Abstract
Purpose
Minimal data exist regarding documentation of therapy-associated infertility risk (IR) and fertility preservation (FP) options during the initial oncology consultation prior to systemic therapy. This study investigated factors affecting IR/FP documentation and assessed the effect of implementation of an Adolescent and Young Adult (AYA) program on documentation rates.
Methods
A retrospective review of charts of patients receiving gonadotoxic therapy was undertaken for documentation of IR/FP pre- and post-implementation of an AYA program. Change in documentation rates was assessed using univariate and multiple logistic regression.
Results
A total of 173 charts were reviewed. On univariate analysis, IR/FP documentation was less likely if patients had metastatic disease (P < 0.01, P < 0.01), by tumor type (P < 0.01, P < 0.01), received less intensive chemotherapy (P = 0.03, P = 0.06), were older (P = 0.14, P < 0.01), had more children (P < 0.01, P < 0.01), or lacked AYA program involvement (P < 0.01, P < 0.01). FP discussion was more common in males (P = 0.02). On multivariable analysis, more children (P = 0.01, P = 0.03), older age (P < 0.01, P < 0.01), tumor type (P < 0.01, P = 0.01), stage (P = 0.02, NS), relationship (P = 0.03, NS), and lack of AYA involvement (P < 0.01, P < 0.01) were associated with lower rates of IR/FP documentation. Following AYA program implementation, IR/FP rates increased from 56% (CI 46–65%) to 85% (CI 74–92%, P < 0.01) and 54% (CI 45–64%) to 86% (CI 75–93%, P < 0.01), respectively. The effect of AYA program implementation on IR/FP documentation was most noticeable in leukemia, lymphoma, and breast groups (P < 0.01).
Conclusions
Implementing an AYA consultation service at an adult cancer institution had a positive effect on the rates of IR/FP documentation. Specific programming can improve service delivery to AYA cancer patients, and fertility counseling should be integrated for patients undergoing gonadotoxic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The association between cancer treatment and loss of fertility is well known. Cytotoxic chemotherapy, especially alkylating agents [1], and radiation, particularly to the pelvic region [2], affect female and male fertility by damaging cell division and DNA function within the oocytes and spermatogonia, respectively [1]. The degree of impact on fertility ultimately depends on both patient- and treatment-related factors including baseline fertility, age of the patient, cumulative dose of alkylating drugs, dose intensity, and specific treatment regimens [1]. Despite increasing awareness of therapy-associated infertility and recent publication of guidelines by the American Society of Clinical Oncology (ASCO) supporting fertility preservation (FP) counseling [3], variable rates of discussions regarding these risks remain [4–6]. For example, one study reported that only 26% of providers had documented fertility discussions and 13% had documented referrals made to a fertility specialist [7].
Supportive care in cancer is defined as the prevention and management of side effects of cancer and its treatment across the full treatment continuum. Counseling regarding potential infertility risk (IR) and FP options prior to cancer therapy initiation falls under the supportive care paradigm and is key to holistic adolescent and young adult (AYA) management, independent of prognosis or parity [3, 8, 9]. FP discussions are of great importance to patients [10], can improve quality of life [11], and can contribute to psychological health [12]. The increasing success of FP options in females [10, 13, 14] in addition to well-established FP options for males with sperm cryopreservation further underlies the need for equitable access to discussion regarding FP. However, barriers to these discussions still exist including those related to the patient (failing to mention infertility concerns due to being overwhelmed with the cancer diagnosis) [2], the physician (lack of time, inadequate knowledge on fertility preservation methods, not wishing to delay treatment) [15–19], and institution (lack of policy or dedicated programming) [15, 20].
With increasing awareness of the specific needs of AYA cancer patients [21], such as the requirement for unique psychosocial supports, there has been an increasing impetus to develop AYA dedicated programming in multi-disciplinary cancer centers. The majority of AYA patients are managed within adult cancer centers that provide care based on a disease-focused model. Dedicated AYA programming in these centers has been aimed at addressing the distinct requirements of this population [21]. However, there is little real-time data on the effects and benefits of implementing AYA programs, especially with regard to the effect of these programs on fertility counseling.
The Princess Margaret Cancer Centre (PM) is a Canadian large urban cancer center that sees approximately 1500 new AYA patients (aged 15 to 39) per year [21]. In order to address the specific needs of its AYA patient population and to enhance their overall treatment experience, a program was launched in May 2014 with a number of aims: (1) implementing standardized AYA assessments, (2) educating oncology health-care providers on AYA needs, (3) providing patient consultation and psychosocial support, and (4) ensuring AYA have access to relevant hospital and community programs. An important component of the program included educating health-care providers on IR and FP, developing fertility-related resources (e.g., pamphlets and institutional guidelines), and promoting routine pre-therapy counseling to patients by a clinical nurse specialist (CNS). Patients were referred by their health-care teams to the AYA CNS, who then met with them in consultation and reviewed and provided information and counseling on all possible needs including IR and FP.
As a discussion of IR and FP options is a key element aiming to mitigate the gonadotoxic effects of chemotherapy, this study aimed to (1) determine factors predicting the prevalence of documented IR or FP discussions and (2) compare the proportion of documented IR/FP discussions before and after the implementation of the AYA program at PM.
Methods
Fertility resources pre- and post-AYA program
Prior to the implementation of the AYA program, an analysis was conducted to identify available fertility services and resources accessed by disease site groups at PM and assess awareness of practitioners regarding these resources. Those disease sites familiar with making referrals to local fertility clinics did not necessarily have direct contact with them, nor were there pathways for referring inpatients or those requiring urgent fertility preservation. Furthermore, although a Canadian-wide fertility reimbursement program was available to patients, this resource was not well known by the health-care teams. In this setting, the AYA program was initiated in May 2014 and a component of the service delivery was provision of health-care provider education on IR and FP, development of specific fertility-related resources, and advocating and offering routine pre- and post-therapy counseling to patients led by the CNS.
Design
To assess the effect of the AYA program on documentation of discussion of IR and FP options, a retrospective analysis of two patient cohorts was performed: (1) Cohort A included consecutive AYA patients encountered at PM between January 1, 2013, and December 31, 2013 (prior to the AYA program initiation) and (2) cohort B included AYA patients encountered between November 1, 2014, and April 30, 2015 (6 months post-AYA program implementation).
After institutional research ethics board approval, patient records were identified via the PM Cancer Registry. Details regarding patient demographics, tumor type, and treatment and clinical details (documentation of IR and FP discussion; whether documentation was conducted by the AYA CNS or primary oncologist) were retrospectively retrieved from medical records. Institutional review board approval was obtained prior to study initiation. For this type of retrospective study, formal informed consent was not required.
Eligibility
Patients were eligible for inclusion if they had treatment that involved any type of chemotherapy or pelvic radiotherapy; were less than age 40 years at diagnosis; were diagnosed with sarcoma, leukemia, lymphoma, testicular cancer, or breast cancer; and had a documented initial consultation with a PM oncologist. These five tumor sites were selected as these cancers have the greatest incidence in this age group. Patients were excluded if their consultation at PM was for a second opinion or if they had received previous gonadotoxic therapy.
Medical record abstraction
A standardized abstraction form was used for all eligible cases. Three abstractors were trained (JM, ST, NP) under supervision (JL, AG) using sample cases and forms. Abstractors reviewed the medical records with the supervising physician, and each case was subsequently cross reviewed to ensure homogeneity. Abstractors defined “infertility risk” as any potential risk to future reproduction from the therapy being proposed, and “fertility preservation” was defined as any potential option to preserve future reproduction. At the end of case abstraction, 10% of cases were revisited to ensure accuracy. All abstractors entered relevant medical record data into a hard-copy abstraction form and then transferred it onto a password-protected electronic case report form stored on the hospital server. This information was de-identified when processed for further statistical analysis.
Statistical analysis
Serial cases were identified pre- (cohort A) and post-AYA program initiation (cohort B) with an aim for a sample size of 100 patients in each cohort (40 cases per histology) and calculated based on accounting for the number of variables that were being investigated. Descriptive statistics were used to report demographic and clinical data and were presented as means, medians, and ranges for continuous factors and frequencies for categorical factors. The proportion of patients with documentation of IR and FP with the 95% confidence interval (CI) was calculated with binomial distribution. Exploratory univariate and multivariable analyses were used to evaluate factors that were associated with fertility discussions on the entire cohort (cohort A + B). Logistic regressions were performed to assess the associations of discussions with demographic and clinical factors. Chemotherapy infertility risk groups were defined as low <20% IR or high >80% IR (Supplementary Table 1) [9]. Data were analyzed with SAS v9.4. For the final multiple models, a P value of <0.05 was considered statistically significant.
Results
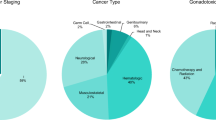
A total of 173 patient records met the inclusion criteria for the study (cohort A 108, cohort B 65). Baseline patient demographics are shown in Table 1. Patients had a median age of 30 years (range 17–39) with the majority being male (57%) and with localized disease (53%). The pre- and post-AYA initiation cohorts were well balanced with regard to baseline demographics.
Predictors of documentation of IR and FP
Table 2 lists the demographic variables and summarizes the univariate logistic regression models for the predictors of IR and FP discussion. Documentation of IR was significantly less likely in patients with metastatic disease (P value < 0.001), in patients treated with low-infertility-risk chemotherapy when compared to those treated with intermediate- or high-infertility-risk chemotherapy (P value = 0.03), in certain cancer types (e.g., leukemia compared to testicular cancer) (P value = 0.003), in those who already had children (P value < 0.001), and in those without the AYA program involvement (P value < 0.001). Age and gender were not factors in predicting IR in univariate analysis. Documentation of FP options was significantly less likely in patients with metastatic disease (P value < 0.001), in females (P value = 0.02), and according to tumor type (P value < 0.001). In addition, documentation of FP options was significantly less likely in older patients (P value = 0.006), in those with children (P value < 0.001), and in those without AYA program involvement (P value < 0.001). On univariate analysis, documented knowledge of relationship status (in a relationship versus not in a relationship) did not predict either IR or FP option discussion.
Based on univariate selection criteria (i.e., P < 0.25 [22] or clinically meaningful variables), the following factors were entered into the multivariable model: stage, age, number of children, relationship, tumor type, gender, chemo-infertility risk group, and AYA program involvement. Table 3 summarizes the significant factors on the multivariable logistic regression models for fertility-related IR and FP discussion. Increasing age (P value < 0.01), increased number of children (P value = 0.01), higher tumor stage (P value = 0.02), relationship status (P value = 0.03), certain tumor types (leukemia compared to testicular cancer) (P value < 0.01), and lack of involvement in the AYA program (P value < 0.01) were associated with less IR documentation. Certain tumor types (e.g., leukemia compared to testicular cancer) (P value = 0.01), increasing age (P value < 0.01), increasing number of children (P value = 0.03), and lack of involvement in the AYA program (P value < 0.01) were also predictive of lower likelihood of FP documentation.
Implementation of the AYA program
Following the implementation of the AYA service, rates of IR discussion increased from 56% (CI 46–65%) to 85% (CI 74–92%, P value < 0.0001) while rates of FP option documentation increased from 54% (CI 45–64%) to 86% (75–93%, P value < 0.0001). The overall rate of documentation for the whole study (cohorts A and B combined) was 115 (66%) for IR and 114 (66%) for FP. Documentation in cohort B (post-AYA program initiation) was conducted solely by the primary oncologist in 44% and with involvement of or by the AYA CNS in 56%. The effect of AYA program improvement on IR discussion was most noticeable in patients with leukemia (20% to 73%, P value < 0.001), lymphoma (56% to 88%, P value = 0.03), and breast cancer (59% to 94%, P value = 0.01) (Fig. 1a). The AYA program effect on FP option documentation was also seen in leukemia (20% to 73%, P value < 0.001), lymphoma (61% to 100%, P value = 0.004), and breast cancer (41% to 89%, P value = 0.001) (Fig. 1b).
Discussion
A major focus of the AYA program at PM is to bring dedicated support to AYA patients, provide additional counseling when required, and offer clinicians’ resources based on their information needs. Regarding fertility, the program offered routine pre-chemotherapy/radiotherapy counseling as well as clinician education and development of fertility-related resources for patients and clinicians (e.g., patient pamphlets and institutional guidelines). To our knowledge, this is the first study of its kind demonstrating a significantly positive impact of a dedicated AYA program on the rate of documentation of IR and FP options in multiple tumor types. This effect was mainly seen in leukemia, lymphoma, and breast cancer site groups, areas that were specifically targeted by our CNS. As mitigating cancer treatment toxicities is a component of supportive care, mechanisms to improve both delivery and documentation of infertility discussions are an important aspect of holistic management.
Of note, the overall rate of documentation for IR/FP of 66% for the entire cohort was higher than other similar published reports. The rate of documentation we observed was considerably higher than that reported by Quinn et al. [7], who showed an IR documentation rate of 26% and FP option discussion rate of 24% in 231 records across four institutions. While it may be assumed that FP options for men are readily accessible, Grover et al. recently reported documentation of fertility counseling in just 29% of males and 11% attempted sperm banking [23]. The higher documentation rates at our institution remain obscure although they may reflect awareness of fertility guidelines [24, 25] and the effect of the AYA program prior to routine consultations or potentially relate to institutional differences with regard to documentation rates. Since adherence to supportive care guidelines can be tenuous, the likelihood this accounts for such a large documentation increase is likely to be small [26].
Results of this study suggest that documentation rates of both IR and FP were less likely if patients had metastatic disease, had leukemia (compared with testicular cancer), received less intensive gonadotoxins, were of older age, and had more children. Health-care providers may tend to base fertility discussions on the stage of the malignancy, assuming that only patients with lower-risk disease would have concerns about potential infertility [27]. However, studies have indicated that fertility concerns are present regardless of extent of disease [27] and ASCO guidelines recommend discussion of fertility preservation whether or not patients have metastatic disease [3]. In fact, the delivery of information regarding IR and FP options should be uniform, even though the choice to proceed with actual intervention may vary. For example, the “7 + 3” cytarabine-daunorubicin induction regimen for leukemia is associated with a low risk of compromising fertility [28], and studies have indicated that even high doses of cytarabine have minimal effect on the chances of pregnancy in both male and female patients [29–31]. With such considerations, physicians may be less inclined to undergo fertility discussion when prescribing low-risk regimens (e.g., “7 + 3” for leukemia) when compared to moderate- or high-risk regimens that are heavy in alkylating agents. However, AYA patients want to have this information and be actively involved in the decision-making process [32], rather than health-care professionals making this decision independent of the patient. Ultimately, those who had received fertility counseling have less regret than those who did not [33, 34]. It may be impractical for an acutely unwell patient to go for any procedures to preserve fertility, especially with a new diagnosis of leukemia; however, a discussion regarding fertility risks should still occur and be documented by the health-care provider. For women, considerations of invasive procedures required for oocyte cryopreservation are particularly problematic especially in the setting of low blood counts, but information delivery and discussion remain key and are particularly important to avoid regret in this vulnerable population [35]. Even for men, being able to produce a semen sample may be challenging, but these factors should not preclude access to information and are crucial for holistic management. Moreover, it may be equally impractical to preserve fertility at relapse (e.g., leukemia where patients may be medically unwell at relapse), at which point the salvage treatment may in fact be sterilizing (e.g., allogeneic transplantation).
The findings that age predicted IR and FP discussions suggest that clinicians are inferring whether patients are interested in FP or assuming that patients are not of childbearing age (defined as age 18 to 45 years) [3, 34]. Female fertility declines above the age of 40 due to the sharp reduction in oocyte production starting from their late 30s [36]. With exposure to alkylator-based chemotherapy, there is accelerated decline of oocyte loss and increased chance of irreversible amenorrhea [37, 38]. The optimal time to raise FP options is prior to treatment [3], and clinicians should not assume any specific fertility preferences based on age alone and initiate discussion as early as possible. Many fertility clinics decline oocyte cryopreservation in women above the age of 42 years, but all patients in our study were less than age 40 years.
Regardless of the decision of proceeding to preservation, it has been shown that women benefit from an informed-decision-making process [34]. FP options for women are not as straightforward as certain tumor types may be sensitive to hormonal manipulation [39], processes that involve stimulating the ovaries and harvesting oocytes [40–42]. Many of the assisted reproductive technologies not only are physically and psychologically demanding [40] but also yield variable chances of a successful pregnancy in older-aged women [7]. For many women, the risk of infertility can be as distressing as the cancer diagnosis itself [41–43]. Some women indicate that fertility concerns have impacted their treatment decisions [27]. Post-treatment counseling should also occur and, although not measured in this study, is an important part of the service provided by our AYA team. Women may still have an opportunity for oocyte preservation following chemotherapy, and appropriate referrals for ovarian function assessment should be considered in survivorship.
In contrast, for men, there is no specific age threshold for sperm production [44]. Preserving fertility in men with cryopreservation of sperm is relatively straightforward and, with advances in technology, only one live sperm cell is required for fertilization of an oocyte [45]. Men should always be offered a choice to bank sperm prior to receiving cancer therapy. In specialized centers, testicular extraction of sperm can also be offered to men who are unable to produce a viable sample through ejaculation [46]. Systems such as our AYA program need to be put in place to ensure that clinicians are aware of and can access these options where appropriate.
There are some important limitations to this study: (1) given the retrospective nature of this study, lack of documentation does not necessarily mean that a fertility conversation did not occur [47, 48]; (2) we assume that the improvement in IR and FP documentation was temporally related to the AYA implementation; however, it is possible there may have been other factors driving the improvement such as insurance status and socioeconomic factors [7]; (3) we were unable to accurately assess whether the IR and FP option discussion led specifically to fertility specialist referral; and lastly, (4) it is unknown whether fertility counseling led to increased patient satisfaction [19].
In conclusion, we were able to identify baseline predictors of fertility discussions and found that the rate of documentation of IR and FP options was significantly improved after a dedicated AYA program which included provider education, patient materials, and specific AYA consultation. A more in-depth assessment of AYA programming is required, specifically whether interventions such as these improve referral to fertility specialists as well as increased patient and clinician satisfaction.
References
Levine J, Canada A, Stern CJ (2010) Fertility preservation in adolescents and young adults with cancer. J Clin Oncol 28:4831–4841. doi:10.1200/JCO.2009.22.8312
Schover LR (1999) Psychosocial aspects of infertility and decisions about reproduction in young cancer survivors: a review. Med Pediatr Oncol 33:53–59
Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, Quinn G, Wallace WH, Oktay K, American Society of Clinical Oncology (2013) Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31:2500–2510. doi:10.1200/JCO.2013.49.2678
Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, Keefe DL, Albrecht TL (2009) Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol 27:5952–5957. doi:10.1200/JCO.2009.23.0250
Forman EJ, Anders CK, Behera MA (2009) Pilot survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. J Reprod Med 54:203–207
Salsman JM, Yanez B, Smith KN, Beaumont JL, Snyder MA, Barnes K, Clayman ML (2016) Documentation of fertility preservation discussions for young adults with cancer: examining compliance with treatment guidelines. J Natl Compr Cancer Netw 14:301–309
Quinn GP, Block RG, Clayman ML et al (2015) If you did not document it, it did not happen: rates of documentation of discussion of infertility risk in adolescent and young adult oncology patients’ medical records. J Oncol Prac 11:137–144. doi:10.1200/JOP.2014.000786
Coccia PF, Altman J, Bhatia S et al (2012) Adolescent and young adult oncology. Clinical practice guidelines in oncology. J Natl Compr Cancer Netw 10:1112–1150
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K, American Society of Clinical Oncology (2006) American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol 24(18):2917–2931. doi:10.1200/JCO.2006.06.5888
Maltaris T, Seufert R, Fischl F, Schaffrath M, Pollow K, Koelbl H, Dittrich R (2007) The effect of cancer treatment on female fertility and strategies for preserving fertility. Eur J Obstet Gynecol Reprod Biol 130:148–155. doi:10.1016/j.ejogrb.2006.08.006
Wenzel L, Dogan-Ates A, Habbal R, Berkowitz R, Goldstein DP, Bernstein M, Kluhsman BC, Osann K, Newlands E, Seckl MJ, Hancock B, Cella D (2005) Defining and measuring reproductive concerns of female cancer survivors. J Natl Cancer Inst Monogr 34:94–98. doi:10.1093/jncimonographs/lgi017
Gorman JR, Su HI, Roberts SC, Dominick SA, Malcarne VL (2015) Experiencing reproductive concerns as a female cancer survivor is associated with depression. Cancer 121(6):935–942. doi:10.1002/cncr.29133
Seli E, Tangir J (2005) Fertility preservation options for female patients with malignancies. Curr Opin Obstet Gynecol 17:299–308
Morice P, Juncker L, Rey A, El-Hassan J, Haie-Meder C, Castaigne D (2000) Ovarian transposition for patients with cervical carcinoma treated by radiosurgical combination. Fertil Steril 74:743–748
Quinn GP, Vadaparampil ST, Bell-Ellison BA, Gwede CK, Albrecht TL (2008) Patient-physician communication barriers regarding fertility preservation among newly diagnosed cancer patients. Soc Sci Med 66:784–789. doi:10.1016/j.socscimed.2007.09.013
Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, Wilson C, Munster P (2007) Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv 1:146–155. doi:10.1007/s11764-007-0019-9
Schover LR, Brey K, Lichtin A, Lipschultz LI, Jeha S (2002) Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol 20:1890–1897
Goossens J, Delbaere I, Van Lancker A, Beeckman D, Verhaeghe S, Van Hecke A (2014) Cancer patients’ and professional caregivers’ needs, preferences and factors associated with receiving and providing fertility-related information: a mixed-methods systematic review. Int J Nurs Stud 51:300–319. doi:10.1016/j.ijnurstu.2013.06.015
Kelvin JF, Thom B, Benedict C, Carter J, Corcoran S, Dickler MN, Goodman KA, Margolies A, Matasar MJ, Noy A, Goldfarb SB (2016) Cancer and fertility program improves patient satisfaction with information received. J Clin Oncol 34:1780–1786. doi:10.1200/JCO.2015.64.5168
Schover LR, Brey K, Lichtin A, Lipschultz LI, Jeha S (2002) Knowledge and experience regarding cancer, infertility, and sperm banking in younger male survivors. J Clin Oncol 20:1880–1889
Gupta AA, Papadakos JK, Jones JM, Amin L, Chang EK, Korenblum C, Mina DS, McCabe L, Mitchell L, Giuliani ME (2016) Reimagining care for adolescent and young adult cancer programs: moving with the times. Cancer 122:1038–1046. doi:10.1002/cncr.29834
Hosmer DW, Lemeshow S (1989) Applied logistic regression. Wiley, New York
Grover NS, Deal AM, Wood WA, Mersereau JE (2016) Young men with cancer experience low referral rates for fertility counseling and sperm banking. J Oncol Pract 12:465–471. doi:10.1200/JOP.2015.010579
Clayman ML, Harper MM, Quinn GP, Reinecke J, Shah S (2013) Oncofertility resources at NCI-designated comprehensive cancer centers. J Natl Compr Cancer Netw 11:1504–1509
Reinecke JD, Kelvin JF, Arvey SR, Quinn GP, Levine J, Beck LN, Miller A (2012) Implementing a systematic approach to meeting patients’ cancer and fertility needs: a review of the Fertile Hope Centers Of Excellence program. J Oncol Pract 8:303–308. doi:10.1200/JOP.2011.000452
Aapro M, Molassiotis A, Dicato M, Peláez I, Rodríguez-Lescure Á, Pastorelli D, Ma L, Burke T, Gu A, Gascon P, Roila F (2012) The effect of guideline-consistent antiemetic therapy on chemotherapy-induced nausea and vomiting (CINV): the Pan European Emesis Registry (PEER). Ann Oncol 23:1986–1992
Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, Rosenberg R, Przypyszny M, Rein A, Winer EP (2004) Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol 22:4174–4183. doi:10.1200/JCO.2004.01.159
Salooja N, Chatterjee R, McMillan AK, Kelsey SM, Newland AC, Milligan DW, Franklin IM, Hutchinson RM, Linch DC, Goldstone AH (1994) Successful pregnancies in women following single autotransplant for acute myeloid leukemia with a chemotherapy ablation protocol. Bone Marrow Transplant 13(4):431–435
Molgaard-Hansen L, Skou AS, Juul A, Glosli H, Jahnukainen K, Jarfelt M, Jonmundsson GK, Malmros J, Nysom K, Hasle H, Nordic Society of Pediatric H, Oncology (2013) Pubertal development and fertility in survivors of childhood acute myeloid leukemia treated with chemotherapy only: a NOPHO-AML study. Pediatr Blood Cancer 60:1988–1995. doi:10.1002/pbc.24715
Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, Donaldson SS, Byrne J, Robison LL (2009) Fertility of female survivors of childhood cancer: a report from the childhood cancer survivor study. J Clin Oncol 27:2677–2685. doi:10.1200/JCO.2008.20.1541
Green DM, Kawashima T, Stovall M, Leisenring W, Sklar CA, Mertens AC, Donaldson SS, Byrne J, Robison LL (2010) Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol 28:332–339. doi:10.1200/JCO.2009.24.9037
Zebrack B, Isaacson S (2012) Psychosocial care of adolescent and young adult patients with cancer and survivors. J Clin Oncol 30:1221–1226. doi:10.1200/JCO.2011.39.5467
Partridge AH, Gelber S, Peppercorn J, Ginsburg E, Sampson E, Rosenberg R, Przypyszny M, Winer EP (2008) Fertility and menopausal outcomes in young breast cancer survivors. Clin Breast Cancer 8:65–69. doi:10.3816/CBC.2008.n.004
Letourneau JM, Ebbel EE, Katz PP, Katz A, Ai WZ, Chien AJ, Melisko ME, Cedars MI, Rosen MP (2012) Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer 118:1710–1717. doi:10.1002/cncr.26459
Connell S, Patterson C, Newman B (2006) A qualitative analysis of reproductive issues raised by young Australian women with breast cancer. Health Care Women Int 27:94–110. doi:10.1080/07399330500377580
Lansac J (1995) Delayed parenting. Is delayed childbearing a good thing? Hum Repro 10:1033–1035
Maltaris T, Weigel M, Mueller A, Schmidt M, Seufert R, Fischl F, Koelbl H, Dittrich R (2008) Cancer and fertility preservation: fertility preservation in breast cancer patients. Breast Cancer Res 10:206. doi:10.1186/bcr1991
Lobo RA (2005) Potential options for preservation of fertility in women. N Engl J Med 353:64–73. doi:10.1056/NEJMra043475
Partridge AH (2008) Fertility preservation: a vital survivorship issue for young women with breast cancer. J Clin Oncol 26:2612–2613. doi:10.1200/JCO.2008.16.1976
Surbone A, Petrek JA (1997) Childbearing issues in breast carcinoma survivors. Cancer 79:1271–1278
Dow KH (1994) Having children after breast cancer. Cancer Pract 2:407–413
Schover LR, Rybicki LA, Martin BA, Bringelsen KA (1999) Having children after cancer. A pilot survey of survivors’ attitudes and experiences. Cancer 86:697–709
Meirow D (1999) Ovarian injury and modern options to preserve fertility in female cancer patients treated with high dose radio-chemotherapy for hemato-oncological neoplasias and other cancers. Leuk Lymphoma 33:65–76. doi:10.3109/10428199909093726
Kidd SA, Eskenazi B, Wyrobek AJ (2001) Effects of male age on semen quality and fertility: a review of the literature. Fertil Steril 75:237–248
Palermo GD, Cohen J, Alikani M, Adler A, Rosenwaks Z (1995) Intracytoplasmic sperm injection: a novel treatment for all forms of male factor infertility. Fertil Steril 63:1231–1240
Damani M, Masters V, Meng M, Burgess C, Turek P, Oates R (2002) Postchemotherapy ejaculatory azoospermia: fatherhood with sperm from testis tissue with intracytoplasmic sperm injection. J Clin Oncol 20:930–936
Luck J, Peabody JW, Dresselhaus TR, Lee M, Glassman P (2000) How well does chart abstraction measure quality? A prospective comparison of standardized patients with the medical record. Am J Med 108:642–649
Dresselhaus TR, Luck J, Peabody JW (2002) The ethical problem of false positives: a prospective evaluation of physician reporting in the medical record. J Med Ethics 28:291–294
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of retrospective study, formal consent was not required.
Funding
The authors have no relevant funding or disclosures.
Additional information
Relevance
The implementation of an AYA program had a significantly positive effect on documentation of infertility risk and fertility preservation options and demonstrates the importance of dedicated programming in managing AYA cancer care.
Jeremy Lewin and Justin Ming Zheng Ma share first authorship.
Electronic supplementary material
Table 1
(DOCX 12 kb).
Rights and permissions
About this article
Cite this article
Lewin, J., Ma, J.M.Z., Mitchell, L. et al. The positive effect of a dedicated adolescent and young adult fertility program on the rates of documentation of therapy-associated infertility risk and fertility preservation options. Support Care Cancer 25, 1915–1922 (2017). https://doi.org/10.1007/s00520-017-3597-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-017-3597-8