Abstract
Purpose
Traveling for cancer care is difficult as patients might be suffering from the side effects of treatment, need to cover additional costs, and face disruption of daily life. The aim of this review was to synthesize the evidence on travel needs and experiences during cancer treatment from the point of view of patients and their families.
Methods
This is a systematic review of the literature. The PRISMA statement was used to guide the reporting of the methods and findings. We searched for peer-reviewed articles in MEDLINE, CINAHL PLUS, and Web of Science and selected articles based on the following criteria: focused on patients and their families; presented findings from empirical studies; and examined travel and transport experiences for cancer screening, treatment, and related care. The MMAT was used to assess the quality of the studies.
Results
A total of 16 articles were included in the review. Most of the studies used a qualitative design, were carried out in high-income countries and were conducted more than 10 years ago. Several problems were reported regarding travel and relocation: social and physical demands of transport, travel, and relocation; life disruption and loss of daily routines; financial impact; and anxieties and support needs when returning home.
Conclusions
Patients and carers consistently reported lack of support when traveling, relocating, and returning home. Future research needs to explore patient experiences under current treatment protocols and healthcare delivery models, in a wider range of geographical contexts, and different stages of the patient pathway.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Many cancer patients around the world will need to travel for at least one part of their treatment [1]. The need to travel is often produced by the fact that cancer care is offered in specialist centres, which are not always located close to patients’ place of residence [2, 3]. Patients might need to travel to have all of their care in specialist centres or only for specific aspects of their treatment (i.e., surgery) [4]. In some instances, patients and their families might choose to travel and relocate to access care in hospitals they believe can provide a higher quality of care [5, 6].
The literature has indicated that travel during cancer treatment is difficult as patients might be dealing with side effects of treatment such as fatigue or nausea [7, 8]. Travel is also expensive and leads to disruption of normal daily life, family separation, and the interruption of employment and education [1, 9]. In the case of patients who have to relocate temporarily in another place to access treatment, long periods away from home can produce feelings of loneliness, boredom, and home sickness [10, 11]. As many cancers move into the umbrella of long-term conditions, these factors may become more relevant for patients and carers.
Despite the difficulties associated with traveling, some studies have found that patients are willing to travel long distances to obtain a cancer diagnosis and access care [5, 6]. Some patients and families prefer to relocate and stay close to the specialist centre during treatment, as knowing they can access specialist care at any time and in cases of complication, gives them a sense of security [8]. Studies have also found that proximity to the specialist centre means that patients are able to interact with other patients (‘peers’), forming helpful support groups during treatment [12].
Various programmes and interventions have been implemented to limit patients’ travel for treatment (i.e. telemedicine, community-based care, outreach care) or support for patients as they travel (i.e., financial support, patient navigator roles) [13, 14], with varying degrees of success. Patients’ travel needs and preferences vary in relation to age, diagnosis, prognosis, place of residence, and occupation and might change throughout stages of treatment [5]. Therefore, in-depth analysis of patients’ and carers’ views and experiences of travel during treatment is required to inform and shape care delivery.
Some reviews have explored travel for cancer care, but these have mainly focused on the impact of travel time and distance to a specialist centre on patients’ choice, access, adherence to treatment, and outcomes [4, 15, 16]. Travel costs have also been explored, but normally in relation to treatment delays or interruptions [15]. To our knowledge, there is only one review that examined the impact of travel on cancer patients’ experiences, but it reviewed literature published 20 years ago [17]. The aim of our review is to address this gap in knowledge by synthesizing the evidence on travel needs and experiences during cancer treatment from the point of view of patients and their families. We hope the findings from this review can be used to tailor care and patient support services.
Methods
Design
This is a systematic review of the literature based on peer-reviewed academic articles. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement was used to guide the reporting of the methods and findings [18]. The review was registered with PROSPERO (Ref: CRD42017078530).
Research questions
The review sought to explore the following questions:
-
1.
How do patients and family members describe their experiences of travel during screening and cancer treatment?
-
2.
What are the main problems encountered by traveling patients and their families?
-
3.
How does the need to travel affect potential patients’ and patients’ treatment experiences?
-
4.
What is the financial impact of traveling for cancer treatment?
-
5.
Are there any initiatives or support programs described to assist patients and family members with travel needs?
Search strategy
We used the PICOS (Population, Intervention, Comparison, Outcomes, Setting) framework [19] to develop the search strategy (Appendix 1). We conducted a review of published literature using multiple databases: MEDLINE, CINAHL PLUS, and Web of Science. Details of the online search strategy can be found in Appendix 1. The searches were conducted in October 2017. Results were combined into RefWorks and duplicates were removed. The reference lists of included articles were screened to identify additional relevant publications.
Selection
Two of the authors screened the articles in three phases (title, abstract, and full text) based on the following inclusion criteria: (1) the article was published in a peer-reviewed journal, (2) the study focused on patients (or potential patients) receiving cancer treatment and their families, (3) the study presented findings from empirical studies, and (4) the study examined travel and transport experiences for cancer screening, treatment, and related care (including local, national, and international travel). Disagreements were discussed until consensus was reached. We did not apply any restrictions in terms of language or date of publication.
Data extraction and management
The included articles were analyzed using a data extraction form developed in REDCap (Research Electronic Data Capture). The categories used in the data extraction form are summarized in Appendix 2. The form was developed after the initial screening of full-text articles. It was then piloted independently by two of the authors using a random sample of five articles. Disagreements were discussed until consensus was reached. The form was changed based on the findings from the pilot.
Data synthesis
Data were exported from REDCap and the main article characteristics were synthesized. The REDCap report presented quantitative summaries of some of the entries in our data extraction form (for details, see Appendix 2). The information entered in free text boxes was exported from REDCap and analyzed using framework analysis [20]. The themes were based on our research questions, but we were also sensitive to themes emerging from the data.
Quality assessment
We used the Mixed Methods Appraisal Tool (MMAT) to assess the quality of the articles [21, 22]. Two of the authors rated these articles independently. In cases of disagreement, the raters discussed their responses until consensus was reached. Inter-rater reliability was calculated using the kappa statistic [23].
Results
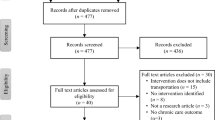
Identification of articles
The initial search yielded 4117 published articles (Fig. 1). These were screened based on title and type of article, resulting in 410. Screening based on abstracts left 118 articles for full-text review. This phase in screening led to 16 articles that met the inclusion criteria. We excluded articles that examined distance to specialist centres where care was delivered or cost of travel for treatment, but did not explore experiences of travel or relocation for care.
The MMAT tool was used by two of the authors to assess the quality of the 16 studies (see Table 1 for study-specific appraisal results). Inter-rater agreement was 87% with a Cohen’s kappa indicating near perfect agreement (k = 0.83). Overall, most studies covered three out of four criteria. A common limitation found in the articles was the low response rate in quantitative studies and lack of reflection on the researcher’s influence over the findings in the qualitative studies.
Main characteristics of included articles
The characteristics of the 16 articles included in the review are presented in Table 1. The articles were published between 1995 and 2015. All articles were published in English. The locations of the studies included Canada (4 studies), Australia (4 studies), the UK (4 studies), the USA (2 studies), New Zealand (1 study), and Argentina (1 study). Most of the studies aimed to explore patients’ care experiences and explored travel as a component of these experiences (8 studies). Three studies focused specifically on the travel experiences of patients from remote rural areas who had to travel long distances to access care [9, 24, 28]. Three studies were interested in understanding patients’ needs after completing treatment in a different location and returning home [7, 12]. Two studies examined patients’ views of transport services [29, 30].
Study designs and methods
Most of the studies included in the review (12 studies) used a qualitative research design. Three studies were quantitative and one study was mixed-methods. In the qualitative studies, the most commonly used method for data collection was interviews. In two cases, interviews were combined with focus groups and another study used interviews and drawings. All of the quantitative studies relied on surveys to collect data. The mixed-methods study combined a survey with focus groups.
Study samples
Almost half of the studies (seven studies) recruited patients. Five studies included both patients and family members. Three studies only focused on the views of family members and one study included patients, carers, and healthcare professionals. In most cases, patients received treatment for a wide range of cancer diagnoses. Three studies only included patients with hematological malignancies [3, 9, 12]. Fitch et al. [26, 27] focused on patients with breast or prostate cancer and Davis et al. [24] only recruited patients with breast cancer. Three studies focused on the experiences of paediatric patients and their parents [8, 10, 11].
In terms of the stage of treatment of patients included in the studies, most patients were in active treatment (12 studies), one study focused on patients receiving end of life care, and three studies documented the experiences of cancer survivors. Even though we included studies that focused on screening for cancer in our inclusion criteria, we did not find any articles that examined patients’ experiences of travel for screening.
Modes and types of travel
Most of the patients and carers in the studies included in the review traveled by car. In the case of one study, patients traveled by car to the city where they received treatment and then used public transport to move around the city [28]. In the case of four studies, patients used ambulance transport services [25, 26, 29, 30]. Patients traveled by plane in one study where mothers migrated to the USA to obtain paediatric oncology treatment [10]. Families traveled by bus in another study on the experiences of families migrating from Bolivia and Paraguay to Argentina for paediatric oncology treatment [11].
One of the aims of the review was to explore the characteristics of the travel endured by patients and their carers, but most of the studies did not describe the duration, types, or frequency of travel. Wilkes [28] indicated that the patients included in the study traveled between 120 to 450 km for treatment. Davis et al. [24] reported that more than half of the patients included in the study traveled at least 200 km.
Problems identified by patients and their families
We analyzed the findings of the 16 studies to identify the main problems reported by patients and their families while traveling for care and returning home after treatment. We have listed these in Table 2. We were able to group the problems in four main categories: (1) the social and physical demands of transport, travel, and relocation; (2) life disruption and loss of daily routines; (3) financial impact; and (4) anxieties and support needs when returning home.
Long journeys contributed to patients’ exhaustion and were difficult to endure if the patient felt nauseous or in pain. Two studies found important limitations with regard to the ambulance service transport, such as long waiting times for the transport, missing appointments, and the need to endure long journeys home due to transport delays [25, 29]. Problems with ambulance services were also highlighted by Ingleton et al. [30] in the case of emergencies. Relocation was difficult for most patients, as many had to travel to unfamiliar cities and did not have enough information regarding travel and accommodation [11, 24, 28].
An interesting finding in relation to relocation was McGrath’s [9] proposal to distinguish between travel-based relocation and accommodation-based relocation. According to the author, most of the attention is normally placed on patients and family members who move close to the centre where they will receive cancer treatment (accommodation-based relocation). However, there are other patients and carers who experience more temporal types of relocation (i.e., only a few days) who encounter different problems and have other needs. According to McGrath [9], the identification of different types of relocation can help tailor care and support services according to patients’ and their carers’ needs.
More than half of the studies mentioned the impact of traveling for treatment on patients’ and families’ daily routines. The need to travel long distances for treatment led to family separation [1, 8, 11, 24]. Patients and carers needed to take time away from work [2, 7, 8, 11, 24, 28]. In cases where the patients were children, they had to take time away from school [2, 11]. Patients and carers with young children needed to arrange childcare for children who stayed at home [8]. Patients living in rural areas reported difficulties associated with leaving their homes, crops, and animals for long periods of time [9, 26].
A considerable number of studies (11 studies) mentioned the financial impact of traveling and relocating for cancer treatment. Patients and carers reported an increase in family expenses to cover the costs of travel (fuel, parking, train, or airplane tickets); relocation (accommodation, meals, and other expenses in the city where care was received); and arrangements required to take care of home responsibilities while they were away (i.e., childcare, caring for animals) [2, 7, 9, 11, 12, 27, 28]. Patients also reported a reduction in family income due to the interruption or loss of employment of the patient and/or the carer [2, 7, 8, 11, 24, 28]. In cases where financial support was available, patients indicated it was not enough to cover all expenses [26].
Three studies explored the experiences of patients and carers who returned home after treatment [7, 12, 30]. These studies pointed to problems experienced by patients and their families when trying to manage the patient’s care in the home, which included lack of knowledge, the need to modify the home, or fear regarding what to do in cases of medical emergencies. Patients’ perception of local healthcare teams was often negative, as they believed staff did not have enough knowledge to manage their condition. Furthermore, some patients believed the communication between the specialist centres and their local centres was poor. McGrath [12] found that carers did not receive the support they needed from other family members and friends when returning home (see also Payne et al. [1]). In the study by Howard [7], patients also reported not receiving information on support groups they could access close to home after completing treatment.
Support
The main type of support requested by patients and carers was financial support to cover the costs of travel and relocation [3, 7, 11, 26, 28]. Davis et al. [24] found that only 39% of the patients included in their study had financial support. Wilkes also reported a low number of patients receiving financial assistance, and both Howard [7] and Vindrola-Padros and Whiteford [11] indicated that many patients included in their studies were not eligible for government funding to cover travel costs. Fitch [26] highlighted that a cost reimbursement scheme existed for traveling patients, but expenses were not always covered in a timely manner.
The need for other types of support was also mentioned in some of the studies, such as emotional support and help for carers once the patient returned home after treatment [10, 12]. Patients were also interested in receiving information on how to access support groups in the community [10, 12]. Four studies proposed the use of telemedicine, in the form of online video consultations, as a way to support patients by reducing the frequency of travel [7, 9, 24, 25].
Limitations of the studies and future areas of research
The main study limitation mentioned in the articles included in the review was small sample size [2, 8, 24, 27]. One proposal was to carry out research with larger groups of patients and carers. Another proposed area for future research was the study of patients’ travel experiences across the entire pathway of care, including primary, secondary, and tertiary care [2]. Fitch [26] also argued that greater attention needs to be paid to the different ways in which patients cover the costs of travel and relocation and proposed comparing the experiences of patients across different reimbursement schemes. Alternative research designs were also proposed, including mixed-methods studies [3], a combination of retrospective and prospective samples of patients [25], and longitudinal studies capable of capturing changes in patient experience and needs over time [8].
Discussion
The aim of this review was to synthesize the evidence on experiences of travel from the point of view of cancer patients and their carers. Most of the studies we found were carried out in high-income countries, leaving the experiences of patients and families in other regions of the world largely unexplored. More than two thirds of the studies were carried out more than 10 years ago, pointing to the small amount of current research on this topic. This represents a limitation in our understanding of patient needs and experiences under more recent care delivery models, which might have tried to reduce the need to travel for specialist care and offer at least some parts of treatment closer to the patient’s home [31, 32].
Even though most of the studies included in the review explored experiences of travel within a wider analysis of patients’ experiences of care, we also found studies that addressed specific aspects of travel such as transport, focused on distinctive populations (i.e., patients in rural and remote areas), or concentrated on particular parts of the pathway of care (the return home after treatment and continuation of follow-up care in local facilities). We believe this not only points to the diversification of this field of study but also highlights gaps in research that remain, such as patients’ experiences of travel for screening and less frequent travel that might be carried out after treatment is complete, but where the patient still needs to visit the specialist centre. How is travel experienced and arranged after patients and their families have reintegrated themselves in their normal family routines?
Most of the studies included in the review used a qualitative design and one-time interviews were commonly used to capture patients’ and carers’ experience. This synchronic approach means that research is not capturing how patients’ and carers’ experiences change through time. As McGrath [12] argued, patients often indicate that experiences at diagnosis are not the same as those after treatment and needs change as they move through different stages of their care pathways. We need more information on how experiences of travel change not only as patients become more familiar with travel routes and demands, becoming more ‘proficient travelers’, but also as the characteristics of travel (length, duration, frequency) change to adapt to modifications in treatment protocols.
The prevalence of interviews over other methods also means that experience is only being captured in relation to the perceptions of interviewees communicated during the interview encounter. This means that research has not been able to capture how travel and relocation are performed in practice. The combination of interviews with observations carried out during travel, medical consultations, and places of relocation would provide a richer picture of the experiences of patients and carers. Researchers might also consider accompanying patients and carers on their journeys to fully grasp the nuances of traveling and relocating for cancer treatment.
Our analysis of the findings of the studies included in this review allowed us to create four main categories of problems faced by patients and carers when traveling for cancer treatment: (1) the social and physical demands of transport, travel, and relocation; (2) life disruption and loss of daily routines; (3) financial impact; and (4) anxieties and support needs when returning home. An important finding was that, despite these difficulties, most patients adhered well to their treatment protocols. As cancer becomes a long-term condition in many parts of the world, an important future area of research will need to examine if this adherence persists despite the problems associated with travel.
Clinical implications
Additional work is required to support traveling patients and their families and consider that they have unique needs that can be addressed by professionals in charge of their care. Howard et al. [7], for instance, propose the creation of administrative roles such as patient navigators who can assist patients with making travel arrangements. Another suggestion was the establishment of appointment times convenient for those traveling long distances to the specialist centre [26]. Financial support should also be highlighted as an area that requires attention as the increase in family expenses as a result of traveling and relocating for treatment was mentioned frequently by patients.
Another important area covered in this review was not only patients’ and carers’ experiences of returning home after treatment in a different city, which meant a return to normal life, but also additional burden placed on carers. The literature on cancer caregivers has pointed to the need to focus on caregivers’ quality of life to prevent burnout [33]. The findings from this review indicate that additional research is needed to understand how caring demands change once patients and carers return home after treatment.
Several of the studies found that, despite being home, patients and carers continued to face anxiety and fear regarding the patient’s condition and care. This situation was mainly produced by patients’ and carers’ perception that local care was not of the same quality as care delivered at the specialist centre. We believe additional work needs to be carried out on these perceptions of care to understand how they might influence patients’ and carers’ decision to seek care in cities that are far away despite having other care options closer to home. Furthermore, as several countries are now advocating in favour of the delivery of follow-up care and some treatments closer to the patients’ home, we need to understand how this locally delivered care is perceived and experienced by patients and carers.
Limitations of the review
This review has a series of limitations. The literature search for academic articles was carried out in October 2017, so any articles published after this date were not included. Furthermore, although we employed multiple broad search terms, it is possible that we missed articles that did not use these terms. We did not include grey literature, thus potentially excluding studies that have not been published in academic journals. The tool we used to assess the quality of the studies, the MMAT, also has limitations and these have been discussed elsewhere [34, 35].
Conclusions
As healthcare models around the world are changing to become more patient-centred and respond better to patient needs, it is essential to understand patients’ and carers’ experiences of care. Since many cancer patients will need to travel for at least one part of their treatment, our exploration of experiences of care will need to include travel and relocation for care. In this review, we have synthesized the evidence on patients’ and carers’ travel experiences for cancer care in the attempt to highlight the main trends identified in the literature and propose future areas of research. The findings from this review have highlighted that patients and families encounter problems dealing with the social and physical demands of travel, travel and relocation expenses, and disruption with daily routines. Patients and carers also experience difficulties when they return home after treatment, as they are often left without support and information on how to manage the patient’s condition.
The findings of the review also pointed to gaps in knowledge that need to be addressed in future research. Most of the research on this topic was carried out more than 10 years ago, leaving experiences under current treatment protocols and healthcare delivery models unexplored. Most explorations of patient and carer experience were made at one time in the patient’s cancer journey, thus not being able to capture how experiences change as patients move through the different stages of the pathway. Research also needs to focus on the experiences of patients in middle- and low-income countries, who might be encountering different challenges when traveling and relocating for cancer care. We hope the findings of this review can help invigorate future research on this topic and, ultimately, improve the care delivered to patients and their carers.
References
Payne S, Jarrett N, Jeffs D, Brown L (2001) Implications of social isolation during cancer treatment. The implications of residence away from home during cancer treatment on patients’ experiences: a comparative study. Health Place 7(4):273–282
Fluchel MN, Kirchhoff AC, Bodson J, Sweeney C, Edwards SL, Ding Q, Stoddard GJ, Kinney AY (2014) Geography and the burden of care in pediatric cancers. Pediatr Blood Cancer 61(11):1918–1924
McGrath P, Holewa H (2012) Reconceptualising relocation for specialist treatment: insights from New Zealand. Support Care Cancer 20(3):499–505
Kelly C, Hulme C, Farragher T, Clarke G (2016) Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open 6:e013059
Zullig LL, Jackson GL, Provenzale D, Griffin JM, Phelan S, van Ryn M (2012) Transportation: a vehicle or roadblock to cancer care for VA patients with colorectal cancer? Clin Colorectal Cancer 11(1):60–65
Vindrola-Padros C, Brage E (2016) Child medical travel in Argentina: narratives of family separation and moving away from home. In: Ergler C, Kearns R, Witten K (eds) Children’s health and wellbeing in urban environments. Routledge, London, pp 128–144
Fuchsia Howard A, Smillie K, Turnbull K, Zirul C, Munroe D, Ward A, Tobin P, Kazanjian A, Olson R (2014) Access to medical and supportive care for rural and remote cancer survivors in northern British Columbia. J Rural Health 30(3):311–321
Shepherd EJ, Woodgate RL (2011) A journey within a journey: the lived experience of parents who do not live near their child’s tertiary cancer center. J Pediatr Oncol Nurs 28(4):231–243
McGrath P (2015) Overcoming the distance barrier in relation to treatment for haematology patients: Queensland findings. Aust Health Rev 39(3):344–350
Crom DB (1995) The experience of South American mothers who have a child being treated for malignancy in the United States. J Pediatr Oncol Nurs 12(3):104–112 discussion 113-4
Vindrola-Padros C, Whiteford L (2012) The search for medical technologies abroad: the case of medical travel and pediatric oncology treatment in Argentina. Technol Innov 14:25–38
McGrath P (2001) Returning home after specialist treatment for hematological malignancies: an Australian study. Fam Community Health 24(2):36–48
McGrath P (1998) Relocation for treatment for leukaemia: a description of need. Aust Health Rev 21(4):143–154
Zucca A, Boyes A, Newling G, Hall A, Girgis A (2011) Travelling all over the countryside: travel-related burden and financial difficulties reported by cancer patients in New South Wales and Victoria. Aust J Rural Health 19(6):298–305
Ambroggi M, Biasini C, Del Giovane C, Fornari F, Cavanna L (2015) Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist 20:1378–1385
Chamberlain C, Owen-Smith A, Donovan J, Hollingworth W (2016) A systematic review of geographical variation in access to chemotherapy. BMC Cancer 16:1–15
Payne S, Jarrett N, Jeffs D (2000) The impact of travel on cancer patients’ experiences of treatment: a literature review. Eur J Cancer Care (Engl) 9(4):197–203
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:332–336
Robinson KA, Saldanha I, McKoy N (2011) Development of a framework to identify research gaps from systematic reviews. J Clin Epidemiol 64(12):1325–1330
Gale N, Health G, Cameron E, Rashid S, Redwood S (2013) Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 13:117
Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, Seller R (2012) Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 49(1):47–53
Pluye P, Hong QN (2014) Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Ann Rev Public Health 35(1):29–45
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Davis C, Girgis A, Williams P, Beeney L (1998) Needs assessment of rural and remote women travelling to the city for breast cancer treatment. Aust N Z J Public Health 22(5):525–527
Atkinson J, Kennedy E, Goldsworthy S, Drummond S (2002) Patients’ cancer journeys in Kintyre—a qualitative study of the care, support and information needs of people with cancer and their carers. Eur J Oncol Nurs 6(2):85–92
Fitch MI, Gray RE, McGowan T, Brunskill I, Steggles S, Sellick S, Bezjak A, McLeese D (2003) Travelling for radiation cancer treatment: patient perspectives. Psycho-Oncology 12(7):664–674
Fitch MI, Gray RE, Mcgowan T, Brunskill I, Steggles S, Sellick S et al (2005) Travelling for radiation cancer treatment: patient satisfaction. Can Oncol Nurs J 15(2):107–119
Wilkes LM, White K, Mohan S, Beale B (2006) Accessing metropolitan cancer care services: practical needs of rural families. J Psychosoc Oncol 24(2):85–101
Hubbard G, Maguire R, Kidd L, Kearney N, Hilliam A (2006) Patient views of transport for cancer treatment. Eur J Oncol Nurs 10(5):391–395
Ingleton C, Payne S, Sargeant A, Seymour J (2009) Barriers to achieving care at home at the end of life: transferring patients between care settings using patient transport services. Palliat Med 23(8):723–730
Chan BA, Larkins SL, Evans R, Watt K, Sabesan S (2015) Do teleoncology models of care enable safe delivery of chemotherapy in rural towns? Med J Aust 203(10):406–6.e6
Kuntz G, Tozer JM, Snegosky J, Fox J, Neumann K (2014) Michigan oncology medical home demonstration project: first-year results. J Oncol Pract 10(5):294–297
Lapid MI, Atherton PJ, Kung S, Sloan JA, Shahi V, Clark MM, Rummans TA (2016) Cancer caregiver quality of life: need for targeted intervention. Psycho-Oncology 25:1400–1407
Crowe M, Sheppard L (2011) A review of critical appraisal tools show they lack rigor: alternative tool structure is proposed. J Clin Epidemiol 64(1):79–89
O’Cathain A, Murphy E, Nicholl J (2008) The quality of mized methods studies in health services research. J Health Serv Res Policy 13(2):92–98
Funding
This review emerged out of a collaborative relationship between CV-P and EB, which was funded in part by a Global Engagement Grant awarded by the UCL Global Engagement Office.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PC is co-investigator on a Janssen Pharma-sponsored study. CV-P and EB declare no conflicts of interest. This review emerged out of collaborative work between the authors that was funded by UCL Global Engagement Funds (provided by the UCL Global Engagement Office).
Rights and permissions
About this article
Cite this article
Vindrola-Padros, C., Brage, E. & Chambers, P. On the road and away from home: a systematic review of the travel experiences of cancer patients and their families. Support Care Cancer 26, 2973–2982 (2018). https://doi.org/10.1007/s00520-018-4266-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-018-4266-2