Abstract
Purpose
Chemotherapy-induced peripheral neuropathy (CIPN) limits the dose of chemotherapy and reduces patients’ quality of life. Goshajinkigan is a Japanese herbal medicine used to alleviate neuropathy and general pain. A clinical guideline for prevention and management of CIPN stated that the prophylactic efficacy of goshajinkigan against CIPN was inconclusive. We conducted a systematic review to examine whether goshajinkigan prevents CIPN in patients receiving neurotoxic chemotherapy.
Methods
We searched PubMed, EMBASE, Ichushi, and the Cochrane Central Register of Controlled Trials for eligible trials. Randomized controlled trials that examined the efficacy and safety of goshajinkigan for prevention of CIPN were included. Our primary outcomes were incidence of CIPN, response to chemotherapy, and adverse effects. We pooled data using a random effects model.
Results
We analyzed five trials involving a total of 397 patients. When evaluated with Neurotoxicity Criteria of Debiopharm, goshajinkigan was associated with reduced incidence of CIPN of grade ≥ 1 (risk ratio [RR] 0.43; 95% CI, 0.27 to 0.66) and grade 3 (RR 0.42; 95% CI, 0.25 to 0.71), but this beneficial association was not found for grade ≥ 2 of CIPN. Goshajinkigan was not associated with reduced incidence of CIPN when assessed with the National Cancer Institute Common Terminology Criteria for Adverse Events, or improved response to chemotherapy. Goshajinkigan was well tolerated based on one trial.
Conclusions
Goshajinkigan is unlikely to prevent CIPN in patients undergoing neurotoxic chemotherapy. Given the low quality and insufficient amount of the evidence, use of goshajinkigan as standard of care is not currently recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chemotherapy-induced peripheral neuropathy (CIPN) is a common treatment-related adverse effect. The prevalence of CIPN varies according to the type of chemotherapy, but is generally estimated to be 68 and 30% in the short and long term, respectively [31]. CIPN limits physical function and functional quality of life in cancer patients, leading to dose limiting of chemotherapy [25]. The economic impact of CIPN is also substantial, because CIPN leads to excess healthcare costs and resource use in addition to the impact of cancer treatment [30]. Given the negative influence of CIPN on every aspect of the lives of cancer patients, prevention of CIPN is needed.
Goshajinkigan, which is a Japanese herbal medicine empirically used to treat CIPN [12], is a mixture of extracts from ten raw botanical materials in fixed proportions [5] and has been used in Japan to treat diabetic neuropathy [33, 36], overactive bladder [15], and non-specific pain and numbness. A modest-sized, randomized trial in ovarian or endometrial cancer [16] and two observational studies in colorectal cancer [19, 37] suggest potential benefit of goshajinkigan for mitigation of CIPN. Some observational and animal studies have also suggested that goshajinkigan may prevent CIPN [2,3,4, 13, 17, 21, 23, 24, 35]. A clinical guideline for prevention and management of CIPN in adult cancer patients was published by the American Society of Clinical Oncology in 2014 [9]. In this guideline, goshajinkigan was mentioned, but its prophylactic efficacy on CIPN was considered inconclusive based on one randomized trial [26]. Randomized trials have been conducted to examine the effect of goshajinkigan for prophylaxis of CIPN, but results have been conflicting. To our knowledge, however, no systematic review has summarized these study results.
Herein, we conducted a systematic review and meta-analysis to assess the evidence on efficacy and safety of goshajinkigan for prevention of CIPN.
Materials and methods
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for reporting systematic reviews [22]. Our protocol was registered at PROSPERO (CRD42017062691). Using Medline [inception to August 15, 2017], EMBASE [inception to August 10, 2017], Ichushi (Japanese database of scientific literature and abstracts of scientific meetings) [inception to August 15, 2017], and the Cochrane Central Register of Controlled Trials [inception to August 15, 2017], we searched for randomized trials of goshajinkigan for prevention of CIPN. Our search strategy included the following terms: “goshajinkigan,” “gosha-jinki-gan,” “go-sha-jinki-gan,” “niu-che-shen-qi-wan,” and “TJ-107” (Supplementary Table 1). We also reviewed references within the retrieved articles, searched Google Scholar, and contacted Tsumura & Co., the manufacturer of goshajinkigan, for potentially relevant studies. We placed no language restrictions on our search.
We included randomized controlled trials that assessed the efficacy and safety of goshajinkigan for prevention of CIPN in cancer patients undergoing neurotoxic chemotherapy. We considered adult patients aged ≥ 18 who had cancer, such as colon, ovarian, or breast cancers, and who received neurotoxic chemotherapy including taxanes, vinca alkaloids, and platinum agents. We excluded patients that had already developed CIPN. We considered goshajinkigan of any dose as a “prophylactic” intervention against CIPN. We excluded studies that examined goshajinkigan as a “treatment” of CIPN that had already developed in patients. We accepted the following comparators as the control: placebo, no intervention, and any agents that are currently known to not reduce or prevent CIPN. We excluded quasi-randomized and non-randomized trials, and observational studies. Two authors (AK and KE) independently reviewed the list of articles obtained by the search and selected eligible articles. These same authors then independently extracted the following data: (1) patient demographics (age, sex, underlying malignancy), (2) study characteristics (study sites, trial registry numbers), (3) information on interventions (dose of goshajinkigan, comparators), and (4) outcomes of interest. We also assessed the risk of bias using the Cochrane risk of bias assessment tool [10]. Any discrepancy was resolved through consensus.
Our primary outcomes were the following: (1) incidence of CIPN, (2) response to chemotherapy, and (3) adverse events related to goshajinkigan. Our secondary outcomes included the following: (1) proportion of patients that completed scheduled courses of chemotherapy and (2) disease control. We considered all these outcomes at the latest time points of the trial.
Dichotomous outcomes were combined using risk ratios (RRs). When trials had zero events in either arm, continuity corrections were applied with the addition of 0.5 to each cell of 2 × 2 tables from the trial [32]. We attempted to ask the original study investigators for necessary information if an email address was provided. Three authors from four trials responded [18, 20, 26, 27]. We pooled data using the DerSimonian and Laird random effects model [6]. Statistical heterogeneity was assessed visually with Galbraith plots [8] and statistically with the I 2 and Q statistics [11]. Given the limited number of trials, we were unable to assess small study effects or publication bias.
We conducted sensitivity analysis by excluding trials with high or unclear risk of bias in sequence generation, allocation concealment, and blinding of outcome assessors. The threshold of statistical significance was set at p < 0.05. All analyses were performed with Stata SE, version 15.0 (Stata Corp., College Station, TX, USA).
Results
Overview of the included trials
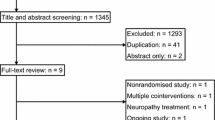
Our search yielded 234 articles (Fig. 1). After application of our inclusion and exclusion criteria, five trials involving a total of 397 patients were included for analysis [1, 18, 20, 26, 27] (Table 1). Three trials included patients with colorectal cancer [20, 26, 27] and two with breast cancer [1, 18]. Accordingly, two trials used modified FOLFOX 6 [26, 27], one used FOLFOX 4 or modified FOLFOX 6 [20], one employed weekly paclitaxel, and one used docetaxel-based therapy [1, 18]. Three trials reported the cumulative dose of chemotherapy; two trials administered oxaliplatin of 1105 to 1120 mg/m2 and 750 to 793 mg/m2, respectively [26, 27]; and one trial [1] administered docetaxel of approximately 340 mg/m2. The number of patients per trial ranged from 18 to 186, and ages ranged from 35 to 88 years. Study durations varied from 12 to 26 weeks, and two trials did not state the trial duration. In all trials, patients were orally administered 7.5 g per day of goshajinkigan during the study period. For the comparator, two trials used placebo [20, 27], two used no intervention [18, 26], and the remaining trial administered mecobalamin [1], for which no evidence supports its ability to prevent CIPN. One trial was terminated early [27]. Oki et al. conducted a phase III, double-blind, placebo-controlled trial in patients with colon cancer undergoing oxaliplatin-based chemotherapy. They planned to enroll 310 patients, but the study was terminated due to an interim analysis of 142 patients suggesting an increased incidence of CIPN in the goshajinkigan group (hazard ratio, 1.908; p = 0.007).
Risk of bias assessment
Overall, four trials (80%) had adequate sequence generation and adequate concealed allocation, and outcome assessors were judged to be adequately blinded in two trials (40%) (Table 2). Three studies (60%) were deemed to be at low risk of incomplete outcome data. Four trials (80%) were registered and free of selective reporting.
Primary outcomes
Two definitions for CIPN were used: the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) in four studies [1, 18, 20, 27] and the Neurotoxicity Criteria of Debiopharm (DEB-NTC) in three [1, 26, 27]. For trials using NCI-CTCAE, goshajinkigan was not associated with reduced incidence of any grade of CIPN compared with the control (Fig. 2; Supplementary Table 2). For trials using DEB-NTC, goshajinkigan was associated with significantly reduced incidence of grade ≥ 1 CIPN (RR 0.43; 95% confidence interval [CI], 0.27 to 0.66), and grade 3 CIPN (RR 0.42; 95% CI, 0.25 to 0.71; df = 1; I 2 = 0.0%; p = 0.93) (Fig. 3; Supplementary Table 2). However, goshajinkigan was not associated with reduced incidence of grade ≥ 2 CIPN (RR 0.78; 95% CI, 0.36 to 1.72; df = 2; I 2 = 94.7%; p < 0.001), when measured with DEN-NTC.
Compared with the control, goshajinkigan was not associated with improved tumor response (RR 1.01; 95% CI, 0.72 to 1.42; Q = 1.13; df = 1; I 2 = 11.2%; p = 0.29).
Adverse events related specifically to goshajinkigan were mentioned in only one trial, which reported that goshajinkigan was well tolerated.
Secondary outcomes
The number of patients who completed the scheduled chemotherapy was reported in only one trial [1]; all patients from each treatment group completed the therapy.
Disease control was reported in two trials [20, 26]. Compared with the control, goshajinkigan was not associated with better disease control (RR 0.96; 95% CI, 0.85 to 1.08; Q = 0.31; df = 1; I 2 = 0.0%; p = 0.56).
Sensitivity analysis
We conducted sensitivity analyses of the incidence of CIPN (Table 3). Many analyses were hindered by the small number of included trials. However, all possible sensitivity analyses showed results similar to those of the primary analyses.
Discussion
Our analysis suggests that goshajinkigan was not associated with reduced incidence of CIPN when measured with NCI-CTCAE. Goshajinkigan was associated with reduced incidence of grade ≥ 1 and grade 3 CIPN when measured with DEB-NTC, but this significant association disappeared in the incidence of grade ≥ 2 CIPN. All sensitivity analyses were consistent with the primary outcome analysis regarding the incidence of CIPN, thereby confirming the robustness of our analysis. However, we identified no evidence to support the use of goshajinkigan for other outcomes, and we found a paucity of safety information related to goshajinkigan.
Our study provided conflicting results about the incidence of CIPN when measured with DEB-NTC; there was a beneficial association found for grade ≥ 1 and grade 3 CIPN, and none for grade ≥ 2 CIPN. There are two potential explanations for this finding. First, Oki et al. reported an increased incidence of grade ≥ 2 CIPN associated with goshajinkigan [27]; their study did not detail the incidence of grade ≥ 1 and grade 3 CIPN measured with CIPN. The other two studies showed a beneficial effect of goshajinkigan to prevent CIPN for most grades of CIPN [1, 26]. Second, the study by Oki et al. was much larger than the others in sample size, and thus, the pooled outcomes for grade ≥ 2 might have been non-significant. It is known that large treatment effects emerge from small-sized studies [29]. Thus, when future studies of goshajinkigan to prevent CIPN are conducted with larger sample sizes, their results might not support the benefit that our study found for grade ≥ 1 and grade 3 CIPN.
Although we acknowledge that our findings represent low-quality evidence, the difference in the finding between the DEB-NTC and the NCI-CTCAE outcomes suggests that goshajinkigan may potentially have beneficial effects on duration of peripheral neurotoxicity, though less so on the composite of activities of daily living. NCI-CTCAE assesses the severity of neuropathy that affects daily living, whereas DEB-NTC focuses on the duration of peripheral neurotoxicity. A discrepancy in evaluations between the scales has been reported [14]. This discrepancy may have resulted in the inconsistent findings regarding the prophylactic efficacy of goshajinkigan in our meta-analysis. Our study narrowly suggested that goshajinkigan might be favored in terms of the duration of peripheral neurotoxicity compared with controls as shown in the measurement of DEB-NTC.
Avoiding dose limitations, completing chemotherapy, and achieving disease control are the ultimate patient-oriented goals associated with prophylaxis of chemotherapy-induced adverse effects. However, these patient-oriented outcomes were reported in only a few trials, and we could not draw firm conclusions about the efficacy of goshajinkigan for these outcomes. Any supportive care should be safe and well tolerated, because patients already endure chemotherapy-related adverse effects. However, our review failed to demonstrate the safety of goshajinkigan, due to under-reporting of adverse effects associated with goshajinkigan in original studies, similar to what has been seen in trials of other forms of herbal medicine [7, 28]. Some trials in other populations with benign disease have reported gastrointestinal symptoms (nausea, gastric discomfort, and diarrhea) as adverse effects related to goshajinkigan [15, 38].
Animal studies have shown that goshajinkigan may prevent acute and chronic CIPN in rodents given paclitaxel, oxaliplatin, and vincristine without affecting the anti-tumor effects of these agents [3, 4, 17, 21, 23, 24, 35]. Pretreatment or co-administration of goshajinkigan was common in these studies. However, Kono et al. suggested that given the fast absorption of some neuroprotective compounds in goshajinkigan (30 to 60 min after administration) and the delayed peak of oxaliplatin concentration in serum (90 min after administration), goshajinkigan should be administered before oxaliplatin for efficient neuroprotective effects [21]. This needs to be investigated in future trials to elucidate an effective schedule for administration of goshajinkigan.
The latest clinical guideline for prevention and management of CIPN suggests that only a limited number of agents (acetylcysteine, carbamazepine, glutamate, venlafaxine, and goshajinkigan) can provide prophylaxis of CIPN, but the evidence supporting such a recommendation was considered insufficient or inconclusive [9]. When our findings of the incidence of CIPN were assessed with the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system [10], the quality of evidence for goshajinkigan for prophylaxis of CIPN was mostly low or very low (Table 3). More high-quality research is needed.
Our study had some strengths. First, we conducted an extensive search in four databases including a Japanese one. We also asked the pharmaceutical company that manufactures goshajinkigan for more potentially eligible studies, which ensured that our search was comprehensive. Second, this is the first systematic review and meta-analysis that examined goshajinkigan as a preventive agent of CIPN. Our study found few merits of goshajinkigan as a prophylactic option against CIPN. However, we elucidated the weakness of the original studies to facilitate a better conduct of future studies.
Our study also has some limitations. First, the types of chemotherapy and underlying cancer types varied across studies. Our study included trials that employed taxane- and platinum-based chemotherapy, the most common and important therapies. However, the small number of trials precluded an analysis of which patients would potentially benefit from goshajinkigan. Second, clinically important outcomes such as the definitions of CIPN, disease control, and adverse effects were not uniformly reported, which precluded analyses due to an insufficient number of trials. Future trials should report CIPN using several definitions to look at different aspects of CIPN [14] and clinically important patient-oriented outcomes.
Currently, at least one ongoing trial is examining the prophylactic efficacy of goshajinkigan in patients receiving neurotoxic chemotherapy (UMIN000021361) [34]. Also, Oki et al. plan to assess the 5-year prognosis of their enrolled patients. The investigators of trials assessing goshajinkigan for prophylaxis of CIPN should clarify the points stated above to overcome the limitations of the previous studies and to facilitate improved analysis that will inform clinicians and patients.
Conclusion
Goshajinkigan is unlikely to prevent CIPN in patients undergoing neurotoxic chemotherapy. Use of goshajinkigan as standard of care for prophylaxis of CIPN is not currently recommended. However, given the low quality and insufficient amount of the current evidence, the efficacy of goshajinkigan as prophylaxis against CIPN is still inconclusive. More trials with better, standardized reporting of clinically important outcomes are needed.
References
Abe H, Kawai Y, Mori T, Tomida K, Kubota Y, Umeda T, Tani T (2013) The Kampo medicine Goshajinkigan prevents neuropathy in breast cancer patients treated with docetaxel. Asian Pac J Cancer Prev 14(11):6351–6356. https://doi.org/10.7314/APJCP.2013.14.11.6351
Andoh T, Kitamura R, Fushimi H, Komatsu K, Shibahara N, Kuraishi Y (2014) Effects of goshajinkigan, hachimijiogan, and rokumigan on mechanical allodynia induced by paclitaxel in mice. J Tradit Complement Med 4(4):293–297. https://doi.org/10.4103/2225-4110.128906
Andoh T, Kato M, Kitamura R, Mizoguchi S, Uta D, Toume K, Komatsu K, Kuraishi Y (2016) Prophylactic administration of an extract from Plantaginis Semen and its major component aucubin inhibits mechanical allodynia caused by paclitaxel in mice. J Tradit Complement Med 6(3):305–308. https://doi.org/10.1016/j.jtcme.2015.12.001
Bahar MA, Andoh T, Ogura K, Hayakawa Y, Saiki I, Kuraishi Y (2013) Herbal medicine goshajinkigan prevents paclitaxel-induced mechanical allodynia without impairing antitumor activity of paclitaxel. Evid Based Complement Alternat Med 2013:849754
Cascella M, Muzio MR (2017) Potential application of the Kampo medicine goshajinkigan for prevention of chemotherapy-induced peripheral neuropathy. J Integr Med 15(2):77–87. https://doi.org/10.1016/S2095-4964(17)60313-3
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Gagnier JJ, DeMelo J, Boon H, Rochon P, Bombardier C (2006) Quality of reporting of randomized controlled trials of herbal medicine interventions. Am J Med 119:800 e801–800 e811
Galbraith RF (1988) A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med 7:889–894
Hershman DL, Lacchetti C, Dworkin RH, Lavoie Smith EM, Bleeker J, Cavaletti G, Chauhan C, Gavin P, Lavino A, Lustberg MB, Paice J, Schneider B, Smith ML, Smith T, Terstriep S, Wagner-Johnston N, Bak K, Loprinzi CL, American Society of Clinical O (2014) Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 32:1941–1967
Higgins J, Green S (2008) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, Ltd, Chichester. https://doi.org/10.1002/9780470712184
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ (Clin Res ed) 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Hirayama Y, Sasaki J, Dosaka-Akita H, Ishitani K (2016) Survey of the management of chemotherapy-induced peripheral neuropathy in Japan: Japanese Society of Medical Oncology. ESMO open 1:e000053
Hosokawa A, Ogawa K, Ando T, Suzuki N, Ueda A, Kajiura S, Kobayashi Y, Tsukioka Y, Horikawa N, Yabushita K, Fukuoka J, Sugiyama T (2012) Preventive effect of traditional Japanese medicine on neurotoxicity of FOLFOX for metastatic colorectal cancer: a multicenter retrospective study. Anticancer Res 32(7):2545–2550
Inoue N, Ishida H, Sano M, Kishino T, Okada N, Kumamoto K, Ishibashi K (2012) Discrepancy between the NCI-CTCAE and DEB-NTC scales in the evaluation of oxaliplatin-related neurotoxicity in patients with metastatic colorectal cancer. Int J Clin Oncol 17(4):341–347. https://doi.org/10.1007/s10147-011-0298-z
Kajiwara M, Mutaguchi K (2008) Clinical efficacy and tolerability of gosha-jinki-gan, Japanese traditional herbal medicine, in females with overactive bladder. Hinyokika kiyo Acta urologica Japonica 54:95–99
Kaku H, Kumagai S, Onoue H, Takada A, Shoji T, Miura F, Yoshizaki A, Sato S, Kigawa J, Arai T, Tsunoda S, Tominaga E, Aoki D, Sugiyama T (2012) Objective evaluation of the alleviating effects of Goshajinkigan on peripheral neuropathy induced by paclitaxel/carboplatin therapy: a multicenter collaborative study. Exp Ther Med 3(1):60–65. https://doi.org/10.3892/etm.2011.375
Kamei J, Hayashi S-S, Miyata S (2008) Effect of Gosha-jinki-gan on vincristine-induced painful neuropathy in mice. Jpn J Pharm Palliat Care Sci 1:19–24
Kawabata K, Kawajiri H, Takashima T, Nakano T, Mitukawa Y, Kawakami N (2013) P2-043 * reduction of paclitaxel-related peripheral sensory neuropathy by Gosha-jinki-gan or carbon dioxide feet and hand bathing. Ann Oncol 24:ix80
Kono T, Mamiya N, Chisato N, Ebisawa Y, Yamazaki H, Watari J, Yamamoto Y, Suzuki S, Asama T, Kamiya K (2011) Efficacy of goshajinkigan for peripheral neurotoxicity of oxaliplatin in patients with advanced or recurrent colorectal cancer. Evid Based Compl Alternat Med 2011:418481
Kono T, Hata T, Morita S, Munemoto Y, Matsui T, Kojima H, Takemoto H, Fukunaga M, Nagata N, Shimada M, Sakamoto J, Mishima H (2013) Goshajinkigan oxaliplatin neurotoxicity evaluation (GONE): a phase 2, multicenter, randomized, double-blind, placebo-controlled trial of goshajinkigan to prevent oxaliplatin-induced neuropathy. Cancer Chemother Pharmacol 72(6):1283–1290. https://doi.org/10.1007/s00280-013-2306-7
Kono T, Suzuki Y, Mizuno K, Miyagi C, Omiya Y, Sekine H, Mizuhara Y, Miyano K, Kase Y, Uezono Y (2015) Preventive effect of oral goshajinkigan on chronic oxaliplatin-induced hypoesthesia in rats. Sci Rep 5(1):16078. https://doi.org/10.1038/srep16078
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 151(4):W65–W94
Matsumura Y, Yokoyama Y, Hirakawa H, Shigeto T, Futagami M, Mizunuma H (2014) The prophylactic effects of a traditional Japanese medicine, goshajinkigan, on paclitaxel-induced peripheral neuropathy and its mechanism of action. Mol Pain 10:61
Mizuno K, Kono T, Suzuki Y, Miyagi C, Omiya Y, Miyano K, Kase Y, Uezono Y (2014) Goshajinkigan, a traditional Japanese medicine, prevents oxaliplatin-induced acute peripheral neuropathy by suppressing functional alteration of TRP channels in rat. J Pharmacol Sci 125(1):91–98. https://doi.org/10.1254/jphs.13244FP
Mols F, Beijers T, Vreugdenhil G, van de Poll-Franse L (2014) Chemotherapy-induced peripheral neuropathy and its association with quality of life: a systematic review. Support Care Cancer 22(8):2261–2269. https://doi.org/10.1007/s00520-014-2255-7
Nishioka M, Shimada M, Kurita N, Iwata T, Morimoto S, Yoshikawa K, Higashijima J, Miyatani T, Kono T (2011) The Kampo medicine, Goshajinkigan, prevents neuropathy in patients treated by FOLFOX regimen. Int J Clin Oncol 16(4):322–327. https://doi.org/10.1007/s10147-010-0183-1
Oki E, Emi Y, Kojima H, Higashijima J, Kato T, Miyake Y, Kon M, Ogata Y, Takahashi K, Ishida H, Saeki H, Sakaguchi Y, Yamanaka T, Kono T, Tomita N, Baba H, Shirabe K, Kakeji Y, Maehara Y (2015) Preventive effect of Goshajinkigan on peripheral neurotoxicity of FOLFOX therapy (GENIUS trial): a placebo-controlled, double-blind, randomized phase III study. Int J Clin Oncol 20(4):767–775. https://doi.org/10.1007/s10147-015-0784-9
Pan X, Lopez-Olivo MA, Song J, Pratt G, Suarez-Almazor ME (2017) Systematic review of the methodological quality of controlled trials evaluating Chinese herbal medicine in patients with rheumatoid arthritis. BMJ Open 7(3):e013242. https://doi.org/10.1136/bmjopen-2016-013242
Pereira TV, Horwitz RI, Ioannidis JP (2012) Empirical evaluation of very large treatment effects of medical interventions. JAMA 308(16):1676–1684. https://doi.org/10.1001/jama.2012.13444
Pike CT, Birnbaum HG, Muehlenbein CE, Pohl GM, Natale RB (2012) Healthcare costs and workloss burden of patients with chemotherapy-associated peripheral neuropathy in breast, ovarian, head and neck, and nonsmall cell lung cancer. Chemother Res Pract 2012:913848
Seretny M, Currie GL, Sena ES, Ramnarine S, Grant R, MacLeod MR, Colvin LA, Fallon M (2014) Incidence, prevalence, and predictors of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Pain 155(12):2461–2470. https://doi.org/10.1016/j.pain.2014.09.020
Sweeting MJ, Sutton AJ, Lambert PC (2004) What to add to nothing? Use and avoidance of continuity corrections in meta-analysis of sparse data. Stat Med 23(9):1351–1375. https://doi.org/10.1002/sim.1761
Tawata M, Kurihara A, Nitta K, Iwase E, Gan N, Onaya T (1994) The effects of goshajinkigan, a herbal medicine, on subjective symptoms and vibratory threshold in patients with diabetic neuropathy. Diabetes Res Clin Pract 26(2):121–128. https://doi.org/10.1016/0168-8227(94)90149-X
UMIN000021361. Comparing investigation of the curative effect by Goshajinkigan and Pregabalin for -Induced Peripheral Neuropathy. (Accessed as of May 5, 2017). In: Editor (ed)^(eds) Book Comparing investigation of the curative effect by Goshajinkigan and Pregabalin for -Induced Peripheral Neuropathy. (Accessed as of May 5, 2017), City
Ushio S, Egashira N, Sada H, Kawashiri T, Shirahama M, Masuguchi K, Oishi R (2012) Goshajinkigan reduces oxaliplatin-induced peripheral neuropathy without affecting anti-tumour efficacy in rodents. Eur J Cancer (Oxford, England: 1990) 48(9):1407–1413. https://doi.org/10.1016/j.ejca.2011.08.009
Watanabe K, Shimada A, Miyaki K, Hirakata A, Matsuoka K, Omae K, Takei I (2014) Long-term effects of goshajinkigan in prevention of diabetic complications: a randomized open-labeled clinical trial. Evid Based Complement Alternat Med 2014:128726
Yoshida N, Hosokawa T, Ishikawa T, Yagi N, Kokura S, Naito Y, Nakanishi M, Kokuba Y, Otsuji E, Kuroboshi H, Taniwaki M, Taguchi T, Hosoi H, Nakamura T, Miki T (2013) Efficacy of goshajinkigan for oxaliplatin-induced peripheral neuropathy in colorectal cancer patients. J Oncol 2013:139740
Yoshimura K, Shimizu Y, Masui K, Okuno H, Ueda T, Soda T, Ogawa O (2012) Furosemide versus gosha-jinki-gan, a blended herbal medicine, for nocturnal polyuria: a randomized crossover trial. Lower Urinary Tract Symptoms 4(2):77–81. https://doi.org/10.1111/j.1757-5672.2011.00132.x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflicts of interest.
Electronic supplementary material
Supplementary Table 1
(DOC 25 kb)
Supplementary Table 2
(DOC 34 kb)
Rights and permissions
About this article
Cite this article
Kuriyama, A., Endo, K. Goshajinkigan for prevention of chemotherapy-induced peripheral neuropathy: a systematic review and meta-analysis. Support Care Cancer 26, 1051–1059 (2018). https://doi.org/10.1007/s00520-017-4028-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-4028-6