity scale [28] that assesses pain “at its worst in the last week,” “at its least in the last week,” “on average,” and “right now” (0 = no pain, 10 = pain as bad as you can imagine). Scores were averaged for an overall pain intensity score (α = 0.88).
Breast pain was assessed pre-biopsy using two items adapted from the BPI [28]. The scale measured average breast pain intensity in the past month and currently on a 0–10 Likert scale. The items were averaged, creating an overall breast pain score (α = 0.89). Breast pain was assessed post-biopsy, post-result, and post-surgery using a two-item scale adapted from the BPI (i.e., average breast pain intensity since receipt of biopsy result/surgery and right now; 0–10 scale). These items were averaged, creating an overall continuing breast pain score (α = 0.70).
Fatigue was assessed using the FACIT Fatigue scale which measures fatigue over the past 7 days [29]. Items were summed, creating a total score (α = 0.91).
Physiologic reactivity was measured via BP and HR. BP measurements (systolic/diastolic) and HR were obtained using an automated inflation blood pressure cuff. Follow-up BP and HR assessments were obtained from electronic health records.
Self-compassion was measured using the Self-Compassion Scale-Short Form (SCS-SF) [30]. Scores on the subscales were averaged, producing an overall self-compassion score (α = 0.88).
Intervention practice was assessed using a two-item self-report measure, evaluating the frequencies with which patients (1) formally (i.e., listening to CDs) or (2) informally (e.g., repeating LKM phrases to oneself without the CD; listening to any music to relax) practiced the LKM or music intervention since biopsy/surgery.
Demographic and medical variables were obtained from a background information form and electronic medical records.
Feasibility was measured by participant accrual (at least a 60% participation rate), attrition (at least 80% of consented participants completing the study protocol), and adherence (proportion of participants successfully completing all assessments, with at least 75% completion rates serving as a benchmark).
Statistical analysis
Descriptive statistics were computed. Chi-square tests and analysis of variance were used to test for baseline differences across groups.
Study aims were tested with multilevel modeling (MLM) in SPSS 20.0. Intention-to-treat analyses were employed [31]. This method can be used for correlated data (e.g., repeated measures collected from an individual) and uses all repeated data allowing for randomly missing data points within a participant. There was limited missing data in this study. Across all assessments, only 10 assessments were missing—4% missing data. There were no differences in percentage of missing data across conditions. As this was a pilot study, post hoc comparisons between treatment conditions and simple slope analyses were conducted if the omnibus test for the treatment effect was significant (p < .05) or the pattern of data suggested a trend (p < 0.20). Simple slope analyses were conducted to examine whether the rate of change within each treatment condition differed from zero. As recommended, 95% confidence intervals are provided for estimates of slope [32].
In all MLM models, time was coded so that the intercept reflected the outcome variable at its first assessment. Each model included fixed effects for initial status (intercept), time, treatment condition, the effect of treatment condition on rate of change (treatment condition X time interactions), and covariates. All models included a random effect for the intercept. A random effect for time was included unless the model was not able to converge. Random effects for time were included for fatigue and self-compassion.
To examine whether intervention practice might have influenced significant findings, multilevel models including an intervention practice variable were conducted in the LKM and music conditions. A practice variable was calculated by averaging the amount of formal and informal LKM or music practice engaged in since biopsy/surgery. Each model included fixed effects for initial status (intercept), time, and average practice. Random effects for time were included as described.
Several of the outcome variables were identified as having non-normal distributions (skew > 2). We reran the models after transforming the outcome variables using a log transformation and results were unchanged. As interpretation of outcomes is difficult with transformed variables, results from the models with the original variables are presented.
Results
Descriptive statistics and baseline treatment condition comparability
Table 1 displays participant characteristics. There were no statistically significant differences at baseline among the treatment conditions on demographic, medical, or surgical factors, except for surgical history (x2(2) = 6.38, p = 0.04). Participants in the music condition were more likely to have a history of breast cancer surgery compared to participants in LKM or UC. Thus, surgical history was included as a control variable in all analyses.
Table 2 displays means and standard deviations of outcome measures for each condition by assessment period.
Feasibility
Among eligible patients approached for the study (N = 203), 138 consented to participate prior to biopsy (68% participation accrual rate). Among consented patients who received an abnormal biopsy result and subsequently underwent surgery (N = 56), five patients were lost-to-follow-up after biopsy and did not complete the study protocol (91% retention). Adherence to assessments was 96%. Across all assessments, 10 assessments were not completed.
Treatment outcomes
Table 3 displays fixed effects for multilevel models examining whether the LKM condition differed from music or UC in improving primary outcome variables. In these models, the intercept indicates the value of the outcome variable at initial assessment in the LKM condition. The time effect represents the rate of change in the outcome variable in the LKM condition. The main effects for music and UC are the difference between the initial value of the outcome variable in music and UC compared to LKM. The treatment condition × time interaction terms represent the difference between the rate of change in music and UC compared to LKM. Simple slope analyses examined whether the slope (i.e., rate of change) within each treatment condition differed significantly from zero.
Anxiety
For state anxiety, the ominibus test for intervention condition was F(2,144) = 2.11, p = 0.13. For this pilot study, pairwise comparisons were conducted. When comparing the LKM and UC conditions, the treatment × time interaction was significant (p = 0.046), indicating that UC showed greater increases in anxiety over time compared to LKM. LKM and music did not differ significantly over time (p = 0.21). Treatment × time interactions for music and UC were not significant (p = 0.52). Simple slope analyses showed that anxiety significantly decreased over time in LKM (B = − 4.05, SE = 0.87, t = − 4.65, p < 0.001, 95% CI = − 5.77, − 2.33) and music (B = − 2.28, SE = 1.06, t = − 2.15, p = 0.03, 95% CI = − 4.37, −0.19) but not in UC (p = 0.16).
Body and breast pain
For body pain, the overall treatment × time interaction was significant [F(2,83) = 3.56, p = 0.03]. When comparing both LKM and music conditions to UC, treatment × time interactions were significant (p = 0.02; p = 0.04, respectively), indicating that UC showed greater increases in body pain over time compared to LKM and music. Simple slope analyses showed that body pain significantly increased over time in UC (B = 0.48, SE = 0.24, t = 2.03, p = 0.046, 95% CI = 0.01, 0.95) but not in LKM (p = 0.16) or music (p = 0.35). LKM and music did not differ significantly over time (p = 0.99). The overall treatment × time interactions were not significant for breast pain [F(2,46) = 0.26, p = 0.77], suggesting no differences between groups.
Fatigue
The overall treatment × time interaction was not significant for fatigue [F(2,59) = 0.45, p = 0.64], suggesting no differences between groups.
Physiologic reactivity
The overall treatment × time interaction was significant for HR [F(2,40) = 3.68, p = 0.03]. When comparing LKM to music and UC conditions, the treatment × time interactions were significant (p < 0.05). There were no significant group differences between music and UC over time (p = 0.84). Simple slope analyses demonstrated that HR significantly increased over time in music (B = 3.84, SE = 1.31, t = 2.94, p = 0.01, 95% CI = 1.21, 6.48) and UC (B = 2.91, SE = 1.17, t = 2.48, p = 0.02, 95% CI = 0.53, 5.28) and did not change over time in LKM (p = 0.71).
The overall treatment × time interaction was not significant for diastolic BP [F(2,144) = 0.74, p = 0.48] or systolic BP [F(2,46) = 0.39, p = 0.68], suggesting no differences between groups.
Self-compassion
The overall treatment × time interaction was significant for self-compassion [F(2,41) = 4.51, p = 0.02]. When comparing the LKM to music condition, the treatment × time interaction was significant (p = 0.004), indicating that music showed greater reductions in self-compassion over time compared to LKM. LKM and UC did not differ significantly over time (p = 0.18). Treatment × time interactions for music and UC were not significant (p = 0.10). Simple slope analyses demonstrated that self-compassion significantly increased over time in LKM (B = 0.16, SE = 0.05, t = 3.59, p = 0.001, 95% CI = 0.07, 0.25) but not in music (p = 0.33) or UC (p = 0.18).
Relationship between intervention practice and outcomes
Analyses were conducted to examine the relationship between intervention practice and outcome variables within LKM and music conditions. In LKM, the practice × time interaction was significant for anxiety (p = 0.004) and HR (p = 0.03), indicating that practicing LKM led to reductions in anxiety and heart rate over time. There were no significant effects in multilevel models in music, indicating no practice effects for the music group.
Conclusions
To our knowledge, this is the first randomized controlled pilot study to investigate the efficacy of a LKM intervention for patients undergoing biopsy and breast cancer surgery. Results offer preliminary evidence that a brief LKM intervention is feasible, can improve negative physical symptoms, and can support positive adjustment during the diagnostic and surgical period of breast cancer. Findings also suggest that LKM may impact anxiety during this timeframe. The music intervention demonstrated positive effects on pain but did not improve positive adjustment.
One key finding of this study was that body pain remained stable in the LKM and music interventions, while it increased among patients in the UC condition. This is noteworthy as patients were exposed to several procedures that could increase pain (e.g., breast biopsy, axillary lymph node dissection, surgery). Past research indicates that increased pain levels are common among breast cancer patients in the surgical period (up to 50% post-surgery), and are associated with negative outcomes post-surgery (e.g., increased medication, delayed discharge, persistent pain) [33, 34]. Additionally, the development of persistent pain can lead to changes in neural plasticity [35], which can affect how pain is processed (e.g., increase pain response via central sensitization). Thus, the fact that participants were able to maintain stable levels of pain during the diagnostic and surgical period suggests that LKM and music protocols may protect women from a range of distressing symptoms and neuropsychological changes post-surgery.
It is surprising that LKM had no effect on breast pain compared to the music and UC conditions, given that breast pain is a component of body pain and would be expected to behave similarly. The body pain questionnaire was potentially a more valid measure of pain related to breast procedures compared to the two-item breast pain measure, as patients often experience pain in multiple body regions surrounding the breast (e.g., armpit, chest wall).
Another interesting finding was the trend suggesting that LKM could reduce anxiety, by approximately four points per assessment. A similar pattern was observed in the music condition but only by two points per assessment. For pilot studies, examining estimated effects (e.g., simple slopes with CI) for outcomes of interest is often recommended, as these results can provide valuable information about the pattern of data [32]. These results are promising and highlight the need for additional larger studies with greater power.
The LKM intervention led to improvements in positive psychological and physiological adjustment. Specifically, patients in the LKM intervention demonstrated increased self-compassion over time compared to the music condition. Developing self-compassion (i.e., qualities of self-kindness, common humanity, mindfulness [36]) could provide patients with useful emotion regulation strategies when experiencing distressing symptoms related to diagnosis and treatment. Self-compassion may play a protective role for patients during the breast cancer diagnostic and surgical period, and a larger RCT should explore whether self-compassion is a psychological resource that might mediate LKM treatment effects.
Patients in the LKM intervention showed no change in HR over time compared to increased HR among patients in the music and UC conditions. This finding suggests that the LKM protocol might have positively affected participants’ physiological activity. Research should further evaluate the effect of LKM on physiological outcomes during the diagnostic and surgical period by assessing variables such as HR variability and cortisol.
Interestingly, patients who practiced formal and informal LKM regularly were more likely to have significant reductions in anxiety and HR over time. There were no practice effects for the music condition. Future studies should test behavior technology (e.g., text messages) to encourage regular practice to better understand intervention dose and practice effects.
This study had several limitations. First, the sample included participants who experienced a range of surgical procedures (e.g., excisional biopsy, lumpectomy, mastectomy) and treatment regimens (e.g., immediate surgery, neoadjuvant chemotherapy before surgery). Second, the small sample size and inclusion of patients who were well-educated (61% had a college degree or higher) raise generalizability concerns, suggesting the need to replicate this study in community hospitals serving a broader population. Third, this study was not blinded. While this possibly impacted staff interactions and patients’ engagement with interventions, our study staff were extensively trained to follow standardized protocols with participants. Future work should employ blinding protocols to the greatest possible extent. Lastly, larger studies are needed to further evaluate the impact of LKM and music protocols on key outcomes.
In summary, this randomized controlled pilot study offers preliminary evidence that LKM can improve discomfort and distress during the diagnostic and surgical period of breast cancer, while also supporting positive physiological and psychological adjustment. These findings have important clinical implications, suggesting that a LKM protocol delivered at biopsy can lead to significant physical and psychological health benefits and be easily implemented in clinical settings.
Data availability
Dr. Wren has full access to the primary data. Data are stored at Duke University and Drs. Shelby and Keefe have full control of study data.
References
American Cancer Society (2017) Cancer facts and figures. American Cancer Society, Atlanta
Carpenter JS, Andrykowski MA, Sloan P, Cunningham L, Cordova MJ, Studts JL, McGrath PC, Sloan D, Kenady DE (1998) Postmastectomy/postlumpectomy pain in breast cancer survivors. J Clin Epidemiol 51(12):1285–1292
Keller M (1998) Psychosocial care of breast cancer patients. Anticancer Res 18(3C):2257–2259
Montgomery GH, Bovbjerg DH (2004) Presurgery distress and specific response expectancies predict postsurgery outcomes in surgery patients confronting breast cancer. Health Psychol 23(4):381–387. https://doi.org/10.1037/0278-6133.23.4.381
Payne DK, Sullivan MD, Massie MJ (1996) Women’s psychological reactions to breast cancer. Semin Oncol 23(1 Suppl 2):89–97
Liao MN, Chen MF, Chen SC, Chen PL (2008) Uncertainty and anxiety during the diagnostic period for women with suspected breast cancer. Cancer Nurs 31(4):274–283. https://doi.org/10.1097/01.NCC.0000305744.64452.fe
Maxwell JR, Bugbee ME, Wellisch D, Shalmon A, Sayre J, Bassett LW (2000) Imaging-guided core needle biopsy of the breast: study of psychological outcomes. Breast J 6(1):53–61
Nosarti C, Roberts JV, Crayford T, McKenzie K, David AS (2002) Early psychological adjustment in breast cancer patients: a prospective study. J Psychosom Res 53(6):1123–1130
Ozalp G, Sarioglu R, Tuncel G, Aslan K, Kadiogullari N (2003) Preoperative emotional states in patients with breast cancer and postoperative pain. Acta Anaesthesiol Scand 47(1):26–29
Tjemsland L, Soreide JA, Matre R, Malt UF (1997) Pre-operative [correction of Properative] psychological variables predict immunological status in patients with operable breast cancer. Psychooncology 6(4):311–320. https://doi.org/10.1002/(SICI)1099-1611(199712)6:4<311::AID-PON285>3.0.CO;2-C
Samarel N, Fawcett J, Davis MM, Ryan FM (1998) Effects of dialogue and therapeutic touch on preoperative and postoperative experiences of breast cancer surgery: an exploratory study. Oncol Nurs Forum 25(8):1369–1376
Larson MR, Duberstein PR, Talbot NL, Caldwell C, Moynihan JA (2000) A presurgical psychosocial intervention for breast cancer patients. Psychological distress and the immune response. J Psychosom Res 48(2):187–194
Greenlee H, DuPont-Reyes MJ, Balneaves LG, Carlson LE, Cohen MR, Deng G, Johnson JA, Mumber M, Seely D, Zick SM, Boyce LM, Tripathy D (2017) Clinical practice guidelines on the evidence-based use of integrative therapies during and after breast cancer treatment. CA Cancer J Clin 67(3):194–232. https://doi.org/10.3322/caac.21397
Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, Maglione MA (2017) Mindfulness meditation for chronic pain: systematic review and meta-analysis. Ann Behav Med 51(2):199–213. https://doi.org/10.1007/s12160-016-9844-2
Garland EL, Geschwind N, Peeters F, Wichers M (2015) Mindfulness training promotes upward spirals of positive affect and cognition: multilevel and autoregressive latent trajectory modeling analyses. Front Psychol 6:15. https://doi.org/10.3389/fpsyg.2015.00015
Salzberg S (1997) Lovingkindness: the revolutionary art of happiness. Shambala, Boston
Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM (2008) Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. J Pers Soc Psychol 95(5):1045–1062. https://doi.org/10.1037/a0013262
Carson JW, Keefe FJ, Lynch TR, Carson KM, Goli V, Fras AM, Thorp SR (2005) Loving-kindness meditation for chronic low back pain: results from a pilot trial. J Holist Nurs 23(3):287–304. https://doi.org/10.1177/0898010105277651
Hutcherson CA, Seppala EM, Gross JJ (2008) Loving-kindness meditation increases social connectedness. Emotion 8(5):720–724. https://doi.org/10.1037/a0013237
Tonelli ME, Wachholtz AB (2014) Meditation-based treatment yielding immediate relief for meditation-naive migraineurs. Pain Manag Nurs 15(1):36–40. https://doi.org/10.1016/j.pmn.2012.04.002
Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, Brantley M, Fredrickson BL (2013) How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol Sci 24(7):1123–1132. https://doi.org/10.1177/0956797612470827
Galante J, Galante I, Bekkers MJ, Gallacher J (2014) Effect of kindness-based meditation on health and well-being: a systematic review and meta-analysis. J Consult Clin Psychol 82(6):1101–1114. https://doi.org/10.1037/a0037249
Soo MS, Jarosz JA, Wren AA, Soo AE, Mowery YM, Johnson KS, Yoon SC, Kim CM, Hwang ES, Keefe FJ, Shelby RA (2016) Imaging-guided core-needle breast biopsy: impact of meditation and music interventions on patient anxiety, pain, and fatigue. J Am Coll Radiol 13(5):526–534
Palmer JB, Lane D, Mayo D, Schluchter M, Leeming R (2015) Effects of music therapy on anesthesia requirements and anxiety in women undergoing ambulatory breast surgery for cancer diagnosis and treatment: a randomized controlled trial. J Clin Oncol 33(28):3162–3168. https://doi.org/10.1200/JCO.2014.59.6049
Cho SW, Choi HJ (2016) Effect of music on reducing anxiety for patients undergoing transrectal ultrasound-guided prostate biopsies: randomized prospective trial. Urol J 13(2):2612–2614
Chang YH, Oh TH, Lee JW, Park SC, Seo IY, Jeong HJ, Kwon WA (2015) Listening to music during transrectal ultrasound-guided prostate biopsy decreases anxiety, pain and dissatisfaction in patients: a pilot randomized controlled trial. Urol Int 94(3):337–341. https://doi.org/10.1159/000368420
Spielberger C (1977) State-trait anxiety inventory. Consulting Psychologists Press, Palo Alto
Cleeland CS, Ryan KM (1994) Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singap 23(2):129–138
Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E (1997) Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manag 13(2):63–74
Raes F, Pommier E, Neff KD, Van Gucht D (2011) Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother 18(3):250–255. https://doi.org/10.1002/cpp.702
Hollis S, Campbell F (1999) What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ 319(7211):670–674
Moore CG, Carter RE, Nietert PJ, Stewart PW (2011) Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci 4(5):332–337
Jung BF, Ahrendt GM, Oaklander AL, Dworkin RH (2003) Neuropathic pain following breast cancer surgery: proposed classification and research update. Pain 104(1–2):1–13
Tasmuth T, von Smitten K, Kalso E (1996) Pain and other symptoms during the first year after radical and conservative surgery for breast cancer. Br J Cancer 74(12):2024–2031
Jensen (2010) A neuropsychological model of pain: research and clinical implications. J Pain 11(1):2–12. https://doi.org/10.1016/j.jpain.2009.05.001
Neff (2003) Development and validation of a scale to measure self-compassion. Self Identity 2:223–250
Acknowledgments
The authors wish to thank Mary Brantley, MA, LMFT, and Dee Campbell, MSEE for their assistance with this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wren, A.A., Shelby, R.A., Soo, M.S. et al. Preliminary efficacy of a lovingkindness meditation intervention for patients undergoing biopsy and breast cancer surgery: A randomized controlled pilot study. Support Care Cancer 27, 3583–3592 (2019). https://doi.org/10.1007/s00520-019-4657-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-019-4657-z