Abstract
Purpose
Pain is common for hematopoietic stem cell transplant (HSCT) patients and may be experienced pre-transplant, acutely post-transplant, and for months or years following transplant. HSCT patients with persistent pain may be at risk for poor quality of life following transplant; however, the impact of pre-transplant pain on quality of life post-transplant is not well understood. Self-efficacy for chronic disease management is associated with quality of life among cancer patients and may impact quality of life for HSCT patients. The primary aim was to examine the effect of pre-transplant pain and self-efficacy on quality of life domains in the year following transplant.
Methods
One hundred sixty-six HSCT patients completed questionnaires providing information on pain, self-efficacy, and quality of life prior to transplant, at discharge, and 3-, 6-, and 12-months post-transplant as part of a longitudinal, observational study. Linear mixed modeling examined the trajectories of these variables and the effect of pre-transplant pain and self-efficacy on post-transplant quality of life.
Results
Pain and social and emotional quality of life remained stable in the year following transplant while self-efficacy and physical and functional quality of life improved. Pre-transplant pain was significantly related to lower physical well-being post-transplant. Lower pre-transplant self-efficacy was related to lower quality of life across all domains post-transplant.
Conclusion
Above and beyond the effect of pre-transplant pain, self-efficacy for managing chronic disease is important in understanding quality of life following transplant. Identifying patients with pain and/or low self-efficacy pre-transplant may allow for early intervention with self-management strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hematopoietic stem cell transplantation (HSCT) is a common and intensive treatment for many blood and marrow cancers [1]. Prior to transplantation, patients undergo a lengthy preparative regimen consisting of maximally tolerated doses of chemotherapy and/or radiation to both treat the disease and provide adequate immunosuppression to prevent rejection of the transplanted cells [2]. After completing the preparative regimen, patients receive either an autologous or allogeneic HSCT, receiving their own or donated stem cells, respectively [2].
Selection of transplant type is associated with many factors including the patient’s age, type of malignancy, as well as stage, disease status, and the availability of a donor [3]. While HSCT is associated with a higher survival rate overall, patients may experience a variety of physical (e.g., fatigue, nausea, pain) and psychological (e.g., anxiety, depression, cognitive problems) problems [4]. Patients receiving an allogeneic transplant face the added challenge of the potential for graft versus host disease (GvHD) and the continued use of immunosuppressive agents to prevent or treat GvHD post-transplant [2].
Pain, in particular, presents a significant challenge for many patients as they undergo transplant and may negatively impact patients’ quality of life following transplant [5,6,7]. Cancer patients with higher levels of pain often report decreased overall quality of life, poor physical and emotional functioning, and increased psychological distress [8, 9]. Pain is common for HSCT patients and may be experienced pre-transplant, acutely post-transplant, and for months or years following transplant. Previous research suggests that 26–58% of HSCT patients report pain, with joint, bone, headache, mouth, gastro-intestinal, neuropathic, and thoracic pain being most frequently endorsed [8,9,10,11]. Pain experienced as a result of HSCT is often related to the conditioning regimen (e.g., chemotherapy, irradiation) or to GvHD [5]. Pain that is present pre-transplant and persists in the years following transplant may be due to past treatments (e.g., chemotherapy-related neuropathic pain), disease-related pain (e.g., multiple myeloma bone pain), and/or comorbid chronic conditions (e.g., arthritis, diabetic neuropathy) [5].
Studies have demonstrated that patients with pain pre-transplant continue to experience significant pain in the years following transplant, and persistent pain is described as one of the most problematic symptoms [12]. HSCT patients endorsing post-transplant pain report lower levels of both physical and emotional functioning post-transplant, including less energy, worse mood, and greater sexual dysfunction [10]. In addition to the burden resulting from life-threatening chronic illness, invasive treatment regimens, and interruptions to normal routine, HSCT patients with a persistent pattern of pre- and post-transplant pain may be at risk for poor quality of life in the months following HSCT. However, the impact of pre-transplant pain on HSCT patients’ physical, emotional, social, and functional quality of life in the months and years following transplant is not well understood [5].
Self-efficacy for chronic disease management, or confidence in one’s ability to manage their disease symptoms [13], may be an important factor in predicting HSCT patients’ post-transplant quality of life. HSCT patients with persistent pain may experience low self-efficacy for managing their disease and its symptoms, which can be related to lower levels of physical and emotional well-being [14]. Cancer survivors, including HSCT patients, often experience multiple, co-occurring symptoms (e.g., pain, fatigue, psychological distress) [4]; any one symptom may serve to exacerbate the effects of another symptom [15]. For example, in two recent studies, pain was found to be a potential risk factor for psychological distress among HSCT patients [9, 16]. As symptoms interact, symptom burden increases, which may significantly impact a patient’s self-efficacy for symptom management [15]. Self-efficacy for symptom management is especially relevant for quality of life in HSCT populations due to the high symptom burden resulting from an intensive and protracted period of medical intervention [4]. While there is limited research on chronic disease self-efficacy and quality of life outcomes in HSCT patients, several studies have indicated that higher self-efficacy is related to better outcomes for chronic disease patients. For example, higher self-efficacy for pain control is related to lower levels of pain for cancer patients [17] and lower levels of pain, disability, and psychological distress for arthritis patients with chronic pain [18, 19].
There is a need to more closely examine the effect of pain and chronic disease self-efficacy on post-transplant quality of life domains. Support for these associations would provide useful information for developing clinical services aimed at improving physical and emotional outcomes for patients following HSCT. The specific aim of the present study was to examine the relative contributions of pre-transplant pain severity and chronic disease self-efficacy to quality of life domains (i.e., physical, emotional, social, and functional) post-transplant. We hypothesized that higher levels of pre-transplant pain and lower levels of pre-transplant chronic disease self-efficacy would be associated with lower levels of physical, emotional, social, and functional quality of life post-transplant.
Method
Participants and procedure
Patients undergoing autologous and allogeneic HSCT were recruited from the adult bone marrow transplant clinic at Duke University Medical Center in the USA between August 2011 and February 2014. The data included in this study are from a larger, ongoing project examining patient quality of life over the course of HSCT. The parent observational, longitudinal study was designed to examine the experience of HSCT patients pre- and post-transplant with patients being asked to complete questionnaires pre-transplant and post-transplant for up to 2 years following transplant. Exclusion criteria included inability to complete self-report questionnaires due to language or medically documented severe cognitive impairments (e.g., dementia, Alzheimer’s disease). All other individuals treated at the adult bone marrow transplant clinic were eligible for the parent study. The study was approved by the Institutional Review Board. Informed consent was obtained from all individual participants included in the study.
The present analyses included data from patients who completed self-report questionnaires assessing pain, chronic disease self-efficacy, and quality of life (i.e., physical, emotional, social, functional) at pre-transplant and again at least once post-transplant (i.e., at discharge to home, 3-, 6-, and/or 12-months post-transplant). Figure 1 presents a depiction of the timeline of assessments. Pre-transplant questionnaires were given to patients in the clinic approximately 1 week prior to their scheduled transplant during the conditioning regimen. Post-transplant questionnaires were given to patients approximately 1 week prior to their scheduled discharge to home, and then completed by mail or web-based platform (Qualtrics) at 3-, 6-, and/or 12-months post-transplantation.
Variables and measurement
Sociodemographic and clinical variables
Patients were asked to provide their age, gender, race, partner status, employment, and highest level of education at the pre-transplant assessment. Clinical variables (i.e., transplant type, diagnosis, date of transplant, and GvHD status) were abstracted from patients’ medical records.
Pain
The pain intensity scale of the Brief Pain Inventory (BPI) [20] was used to assess severity of pain. The pain intensity scale consists of four 0 to 10 scale ratings of the intensity of pain experienced in the past week. These items were averaged to create a total score; higher scores indicated greater pain. Prior studies with this scale have shown good internal reliability, test-retest reliability, and validity [21]. Cronbach’s alpha in this sample was computed for each assessment and ranged from 0.84 to 0.92.
Self-efficacy
Self-efficacy was measured using the Self-Efficacy for Managing Chronic Disease 6-Item Scale (SE-CD) [22], which assesses patients’ confidence in their abilities to manage their symptoms (i.e., fatigue, pain, emotional distress, other symptoms, and health problems) while doing activities and confidence in managing chronic disease. Patients were asked to respond on a scale of 1 “not at all confident” to 10 “totally confident.” The total score was calculated as the average of these items, with higher scores indicating greater self-efficacy. In this sample, Cronbach’s alpha was computed for each assessment and ranged from 0.93 to 0.95.
Quality of life
The Functional Assessment of Cancer Therapy—Bone Marrow Transplant (FACT-BMT) [23] was used to assess quality of life. The FACT-BMT is composed of the Functional Assessment of Cancer Therapy-General (FACT-G) and a 10-item BMT-specific subscale. For the purposes of the present analyses, only the FACT-G was used. The FACT-G is composed of four quality of life domains: physical well-being (seven items), emotional well-being (six items), social well-being (seven items), and functional well-being (seven items). Items are rated on a 5-point scale ranging from 0 “not at all” to 4 “very much.” Items are summed, with higher scores indicating greater physical, emotional, social, and functional well-being. For the purposes of this study, the single pain item was removed from the physical well-being scale prior to scoring. The FACT-G has undergone extensive psychometric testing [24] and has been shown to have good psychometric properties for use with bone marrow transplant patients [23]. For the present study, Cronbach’s alpha was computed for each assessment, and the subscales were found to have high internal consistency reliability (physical well-being α = 0.78 to 0.87; emotional well-being α = 0.71 to 0.87; social well-being α = 0.65 to 0.74, functional well-being α = 0.81 to 0.86).
Statistical analysis
Descriptive statistics are provided for participant demographic characteristics and medical variables. Preliminary analyses (bivariate correlations) were conducted to examine associations between study variables (pain, chronic disease self-efficacy, and quality of life domains) assessed pre-transplant and participant demographic and medical characteristics. Longitudinal linear mixed models (MIXED procedure, SPSS 19) [25] examined changes in pain, self-efficacy for chronic disease management, and each of the four quality of life domains from pre- to post-transplant. Time was coded as months since transplant. Statistical significance was considered at the level of p < 0.05.
Multivariate linear mixed models examined the relative contributions of pre-transplant pain and self-efficacy to post-transplant quality of life. This data analytic method is appropriate for correlated data (e.g., repeated measures collected from an individual), uses all available repeated data, and allows for randomly missing observations within a subject. To address non-independence due to repeated measures from participants, data were nested within participants. Based on preliminary analyses (p < 0.05), we included age, gender, education, marital status, and type of transplant (i.e., autologous vs. allogeneic) as well as pre-transplant quality of life as control variables. For interpretability, pre-transplant pain, self-efficacy, and quality of life were centered at the mean. The model specifications followed Singer and Willett’s (2003) recommendations for identifying the best fitting model for the variances and covariances of the variables under study [26].
Results
Sample description
Figure 2 provides the study flow diagram. Four hundred twenty-seven patients were identified pre-transplant, and 261 (61.1%) completed the pre-transplant assessment. Of the remaining 166, 44.0% (n = 73) declined participation and 56.0% (n = 93) completed post-transplant questionnaires but were unable to complete pre-transplant questionnaires due to their preparative regimen or illness. One hundred sixty-six patients (response rate: 63.6%) completed an assessment pre-transplant and at least one assessment post-transplant (one post-assessment n = 72, two post-assessments n = 44, and three or more post-assessments n = 50). The timing of these post-transplant assessments varied across participants, with 84 completed at discharge to home, 93 completed at 3-month post-transplant, 86 completed 6-month post-transplant, and 61 completed 12-month post-transplant.
Data from the remaining 95 participants were excluded from the present analyses (36.4%). Participants with pre-transplant questionnaires were excluded if they had received a diagnosis of post-transplant chronic, severe GvHD (n = 17), did not complete questionnaire packets post-transplant (n = 36), had incomplete post-transplant data (i.e., did not complete the BPI; n = 1), or were deceased (n = 41). Compared to study participants, patients who did not return questionnaires or returned incomplete questionnaires were significantly younger (M = 55.7 vs. M = 59.8 years; p = .01). Patients who were too ill to participate or deceased were more likely to have undergone allogeneic transplant versus autologous transplant (63.4 vs. 36.6%; p < .001). Participants and non-participants did not significantly (p > .10) differ on other demographic or medical characteristics.
Table 1 reports demographic and medical characteristics for participants. The majority of participants were male (62.4%) and white (84.9%) with an average age of 59.73 (SD = 9.48; range 25 to 83) years. Nearly one third of participants were employed (30.1%), while close to one third were on medical disability (30.1%). The remaining participants were retired (25.9%) or unemployed (10.2%). Employment status was unknown for six participants. Approximately one quarter (25.9%) of participants had a high school diploma or less, 27.7% reported having vocational training or some college, and 42.2% had received a college or graduate degree (4.2% did not report education). The majority (72.9%) of participants received autologous HSCT (i.e., receiving their own stem cells) while just over a quarter (27.1%) received allogeneic HSCT (i.e., donor stem cells).
Bivariate correlations pre-transplant
Correlations between patient characteristics and study variables (pain, chronic disease self-efficacy, and quality of life) at the pre-transplant assessment are presented in Table 2. Older age was associated with greater emotional well-being (r = 0.17, p = .03), and having more education was associated with greater self-efficacy (r = 0.22, p = .01). Women reported lower physical well-being relative to men (r = − 0.15, p = .05). Married patients reported greater social well-being (r = 0.27, p = .01) and lower functional well-being (r = − 0.17, p = .03) compared to unmarried patients. Patients undergoing autologous transplant had greater pain (r = −.19, p = .02) relative to those undergoing allogeneic transplant. Quality of life variables were significantly correlated with each other at the pre-transplant assessment (ps < 0.05; see Table 2), with the exception of social well-being and functional well-being. Greater pain was associated with lower self-efficacy, physical well-being, emotional well-being, and functional well-being (ps < 0.05). Self-efficacy was positively associated with each of the quality of life domains (ps < 0.01).
Linear mixed models
Longitudinal analyses
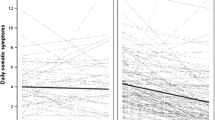
Table 3 presents the means and standard deviations for study variables of interest (i.e., pain, self-efficacy, and quality of life domains) at each of the five time points. Separate longitudinal linear mixed models examined changes in pain, self-efficacy for chronic disease management, and each of the four quality of life domains (physical, emotional, social, and functional well-being) over time. The time effect tested whether variables changed from pre- to post-transplant and across the post-transplant assessments (i.e., discharge to home, 3-month post-transplant, 6-month post-transplant, and 12-month post-transplant). There was no significant effect of time for pain (B = − 0.02, SE = 0.02, t = − 1.11, p = .27), emotional well-being (B = 0.02, SE = 0.03, t = 0.84, p = .40), or social-well-being (B = − 0.01, SE = 0.04, t = − 0.34, p = .73), suggesting that these variables remained stable from pre- to post-transplant. There was a significant effect of time for self-efficacy for disease management (B = 0.05, SE = 0.02, t = 2.39, p = .02), physical well-being (B = 0.31, SE = 0.05, t = 6.48, p < .001), and functional well-being (B = 0.29, SE = 0.06, t = 5.04, p < .001); the magnitudes of the slopes suggest that these variables improve over time.
Multivariate analyses
Table 4 presents the fixed effects for linear mixed models examining associations between pre-transplant pain and chronic disease self-efficacy and post-transplant quality of life domains. Each model controlled for pre-transplant quality of life, age, gender, education, marital status, and type of transplant (i.e., autologous vs. allogeneic) and included pre-transplant pain and self-efficacy as predictors. After accounting for relevant covariates, both pre-transplant pain (B = − 0.42, SE = 0.16, t = − 2.54, p = .01) and self-efficacy (B = 0.46, SE = 0.15, t = 3.10, p = .002) were significantly associated with post-transplant physical well-being. Results showed that a one point increase in pre-transplant pain was associated with a 0.42-point decline in post-transplant physical well-being. A one point increase in pre-transplant self-efficacy was associated with a 0.46-point increase in post-transplant physical well-being. Pre-transplant chronic disease self-efficacy was significantly and positively associated with post-transplant emotional (B = 0.27, SE = 0.11, t = 2.40, p = .02), social (B = 0.30, SE = 0.13, t = 2.30, p = .02), and functional (B = 0.73, SE = 0.19, t = 3.75, p < .001) well-being while pre-transplant pain was not (ps > .05). This suggests that pre-transplant self-efficacy is associated with these quality of life domains above and beyond the effect of pain.
Discussion
This study examined changes in pain, chronic disease self-efficacy, and quality of life from pre- to post-transplant as well as the impact of pre-transplant pain and self-efficacy on post-transplant quality of life across four domains (i.e., physical, emotional, social, and functional). Overall, chronic disease self-efficacy, physical well-being, and functional well-being improved from pre- to post-transplant. Pain, emotional well-being, and social well-being remained stable. In multivariate analyses, patients who had higher levels of pain before undergoing transplant were more likely to have lower physical quality of life post-transplant. We also found that low levels of self-efficacy for chronic disease self-management prior to transplant was associated with decreased quality of life following transplant across all four quality of life domains assessed. These findings are particularly striking given that they were observed for as long as 12 months following transplant and that our analyses allowed us to control for important demographic (i.e., age, gender, education, marital status) and medical (i.e., type of transplant) variables as well as pre-transplant quality of life. Taken together, these results suggest that pain severity and low chronic disease self-efficacy prior to transplant may be risk factors for poor quality of life in the year following transplant.
As expected and consistent with prior research, both physical and functional well-being improved for patients in the year following transplant [27, 28]. The disease itself, patients’ preparative regimens, and the transplantation process may result in impairments in physical and functional well-being [29]. As time since transplantation increases, these quality of life domains appear to recover. Emotional and social well-being remained stable from pre- to post-transplant. Research examining changes in emotional and social well-being has been inconsistent, with some studies reporting improvements and others reporting no change [27, 29,30,31]. Discrepancies found between the results of this study and others may also be a function of the quality of life instrument being used as well as the sample being studied (e.g., allogeneic only, autologous only) [29, 32, 33]. Studies that have included both autologous and allogeneic transplant patients using the FACT-BMT have reported similar results [30, 31].
Pain is a common and burdensome concern for HSCT patients [5, 11]. Many patients report pain pre-transplant and continue to experience pain in the months or years following transplant [5, 11, 12, 34]. The present study suggests that pain severity may remain stable from pre-transplant to up to 1-year post-transplant; this study examined pain for up to 12-month post-transplant and the analyses controlled for important pain-related variables. Our results also suggest that higher pain pre-transplant may negatively impact patients’ physical well-being in the year following transplant. Careful and routine assessment of pain prior to transplant could be potentially useful in identifying HSCT patients at risk for developing persistent pain and poor quality of life following transplant. Future studies should consider examining the impact of pre-transplant pain on a wider array of patient outcomes throughout the course of transplant and recovery (e.g., adherence, complications, functional status, treatment outcomes) and investigate strategies for utilizing assessment of pre-transplant pain to identify patients in need of additional support.
Perhaps the most interesting finding from the present study is the relationship between chronic disease self-efficacy and quality of life. While self-efficacy for chronic disease management appears to improve over time, we found that pre-transplant chronic disease self-efficacy was associated with post-transplant quality of life across all four domains; patients with lower self-efficacy experienced poorer physical, functional, emotional, and social well-being in the year following transplant after controlling for pre-transplant pain and relevant covariates. This suggests that self-efficacy may independently contribute to quality of life for HSCT patients above and beyond the effect of pain on quality of life. This finding highlights the utility of identifying patients with low pre-transplant self-efficacy and providing early intervention to enhance chronic disease self-efficacy during and in the months following HSCT. While significant pre-transplant evaluations of patients are routine in clinic [35], they rarely assess patients’ self-efficacy for chronic disease management. Use of a brief self-efficacy measure, like the one used in the present study [22], during the pre-transplant evaluation may be a feasible strategy for identifying patients who may be at risk for poor post-transplant quality of life and may most benefit from an intervention aimed at improving chronic disease self-efficacy.
Several psychosocial strategies and interventions have been shown to increase self-efficacy for disease and/or symptom (e.g., pain) management in patients with chronic disease [18, 36]. Interventions may include strategies for and assistance with self-management tasks (e.g., symptom management, medical management, role management, emotional management) as well as specific self-management skills like problem solving, decision making, action planning, and self-tailoring. These interventions are thought to improve outcomes by enhancing self-efficacy [36]. For example, Larson et al. (2014) found that an intervention designed to enhance exercise self-efficacy in patients with chronic obstructive pulmonary disease led to improved disease self-management (i.e., increased physical activity) [37]. Another recent study found that a short, mobile health intervention focused on pain management led to increases in self-efficacy for pain management in patients with diverse cancer diagnoses (i.e., breast, lung, prostate, colorectal) [38]. Overall, the use of mobile health technology to deliver interventions to improve self-efficacy for disease and symptom (i.e., pain) management has been found to be feasible, acceptable, and to present low burden to cancer survivors [39]. Results of this work suggest that the magnitude of the effects of mobile health interventions on improvements in patient self-efficacy is comparable to those found for in-person interventions [39]. However, mobile health technology may be a superior treatment modality for HSCT patients because it can help to improve patients’ access to interventions. HSCT patients may live many miles from the medical centers where they have been treated. Mobile health technology can serve to reduce barriers to accessing interventions (e.g., transportation, time, physical limitations, costs). We are currently investigating a pain coping skills training protocol that aims to improve pain management, including self-efficacy for pain management, for patients with pain following HSCT. This protocol uses a tablet computer to deliver the intervention in patients’ homes to increase the accessibility of the intervention.
The majority of interventions have been conducted in the context of clinical research; however, it may be possible to integrate these strategies into the clinical setting. For example, patients receive significant pre-transplant instruction and post-transplant education prior to discharge. Integrating self-management strategies into these sessions may result in long-term benefits for patients post-transplant. Additionally, oncology nurses may be well suited to provide patients with self-management strategies, and, in fact, suggestions for integrating symptom self-management into nurses’ clinical practices have been proposed [15]. Recommendations include having nurses partner with patients to develop a tailored and individualized plan for self-management.
The present study has several strengths, including a longitudinal design and control for covariates shown to be associated with quality of life in prior studies (e.g., age, gender, transplant type, education) [28, 40]. Additionally, this study used a robust analytic strategy, linear mixed modeling, allowing for the inclusion of cases with missing data. This technique is superior to analytic strategies that utilize case-wise or list-wise deletion (e.g., repeated measures ANOVA). Finally, to our knowledge, this study is one of the first to examine the relationship between self-efficacy for disease management and quality of life for HSCT patients and suggests that interventions designed to enhance self-efficacy for chronic disease management may enhance quality of life in the year following transplant.
There are some limitations that should be considered when interpreting the results of the current study. First, this study is observational so no causal statements can be made about the direction of the relationships between pain, chronic disease self-efficacy, and quality of life. Second, all participants were recruited from a single site, the sample was primarily Caucasian and diagnosed with multiple myeloma, and patients with chronic, severe GvHD were excluded, limiting the generalizability of results to other racial/ethnic groups and patients populations. Future studies utilizing a more diverse sample (e.g., recruitment from multiple transplant centers, sample with increased racial diversity, sample with more diverse disease characteristics) of HSCT patients are warranted to confirm the relationships found in the present study. Third, data from 95 participants (36.4%) who completed pre-transplant questionnaires were excluded from analyses (i.e., diagnosis of post-transplant chronic, severe GvHD, did not complete post-transplant questionnaires/had incomplete post-transplant data, were deceased), which may introduce bias. While completers did not differ significantly from non-completers on demographic or medical variables (with the exception of age and transplant type), it is possible that participants who were most ill may have been least likely to complete post-transplant questionnaires.
Finally, our sample included patients who had undergone autologous or allogeneic transplant, with the majority receiving an autologous transplant. The larger number of patients receiving an autologous transplant (72.9 vs. 27.1%) is likely related to the fact that approximately half of patients had received a diagnosis of multiple myeloma (50.3%), for which autologous transplantation is often recommended [41]. There are some important differences between the two transplant types that warrant consideration including differences in preparative regimens, differences in the goals of transplantation (i.e., autologous transplant is often considered life extending while allogeneic may be considered curative), and differences in post-transplant symptoms and side effects. For example, allogeneic transplant patients are at risk of engraftment failure as well as acute and chronic GvHD, which can cause a variety of negative side effects and complications that can significantly impact quality of life. While we controlled for transplant type in the multivariate analyses and failed to find a significant effect of transplant type, additional research utilizing larger samples is needed to better understand the distinct relationships between pain, chronic disease self-efficacy, and quality of life among patients receiving each type of transplant.
Further, persistent pain (i.e., bone) is common for multiple myeloma patients, with more than 70% of patients reporting severe pain [42]. Pain has been described as one of the most bothersome symptoms [43] and is associated with factors that may influence patients’ quality of life including functional limitations [44], increased mood disturbance [45], and fatigue [43]. Although controlling for transplant type likely accounted for the large number of multiple myeloma patients represented in this study, it is possible that the relationship between pain and quality of life domains found in the present study may be influenced by patients’ diagnosis. Additional research is necessary to examine the effect that diagnosis may have on the relationships between pain, self-efficacy and quality domains.
The current study provides new insight into the relationships between pain, chronic disease self-efficacy, and quality of life across the trajectory of HSCT. The relationships between higher pre-transplant pain, lower pre-transplant self-efficacy, and lower quality of life post-transplant suggest that pain and self-efficacy could be used to identify patients at increased risk for poor outcomes following transplant. There is also evidence from intervention work that psychosocial interventions may be useful in helping patients learn to cope with pain and increase their chronic disease self-efficacy. This type of intervention may lead to better overall quality of life for HSCT patients.
References
Bhatia S, Ramsay NKC, Robison LL, Snyder D, Stein A, Forman SJ, Weisdorf DJ, Francisco L, Carter A, Sun C-L, Baker KS, Gurney JG, McGlave PB, Nademanee A, O'Donnell M (2007) Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood 110(10):3784–3792. https://doi.org/10.1182/blood-2007-03-082933
Cutler C (2017) The approach to hematopoietic cell transplantation survivorship. UpToDate, UpToDate, Waltham, MA
Champlin R (2003) Selection of autologous or allogeneic transplantation. In: Kufe DW, Pollock RE, Weischselbaum RR et al (eds) Cancer medicine, 6th edn. BC Decker, Hamilton, ON
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN (2009) Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psycho-Oncology 18(2):113–127. https://doi.org/10.1002/pon.1399
Niscola P, Romani C, Scaramucci L, Dentamaro T, Cupelli L, Tendas A, Piccioni D, Giovannini M, Tolu B, Cartoni C, Arcuri E, Perrotti A, Palumbo R, de Fabritiis P (2008) Pain syndromes in the setting of haematopoietic stem cell transplantation for haematological malignancies. Bone Marrow Transplant 41 (9):757–764
Frodin U, Lotfi K, Fomichov V, Juliusson G, Borjeson S (2015) Frequent and long-term follow-up of health-related quality of life following allogeneic haematopoietic stem cell transplantation. Eur J Cancer Care (Engl) 24(6):898–910. https://doi.org/10.1111/ecc.12350
Reinfjell T, Tremolada M, Zeltzer LK (2017) A review of demographic, medical, and treatment variables associated with health-related quality of life (HRQOL) in survivors of hematopoietic stem cell (HSCT) and bone marrow transplantation (BMT) during childhood. Front Psychol 8:253. https://doi.org/10.3389/fpsyg.2017.00253
Byar KL, Eilers JE, Nuss SL (2005) Quality of life 5 or more years post-autologous hematopoietic stem cell transplant. Cancer Nurs 28(2):148–157. https://doi.org/10.1097/00002820-200503000-00010
Jim HSL, Sutton SK, Jacobsen PB, Martin PJ, Flowers ME, Lee SJ (2016) Risk factors for depression and fatigue among survivors of hematopoietic cell transplantation. Cancer 122(8):1290–1297. https://doi.org/10.1002/cncr.29877
Gruber U, Fegg M, Buchmann M, Kolb HJ, Hiddemann W (2003) The long-term psychosocial effects of haematopoetic stem cell transplantation. Europe J Cancer Care 12(3):249–256. https://doi.org/10.1046/j.1365-2354.2003.00411_2.x
Anderson KO, Giralt SA, Mendoza TR, Brown JO, Neumann JL, Mobley GM, Wang XS, Cleeland CS (2007) Symptom burden in patients undergoing autologous stem-cell transplantation. Bone Marrow Transplant 39(12):759–766. https://doi.org/10.1038/sj.bmt.1705664
Worel N, Biener D, Kalhs P, Mitterbauer M, Keil F, Schulenburg A, Höcker P, Dieckmann K, Fischer G, Rosenmayr A, Linkesch W, Hinterberger W, Lechner K, Greinix HT (2002) Long-term outcome and quality of life of patients who are alive and in complete remission more than two years after allogeneic and syngeneic stem cell transplantation. Bone Marrow Transplant 30(9):619–626. https://doi.org/10.1038/sj.bmt.1703677
Bandura A (1997) Self-efficacy : The exercise of control: The exercise of control, vol Book, Whole. W.H. Freeman, New York
Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S, Henslee-Downey J (2007) Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. J Psychosoc Oncol 25(1):87–101. https://doi.org/10.1300/J077v25n01_05
Hoffman AJ (2013) Enhancing self-efficacy for optimized patient outcomes through the theory of symptom self-management. Cancer Nurs 36(1):E16–E26. https://doi.org/10.1097/NCC.0b013e31824a730a
Smith SR, Hobson ME, Haig AJ (2016) Distress prior to undergoing hematopoietic stem cell transplantation: demographic and symptom correlations and establishing a baseline. Patient Relat Outcome Meas 7:137–144. https://doi.org/10.2147/PROM.S109877
Jerant A, Franks P, Kravitz RL (2011) Associations between pain control self-efficacy, self-efficacy for communicating with physicians, and subsequent pain severity among cancer patients. Patient Educ Couns 85(2):275–280. https://doi.org/10.1016/j.pec.2010.11.007
Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M (2001) Effect of a self-management program on patients with chronic disease. Effect Clin Pract 4(6):256–262
Somers TJ, Shelby RA, Keefe FJ, Godiwala N, Lumley MA, Mosley-Williams A, Rice JR, Caldwell D (2010) Disease severity and domain-specific arthritis self-efficacy: relationships to pain and functioning in patients with rheumatoid arthritis. Arthritis Care Res 62(6):848–856. https://doi.org/10.1002/acr.20127
Cleeland CS (ed) (1989) Measurement of pain by subjective report, vol 12. Issues in Measurement. Raven Press, New York
Serlin RC, Mendoza TR, Nakamura Y, Edwards KR, Cleeland CS (1995) When is cancer pain mild, moderate or severe? Grading pain severity by its inference with function. Pain 61:277–284
Lorig K, Chastain RL, Ung E, Shoor S, Holman HR (1989) Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum 32(1):37–44. https://doi.org/10.1002/anr.1780320107
McQuellon RP, Russell GB, Cella DF, Craven BL, Brady M, Bonomi A, Hurd DD (1997) Quality of life measurement in bone marrow transplantation: development of the functional assessment of cancer therapy-bone marrow transplant (FACT-BMT) scale. Bone Marrow Transplant 19(4):357–368. https://doi.org/10.1038/sj.bmt.1700672
Cella D (1997) Manual of the Functional Assessment of Chronic Illness Therapy (FACIT) measurement system. Centre on Outcomes, Research and Education. Northwestern Healthcare and Northwestern University, Evanston
Raudenbush SW, Bryk AS (2002) Hierarchical linear models: applications and data analysis methods: Applications and data analysis methods, vol 1., vol Book, Whole. Sage Publications, Thousand Oaks
Singer JD, Willett JB (2003) Applied longitudinal data analysis: modeling change and event occurrence: modeling change and event occurrence. vol Book, Whole. Oxford University Press, New York
Bevans M (2010) Health-related quality of life following allogeneic hematopoietic stem cell transplantation. Hematol Am Soc Hematol Educ Program 2010:248–254. https://doi.org/10.1182/asheducation-2010.1.248
Andrykowski MA, Greiner CB, Altmaier EM, Burish TG, Antin JH, Gingrich R, McGarigle C, Henslee-Downey PJ (1995) Quality of life following bone marrow transplantation: findings from a multicentre study. Br J Cancer 71(6):1322–1329
Pidala J, Anasetti C, Jim H (2009) Quality of life after allogeneic hematopoietic cell transplantation. Blood 114(1):7–19. https://doi.org/10.1182/blood-2008-10-182592
McQuellon RP, Russell GB, Rambo TD, Craven BL, Radford J, Perry JJ, Cruz J, Hurd DD (1998) Quality of life and psychological distress of bone marrow transplant recipients: the ‘time trajectory’ to recovery over the first year. Bone Marrow Transplant 21(5):477–486. https://doi.org/10.1038/sj.bmt.1701115
Sherman AC, Simonton S, Latif U, Plante TG, Anaissie EJ (2009) Changes in quality-of-life and psychosocial adjustment among multiple myeloma patients treated with high-dose melphalan and autologous stem cell transplantation. Biol Blood Marrow Transplant 15(1):12–20. https://doi.org/10.1016/j.bbmt.2008.09.023
Hjermstad MJ, Evensen SA, Kvaloy SO, Fayers PM, Kaasa S (1999) Health-related quality of life 1 year after allogeneic or autologous stem-cell transplantation: a prospective study. J Clin Oncol 17(2):706–718. https://doi.org/10.1200/jco.1999.17.2.706
Kopp M, Schweigkofler H, Holzner B, Nachbaur D, Niederwieser D, Fleischhacker WW, Kemmler G, Sperner-Unterweger B (2000) EORTC QLQ-C30 and FACT-BMT for the measurement of quality of life in bone marrow transplant recipients: A comparison. Eur J Haematol 65(2):97–103
Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN (2009) Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psycho-Oncology 18(2):113
Logue M, Savani BN (2013) Understanding basic steps to hematopoietic stem cell transplantation evaluation. Am J Blood Res 3(2):102–106
Lorig KR, Holman H (2003) Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med 26(1):1–7
Larson JL, Covey MK, Kapella MC, Alex CG, McAuley E (2014) Self-efficacy enhancing intervention increases light physical activity in people with chronic obstructive pulmonary disease. Int J Chronic Obstruct Pulmon Dis 9:1081–1090. https://doi.org/10.2147/COPD.S66846
Somers TJ, Abernethy AP, Edmond SN, Kelleher SA, Wren AA, Samsa GP, Keefe FJ (2015) A pilot study of a mobile health pain coping skills training protocol for patients with persistent cancer pain. J Pain Symptom Manag (0). doi:https://doi.org/10.1016/j.jpainsymman.2015.04.013
Somers TJ, Kelleher SA, Westbrook KW, Kimmick GG, Shelby RA, Abernethy AP, Keefe FJ (2016) A small randomized controlled pilot trial comparing mobile and traditional pain coping skills training protocols for cancer patients with pain. Pain Res Treat 2016:2473629. https://doi.org/10.1155/2016/2473629
Chiodi S, Spinelli S, Ravera G, Petti AR, Van Lint MT, Lamparelli T, Gualandi F, Occhini D, Mordini N, Berisso G, Bregante S, Frassoni F, Bacigalupo A (2000) Quality of life in 244 recipients of allogeneic bone marrow transplantation. Br J Haematol 110 (3):614–619. doi:https://doi.org/10.1046/j.1365-2141.2000.02053.x
Rajkumar SV (2017) Autologous hematopoietic cell transplantation in multiple myeloma. UpToDate, UpToDate, Waltham, MA
Terpos E, Berenson J, Raje N, Roodman GD (2014) Management of bone disease in multiple myeloma. Expert Rev Hematol 7(1):113–125. https://doi.org/10.1586/17474086.2013.874943
Mols F, Oerlemans S, Vos AH, Koster A, Verelst S, Sonneveld P, van de Poll-Franse LV (2012) Health-related quality of life and disease-specific complaints among multiple myeloma patients up to 10 yr after diagnosis: results from a population-based study using the PROFILES registry. Eur J Haematol 89 (4):311–319. doi:https://doi.org/10.1111/j.1600-0609.2012.01831.x
Niscola P, Scaramucci L, Romani C, Giovannini M, Tendas A, Brunetti G, Cartoni C, Palumbo R, Vischini G, Siniscalchi A, Pd F, Caravita T (2010) Pain management in multiple myeloma. Expert Rev Anticancer Ther 10(3):415–425. https://doi.org/10.1586/era.10.5
Poulos AR, Gertz MA, Pankratz VS, Post-White J (2001) Pain, mood disturbance, and quality of life in patients with multiple myeloma. Oncol Nurs Forum 28(7):1163–1171
Funding
This work was supported in part by the National Institutes of Health (K07CA138767; 5KL2TR001115-03) and internal funding from the Duke Cancer Patient Support Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
O’Sullivan, M.L., Shelby, R.A., Dorfman, C.S. et al. The effect of pre-transplant pain and chronic disease self-efficacy on quality of life domains in the year following hematopoietic stem cell transplantation. Support Care Cancer 26, 1243–1252 (2018). https://doi.org/10.1007/s00520-017-3947-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3947-6