Abstract
Purpose
Fatigue is a prevalent and debilitating side effect of docetaxel chemotherapy in metastatic prostate cancer. A better understanding of the kinetics and nature of docetaxel-related fatigue may provide a framework for intervention.
Methods
This secondary analysis was performed using the MOTIF database, from a phase III, randomised, double-blind, placebo-controlled study of modafinil (200 mg/day for 15 days) for docetaxel-related fatigue in men with metastatic prostate cancer [1]. The pattern of fatigue was analysed using the MDASI (MD Anderson Symptom Inventory) score. The impact of modafinil, cumulative docetaxel exposure, age and smoking status on fatigue kinetics were explored. Fatigue-related symptoms were assessed using the SOMA6 (fatigue and related symptoms) subset of the SPHERE (Somatic and Psychological Health Report). Mood was tracked using the short form 36 health survey questionnaire (SF-36).
Results
Across four docetaxel cycles, fatigue scores were higher in the first week and decreased over weeks two and three. Whilst men randomised to modafinil had reduced fatigue scores, cumulative docetaxel had little impact. Younger men (55–68 years) had significantly reduced fatigue scores, whereas current and ex-smokers had higher scores. There was no significant change in mood status or haemoglobin across treatment cycles. Men described both ‘somnolence’ and ‘muscle fatigue’ contributing significantly to their symptom complex.
Conclusions
Assessment and management of docetaxel-related fatigue remains an important challenge. Given the complex, multifactorial nature of fatigue, identification through structured interview and interventions targeted to specific ‘at risk’ groups may be the most beneficial. Understanding the temporal pattern (kinetics) and nature of fatigue is critical to guide this process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatigue is one of the most prevalent [2] and anticipated [3] symptoms experienced by patients across a range of tumour types. Cancer-related fatigue (CRF) is a subjective, distressing and persistent sense of physical, emotional and/or cognitive tiredness related to cancer and cancer treatments, not proportional to recent activity, interferes with usual functioning [4] and responds poorly to rest [5]. It is a debilitating and affects quality of life [6]. Chemotherapy-related fatigue is a fatigue state led or augmented by chemotherapy administration.
The term ‘fatigue’ applies to a heterogeneous set of phenomena [7, 8]. Objective fatigue, a measurable drop in muscle strength during exercise, should be distinguished from subjective fatigue (recorded by questionnaire [9, 10] or interview [11]), when loss of muscle performance may not be evident. Physiological fatigue (effort-induced and reversible in healthy individuals) should be distinguished from pathological fatigue (determined by a disease process) and generally not fully reversible, i.e. secondary to myopathy or anaemia. The term ‘physical’ fatigue refers to a sense of weariness or heaviness in the body, whereas ‘mental’ fatigue, a sense of cognitive weariness. Several of these descriptors may apply, and more than one condition may be present simultaneously. Fatigue can also lead to daytime napping, which tends to exacerbate the symptom complex [12].
Chemotherapy is commonly associated with subjective fatigue, which can be a dose-limiting side effect. Docetaxel has demonstrated survival and quality of life benefits in the treatment of prostate cancer [13–16]. In QoliTox, a large, prospective trial investigating quality of life measures in nearly 2700 patients receiving docetaxel chemotherapy for metastatic disease; docetaxel-related fatigue was shown to have a significant, negative health impact [17]. Global health scores were significantly lower in patients who reported grades 3 or 4 docetaxel-related fatigue. In Tannock’s landmark TAX 327 trial, fatigue (all grades) was a significant side effect in 15% of men with castrate-resistant prostate cancer (CRPC) on three-weekly docetaxel [14]. Fatigue is considerably more frequent when docetaxel is paired with other systemic therapies [18, 19].
Despite significant attention and improvement in the management of cancer-related symptoms, fatigue remains a problematic, persistent and distressing side effect of cancer and its treatment. Unlike other chemotherapy-related side effects, fatigue can persist for months or years despite treatment cessation [20].
Using data from MOTIF [1], this secondary analysis provides the first detailed description of fatigue kinetics and the nature of docetaxel-related fatigue.
Methods
Samples
Data for this secondary analysis was obtained from patients enrolled in the MOTIF study [1]. The original phase III, multicentre, randomised (2:1), double-blind, placebo-controlled study evaluated the efficacy of modafinil in patients with metastatic prostate or breast cancer undergoing docetaxel chemotherapy (every 3 weeks; minimum dose 50 mg/m2). The trial enrolled 65 men with metastatic, CRPC and a small number of women with breast cancer, who were excluded from this analysis.
To be eligible for MOTIF, patients must have had at least two previous cycles of docetaxel and were expected to receive at least two more. Patients were eligible for enrolment if they had a self-reported fatigue score of ≥4/10 measured by the fatigue component of the MDASI [9], fatigue that was worse after starting docetaxel, a clinically significant fatigue state (≥3 on the SPHERE somatic subscale) [10] and a haemoglobin of ≥10 g/dL. At the start of their third or subsequent chemotherapy cycle, patients with significant docetaxel-related fatigue were randomised to receive concurrent modafinil 200 mg/day or placebo for 15 days. Modafinil was withheld for 3 days before and 3 days after chemotherapy to reduce the influence of pre-medications, which continued to be prescribed. Docetaxel was continued for up to four further cycles. Exclusion criteria included docetaxel dose reduction (to ≤50 mg/m2), a history of chronic fatigue, uncontrolled hypertension, a psychological condition that prevented treatment or follow-up, or a serious concomitant medical illness, precluding safe prescription of modafinil. Other eligibility criteria have been previously described [1]. Prednisolone at the usual dose of 10 mg daily was given as part of the treatment protocol. Dexamethasone pre-medication, as described in Tannock’s TAX-327 study, included dexamethasone 8 mg orally 12, 3 and 1 h prior to docetaxel [14].
Measures
Fatigue was primarily measured using the single item, 11-point (0–10) fatigue assessment scale from the MDASI [9]. Both the presence and severity of the symptom were recorded, with 0 meaning, “not present” and 10 meaning, “as bad as you can imagine”. Over the study period, fatigue was recorded at its worst in a diary, each morning, during cycles of docetaxel. The MDASI fatigue score versus time was then analysed for each cycle.
The primary end-point of the MOTIF study was defined as the area under the curve (AUC) captured by a plot of cumulative, daily MDASI fatigue scores versus time, during the first 7 days of study medication. For this analysis, daily MDASI scores measured during a 21-day docetaxel +/− modafinil treatment cycle were used to establish patterns of fatigue kinetics in all patients and those grouped according to modafinil exposure, cumulative docetaxel exposure, age and smoking status.
The SOMA subscale of the SPHERE questionnaire, a validated 6-point scale, recorded fatigue-related symptoms to ascertain a clinically significant fatigue state [10]. The questions discern muscle pain after activity, the need for more sleep, prolonged fatigue, poor sleep quality, poor concentration and tired muscles after activity. Patients were asked to score their degree of distress at baseline and then, three to four weekly, at the commencement of the treatment cycle. A clinically significant fatigue state on the SOMA scale was defined according to the previously validated cut-off scores [21].
The SF-36, a valid and reliable tool [22], encompasses eight multi-item scales assessing physical function and limitations secondary to emotional and physical problems, body pain, general health, vitality, emotional and social well-being [23] with higher scores defining a more favourable health state. Two norm-based summary scales of function and well-being are derived using standardised methods, the physical (PCS) and mental (MCS) component summary. As part of this analysis, MCS scores were tracked to establish the stability (or otherwise) of the patient’s mood. The SF-36 was completed at the commencement of a treatment cycle and at the end of study visit.
There was data missing at random from the MOTIF database, which was not included in this secondary analysis. The missing data constituted less than 7% of all the MDASI, SF-36 and SOMA6 variables and approximately 16% of the haemoglobin values.
Data analyses
For this analysis, only data from the 65 men with prostate cancer in the MOTIF database was used.
To establish the pattern of fatigue kinetics using the MDASI scores across a 21-day treatment cycle, all the raw, daily MDASI figures were collated according to treatment cycle (1–4) and treatment cycle day (day 1–day 21). Men were divided according to modafinil exposure, never-smoker and current/past-smoker status, age quartiles and cumulative docetaxel exposure (where pre-trial docetaxel cycle number was combined with trial docetaxel cycle number).
For each of these groups, the mean, standard deviation and 95% confidence interval of the daily raw MDASI scores were calculated with the assistance of EXCEL and then graphed and analysed using GraphPad Prism. A two-way ANOVA was performed (with Tukey’s or Sidak’s multiple comparisons test) on the calculated means in each data set to establish if the differences observed reached statistical significance.
The raw SOMA6 scores were calculated and represented as the percentage of patients with clinically significant fatigue. Individual answers to each item on the SOMA6 were analysed to provide an understanding of the nature of the fatigue state. A chi-squared test was performed to ascertain statistical significance.
The SF-36 MCS and haemoglobin levels were tracked across the treatment cycles. The mean, standard deviation, 95% confidence interval of the SF-36 MCS scores and haemoglobin levels were calculated with the assistance of EXCEL. The database was also interrogated to determine the presence of clinically significant anaemia and haemoglobin range.
Results
Study population
Sixty-five men with metastatic prostate cancer from the MOTIF study were eligible for analysis, and Table 1 summarises their characteristics.
Fatigue kinetics across treatment cycles
The mean MDASI fatigue scores from day 1 to 21, across 4 cycles of docetaxel, revealed that scores were higher from day 1 to 7, peaking at day 5–6 (Fig. 1). The pattern is similar across the four treatment cycles. However, there was a significant difference (p < 0.05) when cycle 1 and cycle 2, and cycle 2 and cycle 4, were compared, with higher mean fatigue scores in cycle 1 and cycle 4.
To establish the impact of cumulative docetaxel exposure on fatigue kinetics, the daily MDASI scores were analysed according to cumulative docetaxel exposure (Fig. 2). Qualitatively, there appears to be little impact of cumulative docetaxel exposure, and the difference did not reach statistical significance. In patients exposed to 3–5 cumulative cycles, the fatigue kinetics appear slightly different. Scores tended to be higher in the first and last week following docetaxel exposure, a pattern not reflected in the 6 and 7–11 cumulative cycle groups. For patients in the 6 and 7–11 cumulative cycle groups, the fatigue kinetics were similar to those seen across all patient groups (Fig. 1).
MDASI fatigue scores across four treatment cycles were combined and then analysed based on exposure to modafinil (Fig. 3). Qualitatively, the mean fatigue scores for the modafinil arm were significantly lower on treatment days 1–17 and day 21 (p < 0.05) when compared to placebo.
Mean MDASI scores across a treatment cycle and separated into age quartiles (25th: 68 years; 50th: 73 years; 75th: 80 years; range 55–90 years; mean 73 years) (Fig. 4). Men aged between 55 and 67 years had significantly lower fatigue scores when compared to their older male counterparts aged 68–72 years (p < 0.0001), 73–79 years (p = 0.0009) and 80–90 years (p < 0.0001). Significant differences were also seen when the 68–72 year old group was compared to the 73–79 year old group (p = 0.006) and when the 73–79 year old group was compared to the 80–90 year old group (p < 0.0001).
When the mean MDASI scores across all 4 cycles, for all patients, are plotted across a cycle length and then separated according to smoking status, the overall shape of the curves is the same, and whilst smokers (ex and current) appear to have higher fatigue scores during the first week, this trend did not reach statistical significance.
Nature of docetaxel-related fatigue across treatment cycles
The SOMA6 scores were analysed at each visit, across all patient groups, to better understand the nature of docetaxel-related fatigue. At one visit (baseline), 57/58 (~98%) of men completing the SOMA6 survey reported a clinically significant fatigue state; however, this decreased significantly to 27/54 people (50%) after treatment cycles were commenced.
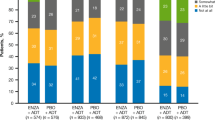
When the SOMA6 scores were analysed according to question number and cycle, another distinct, statistically significant pattern emerged (Fig. 5). Across each visit during the study, patients reported higher scores (more distress) for questions 2, 3, and 6 (p < 0.05). These questions relate to the need to sleep longer, a feeling of prolonged tiredness after activity and having tired muscles after activity.
SOMA 6 questionnaires answered at each visit (V1–V5), outlining the collated data according to SOMA6 question number (Q1–Q6); SOMA6 questions 1–6 outlined; two asterisks indicate statistically significant difference across visits, indicating patients likely experienced the need to sleep longer and both prolonged fatigue and tired muscles after activity
Impact of mood and anaemia on docetaxel-related fatigue across treatment cycles
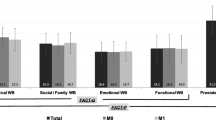
To track and account for changes in mood during the MOTIF treatment period, the SF-36 MCS data was calculated and analysed prior to commencement of each treatment cycle (Table 2). The MCS scores are similar across the treatment visits, indicating a little change in mood status.
Haemoglobin was assessed at the beginning of each treatment cycle. The levels were tracked across the study period, and there was no significant difference in the mean haemoglobin across study cycles (data not shown). Of the 65 men included in this analysis, three had a clinically significant change in haemoglobin during the study period. Haemoglobin dropped by no more than 2.5 g/dL, to a trough of 8.3 g/dL.
Discussion
In Australia, prostate cancer accounts for 30% of all new cancer diagnoses (excluding non-melanoma skin cancers) in men. It is the second most common cause of cancer-related death and the fourth leading cause of death in males, with 75% of these diagnoses occurring in men aged 65 years and over [24].
Chemotherapy has traditionally been reserved for overt metastatic disease, in the castrate-resistant setting, after failure of hormone deprivation. Pivotal trials have shown that docetaxel improves median overall survival. Docetaxel and estramustine improved median survival by nearly 2 months, when compared to mitoxantrone and prednisolone in the SWOG 9916 study [13]. The TAX-327 trial showed improved quality of life, pain control and overall survival with a 21-day cycle of docetaxel and prednisolone, when compared to mitoxantrone [14]. This study was practice changing, and docetaxel is the first line cytotoxic for management of advanced CRPC, in patients who can tolerate chemotherapy.
Recently, docetaxel has moved earlier into the treatment paradigm for hormone sensitive prostate cancer (HSPCa). The pivotal STAMPEDE [15] and CHAARTED [16] phase III randomised trials both demonstrated that patients with newly diagnosed HSPCa had improved overall survival when docetaxel was commenced within 12 weeks of hormone deprivation. These trials have led to earlier exposure of docetaxel in the hormone sensitive setting also.
In terms of extrapolating the findings from our analysis to the HSPCa population, it is important to note that the patients receiving docetaxel in CHAARTED and STAMPEDE did not routinely receive concomitant prednisolone. The original MOTIF trial and this analysis only includes patients receiving docetaxel, with prednisolone, for CRPC, so it is unclear if these results can be extrapolated to the HSPCa population.
CRF is a common, debilitating symptom for patients with cancer, disproportionate to exertion level and not relieved by rest [25]. In a large sample of breast cancer patients who had received adjuvant systemic therapy, 26% met clinical criteria for CRF at the completion of treatment [26]. In another large prospective study, again predominantly of women with breast cancer, utilising strict application of diagnostic criteria, the prevalence of CRF at least 12 months after systemic therapy completion was 17% [27].
The aetiology of CRF is unknown but is probably multifactorial and likely involves dysregulation of several interrelated physiological, biochemical and psychological systems [28]; all of which are affected by cancer and chemotherapy. Several different mechanisms of CRF have been proposed. In older adults with cancer and fatigue, mitochondrial dysregulation, oxidative stress, chronic inflammation and aberrant changes in neurotransmitter signalling have all been postulated [29]. Hypogonadism via castration remains an important potential mechanism for the development of fatigue in men with metastatic prostate cancer [30].
Chemotherapy-related fatigue is also a common and debilitating, therapy-related fatigue state and an appropriate understanding of its nature, and fatigue kinetics will help guide appropriate management.
The primary instrument to record fatigue for the current analysis, the MDASI, is a valid, reliable and sensitive symptom-assessment tool for men with prostate cancer [31]. As seen in Fig. 1, the burden of fatigue qualitatively seems to be greatest in the first week of the cycle, immediately after exposure to docetaxel, and diminishes in the latter 14 days. This pattern suggests that docetaxel exposure has a direct but likely reversible impact on fatigue kinetics.
Cumulative docetaxel exposure appears unlikely to contribute to a more severe fatigue state. Patients exposed to more docetaxel cycles did not report significantly higher MDASI scores across a treatment cycle (Fig. 2). For patients exposed to 3–5 cumulative cycles, the fatigue kinetics are slightly different. Scores tended to be higher in the first and last week following docetaxel exposure, and this pattern was not reflected in the other cumulative cycle groups. Whilst the mechanism behind this is unclear, the number of patients included in each cumulative cycle group may confound these results. Given that the median number of cycles for all 65 men was 6 and 35 men fell into this category alone, the sub-division was necessarily unequal. Regardless, the data does suggest that cumulative docetaxel cycle exposure does not necessarily contribute to this element of fatigue kinetics.
There was a difference in fatigue scores when men exposed to modafinil were compared to placebo (Fig. 3). Mean MDASI scores in the modafinil arm were significantly lower from days 1 to 17 and on day 21, indicating less severe fatigue. These results are reflective of the non-significant trend towards a treatment effect seen in the original MOTIF study. Interestingly, the overall pattern of fatigue kinetics in both treatment arms is similar, with scores highest in the first week and returning to baseline at the end of the treatment cycle. Modafinil, a non-amphetamine psychostimulant, has been studied as an agent for CRF for the past decade [32]. These studies combined with this secondary analysis highlight that the treatment of fatigue is complex and multifaceted. Modafinil may have a differential impact on fatigue depending on a number of variables.
Other pharmacological agents such as dexamethasone [33], methylphenidate [34] and traditional Chinese medicine [35] have also been studied, with mixed results. Whilst non-pharmacological approaches such as aerobic exercise [36], medical qijong [37] and cognitive behavioural therapy [38] have shown promise, no intervention has been efficacious enough to be recommended for the management of chemotherapy-related fatigue or CRF states. These findings likely reflect the complexity of fatigue management and the need for an approach that identifies and manages multiple variables.
When analysing the impact of age on fatigue kinetics, it was qualitatively and statistically evident that men in the youngest age bracket (55–68 years) had significantly lower fatigue scores than older men (Fig. 4). The pattern of MDASI fatigue scores across treatment cycles was largely unchanged. The higher fatigue scores in older men have been noted in previous analyses [39] and may be related to frailty in the older population, which was not measured in MOTIF.
Men who had a current or past history of smoking tended to have higher overall fatigue scores, but this did not reach statistical significance. A retrospective study of 522 patients, designed to investigate the differences in symptom burden across smoking status in patients with cancer found that smokers experienced more pain, fatigue, diminished appetite, mood disorders and insomnia when compared to non-smokers [40].
The SOMA6 data provided interesting insights into the nature of docetaxel-related fatigue. The data indicated that patients felt they needed to sleep longer and experience both prolonged tiredness and muscle fatigue after activity (Fig. 5). This suggests that docetaxel-related fatigue is a combination of pathological and physical fatigue and is experienced throughout the treatment period. In addition, a greater percentage of patients recorded a clinically significant fatigue state at study commencement, and this decreased markedly as treatment commenced.
The presence of anxiety, depression and anaemia can confound fatigue scores. Fatigue is a common symptom of depression and a large survey of breast cancer survivors showed that they commonly co-exist [41]. The SF-36 MCS scores were similar at the beginning of each treatment cycles (Table 2). Haemoglobin levels tracked throughout the study period were also stable. This data indicates that changes in mood symptoms and anaemia are unlikely confounders in this analysis.
There are limitations associated with this secondary analysis. It is a retrospective study, analysing data from the MOTIF database. Docetaxel-related fatigue was not the primary end-point of the MOTIF study, which instead analysed the efficacy of modafinil. However, since at least one-third of patients included in this secondary analysis were given placebo, and modafinil was found to have a non-significant treatment impact on fatigue, we argue that the kinetics of fatigue were not appreciably different between the treatment group and placebo. In addition, the number of patients included in the treatment cycles diminished with time, making interpretation of the difference in fatigue kinetics across the four treatment cycles challenging.
Whilst information about the presence of thyroid dysfunction was available for all patients screened for the MOTIF trial, TSH was not re-evaluated during the study period. So whilst hypothyroidism cannot be objectively ruled out as a confounder, it is far less common than CRPC and is considered unlikely to be a variable contributing to the fatigue states seen in this analysis.
Our findings highlight the complex nature of docetaxel-related fatigue and the interplay of physical, psychological and cognitive factors. Given the depth and breadth of diagnostic possibilities when a cancer patient complains of fatigue, a structured approach, such as a semi-structured interview [11] may identify discriminatory phenomena and provide the key for future therapeutic interventions.
Conclusion
In this analysis, we have described fatigue kinetics and provided insight into the nature of docetaxel-related fatigue in advanced prostate cancer. These results highlight the complexity of docetaxel-related fatigue and variables that have an impact on fatigue kinetics. It is highly likely that an interplay of physical and pathological factors contribute to fatigue in this setting, and identification through structured interview may be the most beneficial approach to patients affected by this troublesome symptom complex.
References
Hovey E, Souza P de, Marx G, et al (2014) Phase III, randomized, double-blind, placebo-controlled study of modafinil for fatigue in patients treated with docetaxel-based chemotherapy. Support Care Cancer 22:1233–1242. doi: 10.1007/s00520-013-2076-0
Cella D (1997) The Functional Assessment of Cancer Therapy-Anemia (FACT-An) Scale: a new tool for the assessment of outcomes in cancer anemia and fatigue. Semin Hematol 34:13–19
Hofman M, Morrow GR, Roscoe JA et al (2004) Cancer patients’ expectations of experiencing treatment-related side effects: a University of Rochester Cancer Center--Community Clinical Oncology Program study of 938 patients from community practices. Cancer 101:851–857. doi:10.1002/cncr.20423
Berger AM, Mooney K, Alvarez-Perez A et al (2015) Cancer-related fatigue, version 2.2015. J Natl Compr Cancer Netw 13:1012–1039
Heins MJ, Korevaar JC, Rijken PM, Schellevis FG (2013) For which health problems do cancer survivors visit their General Practitioner? Eur J Cancer 49:211–218. doi:10.1016/j.ejca.2012.07.011
Jacobsen PB, Hann DM, Azzarello LM et al (1999) Fatigue in women receiving adjuvant chemotherapy for breast cancer: characteristics, course, and correlates. J Pain Symptom Manag 18:233–242
Evans WJ, Lambert CP (2007) Physiological basis of fatigue. Am J Phys Med Rehabil 86:S29–S46
(2002) Chronic fatigue syndrome. Clinical practice guidelines--2002. Med J Aust 176 Suppl:S23–56
Cleeland CS, Mendoza TR, Wang XS et al (2000) Assessing symptom distress in cancer patients: the M.D. Anderson Symptom Inventory. Cancer 89:1634–1646. doi:10.1002/1097-0142(20001001)89:7<1634::AID-CNCR29>3.0.CO;2-V
Hadzi-Pavlovic D, Hickie IB, Wilson AJ et al (2000) Screening for prolonged fatigue syndromes: validation of the SOFA scale. Soc Psychiatry Psychiatr Epidemiol 35:471–479
Bennett BK, Goldstein D, Chen M et al (2014) Characterization of fatigue states in medicine and psychiatry by structured interview. Psychosom Med 76:379–388
Roscoe JA, Kaufman ME, Matteson-Rusby SE et al (2007) Cancer-related fatigue and sleep disorders. Oncologist 12(Suppl 1):35–42. doi:10.1634/theoncologist.12-S1-35
Petrylak DP, Tangen CM, Hussain MH et al (2004) Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med 351:1513–1520. doi:10.1056/NEJMoa041318
Tannock IF, Wit R de, Berry WR, et al (2004) Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 351:1502–1512. doi: 10.1056/NEJMoa040720
James ND, Sydes MR, Clarke NW et al (2016) Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 387:1163–1177. doi:10.1016/S0140-6736(15)01037-5
Sweeney CJ, Chen Y-HH, Carducci M et al (2015) Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med 373:737–746. doi:10.1056/NEJMoa1503747
Al-Batran S-EE, Hozaeel W, Tauchert FK et al (2015) The impact of docetaxel-related toxicities on health-related quality of life in patients with metastatic cancer (QoliTax). Ann Oncol 26:1244–1248. doi:10.1093/annonc/mdv129
Dreicer R, Petrylak D, Agus D et al (2007) Phase I/II study of bortezomib plus docetaxel in patients with advanced androgen-independent prostate cancer. Clin Cancer Res 13:1208–1215. doi:10.1158/1078-0432.CCR-06-2046
Awada A, Hendlisz A, Christensen O et al (2012) Phase I trial to investigate the safety, pharmacokinetics and efficacy of sorafenib combined with docetaxel in patients with advanced refractory solid tumours. Eur J Cancer 48:465–474. doi:10.1016/j.ejca.2011.12.026
Goldstein D, Bennett BK, Webber K et al (2012) Cancer-related fatigue in women with breast cancer: outcomes of a 5-year prospective cohort study. J Clin Oncol 30:1805–1812. doi:10.1200/JCO.2011.34.6148
Hickie IB, Davenport TA, Hadzi-Pavlovic D et al (2001) Development of a simple screening tool for common mental disorders in general practice. Med J Aust 175(Suppl):S10–S17
Brazier JE, Harper R, Jones NM et al (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164. doi:10.1136/bmj.305.6846.160
Farivar S, Cunningham W, Hays R (2007) Correlated physical and mental health summary scores for the SF-36 and SF-12 health survey, V.1. Health Qual Life Out 5:1–8. doi:10.1186/1477-7525-5-54
Ketchandji M, Kuo Y-FF, Shahinian VB, Goodwin JS (2009) Cause of death in older men after the diagnosis of prostate cancer. J Am Geriatr Soc 57:24–30. doi:10.1111/j.1532-5415.2008.02091.x
Glaus A, Crow R, Hammond S (1996) A qualitative study to explore the concept of fatigue/tiredness in cancer patients and in healthy individuals. Support Care Cancer 4:82–96
Andrykowski MA, Schmidt JE, Salsman JM et al (2005) Use of a case definition approach to identify cancer-related fatigue in women undergoing adjuvant therapy for breast cancer. J Clin Oncol 23:6613–6622. doi:10.1200/JCO.2005.07.024
Cella D, Davis K, Breitbart W, Curt G (2001) Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J Clin Oncol 19:3385–3391
Ryan JL, Carroll JK, Ryan EP et al (2007) Mechanisms of cancer-related fatigue. Oncologist 12(Suppl 1):22–34. doi:10.1634/theoncologist.12-S1-22
Alexander NB, Taffet GE, Horne FM et al (2010) Bedside-to-bench conference: research agenda for idiopathic fatigue and aging. J Am Geriatr Soc 58:967–975. doi:10.1111/j.1532-5415.2010.02811.x
Naeim A, Aapro M, Subbarao R, Balducci L (2014) Supportive care considerations for older adults with cancer. J Clin Oncol 32:2627–2634. doi:10.1200/JCO.2014.55.3065
Jones D, Zhao F, Fisch MJ et al (2014) The validity and utility of the MD Anderson symptom Inventory in patients with prostate cancer: evidence from the Symptom Outcomes and Practice Patterns (SOAPP) data from the Eastern Cooperative Oncology Group. Clin Genitourin Cancer 12:41–49. doi:10.1016/j.clgc.2013.07.003
Spathis A, Fife K, Blackhall F et al (2014) Modafinil for the treatment of fatigue in lung cancer: results of a placebo-controlled, double-blind, randomized trial. J Clin Oncol 32:1882–1888. doi:10.1200/JCO.2013.54.4346
Yennurajalingam S, Frisbee-Hume S, Palmer JL et al (2013) Reduction of cancer-related fatigue with dexamethasone: a double-blind, randomized, placebo-controlled trial in patients with advanced cancer. J Clin Oncol 31:3076–3082. doi:10.1200/JCO.2012.44.4661
Bruera E, Yennurajalingam S, Palmer JL et al (2013) Methylphenidate and/or a nursing telephone intervention for fatigue in patients with advanced cancer: a randomized, placebo-controlled, phase II trial. J Clin Oncol 31:2421–2427. doi:10.1200/JCO.2012.45.3696
Barton DL, Liu H, Dakhil SR et al (2013) Wisconsin ginseng (Panax quinquefolius) to improve cancer-related fatigue: a randomized, double-blind trial, N07C2. J Natl Cancer Inst 105:1230–1238. doi:10.1093/jnci/djt181
Cramp F, Byron-Daniel J (2012) Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev 11:CD006145. doi:10.1002/14651858.CD006145.pub3
Oh B, Butow P, Mullan B et al (2010) Impact of medical qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial. Ann Oncol 21:608–614. doi:10.1093/annonc/mdp479
Goedendorp MM, Gielissen MF, Verhagen CA, Bleijenberg G (2009) Psychosocial interventions for reducing fatigue during cancer treatment in adults Cochrane Database Syst Rev:CD006953. doi:10.1002/14651858.CD006953.pub2
Respini D, Jacobsen PB, Thors C et al (2003) The prevalence and correlates of fatigue in older cancer patients. Crit Rev Oncol Hematol 47:273–279. doi:10.1016/S1040-8428(02)00176-2
Novy DM, Lam C, Gritz ER et al (2012) Distinguishing features of cancer patients who smoke: pain, symptom burden, and risk for opioid misuse. J Pain 13:1058–1067. doi:10.1016/j.jpain.2012.07.012
Bower JE, Ganz PA, Desmond KA et al (2000) Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol 18:743–753
Acknowledgments
The original MOTIF study (published in 2014) was conducted with funding support from Sanofi Australia Pty Ltd. No funding was supplied for this secondary analysis. The authors would like to thank the patients and their caregivers involved in the original MOTIF study. AB would like to acknowledge the assistance of Dr. Kirsten Hogg, who helped with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
All procedures performed were in accordance with the ethical standards of the institutional research boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this study, formal consent was not required.
Rights and permissions
About this article
Cite this article
Bergin, A.R.T., Hovey, E., Lloyd, A. et al. Docetaxel-related fatigue in men with metastatic prostate cancer: a descriptive analysis. Support Care Cancer 25, 2871–2879 (2017). https://doi.org/10.1007/s00520-017-3706-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3706-8