Abstract
Chemotherapy-induced nausea and vomiting (CINV) is a common toxicity that may impair the quality of life of patients with a variety of early- and end-stage malignancies. In light of recent changes in the optimal management of CINV, we undertook this narrative review to compare the latest guidelines published by ASCO (2017), NCCN (2018), and MASCC/ESMO (2016). The processes undertaken by each organization to evaluate existing literature were also described. Although ASCO, NCCN, and MASCC/ESMO guidelines for the treatment and prevention of CINV share many fundamental similarities, literature surrounding low and minimal emetic risk regimens is lacking. Data regarding the use of complementary alternative medicine for CINV is particularly scarce and in need of further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced nausea and vomiting (CINV) is one of the most distressing side effects among patients undergoing cancer treatment [1,2,3]. Although emesis and nausea were more common historically, when drugs for the prevention and treatment of CINV were limited, a recent study by Kuchuk et al. indicates that moderate to severe nausea remains one of the most feared side effects among women with breast cancer [3]. Further, nausea and vomiting have been associated with reduced quality of life [4], which is clearly undesirable for patients receiving both curative- and palliative-intent chemotherapy and may even compromise adherence to treatment.
Given a wide range of targeted and cytotoxic agents, anti-cancer therapies have been divided into four main categories to describe emetic risk. These include (i) highly emetogenic chemotherapy (HEC) which causes CINV among ≥ 90% of patients, (ii) moderately emetogenic chemotherapy (MEC) that causes CINV in 30–90% of patients, and (iii) low emetic risk and (iv) minimal emetic risk chemotherapies that incite CINV in 10–30% and ≤ 10% of patients, respectively [5]. There are a limited number of HEC regimens, which include high-dose cisplatin, carmustine, cyclophosphamide at doses greater than 1500 g/m2, dacarbazine, mechlorethamine, streptozocin, and combinations of anthracyclines and cyclophosphamide (AC). There is most variability among the MEC regimens that include but are not limited to carboplatin, doxorubicin, irinotecan, oxaliplatin, and cyclophosphamide. Drugs that fall into a low-risk category include certain targeted agents (cetuximab, panitumumab, pertuzumab, TDM1), immunotherapy drugs (ipilumumab, atezolizumab), and cytotoxic agents (docetaxel, pemetrexed, eribulin). Finally, bevacizumab, trastuzumab, vinorelbine, nivolumab, and pembrolizumab are among agents that pose minimal emetic risk agents.
Chemotherapy drugs are further described to pose a risk of either acute (within 24 h of receiving chemotherapy) or delayed (between 2 and 5 days following treatment) CINV. Delayed CINV is typically more prevalent than acute CINV [6], possibly due to more aggressive prevention strategies in the acute-phase setting. Finally, breakthrough CINV is the continuation of emesis and nausea within 5 days of receiving antiemetics [7].
Despite recent advances in the study and application of antiemetic regimens, there is still much room for improvement. A prospective, observational study conducted by Escobar et al. evaluated the incidence of CINV among patients receiving CINV prophylaxis primarily with a 5-HT3 receptor antagonist (RA) and a corticosteroid (n = 240) for colorectal (47.5%), lung (17.9%), and other cancers [8]. In this study, 31% of patients did not achieve complete response (no emesis and no rescue therapy) in cycle 1 and 38% did not achieve complete protection (no emesis, no significant nausea, and no rescue therapy) despite receiving prophylaxis. Additional studies have demonstrated similar results among 1910 patients receiving HEC and MEC regimens [9] and 276 patients receiving highly emetogenic anti-cancer agents [10]; in these studies, 49% and 41% of patients required breakthrough antiemetics for CINV, respectively. Such evidence of sub-optimal prophylaxis has motivated changes to CINV guidelines, which have recently been published by the American Society of Clinical Oncology (ASCO) and National Comprehensive Cancer Network (NCCN) in 2017 and 2018, respectively, as well as the Multinational Association of Supportive Care in Cancer and the European Society of Medical Oncology (MASCC and ESMO) in 2016 [11,12,13].
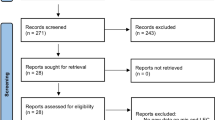
Methods
Major updates for the prophylaxis and treatment of CINV were extracted from the most recent guidelines published by ASCO, NCCN, and MASCC/ESMO and were organized by emetogenic risk. Only recommendations for adult patients were included. The process of each organization in evaluating the clinical evidence and strength of recommendations was also analyzed and compared.
Results
Treatment recommendations and updates
Antiemetic recommendations and updates provided by ASCO, NCCN, and MASCC/ESMO are summarized in Tables 1, 2, 3, and 4 and are organized by emetic risk of the antineoplastic agents. Since its last update in 2015, ASCO has implemented the use of a four-drug prophylactic regimen for HEC (Table 1), with the addition of olanzapine to an NK1 RA, 5-HT3 RA, and dexamethasone [11]. While olanzapine and dexamethasone are both administered on days 2–4 in non-AC HEC regimens, ASCO suggests that dexamethasone on days 2–4 may be omitted in AC regimens.
NCCN offers three different antiemetic regimens for the treatment of CINV following HEC, titled options A to C [12]. Option A consists of a 5-HT3 RA, NK1 RA, and dexamethasone for management of acute CINV. Options B and C both include olanzapine and dexamethasone in the acute phase, but differ slightly in their regimens, with option B including palonosetron and option C including any 5-HT3 RA along with an NK1 RA. Aprepitant is now being recommended by NCCN for the first time as an injectable emulsion at a dose of 130 mg in the acute phase. Options A and C consist of aprepitant and dexamethasone for delayed CINV, with option C also including olanzapine. Option B consists solely of olanzapine for the delayed phase. MASCC/ESMO recommend a three-drug antiemetic regimen consisting of an NK1 RA, a 5-HT3 RA, and dexamethasone for acute CINV following HEC [13]. The administration of dexamethasone on days 2–4 following chemotherapy is recommended for patients receiving non-AC HEC regimens. For patients receiving AC, delayed administration of dexamethasone or aprepitant is only recommended if aprepitant is administered on the day of chemotherapy. For cisplatin-treated patients, the use of either dexamethasone and aprepitant (if aprepitant is used acutely) or dexamethasone and metoclopramide is recommended on days 2–4.
For the prophylaxis of acute CINV resulting from MEC regimens (Table 2), ASCO [11] and MASCC/ESMO [13] recommend a two-drug antiemetic regimen consisting of a 5-HT3 RA and dexamethasone. For MEC regimens containing carboplatin area under the curve (AUC) greater than or equal to 4 mg/mL/min, both organizations have updated their recommendations to include an NK1 RA. Recommended acute dosages of common NK1 RAs are described in Table 3. ASCO and MASCC/ESMO have recommended the administration of dexamethasone on days 2 and 3 following chemotherapy for MEC agents that are known to cause delayed CINV such as cyclophosphamide, doxorubicin, and oxaliplatin. MASCC/ESMO recommend the use of aprepitant for delayed CINV in carboplatin-based regimens only if it has also been used in the acute phase, whereas ASCO has not provided any specific recommendations for delayed CINV in these regimens.
For the prophylaxis of CINV from MEC regimens, NCCN provides three antiemetic options, titled as options D to F [12]. Each includes dexamethasone and a 5-HT3 RA for the treatment of acute CINV. Option D specifies that palonosetron should be the 5-HT3 RA of choice, while also including olanzapine. Option F also includes an NK1 RA in its acute regimen. For delayed CINV, all of the options vary slightly, with option D providing a choice of a 5-HT3 RA or dexamethasone, option E including olanzapine only, and option F including both aprepitant and dexamethasone. It should be noted that regimens containing carboplatin must be AUC less than 4 mg/mL/min to be classified as MEC by NCCN.
For chemotherapeutic regimens of low emetic risk (Table 4), ASCO recommends the administration of either a 5-HT3 RA or dexamethasone for the treatment of acute CINV [11]. NCCN recommends the administration of one of dexamethasone, metoclopramide, prochlorperazine, or a 5-HT3 RA [12]. MASCC/ESMO recommend one of a 5-HT3 RA, dopamine RA, or dexamethasone [13]. No routine prophylaxis is recommended for delayed CINV resulting from low emetic risk regimens by any of the organizations.
Further, none of the organizations recommend prophylactic or rescue measures for chemotherapeutic agents with minimal emetic risk (Table 4) [11,12,13].
While MASCC/ESMO make no mention of alternative medicine for the treatment of emesis and nausea, ASCO has stated that the use of ginger, acupuncture, cannabis, and other alternative antiemetics can be neither recommended nor discouraged due to a lack of supporting evidence [11, 13]. Conversely, NCCN has suggested the use acupuncture and behavioral therapy (i.e., hypnosis, music therapy, cognitive distraction) for anticipatory emesis and nausea [12].
Discussion
ASCO and NCCN guidelines for the management of CINV are generally concordant in their recommendations, with some dissimilarity stemming from the MASCC/ESMO recommendations. Perhaps the biggest update is the use of the so-called quadruple therapy for HEC in the ASCO and NCCN guidelines, which incorporates olanzapine into the backbone of a 5-HT3 RA, NK1 RA, and dexamethasone. It should be noted that NCCN first included olanzapine in their recommendations as part of their previous update in 2017 [14]. This update was informed by a phase III, double-blind randomized control trial (RCT) which randomized 380 patients (primarily women with breast cancer) receiving AC chemotherapy to either a four-drug regimen (5-HT3 RA, NK1 RA, dexamethasone, and olanzapine) or an identical three-drug regimen without olanzapine, where the primary endpoint was no nausea [15]. The four-drug regimen showed superior complete response rates in the acute (86% vs. 65%, P < 0.001) and delayed phases (67% vs. 52%, P = 0.007). This article was released after MASCC/ESMO’s guidelines had already been updated, which rationalizes MASCC/ESMO’s recommendation to use olanzapine for breakthrough CINV only.
The routine addition of olanzapine to HEC antiemetic regimens would come at a minimal incremental cost, with prices of generic brands listed at $8.50 CAD per dose (both 5-mg and 10-mg doses) [11]. Despite the minimal cost implications, sedation is a potential barrier to common use of olanzapine, particularly among elderly patients. In the RCT by Navari et al., olanzapine was found to significantly increase rates of sedation when compared to the placebo, with 5% of patients experiencing significantly increased sedation relative to baseline [15]. In a phase II dose-finding RCT by Hashimoto et al., patients with a median age of 57 (n = 153) receiving 5 mg of olanzapine had higher rates of complete response than those receiving a 10-mg dose (85.7% vs. 77.6%), with lower rates of sedation (45.5% vs. 53.3%) [16]. Although ASCO and NCCN continue to recommend 10-mg doses of olanzapine, a 5-mg dose may be reasonable on the basis of this data.
Similar to the dosing of olanzapine, subtleties in the administration of dexamethasone exist for the treatment of delayed CINV resulting from AC regimens. ASCO no longer recommends the administration of dexamethasone on days 2–4 following AC chemotherapy, whereas MASCC/ESMO and NCCN (which do not distinguish between AC vs. non-AC HEC regimens) state that administration can continue. ASCO followed the use of dexamethasone in two RCTs testing the effectiveness of NK1 RAs in patients on AC regimens, in which dexamethasone was only administered on day 1 [17, 18]. MASCC/ESMO cited a RCT by Roila et al. which compared the effectiveness of aprepitant against dexamethasone in the prevention of delayed CINV after AC regimens, in which the complete response rate was identical (79.5%, P < 0.01) in both groups between days 2 and 5 [19]. These results led MASCC/ESMO to recommend the administration of either aprepitant or dexamethasone on days 2 and 3 following chemotherapy. It should be noted that such steroid-sparing approaches are desirable to avoid side effects, such as insomnia, indigestion, agitation, appetite, weight gain, and acne [20].
MASCC/ESMO’s recommendation of either dexamethasone and aprepitant or dexamethasone and metoclopramide on days 2–4 for cisplatin-treated patients was informed by a randomized, double-blind study assessing the superiority of dexamethasone and aprepitant over dexamethasone and metoclopramide in this patient subgroup (n = 284), in which it was found that complete response rates did not significantly differ between the two groups (80.3% vs. 82.5%, P < 0.4) [21]. The lack of apparent advantage of dexamethasone and aprepitant over dexamethasone and metoclopramide prompted the recommendation of both regimens.
Another notable change in the ASCO, MASCC/ESMO, and NCCN guidelines is the addition of an NK1 RA in the treatment of CINV resulting from MEC regimens containing carboplatin AUC greater than or equal to 4 mg/mL/min. All organizations cited a multicenter, double-blind RCT conducted by Hesketh et al., which assessed the effectiveness of rolapitant (an NK1 RA) in a subgroup of patients taking carboplatin (n = 401) [22]. The rolapitant group achieved significantly higher incidences of complete response in the delayed phase (82.3% vs. 65.6%, P < 0.001) and overall CINV (80.2% vs. 64.6%, P < 0.001) compared to placebo. An additional randomized, double-blind phase III trial by Weinstein et al. evaluating the acute use of fosaprepitant in patients receiving MEC regimens (n = 1015) was cited by each organization; the inclusion of fosaprepitant significantly improved rates of complete response in both the delayed (78.9% vs. 68.5%, P < 0.001) and overall (77.1% vs. 66.9%, P < 0.001) phases [23]. Finally, a randomized, double-blind trial by Yahata et al. of gynecologic cancer patients receiving paclitaxel and carboplatin (n = 297) was cited by ASCO and MASCC/ESMO, where the proportion of patients with no vomiting (78.2 vs. 54.8%, P < 0.0001) and no significant nausea (85.4 vs. 74.7%, P = 0.014) was significantly higher in the aprepitant group than in the control group [24].
ASCO, MASCC/ESMO, and NCCN recommend a single antiemetic for the treatment of acute CINV for low emetic risk regimens. No updates have been made to these regimens since the previous guidelines, with the exception of ASCO which now includes a 5-HT3 RA. ASCO and NCCN both used consensus rather than clinical evidence to support this recommendation. MASCC/ESMO cited a prospective cohort study assessing the effectiveness of granisetron in patients receiving low emetic risk agents and found that patients treated with granisetron had lower unadjusted incidences of acute emesis than those treated with placebo (3.9% vs. 19.0%, P = 0.017) [25]. Due to a lack of supporting literature, the three organizations do not recommend antiemetics for delayed CINV caused by low emetic risk regimens; similarly, antiemetics are not recommended for minimal emetic risk regimens. This lack of evidence for the management of CINV in these low- and minimal-risk settings indicates a potential area of future research.
It is important to note that differences between CINV guidelines of each organization reflect the information that was available at the time of publication. ASCO and NCCN guidelines were updated in 2017 and 2018, respectively, whereas MASC/ESMO’s guidelines were first formulated during a 2015 conference and subsequently published in 2016.
Patterns of practice
The recent CINV practice guidelines published by ASCO, NCCN, and MASC/ESMO provide healthcare providers, individual institutions, and LHINs the opportunity to update their current treatment recommendations. Indeed, a low level of adherence to guidelines has been observed in the management of CINV. For example, a retrospective chart review of patient records and prescription documents was conducted on patients beginning their first cycle of chemotherapy (all emetic classes) between November 2008 and April 2009 (n = 299) to assess levels of adherence to MASCC/ESMO guidelines [26]. Surprisingly, only 61% and 11% of patients received guideline-adherent prophylaxis for acute and delayed CINV respectively. As demonstrated in a prospective observational study of 1295 patients receiving HEC and MEC regimens, individuals who are prescribed guideline-consistent antiemetics have less CINV than those who are prescribed guideline-inconsistent regimens [27]. Considering the potential implications of CINV on quality of life and adherence to chemotherapy, healthcare providers should strive to follow practice-based guidelines as closely as possible.
Potential interventions to improve adherence of healthcare providers to various clinical practice guidelines have been proposed. A study by Mertens et al. found that distribution of ASCO guidelines and adherence data, along with information provided by expert lecturers, did not increase guideline-adherent practices among physicians [28]. However, physicians were more likely to engage in compliant practices when immediate patient outcomes were reported following guideline-non-compliant clinical care. An additional retrospective study by Bruce et al. assessed the effectiveness of an intervention that included direct, confidential feedback to HCPs on the appropriateness of their chemotherapeutic prescriptions [29]. A significant decrease in prescribing errors was observed over a 4-week period, from the pre- to post-intervention phases (7% vs. 3.9%, P < 0.001). Hence, direct feedback to healthcare providers may not only improve adherence to practice guidelines but also reduce prescription errors.
Alternative antiemetics
It is acknowledged that evidence-based guidelines for the use of complementary and alternative medicine (CAM), as well as medicinal cannabis in the setting of CINV, are lacking [30]. However, the use of acupuncture has been of recent interest. In a 2015 randomized trial by Rithirangsriroj et al., women receiving platinum-based chemotherapy for gynecologic cancers (n = 70) who were randomized to receive acupuncture had significantly higher rates of complete response (no emesis, no nausea, and no use of additional antiemetic drugs) when compared to those randomized to ondansetron (52.8% vs. 35.7%, P = 0.02) [31]. This article was mentioned in ASCO’s recent update, but acupuncture was not recommended as an alternative antiemetic; this is likely due to the small sample size of the trial, the concurrent use of dexamethasone on days 1–3 in both arms of the study, as well as lack of generalizability of results.
Given the lack of high-quality clinical trials to prove efficacy of cannabinoid and various CAM products as anti-emetic agents, the potential for toxicity and drug-drug interactions must be carefully weighted against their potential benefits. Since the use of recreational cannabis is already high among cancer patients [32] with possible sedation, psychosis and other side effects [33], efforts to standardize dosing and to study cannabis as a potential anti-emetic agent should be undertaken.
Conclusion
Overall, the recommendations provided by ASCO, NCCN, and MASCC/ESMO have a relatively high degree of concordance, with dissimilarities that can be attributed to the literature available at the time of publication. Potential areas for future research include the treatment of CINV following low and minimal emetic risk regimens, as well as the role of CAM in the prevention of CINV.
References
Coates A, Abraham S, Kaye SB, Sowerbutts T, Frewin C, Fox RM, Tattersall MHN (1983) On the receiving end--patient perception of the side-effects of cancer chemotherapy. Eur J Cancer Clin Oncol 19:203–208
Griffin AM, Butow PN, Coates AS, Childs AM, Ellis PM, Dunn SM, Tattersall MHN (1996) On the receiving end. V: patient perceptions of the side effects of cancer chemotherapy in 1993. Ann Oncol Off J Eur Soc Med Oncol 7:189–195
Kuchuk I, Bouganim N, Beusterien K et al (2013) Patient perceptions about potential side effects and benefits from chemotherapy agents. J Clin Oncol 31:6595–6595. https://doi.org/10.1200/JCO.2013.31.15_SUPPL.6595
Matzka M, Köck-Hódi S, Jahn P, Mayer H (2018) Relationship among symptom clusters, quality of life, and treatment-specific optimism in patients with cancer. Support Care Cancer 26:1–9. https://doi.org/10.1007/s00520-018-4102-8
Grunberg SM, Osoba D, Hesketh PJ, Gralla RJ, Borjeson S, Rapoport BL, du Bois A, Tonato M (2005) Evaluation of new antiemetic agents and definition of antineoplastic agent emetogenicity—an update. Support Care Cancer 13:80–84. https://doi.org/10.1007/s00520-004-0718-y
Hickok JT, Roscoe JA, Morrow GR, Bole CW, Zhao H, Hoelzer KL, Dakhil SR, Moore T, Fitch TR (2005) 5-hydroxytryptamine-receptor antagonists versus prochlorperazine for control of delayed nausea caused by doxorubicin: a URCC CCOP randomised controlled trial. Lancet Oncol 6:765–772. https://doi.org/10.1016/S1470-2045(05)70325-9
Navari RM (2015) Treatment of breakthrough and refractory chemotherapy-induced nausea and vomiting. Biomed Res Int 2015:1–6. https://doi.org/10.1155/2015/595894
Escobar Y, Cajaraville G, Virizuela JA, Álvarez R, Muñoz A, Olariaga O, Tamés MJ, Muros B, Lecumberri MJ, Feliu J, Martínez P, Adansa JC, Martínez MJ, López R, Blasco A, Gascón P, Calvo V, Luna P, Montalar J, del Barrio P, Tornamira MV (2015) Incidence of chemotherapy-induced nausea and vomiting with moderately emetogenic chemotherapy: ADVICE (Actual Data of Vomiting Incidence by Chemotherapy Evaluation) study. Support Care Cancer 23:2833–2840. https://doi.org/10.1007/s00520-015-2809-3
Tamura K, Aiba K, Saeki T et al (2017) Breakthrough chemotherapy-induced nausea and vomiting: report of a nationwide survey by the CINV Study Group of Japan. Int J Clin Oncol 22:405–412. https://doi.org/10.1007/s10147-016-1069-7
Navari RM, Nagy CK, Gray SE (2013) The use of olanzapine versus metoclopramide for the treatment of breakthrough chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Support Care Cancer 21:1655–1663. https://doi.org/10.1007/s00520-012-1710-6
Hesketh PJ, Kris MG, Basch E, Bohlke K, Barbour SY, Clark-Snow RA, Danso MA, Dennis K, Dupuis LL, Dusetzina SB, Eng C, Feyer PC, Jordan K, Noonan K, Sparacio D, Somerfield MR, Lyman GH (2017) Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 35:3240–3261. https://doi.org/10.1200/JCO.2017.74.4789
Ettinger DS, Berger MJ, Aston J, et al (2018) NCCN clinical practice guidelines in oncology antiemesis version 3.2018. Natl Compr Cancer Care Netw
Roila F, Molassiotis A, Herrstedt J, Aapro M, Gralla RJ, Bruera E, Clark-Snow RA, Dupuis LL, Einhorn LH, Feyer P, Hesketh PJ, Jordan K, Olver I, Rapoport BL, Roscoe J, Ruhlmann CH, Walsh D, Warr D, van der Wetering M, participants of the MASCC/ESMO Consensus Conference Copenhagen 2015 (2016) 2016 MASCC and ESMO guideline update for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients. Ann Oncol 27:v119–v133. https://doi.org/10.1093/annonc/mdw270
Ettinger DS, Berger MJ, Aston J, et al (2017) NCCN clinical practice guidelines in oncology antiemesis version 2.2017. Natl Compr Cancer Care Netw
Navari RM, Qin R, Ruddy KJ, Liu H, Powell SF, Bajaj M, Dietrich L, Biggs D, Lafky JM, Loprinzi CL (2016) Olanzapine for the prevention of chemotherapy-induced nausea and vomiting. N Engl J Med 375:134–142. https://doi.org/10.1056/NEJMoa1515725
Hashimoto H, Yanai T, Nagashima K, Tsuda N, Horinouchi H, Tomomi T (2016) A double-blind randomized phase II study of 10 versus 5 mg olanzapine for emesis induced by highly emetogenic chemotherapy with cisplatin [abstract]. J Clin Oncol 34:10111
Aapro M, Rugo H, Rossi G, Rizzi G, Borroni ME, Bondarenko I, Sarosiek T, Oprean C, Cardona-Huerta S, Lorusso V, Karthaus M, Schwartzberg L, Grunberg S (2014) A randomized phase III study evaluating the efficacy and safety of NEPA, a fixed-dose combination of netupitant and palonosetron, for prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy. Ann Oncol 25:1328–1333. https://doi.org/10.1093/annonc/mdu101
Warr DG, Hesketh PJ, Gralla RJ, Muss HB, Herrstedt J, Eisenberg PD, Raftopoulos H, Grunberg SM, Gabriel M, Rodgers A, Bohidar N, Klinger G, Hustad CM, Horgan KJ, Skobieranda F (2005) Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol 23:2822–2830. https://doi.org/10.1200/JCO.2005.09.050
Roila F, Ruggeri B, Ballatori E, Del Favero A, Tonato M (2014) Aprepitant versus dexamethasone for preventing chemotherapy-induced delayed emesis in patients with breast cancer: a randomized double-blind study. J Clin Oncol 32:101–106. https://doi.org/10.1200/JCO.2013.51.4547
Vardy J, Chiew KS, Galica J, Pond GR, Tannock IF (2006) Side effects associated with the use of dexamethasone for prophylaxis of delayed emesis after moderately emetogenic chemotherapy. Br J Cancer 94:1011–1015. https://doi.org/10.1038/sj.bjc.6603048
Roila F, Ruggeri B, Ballatori E, Fatigoni S, Caserta C, Licitra L, Mirabile A, Ionta MT, Massidda B, Cavanna L, Palladino MA, Tocci A, Fava S, Colantonio I, Angelelli L, Ciuffreda L, Fasola G, Zerilli F, on behalf of the Italian Group for Antiemetic Research (2015) Aprepitant versus metoclopramide, both combined with dexamethasone, for the prevention of cisplatin-induced delayed emesis: a randomized, double-blind study. Ann Oncol 26:1248–1253. https://doi.org/10.1093/annonc/mdv132
Hesketh PJ, Schnadig ID, Schwartzberg LS, Modiano MR, Jordan K, Arora S, Powers D, Aapro M (2016) Efficacy of the neurokinin-1 receptor antagonist rolapitant in preventing nausea and vomiting in patients receiving carboplatin-based chemotherapy. Cancer 122:2418–2425. https://doi.org/10.1002/cncr.30054
Weinstein C, Jordan K, Green SA, Camacho E, Khanani S, Beckford-Brathwaite E, Vallejos W, Liang LW, Noga SJ, Rapoport BL (2016) Single-dose fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting associated with moderately emetogenic chemotherapy: results of a randomized, double-blind phase III trial. Ann Oncol 27:172–178. https://doi.org/10.1093/annonc/mdv482
Yahata H, Kobayashi H, Sonoda K, Shimokawa M, Ohgami T, Saito T, Ogawa S, Sakai K, Ichinoe A, Ueoka Y, Hasuo Y, Nishida M, Masuda S, Kato K (2016) Efficacy of aprepitant for the prevention of chemotherapy-induced nausea and vomiting with a moderately emetogenic chemotherapy regimen: a multicenter, placebo-controlled, double-blind, randomized study in patients with gynecologic cancer receiving paclitaxel and carboplatin. Int J Clin Oncol 21:491–497. https://doi.org/10.1007/s10147-015-0928-y
Keat CH, Phua G, Abdul Kassim MS, Poh WK, Sriraman M (2013) Can granisetron injection used as primary prophylaxis improve the control of nausea and vomiting with low- emetogenic chemotherapy? Asian Pac J Cancer Prev 14:469–473
Burmeister H, Aebi S, Studer C, Fey MF, Gautschi O (2012) Adherence to ESMO clinical recommendations for prophylaxis of chemotherapy-induced nausea and vomiting. Support Care Cancer 20:141–147. https://doi.org/10.1007/s00520-010-1079-3
Gilmore JW, Peacock NW, Gu A, Szabo S, Rammage M, Sharpe J, Haislip ST, Perry T, Boozan TL, Meador K, Cao X, Burke TA (2014) Antiemetic guideline consistency and incidence of chemotherapy-induced nausea and vomiting in US community oncology practice: INSPIRE Study. J Oncol Pract 10:68–74. https://doi.org/10.1200/JOP.2012.000816
Mertens WC, Higby DJ, Brown D, Parisi R, Fitzgerald J, Benjamin EM, Lindenauer PK (2003) Improving the care of patients with regard to chemotherapy-induced nausea and emesis: the effect of feedback to clinicians on adherence to antiemetic prescribing guidelines. J Clin Oncol 21:1373–1378. https://doi.org/10.1200/JCO.2003.08.118
Bruce K, Hall L, Castelo S, Evans M, Frangoul H (2012) Direct provider feedback to decrease chemotherapy ordering errors: the “gray envelope” initiative. Pediatr Blood Cancer 59:1330–1331. https://doi.org/10.1002/pbc.24224
Smith LA, Azariah F, Lavender VT, Stoner NS, Bettiol S (2015) Cannabinoids for nausea and vomiting in adults with cancer receiving chemotherapy. Cochrane Database Syst Rev:CD009464. doi:https://doi.org/10.1002/14651858.CD009464.pub2
Rithirangsriroj K, Manchana T, Akkayagorn L (2015) Efficacy of acupuncture in prevention of delayed chemotherapy induced nausea and vomiting in gynecologic cancer patients. Gynecol Oncol 136:82–86. https://doi.org/10.1016/j.ygyno.2014.10.025
Pergam SA, Woodfield MC, Lee CM, Cheng GS, Baker KK, Marquis SR, Fann JR (2017) Cannabis use among patients at a comprehensive cancer center in a state with legalized medicinal and recreational use. Cancer 123(22):4488–4497. https://doi.org/10.1002/cncr.30879
Kelly BF, Nappe TM (2018) Toxicity, Cannabinoids
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TM attended an advisory board for Purdue Pharma. EC attended an advisory board for Purdue Pharma and served as a moderator for a Purdue Pharma dinner seminar. KJJ served as a consultant for and/or attended advisory boards for Genomic Health Inc, Novartis, Purdue Pharma and Roche.
Rights and permissions
About this article
Cite this article
Razvi, Y., Chan, S., McFarlane, T. et al. ASCO, NCCN, MASCC/ESMO: a comparison of antiemetic guidelines for the treatment of chemotherapy-induced nausea and vomiting in adult patients. Support Care Cancer 27, 87–95 (2019). https://doi.org/10.1007/s00520-018-4464-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4464-y